Dyadic Interactions of Treatment-Resistant Schizophrenia Patients Having Followed Virtual Reality Therapy: A Content Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Data Collection
2.3. Data Analysis
2.3.1. Dyadic Interactions
2.3.2. Analysis of Dyads
3. Results
3.1. Sample Characteristics
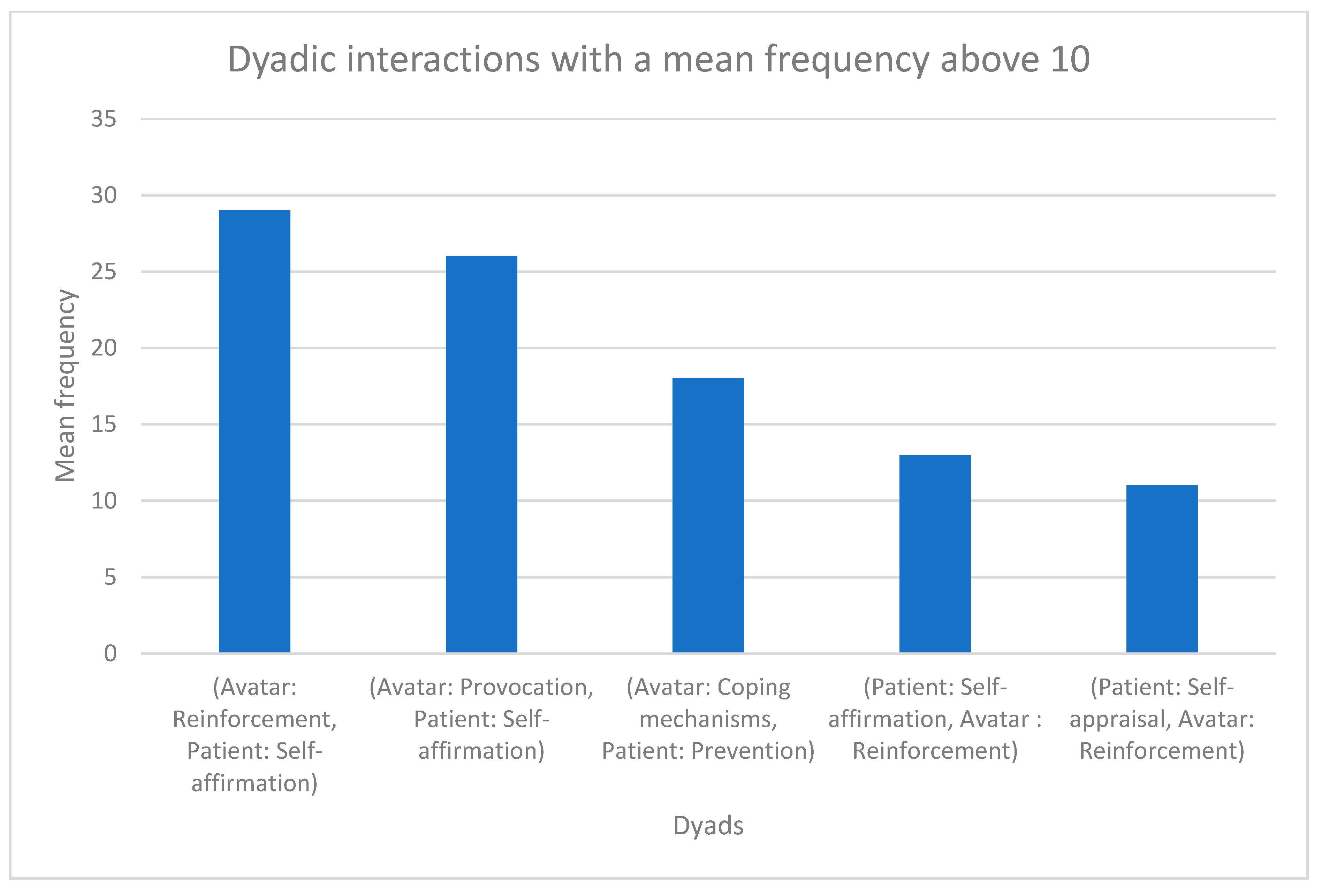
3.2. Dyadic Interactions
3.2.1. Avatar: Reinforcement, Patient: Self-Affirmation
3.2.2. Avatar: Provocation, Patient: Self-Affirmation
3.2.3. Avatar: Coping Mechanisms, Patient: Prevention
3.2.4. Patient: Self-Affirmation, Avatar: Reinforcement
3.2.5. Patient: Self-Appraisal, Avatar: Reinforcement
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weissman, M.; Cuijpers, P. Psychotherapy over the Last Four Decades. Harv. Rev. Psychiatry 2017, 25, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Locher, C.; Meier, S.; Gaab, J. Psychotherapy: A World of Meanings. Front. Psychol. 2019, 10, 460. [Google Scholar] [CrossRef] [PubMed]
- Brent, D.A.; Kolko, D.J. Psychotherapy: Definitions, mechanisms of action, and relationship to etiological models. J. Abnorm. Child Psychol. 1998, 26, 17–25. [Google Scholar] [CrossRef]
- Strauman, T.J.; Goetz, E.L.; Detloff, A.M.; MacDuffie, K.E.; Zaunmüller, L.; Lutz, W. Self-Regulation and Mechanisms of Action in Psychotherapy: A Theory-Based Translational Perspective. J. Pers. 2013, 81, 542–553. [Google Scholar] [CrossRef] [PubMed]
- Tzur Bitan, D.; Shalev, S.; Abayed, S. Therapists’ Views of Mechanisms of Change in Psychotherapy: A Mixed-Method Approach. Front. Psychol. 2022, 13, 565800. [Google Scholar] [CrossRef]
- Bachelor, A. Clients’ and Therapists’ views of the therapeutic alliance: Similarities, differences and relationship to therapy outcome. Clin. Psychol. Psychother. 2013, 20, 118–135. [Google Scholar] [CrossRef]
- Parth, K.; Datz, F.; Seidman, C.; Löffler-Stastka, H. Transference and countertransference: A review. Bull. Menn. Clin. 2017, 81, 167–211. [Google Scholar] [CrossRef]
- Zinn, W.M. Transference Phenomena in Medical Practice: Being Whom the Patient Needs. Ann. Intern. Med. 1990, 113, 293–298. [Google Scholar] [CrossRef]
- Jones, A.C. Transference and countertransference. Perspect. Psychiatr. Care 2004, 40, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Prasko, J.; Ociskova, M.; Vanek, J.; Burkauskas, J.; Slepecky, M.; Bite, I.; Krone, I.; Sollar, T.; Juskiene, A. Managing Transference and Countertransference in Cognitive Behavioral Supervision: Theoretical Framework and Clinical Application. Psychol. Res. Behav. Manag. 2022, 15, 2129–2155. [Google Scholar] [CrossRef]
- Hayes, J.A.; Gelso, C.J.; Goldberg, S.; Kivlighan, D.M. Countertransference management and effective psychotherapy: Meta-analytic findings. Psychotherapy 2018, 55, 496–507. [Google Scholar] [CrossRef]
- Prasko, J.; Diveky, T.; Grambal, A.; Kamaradova, D.; Mozny, P.; Sigmundova, Z.; Slepecky, M.; Vyskocilova, J. Transference and countertransference in cognitive behavioral therapy. Biomed Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 2010, 154, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Polese, D.; Fornaro, M.; Palermo, M.; De Luca, V.; de Bartolomeis, A. Treatment-Resistant to Antipsychotics: A Resistance to Everything? Psychotherapy in Treatment-Resistant Schizophrenia and Nonaffective Psychosis: A 25-Year Systematic Review and Exploratory Meta-Analysis. Front. Psychiatry 2019, 10, 210. [Google Scholar] [CrossRef] [PubMed]
- Tandon, R.; Gaebel, W.; Barch, D.M.; Bustillo, J.; Gur, R.E.; Heckers, S.; Malaspina, D.; Owen, M.J.; Schultz, S.; Tsuang, M.; et al. Definition and description of schizophrenia in the DSM-5. Schizophr. Res. 2013, 150, 3–10. [Google Scholar] [CrossRef]
- McCutcheon, R.A.; Abi-Dargham, A.; Howes, O.D. Schizophrenia, Dopamine and the Striatum: From Biology to Symptoms. Trends Neurosci. 2019, 42, 205–220. [Google Scholar] [CrossRef]
- Weinstein, J.J.; Chohan, M.O.; Slifstein, M.; Kegeles, L.S.; Moore, H.; Abi-Dargham, A. Pathway-Specific Dopamine Abnormalities in Schizophrenia. Biol. Psychiatry 2016, 81, 31–42. [Google Scholar] [CrossRef]
- Correll, C.U.; Schooler, N.R. Negative Symptoms in Schizophrenia: A Review and Clinical Guide for Recognition, Assessment, and Treatment. Neuropsychiatr. Dis. Treat. 2020, 16, 519–534. [Google Scholar] [CrossRef]
- Elkis, H.; Buckley, P.F. Treatment-Resistant Schizophrenia. Psychiatr. Clin. N. Am. 2016, 39, 239–265. [Google Scholar] [CrossRef]
- Miyamoto, S.; Jarskog, L.F.; Fleischhacker, W.W. New therapeutic approaches for treatment-resistant schizophrenia: A look to the future. J. Psychiatr. Res. 2014, 58, 1–6. [Google Scholar] [CrossRef]
- Nucifora, F.C.; Woznica, E.; Lee, B.J.; Cascella, N.; Sawa, A. Treatment resistant schizophrenia: Clinical, biological, and therapeutic perspectives. Neurobiol. Dis. 2019, 131, 104257. [Google Scholar] [CrossRef] [PubMed]
- Lally, J.; Gaughran, F. Treatment resistant schizophrenia—Review and a call to action. Ir. J. Psychol. Med. 2018, 36, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Rakitzi, S.; Georgila, P. Integrated Psychological Therapy and Treatment-Resistant Schizophrenia: Initial Findings. Psychiatry 2019, 82, 354–367. [Google Scholar] [CrossRef]
- Morrison, A.P.; Pyle, M.; Gumley, A.; Schwannauer, M.; Turkington, D.; MacLennan, G.; Norrie, J.; Hudson, J.; Bowe, S.; French, P.; et al. Cognitive–behavioural therapy for clozapine-resistant schizophrenia: The FOCUS RCT. Health Technol. Assess. 2019, 23, 1–144. [Google Scholar] [CrossRef] [PubMed]
- Morrison, A.P.; Pyle, M.; Gumley, A.; Schwannauer, M.; Turkington, D.; MacLennan, G.; Norrie, J.; Hudson, J.; Bowe, E.S.; French, P.; et al. Cognitive behavioural therapy in clozapine-resistant schizophrenia (FOCUS): An assessor-blinded, randomised controlled trial. Lancet Psychiatry 2018, 5, 633–643. [Google Scholar] [CrossRef]
- Burns, A.M.N.; Erickson, D.H.; Brenner, C.A. Cognitive-Behavioral Therapy for Medication-Resistant Psychosis: A Meta-Analytic Review. Psychiatr. Serv. 2014, 65, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Leff, J.; Williams, G.; Huckvale, M.; Arbuthnot, M.; Leff, A.P. Avatar therapy for persecutory auditory hallucinations: What is it and how does it work? Psychosis 2014, 6, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Craig, T.K.; Calafell, M.D.M.R.; Ward, T.; Leff, J.P.; Huckvale, M.; Howarth, E.; Emsley, R.; Garety, P. AVATAR therapy for auditory verbal hallucinations in people with psychosis: A single-blind, randomised controlled trial. Lancet Psychiatry 2018, 5, 31–40. [Google Scholar] [CrossRef]
- Du Sert, O.P.; Potvin, S.; Lipp, O.; Dellazizzo, L.; Laurelli, M.; Breton, R.; Lalonde, P.; Phraxayavong, K.; O’Connor, K.; Pelletier, J.F.; et al. Virtual reality therapy for refractory auditory verbal hallucinations in schizophrenia: A pilot clinical trial. Schizophr. Res. 2018, 197, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Dellazizzo, L.; Potvin, S.; Phraxayavong, K.; Dumais, A. One-year randomized trial comparing virtual reality-assisted therapy to cognitive–behavioral therapy for patients with treatment-resistant schizophrenia. NPJ Schizophr. 2021, 7, 9. [Google Scholar] [CrossRef]
- Dellazizzo, L.; Percie du Sert, O.; Phraxayavong, K.; Potvin, S.; O’Connor, K.; Dumais, A. Exploration of the dialogue components in Avatar Therapy for schizophrenia patients with refractory auditory hallucinations: A content analysis. Clin. Psychol. Psychother. 2018, 25, 878–885. [Google Scholar] [CrossRef]
- Beaudoin, M.; Potvin, S.; Machalani, A.; Dellazizzo, L.; Bourguignon, L.; Phraxayavong, K.; Dumais, A. The therapeutic processes of avatar therapy: A content analysis of the dialogue between treatment-resistant patients with schizophrenia and their avatar. Clin. Psychol. Psychother. 2021, 28, 500–518. [Google Scholar] [CrossRef]
- Morina, N.; Brinkman, W.-P.; Hartanto, D.; Kampmann, I.L.; Emmelkamp, P.M. Social interactions in virtual reality exposure therapy: A proof-of-concept pilot study. Technol. Health Care 2015, 23, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Hudon, A.; Beaudoin, M.; Phraxayavong, K.; Dellazizzo, L.; Potvin, S.; Dumais, A. Implementation of a machine learning algorithm for automated thematic annotations in avatar: A linear support vector classifier approach. Health Inform. J. 2022, 28. [Google Scholar] [CrossRef] [PubMed]
- Butler, E.A. Interpersonal Affect Dynamics: It Takes Two (and Time) to Tango. Emot. Rev. 2015, 7, 336–341. [Google Scholar] [CrossRef]
- Petrocchi, S.; Iannello, P.; Lecciso, F.; Levante, A.; Antonietti, A.; Schulz, P. Interpersonal trust in doctor-patient relation: Evidence from dyadic analysis and association with quality of dyadic communication. Soc. Sci. Med. 2019, 235, 112391. [Google Scholar] [CrossRef] [PubMed]
- Markin, R.D.; McCarthy, K.S.; Barber, J.P. Transference, countertransference, emotional expression, and session quality over the course of supportive expressive therapy: The raters’ perspective. Psychother. Res. 2013, 23, 152–168. [Google Scholar] [CrossRef] [PubMed]
- Blair, R.J.R. Traits of empathy and anger: Implications for psychopathy and other disorders associated with aggression. Philos. Trans. R. Soc. B Biol. Sci. 2018, 373, 20170155. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Green, M.F. Schizophrenic patients’ sensitivity to social cues: The role of abstraction. Am. J. Psychiatry 1993, 150, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Nikolaides, A.; Miess, S.; Auvera, I.; Müller, R.; Klosterkötter, J.; Ruhrmann, S. Restricted attention to social cues in schizophrenia patients. Eur. Arch. Psychiatry Clin. Neurosci. 2016, 266, 649–661. [Google Scholar] [CrossRef]
- Chaix, J.; Ma, E.; Nguyen, A.; Collado, M.A.O.; Rexhaj, S.; Favrod, J. Safety-seeking behaviours and verbal auditory hallucinations in schizophrenia. Psychiatry Res. 2014, 220, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Bisso, E.; Signorelli, M.; Milazzo, M.; Maglia, M.; Polosa, R.; Aguglia, E.; Caponnetto, P. Immersive Virtual Reality Applications in Schizophrenia Spectrum Therapy: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6111. [Google Scholar] [CrossRef] [PubMed]
- Rückl, S.; Gentner, N.C.; Büche, L.; Backenstrass, M.; Barthel, A.; Vedder, H.; Bürgy, M.; Kronmüller, K.T. Coping with delusions in schizophrenia and af-fective disorder with psychotic symptoms: The relationship between coping strategies and dimensions of delusion. Psychopathology 2015, 48, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Chapman, B.P.; Talbot, N.; Tatman, A.W.; Brition, P.C. Personality Traits and the Working Alliance in Psychotherapy Trainees: An Organizing Role for the Five Factor Model? J. Soc. Clin. Psychol. 2009, 28, 577–596. [Google Scholar] [CrossRef] [PubMed]
- Barber, J.; Solomonov, N. Toward a personalized approach to psychotherapy outcome and the study of therapeutic change. World Psychiatry 2019, 18, 291–292. [Google Scholar] [CrossRef] [PubMed]
| Avatar Themes | Examples |
|---|---|
| Accusations | “You are responsible for this.” |
| Omnipotence | “I am the best.” |
| Beliefs | “I believe that you are ill.’’ |
| Active listening, empathy | “There is no rush, take your time.” |
| Incitements, orders | “You should hit yourself.” |
| Coping mechanisms | “Why are you not happy when I insult you?” |
| Threats | “I will kill you.” |
| Negative emotions | “It’s difficult for me to realize that.” |
| Self-perceptions | “I see myself as worthless.” |
| Positive emotions | “I am feeling great.” |
| Provocation | “Try me.” |
| Reconciliation | “Should we stop arguing?” |
| Reinforcement | “You should do this again.” |
| Patient Themes | Examples |
|---|---|
| Approbation | “You are right” |
| Self-deprecation | “I can’t do this.” |
| Self-appraisal | “I am a nice person.” |
| Other beliefs | “You are the one controlling me” |
| Counterattack | “You are the one who did this, not me!” |
| Maliciousness of the voice | “You are trying to make this hard for everyone.” |
| Negative | “It is not easy.” |
| Negation | “I did not do this.” |
| Omnipotence | “I am everywhere.” |
| Disappearance of the voice | “Please vanish!” |
| Positive | ‘’I am feeling great.” |
| Prevention | “I will try not pay attention to you.” |
| Reconciliation of the voice | “Let’s be friends.” |
| Self-affirmation | “I can do this.” |
| Avatar Themes | Precision | Recall | f1-Score | #Interactions Tested |
|---|---|---|---|---|
| Accusations | 0.74 | 0.66 | 0.70 | 35 |
| Omnipotence | 0.77 | 0.94 | 0.85 | 18 |
| Beliefs | 0.75 | 0.69 | 0.72 | 26 |
| Active listening, empathy | 0.70 | 0.82 | 0.76 | 17 |
| Incitements, orders | 0.78 | 0.70 | 0.74 | 10 |
| Coping mechanisms | 0.96 | 0.88 | 0.92 | 25 |
| Threats | 1.00 | 0.86 | 0.92 | 7 |
| Negative emotions | 0.79 | 0.92 | 0.85 | 12 |
| Self-perceptions | 0.60 | 0.71 | 0.65 | 17 |
| Positive emotions | 0.91 | 0.62 | 0.74 | 16 |
| Provocation | 0.67 | 0.62 | 0.65 | 16 |
| Reconciliation | 0.64 | 0.69 | 0.67 | 13 |
| Reinforcement | 0.73 | 0.84 | 0.78 | 19 |
| Accuracy | 0.76 | 231 | ||
| Weighted average | 0.77 | 0.76 | 0.76 | 231 |
| Patient Themes | Precision | Recall | f1-score | #Interactions tested |
| Approbation | 0.31 | 0.31 | 0.31 | 13 |
| Self-deprecation | 0.53 | 0.67 | 0.59 | 12 |
| Self-appraisal | 0.86 | 0.59 | 0.70 | 32 |
| Other beliefs | 0.52 | 0.65 | 0.58 | 17 |
| Counterattack | 0.70 | 0.54 | 0.61 | 26 |
| Maliciousness of the voice | 0.62 | 0.71 | 0.67 | 14 |
| Negative | 0.72 | 0.64 | 0.68 | 36 |
| Negation | 0.79 | 0.73 | 0.76 | 30 |
| Omnipotence | 0.27 | 0.60 | 0.37 | 10 |
| Disappearance of the voice | 0.78 | 0.64 | 0.70 | 22 |
| Positive | 0.83 | 0.88 | 0.86 | 17 |
| Prevention | 0.86 | 0.59 | 0.70 | 32 |
| Reconciliation of the voice | 0.30 | 1.00 | 0.46 | 3 |
| Self-affirmation | 0.46 | 0.62 | 0.53 | 21 |
| Accuracy | 0.64 | 285 | ||
| Weighted average | 0.69 | 0.64 | 0.65 | 285 |
| Characteristics | Value (n = 32) |
|---|---|
| Sex (male, female) | 24.8 |
| Age (mean in years) | 42.6 ± 11.0 |
| Education (mean in years) | 13.6 ± 3.0 |
| Ethnicity (Caucasian, others) | 93.4%, 6.6% |
| % on Clozapine | 40.0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hudon, A.; Couture, J.; Dellazizzo, L.; Beaudoin, M.; Phraxayavong, K.; Potvin, S.; Dumais, A. Dyadic Interactions of Treatment-Resistant Schizophrenia Patients Having Followed Virtual Reality Therapy: A Content Analysis. J. Clin. Med. 2023, 12, 2299. https://doi.org/10.3390/jcm12062299
Hudon A, Couture J, Dellazizzo L, Beaudoin M, Phraxayavong K, Potvin S, Dumais A. Dyadic Interactions of Treatment-Resistant Schizophrenia Patients Having Followed Virtual Reality Therapy: A Content Analysis. Journal of Clinical Medicine. 2023; 12(6):2299. https://doi.org/10.3390/jcm12062299
Chicago/Turabian StyleHudon, Alexandre, Jonathan Couture, Laura Dellazizzo, Mélissa Beaudoin, Kingsada Phraxayavong, Stéphane Potvin, and Alexandre Dumais. 2023. "Dyadic Interactions of Treatment-Resistant Schizophrenia Patients Having Followed Virtual Reality Therapy: A Content Analysis" Journal of Clinical Medicine 12, no. 6: 2299. https://doi.org/10.3390/jcm12062299
APA StyleHudon, A., Couture, J., Dellazizzo, L., Beaudoin, M., Phraxayavong, K., Potvin, S., & Dumais, A. (2023). Dyadic Interactions of Treatment-Resistant Schizophrenia Patients Having Followed Virtual Reality Therapy: A Content Analysis. Journal of Clinical Medicine, 12(6), 2299. https://doi.org/10.3390/jcm12062299






