Baby Intensive Early Active Treatment (babiEAT): A Pilot Randomised Controlled Trial of Feeding Therapy for Infants with Cerebral Palsy and Oropharyngeal Dysphagia
Abstract
1. Introduction
1.1. Background
1.2. Objectives
2. Materials and Methods
2.1. Trial Design
2.2. Participants
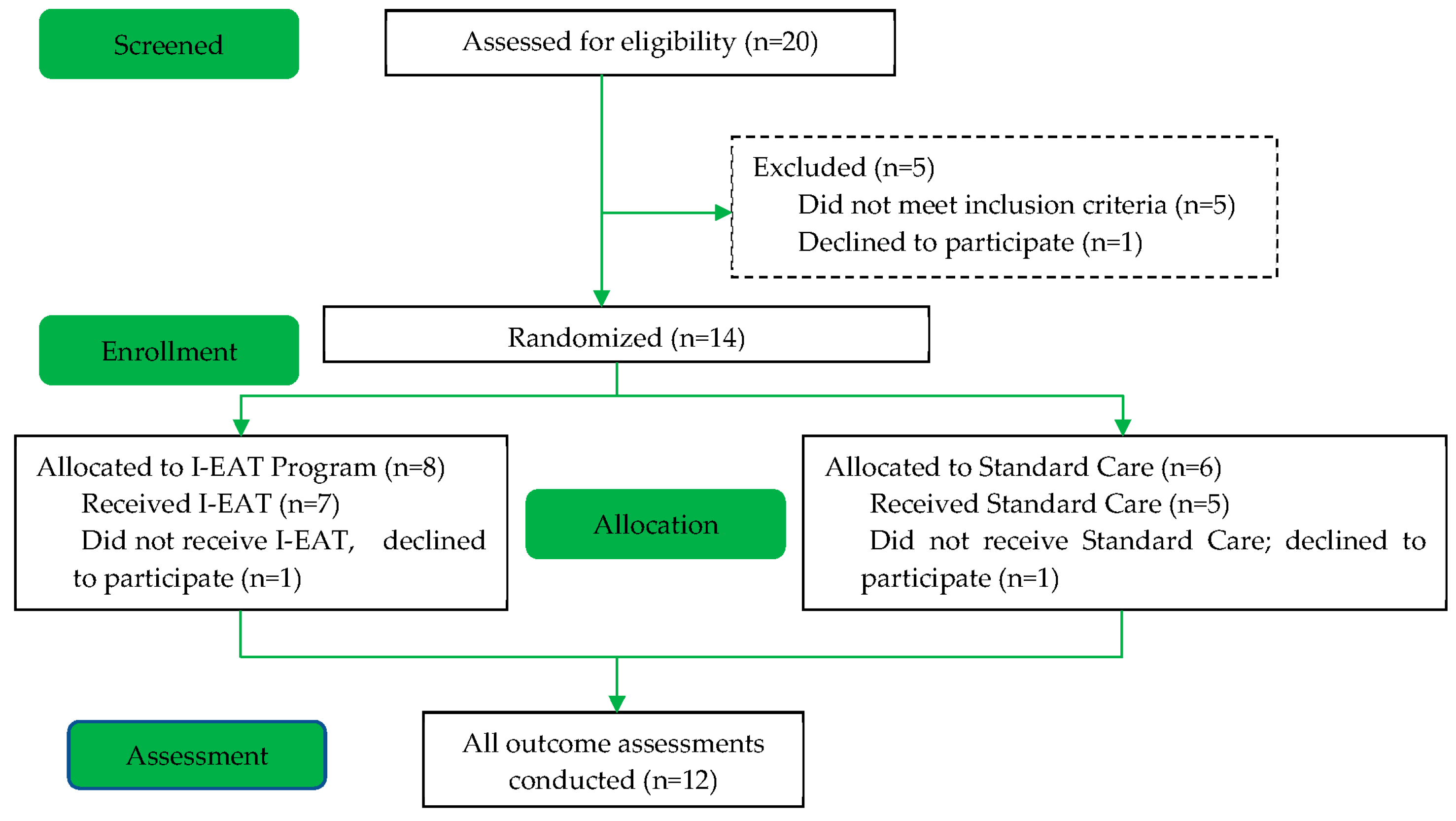
2.3. Recruitment and Randomisation
2.4. Interventions
2.4.1. babiEAT Program
2.4.2. Standard Care
2.5. Outcomes
- (i)
- Oral feeding efficiency: measured by percentage of total volume consumed during first five minutes of the mealtime. It is often recommended that purees and bottle feeding are the focus of intake for young children who have faltering growth as they are perceived to be the most efficient way of consuming nutrition orally. Therefore, there is a risk that feeding efficiency for the babiEAT group may diminish as they are challenged to increase intake of more advanced food and utilise more advanced drinking vessels. Percent volume consumed in the first 5 min is reflective of feeding efficiency [36], with a 30% consumption during this time indicating an efficient feed. Duration of mealtimes was also monitored, as a meal exceeding 30 min is indicative of inefficiency and a red flag for feeding difficulty or OPD [37];
- (ii)
- Feeding and swallowing skills: measured using the Schedule for Oral Motor Assessment (SOMA), recommended International Dysphagia Diet Standardisation Initiative (IDDSI) level, Functional Oral Intake Scale for Infants (FOISi), and the number of compensatory strategies utilised. The SOMA was selected as it is an OPD measurement tool shown to have the strongest validity, reliability, and clinical utility in young children with CP [38]. IDDSI is a universal objective framework for testing and classifying the texture or consistency of food and fluid. Each IDDSI level correlates with the functional skills required to manage that food or fluid; thus, it was employed in this study since change in IDDSI level recommendations is indicative of change in skills [39,40]. The FOISi was used in this study as it is a valid and reliable tool for classifying aspiration risk and OPD severity and evaluating effectiveness of intervention [41]. Compensatory strategies by their nature alter the task and reduce the degree of independence in feeding. They were therefore monitored in this study since a reduction in compensations is clinically associated with an improvement in skill and independent safe feeding.
- (iii)
- (iv)
- Health: measured by recording presence of known risk factors resulting from OPD in infants with CP, weight recorded as Z-score for age using the World Health Organization growth charts (as is convention for infants under 2-years), plus the number of chest infections and hospitalisations in the three months before and during intervention; and
- (v)
- Feeding-Related Quality of Life: Parents of newborns spend a substantial amount of time feeding their children, and a parent’s perception of success is often intertwined with their ability to nourish their baby. The Feeding Swallowing Impact Scale (FSIS), a valid tool for measuring health-related quality of life, was completed by caregivers to determine the impact and stress that feeding difficulties have on the participants’ caregivers [43]. FSIS scores are categorised into three subtests: those that measure impact of the infants’ feeding difficulties on the caregivers’ ability to carry out daily activities, the caregivers’ worry, and the caregiver’s ability to feed their child. Likert scores for each subtest were combined to create a score for each of the three subtests.
2.6. Logbooks
2.7. Blinding
2.8. Statistical Methods
2.9. Impact of COVID-19 Pandemic
3. Results
3.1. Baseline Characteristics
3.2. Intervention
3.2.1. Location
3.2.2. Intensity
3.2.3. Type of Intervention
3.3. Feasibility and Acceptability
3.4. Feeding Efficiency
3.5. Swallowing Skills
3.5.1. Fluids
3.5.2. Solids
3.6. Mealtime Duration
3.7. Health Outcomes
3.8. Quality of Life
4. Discussion
4.1. Evidence-Based Practice
4.2. Feasibility and Acceptability
4.3. Feeding Skill Development
4.4. Health
4.5. Quality of Life
4.6. Limitations
4.7. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [PubMed]
- McIntyre, S.; Goldsmith, S.; Webb, A.; Ehlinger, V.; Hollung, S.J.; McConnell, K.; Arnaud, C.; Smithers-Sheedy, H.; Oskoui, M.; Khandaker, G.; et al. Global prevalence of cerebral palsy: A systematic analysis. Dev. Med. Child Neurol. 2022, 64, 1494–1506. [Google Scholar] [CrossRef] [PubMed]
- Benfer, K.A.; Weir, K.A.; Bell, K.L.; Ware, R.S.; Davies, P.S.; Boyd, R.N. Oropharyngeal dysphagia and gross motor skills in children with cerebral palsy. Pediatrics 2013, 131, e1553–e1562. [Google Scholar] [CrossRef]
- Calis, E.A.; Veugelers, R.; Sheppard, J.J.; Tibboel, D.; Evenhuis, H.M.; Penning, C. Dysphagia in children with severe generalized cerebral palsy and intellectual disability. Dev. Med. Child Neurol. 2008, 50, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Erkin, G.; Culha, C.; Ozel, S.; Kirbiyik, E.G. Feeding and gastrointestinal problems in children with cerebral palsy. Int. J. Rehabil. Res. 2010, 33, 218–224. [Google Scholar] [CrossRef]
- Sullivan, P.; Lambert, B.; Rose, M.; Ford-Adams, M.; Johnson, A.; Griffiths, P. Prevalence and severity of feeding and nutritional problems in children with neurological impairment: Oxford Feeding Study. Dev. Med. Child Neurol. 2000, 42, 674–680. [Google Scholar] [CrossRef]
- Reid, S.M.; Carlin, J.B.; Reddihough, D.S. Survival of individuals with cerebral palsy born in Victoria, Australia, between 1970 and 2004. Dev. Med. Child Neurol. 2012, 54, 353–360. [Google Scholar] [CrossRef]
- Strauss, D.; Cable, W.; Shavelle, R. Causes of excess mortality in cerebral palsy. Dev. Med. Child Neurol. 1999, 41, 580–585. [Google Scholar] [CrossRef]
- Reilly, S.; Skuse, D.; Poblete, X. Prevalence of feeding problems and oral motor dysfunction in children with cerebral palsy: A community survey. J. Pediatr. 1996, 129, 877–882. [Google Scholar] [CrossRef]
- Cerebral Palsy Alliance. Australian Cerebral Palsy Register Report 2018. Available online: https://cpregister.com/wp-content/uploads/2019/02/Report-of-the-Australian-Cerebral-Palsy-Register-Birth-Years-1995-2012.pdf (accessed on 27 March 2023).
- Goday, P.S.; Huh, S.Y.; Silverman, A.; Lukens, C.T.; Dodrill, P.; Cohen, S.S.; Delaney, A.L.; Feuling, M.B.; Noel, R.J.; Gisel, E.; et al. Pediatric Feeding Disorder: Consensus Definition and Conceptual Framework. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 124–129. [Google Scholar] [CrossRef]
- Logemann, J.A. Approaches to management of disordered swallowing. Baillière’s Clin. Gastroenterol. 1991, 5, 269–280. [Google Scholar] [CrossRef]
- Khamis, A.; Novak, I.; Morgan, C.; Tzannes, G.; Pettigrew, J.; Cowell, J.; Badawi, N. Motor Learning Feeding Interventions for Infants at Risk of Cerebral Palsy: A Systematic Review. Dysphagia 2020, 35, 1–17. [Google Scholar] [CrossRef]
- Arvedson, J.; Clark, H.; Lazarus, C.; Schooling, T.; Frymark, T. Evidence-based systematic review: Effects of oral motor interventions on feeding and swallowing in preterm infants. Am. J. Speech-Lang. Pathol. 2010, 19, 321–340. [Google Scholar] [CrossRef]
- Arvedson, J.; Clark, H.; Lazarus, C.; Schooling, T.; Frymark, T. The effects of oral-motor exercises on swallowing in children: An evidence-based systematic review. Dev. Med. Child Neurol. 2010, 52, 1000–1013. [Google Scholar] [CrossRef]
- Greene, Z.; O’Donnell, C.P.; Walshe, M. Oral stimulation for promoting oral feeding in preterm infants. Cochrane Database Syst. Rev. 2016, 9, CD009720. [Google Scholar] [CrossRef] [PubMed]
- Boiron, M.; Nobrega, L.D.; Roux, S.; Henrot, A.; Saliba, E. Effects of oral stimulation and oral support on non-nutritive sucking and feeding performance in preterm infants. Dev. Med. Child Neurol. 2007, 49, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Fucile, S.; Gisel, E.; Lau, C. Oral stimulation accelerates the transition from tube to oral feeding in preterm infants. J. Pediatr. 2002, 141, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Fucile, S.; McFarland, D.H.; Gisel, E.G.; Lau, C. Oral and nonoral sensorimotor interventions facilitate suck-swallow-respiration functions and their coordination in preterm infants. Early Hum. Dev. 2012, 88, 345–350. [Google Scholar] [CrossRef]
- Khamis, A.; Badawi, N.; Morgan, C.; Galea, C.; Novak, I. International Survey of Dysphagia Practice; Practice and Evidence Don’t Align. 2023; Under Review. [Google Scholar]
- Zimmerman, E.; Carnaby, G.; Lazarus, C.L.; Malandraki, G.A. Motor Learning, Neuroplasticity, and Strength and Skill Training: Moving From Compensation to Retraining in Behavioral Management of Dysphagia. Am. J. Speech Lang. Pathol. 2020, 29, 1065–1077. [Google Scholar] [CrossRef]
- Morgan, C.; Fetters, L.; Adde, L.; Badawi, N.; Bancale, A.; Boyd, R.N.; Chorna, O.; Cioni, G.; Damiano, D.L.; Darrah, J.; et al. Early Intervention for Children Aged 0 to 2 Years with or at High Risk of Cerebral Palsy: International Clinical Practice Guideline Based on Systematic Reviews. JAMA Pediatr. 2021, 175, 846–858. [Google Scholar] [CrossRef]
- Robbins, J.; Butler, S.G.; Daniels, S.K.; Gross, R.D.; Langmore, S.; Lazarus, C.L.; Martin-Harris, B.; McCabe, D.J.; Musson, N.D.; Rosenbek, J.C. Swallowing and dysphagia rehabilitation: Translating principles of neural plasticity into clinically oriented evidence. J. Speech Lang. Hear. Res. 2008, 51, S276–S300. [Google Scholar] [CrossRef]
- Kleim, J.A.; Jones, T.A. Principles of experience-dependent neural plasticity: Implications for rehabilitation after brain damage. J. Speech Lang. Hear. Res. 2008, 51, S225–S239. [Google Scholar] [CrossRef]
- Sheppard, J.J. Using motor learning approaches for treating swallowing and feeding disorders: A review. Lang. Speech Hear. Serv. Sch. 2008, 39, 227–236. [Google Scholar] [CrossRef]
- Gillman, A.; Winkler, R.; Taylor, N.F. Implementing the Free Water Protocol does not Result in Aspiration Pneumonia in Carefully Selected Patients with Dysphagia: A Systematic Review. Dysphagia 2017, 32, 345–361. [Google Scholar] [CrossRef]
- Gosa, M.; Schooling, T.; Coleman, J. Thickened Liquids as a Treatment for Children With Dysphagia and Associated Adverse Effects. ICAN Infant Child Adolesc. Nutr. 2011, 3, 344–350. [Google Scholar] [CrossRef]
- Lau, C.; Fucile, S.; Gisel, E.G. Impact of nonnutritive oral motor stimulation and infant massage therapy on oral feeding skills of preterm infants. J. Neonatal-Perinat. Med. 2012, 5, 311–317. [Google Scholar] [CrossRef]
- Gisel, E.G. Effect of oral sensorimotor treatment on measures of growth and efficiency of eating in the moderately eating-impaired child with cerebral palsy. Dysphagia 1996, 11, 48–58. [Google Scholar] [CrossRef]
- Ottenbacher, K.; Scoggins, A.; Wayland, J. The effectiveness of a program of oral sensory-motor therapy with the severely and profoundly developmentally disabled. Occup. Ther. J. Res. 1981, 1, 147–160. [Google Scholar] [CrossRef]
- Sjögreen, L.; Tulinius, M.; Kiliaridis, S.; Lohmander, A. The effect of lip strengthening exercises in children and adolescents with myotonic dystrophy type 1. Int. J. Pediatr. Otorhinolaryngol. 2010, 74, 1126–1134. [Google Scholar] [CrossRef]
- Serel Arslan, S.; Demir, N.; Karaduman, A.A. Effect of a new treatment protocol called Functional Chewing Training on chewing function in children with cerebral palsy: A double-blind randomised controlled trial. J. Oral Rehabil. 2017, 44, 43–50. [Google Scholar] [CrossRef]
- Bernbaum, J.C.; Pereira, G.R.; Watkins, J.B.; Peckham, G.J. Nonnutritive sucking during gavage feeding enhances growth and maturation in premature infants. Pediatrics 1983, 71, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, S.; Prakash, O.; Gupta, A.; Mohan, M.; Anand, N. Evaluation of beneficial effects of nonnutritive sucking in preterm infants. Indian Pediatr. 1990, 27, 263–266. [Google Scholar] [PubMed]
- White-Traut, R.C.; Nelson, M.N.; Silvestri, J.M.; Vasan, U.; Littau, S.; Meleedy-Rey, P.; Gu, G.; Patel, M. Effect of auditory, tactile, visual, and vestibular intervention on length of stay, alertness, and feeding progression in preterm infants. Dev. Med. Child Neurol. 2002, 44, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Griffith, T.; Rankin, K.; White-Traut, R. The Relationship Between Behavioral States and Oral Feeding Efficiency in Preterm Infants. Adv. Neonatal Care 2017, 17, E12–E19. [Google Scholar] [CrossRef] [PubMed]
- Weir, K.; McMahon, S.; Barry, L.; Masters, I.B.; Chang, A.B. Clinical signs and symptoms of oropharyngeal aspiration and dysphagia in children. Eur. Respir. J. 2009, 33, 604–611. [Google Scholar] [CrossRef]
- Benfer, K.A.; Weir, K.A.; Boyd, R.N. Clinimetrics of measures of oropharyngeal dysphagia for preschool children with cerebral palsy and neurodevelopmental disabilities: A systematic review. Dev. Med. Child Neurol. 2012, 54, 784–795. [Google Scholar] [CrossRef]
- Cichero, J.A.Y. Evaluating chewing function: Expanding the dysphagia field using food oral processing and the IDDSI framework. J. Texture Stud. 2020, 51, 56–66. [Google Scholar] [CrossRef]
- Su, M.; Zheng, G.; Chen, Y.; Xie, H.; Han, W.; Yang, Q.; Sun, J.; Lv, Z.; Chen, J. Clinical applications of IDDSI framework for texture recommendation for dysphagia patients. J. Texture Stud. 2018, 49, 2–10. [Google Scholar] [CrossRef]
- Yi, Y.G.; Shin, H.I. Psychometrics of the Functional Oral Intake Scale for Infants. Front. Pediatr. 2019, 7, 156. [Google Scholar] [CrossRef]
- Cusick, A.; McIntyre, S.; Novak, I.; Lannin, N.; Lowe, K. A comparison of goal attainment scaling and the Canadian Occupational Performance Measure for paediatric rehabilitation research. Pediatr. Rehabil. 2006, 9, 149–157. [Google Scholar] [CrossRef]
- Lefton-Greif, M.A.; Okelo, S.O.; Wright, J.M.; Collaco, J.M.; McGrath-Morrow, S.A.; Eakin, M.N. Impact of children’s feeding/swallowing problems: Validation of a new caregiver instrument. Dysphagia 2014, 29, 671–677. [Google Scholar] [CrossRef]
- Arvedson, J.C. Feeding children with cerebral palsy and swallowing difficulties. Eur. J. Clin. Nutr. 2013, 67 (Suppl. S2), S9–S12. [Google Scholar] [CrossRef]
- Gorter, J.W.; Ketelaar, M.; Rosenbaum, P.; Helders, P.J.; Palisano, R. Use of the GMFCS in infants with CP: The need for reclassification at age 2 years or older. Dev. Med. Child Neurol. 2009, 51, 46–52. [Google Scholar] [CrossRef]
- Ko, M.J.; Kang, M.J.; Ko, K.J.; Ki, Y.O.; Chang, H.J.; Kwon, J.Y. Clinical Usefulness of Schedule for Oral-Motor Assessment (SOMA) in Children with Dysphagia. Ann. Rehabil. Med. 2011, 35, 477–484. [Google Scholar] [CrossRef]
- Speyer, R.; Cordier, R.; Parsons, L.; Denman, D.; Kim, J.H. Psychometric Characteristics of Non-instrumental Swallowing and Feeding Assessments in Pediatrics: A Systematic Review Using COSMIN. Dysphagia 2018, 33, 1–14. [Google Scholar] [CrossRef]
| Principles of Neuroplasticity | Principles of Motor Learning | Application to Feeding Interventions |
|---|---|---|
| Use it or lose it [23,24] | Feeding skills may plateau or diminish if infant receives no or limited opportunity to utilize oropharyngeal skills for feeding and/or oral exploration. | |
| Timing [23,24] | Begin intervention as early as possible i.e., with infants under 12 months. | |
| Maximize opportunity for intensive practice [23,24,25] | Use it and improve it. Repetition is essential for skill acquisition. Feeding skills may improve if opportunity is given to safely practice challenging skills. Intense practice and support during early learning phase and tapered off as skill is mastered. | |
| Specificity [23,24,25] | Practice during task as close to meal as possible i.e., interventions involving food/fluid and swallowing (while closely monitoring safety) | |
| Simplification [25] | If tasks are too difficult, infants are at risk of developing maladaptive motor patterns. Compensatory strategies can assist in motor learning if they are used to simplify the task in early stages and are titrated down as soon as is safe to do so, to work towards performing the task unaided. Strategies include modifying texture or sensory features of food or fluid, using different drinking vessels, or slowing the rate of the feed. | |
| Attention and motivation [23,24] | Salient and interesting tasks can be achieved during snacks and at meals using preferred flavours and praise from caregivers. | |
| Extrinsic feedback [23,24] | Knowledge of performance, remaining time or mouthfuls (with simple visuals/prompts where appropriate) and praise provided frequently during early learning and intermittently as skill is mastered | |
| Implicit learning [23,24] | Natural positive reinforcement and feedback provided through enjoyment of food flavours and reduction in deleterious responses e.g., gagging, coughing, choking | |
| Blocked practice [23,24] | Practicing desired skill with one food or drink | |
| Random practice [23,24] | Alternate fluid, chewable and non-chewable textures with every mouthful, once mastered in isolation | |
| Distributed practice [23,24] | Practice skill during many (short) sessions over a longer period (e.g., snacks throughout the day) | |
| Complexity [23,24] | Continual reassessment, upgrade goals, and reducing support to ensure task is as difficult as possible while maintaining safety | |
| Transfer of learning [26,27] | Once skill is mastered with familiar foods in familiar environments, skills can be practiced with novel foods and environments to encourage generalisation of skills. | |
| Intensive Early Active Treatment (babiEAT) Program | Standard Care | |
|---|---|---|
| HOW MUCH | 60-min sessions twice weekly for 4 weeks followed by 60 min sessions once weekly for 8 weeks | As per service protocol, which varies but is typically weekly-to-monthly |
| HOW LONG | 12 weeks | 12 weeks |
| WHERE | Participant’s home | Clinical setting or home, as per service protocol |
| WHO | Individual session, caregiver actively involved | Individual or group or consultation, as per service protocol |
| WHAT |
|
|
| HOW WELL | Caregivers were instructed to complete a logbook of adverse events and time spent on home program. | Caregivers were instructed to keep a logbook of adverse events, number of sessions, recommendations, and time spent on home program. |
| Characteristic | babiEAT (n = 8) | Standard Care (n = 6) | p Value |
|---|---|---|---|
| Corrected age at baseline, mean (SD), months | 9.63 (2.33) | 9.33 (1.75) | 0.46 |
| Sex: M/F | 4/4 | 2/4 | |
| Weight Z-Scores | −0.09 (0.59) | −0.62 (1.59) | 0.03 |
| Percentage of volume consumed in first 5 min-fluids | 41.27 (35.61) | 32.28 (14.99) | 0.01 |
| Percentage of volume consumed in first 5 min-solids | 68.75 (25.99) | 44.5 (22.26) | 0.38 |
| Mealtime duration | 38.13 (6.51) | 29.17 (6.65) | 0.54 |
| SOMA Bottle: Normal/Dysfunctional | 6/2 | 3/3 | |
| SOMA Trainer Cup: Normal/Dysfunctional | 2/6 | 1/5 | |
| SOMA Cup: Normal/Dysfunctional | 1/7 | 2/4 | |
| SOMA Puree: Normal/Dysfunctional | 3/5 | 3/3 | |
| SOMA Semi-Solids: Normal/Dysfunctional | 2/6 | 3/3 | |
| SOMA Solids: Normal/Dysfunctional | 1/7 | 0/6 | |
| SOMA Cracker: Normal/Dysfunctional | 2/6 | 1/5 | |
| IDDSI Level 0-Thin Fluids | n = 5 | n = 3 | |
| IDDSI Level 1-Slightly Thick Fluids | n = 3 | n = 3 | |
| IDDSI Level 2-Moderately Thick Fluids | n = 0 | n = 0 | |
| IDDSI Level 3-Extremely Thick Fluids | n = 0 | n = 0 | |
| IDDSI Level 4–Puree | n = 3 | n = 2 | |
| IDDSI Level 5-Minced & Moist | n = 4 | n = 3 | |
| IDDSI Level 6–Soft | n = 0 | n = 1 | |
| IDDSI Level 7–Regular | n = 1 | n = 0 | |
| FOISi Level 1 | n = 0 | n = 0 | |
| FOISi Level 2 | n = 0 | n = 0 | |
| FOISi Level 3 | n = 2 | n = 0 | |
| FOISi Level 4 | n = 5 | n = 5 | |
| FOISi Level 5 | n = 1 | n = 1 | |
| Number of Compensations-Bottle, mean (SD) | 2.25 (1.83) | 3.50 (2.35) | 1.00 |
| Number of Compensations–Straw, mean (SD) | 7.88 (3.36) | 8.33 (2.66) | 0.61 |
| Number of Compensations-Cup, mean (SD) | 9.63 (1.06) | 8.50 (2.35) | 0.01 |
| Number of Compensations-Puree, mean (SD) | 2.25 (2.05) | 4.67 (2.50) | 0.78 |
| Number of Compensations-Minced and Moist, mean (SD) | 6.00 (3.63) | 5.83 (2.40) | 0.14 |
| Number of Compensations-Soft/Regular, mean (SD) | 8.00 (3.74) | 8.83 (2.86) | 0.33 |
| Number of Compensations-Transitional, mean (SD) | 4.50 (3.74) | 5.83 (2.48) | 0.33 |
| GAS t-score-Fluids, mean (SD) | 25.46 (0) | 25.46 (0) | - |
| GAS t-score-Solids, mean (SD) | 25.46 (0) | 25.46 (0) | - |
| Chest Infections in Past 3 months | 0.63 (0.52) | 0.33 (0.52) | 0.77 |
| Hospitalisations in Past 3 months | 0.63 (0.52) | 0.33 (0.52) | 0.77 |
| FSIS Impact on Daily Activities | 15.13 (5.79) | 14.33 (6.41) | 0.77 |
| FSIS Worry | 23.25 (6.18) | 23.17 (5.98) | 0.85 |
| FSIS Problems Feeding Child | 12.63 (4.24) | 16.17 (5.67) | 0.92 |
| Outcome Measure | babiEAT (n = 7) | Standard Care (n = 5) | p Value |
|---|---|---|---|
| Number of therapy sessions received, median, (IQR) | 16 (16–16) | 2 (0–4) | <0.001 * |
| Hours spent on home program, mean (SD) | 53.43 (0.49) | 9.9 (6.59) | <0.001 * |
| FIPQ Q1, median, (IQR) | 10 (8–10) | 5 (1–10) | 0.07 |
| FIPQ Q2, median, (IQR) | 10 (9–10) | 5 (1–9) | 0.048 * |
| FIPQ Q3, median, (IQR) | 5 (2–8) | 5 (5–5) | 0.27 |
| FIPQ Q4, median, (IQR) | 10 (10–10) | 8 (6–10) | 0.048 * |
| FIPQ Q5, median, (IQR) | 9 (7–10) | 9 (6–10) | 0.64 |
| FIPQ Q6, median, (IQR) | 10 (9–10) | 8 (5–10) | 0.27 |
| FIPQ Q7, median, (IQR) | 10 (10–10) | 8 (5–10) | 0.15 |
| FIPQ Q8, median, (IQR) | 10 (9–10) | 9 (6–10) | 0.28 |
| FIPQ Q9, median, (IQR) | 10 (8–10) | 9 (7–10) | 0.64 |
| Percentage of volume consumed in first 5 min-fluids | 44.00 (37.48) | 29.80 (20.44) | 0.03 * |
| Percentage of volume consumed in first 5 min-solids | 28.29 (33.97) | 35.80 (38.86) | 0.63 |
| Mealtime duration (mins) | 26.43 (3.78) | 31.00 (8.22) | 0.53 |
| SOMA Bottle: Advanced or Maintained Normal/Regressed or Maintained Dysfunctional | 6/1 | 3/2 | 0.31 |
| SOMA Trainer Cup (straw): Advanced or Maintained Normal/Regressed or Maintained Dysfunctional | 4/3 | 1/4 | 0.19 |
| SOMA Cup: Advanced or Maintained Normal/Regressed or Maintained Dysfunctional | 6/1 | 2/3 | 0.09 |
| SOMA Puree: Advanced or Maintained Normal/Regressed or Maintained Dysfunctional | 6/1 | 2/3 | 0.09 |
| SOMA Semi-Solids (Minced and Moist or Soft): Advanced or Maintained Normal/Regressed or Maintained Dysfunctional | 4/3 | 3/2 | 0.92 |
| SOMA Solids (Regular): Advanced or Maintained Normal/Regressed or Maintained Dysfunctional | 3/4 | 0/5 | 0.047 * |
| SOMA Cracker (Transitional): Advanced or Maintained Normal/Regressed or Maintained Dysfunctional | 3/4 | 1/4 | 0.40 |
| IDDSI Fluids: Advanced or Maintained Maximum/Regressed or Maintained Modified | 6/1 | 5/0 | 0.29 |
| IDDSI Solids: Advanced or Maintained Maximum/Regressed or Maintained Modified | 6/1 | 1/4 | 0.02 * |
| FOIS: Advanced or Maintained Maximum/Regressed or Maintained Dysfunctional | 6/1 | 1/4 | 0.02 * |
| Number of Compensations-Bottle, mean (SD) | 0.71 (1.11) | 2.60 (3.44) | 0.28 |
| Number of Compensations-Straw, mean (SD) | 5.00 (3.61) | 7.20 (3.90) | 0.36 |
| Number of Compensations-Cup, mean (SD) | 4.14 (2.67) | 6.80 (3.27) | 0.02 * |
| Number of Compensations-Puree, mean (SD) | 0.71 (1.89) | 1.80 (2.68) | 0.98 |
| Number of Compensations-Minced and Moist or Soft, mean (SD) | 3.00 (3.56) | 6.20 (3.56) | 0.11 |
| Number of Compensations-Regular, mean (SD) | 4.14 (4.38) | 8.00 (2.74) | 0.19 |
| Number of Compensations-Transitional, mean (SD) | 2.57 (3.74) | 4.80 (3.11) | 0.42 |
| GAS T-score-Fluids, mean (SD) | 58.57 (12.15) | 40.00 (17.32) | 0.05 |
| GAS T-score-Solids, mean (SD) | 55.71 (16.18) | 46 (13.42) | 0.30 |
| Weight Z-Scores (WHO) | 35.99 (34.82) | 32.19 (34.40) | 0.51 |
| Chest Infections in Past 3 months | 0.00 (0.00) | 0.020 (0.45) | 0.14 |
| Hospitalisations in Past 3 months | 0.00 (0.00) | 0.020 (0.45) | 0.14 |
| FSIS Impact on Daily Activities | 10.86 (3.24) | 15.00 (4.00) | <0.001 * |
| FSIS Worry | 16.43 (5.32) | 24.40 (3.29) | <0.001 * |
| FSIS Problems Feeding Child | 9.29 (2.93) | 17.20 (4.01) | 0.03 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khamis, A.; Badawi, N.; Morgan, C.; Novak, I. Baby Intensive Early Active Treatment (babiEAT): A Pilot Randomised Controlled Trial of Feeding Therapy for Infants with Cerebral Palsy and Oropharyngeal Dysphagia. J. Clin. Med. 2023, 12, 2677. https://doi.org/10.3390/jcm12072677
Khamis A, Badawi N, Morgan C, Novak I. Baby Intensive Early Active Treatment (babiEAT): A Pilot Randomised Controlled Trial of Feeding Therapy for Infants with Cerebral Palsy and Oropharyngeal Dysphagia. Journal of Clinical Medicine. 2023; 12(7):2677. https://doi.org/10.3390/jcm12072677
Chicago/Turabian StyleKhamis, Amanda, Nadia Badawi, Catherine Morgan, and Iona Novak. 2023. "Baby Intensive Early Active Treatment (babiEAT): A Pilot Randomised Controlled Trial of Feeding Therapy for Infants with Cerebral Palsy and Oropharyngeal Dysphagia" Journal of Clinical Medicine 12, no. 7: 2677. https://doi.org/10.3390/jcm12072677
APA StyleKhamis, A., Badawi, N., Morgan, C., & Novak, I. (2023). Baby Intensive Early Active Treatment (babiEAT): A Pilot Randomised Controlled Trial of Feeding Therapy for Infants with Cerebral Palsy and Oropharyngeal Dysphagia. Journal of Clinical Medicine, 12(7), 2677. https://doi.org/10.3390/jcm12072677








