Abstract
Background: The number of joint revision arthroplasties has increased in the elderly population, which is burdened by several perioperative risks. Methods: Patients who underwent hip and knee revision arthroplasty were retrospectively included, and they were divided into two groups by age: <80 years old (Group 1) and ≥80 years old (Group 2). The primary outcome was to compare perioperative complication rates. The secondary outcome was to compare the 30-day, 90-day, and 1-year readmission rates. Results: In total, 74 patients in Group 1 and 75 patients in Group 2 were included. Postoperative anemia affected 13 patients in Group 1 (17.6%) and 25 in Group 2 (33.3%, p 0.027); blood units were transfused in 20 (26.7%) and 11 (14.9%, p 0.076) patients, respectively. In Group 1, two (2.7%) patients reported wound infection. In Group 2, eight (10.7%) patients presented hematomas, and two (2.7%) patients reported dislocations. No significant differences in the two groups were observed for 30-day (p 0.208), 90-day (p 0.273), or 1-year readmission rates (p 0.784). Conclusion: The revision arthroplasty procedure in patients over 80 years old is not associated with a higher risk of perioperative complications, or higher readmission rate compared with younger patients undergoing hip and knee revision surgery.
1. Introduction
Hip and knee arthroplasties are the most commonly performed elective orthopedic procedures in the over 65 years old population [1]. The number of geriatric patients, defined as people more than 80 years old, is going to increase. As the life expectancy of patients is increasing, more elderly patients are undergoing THA (total hip arthroplasty) and TKA (total knee arthroplasty) due to increasing incidence of osteoarthritis in this age group [2]. Recent advances in health care have enabled these patients to undergo major procedures such as TKA and THA, helping them to pursue more active lifestyles. The longer life expectancy and the higher quality of life of active patients who have undergone total joint replacement leads to the wearing out of various implants and implant failure for various reasons [3]. One of the main components that becomes overloaded and prone to wear is polyetylene; the analysis of tribology and the selection of couplings has a strategic role to improve performance and implant survival [4,5]. Consequently, as patients age and their prosthetic implants wear out, the number of revision arthroplasties in the elderly population over 80 years old performed by orthopedic surgeons will increase [1,6,7]. Advancing age is reported to be a significant risk factor in the incidence of in-hospital complications [6]. Although hip and knee revision arthroplasties in geriatric patients are burdened by a considerable risk, especially in those affected by multiple comorbidities [8,9,10,11,12], they may offer benefits in improving functional independence and the quality of life, consequently increasing patients’ life expectancy [13]. Awareness of a higher incidence of major systemic complications should alert the treating surgeon to carry out comprehensive perioperative management in this subset of patients, which could lead to better outcomes [14].
Although a few studies have already investigated perioperative complications after total hip and knee revision arthroplasty in the elderly [15,16], to the best of our knowledge, only one compared the rate of perioperative complications following aseptic revision of THA in patients aged ≥ 80 with that of those <80 [17]. Because it was based on a national database in the United States, some bias affected the study, such as different perioperative management, application of drug protocols, types of implants, and number of procedures per surgeon. Therefore, further independent cohort studies are required to confirm these findings. The primary outcome of this study was to determine perioperative local and systemic complications after hip and knee revision surgery in a population ≥ 80 years compared to those <80 years. The secondary outcome was to determine the 30-day, 90-day, and 1-year readmission rates after discharge from the hospital in the two groups.
2. Materials and Methods
2.1. Protocol
The present retrospective observational case–control study used medical file records of patients included in a registry of orthopedic surgical procedures. The study included 149 patients undergoing hip or knee revision arthroplasty by senior surgeons experienced in joint replacement surgery, from 1 February 2017 to 31 July 2020 at the Humanitas Research Hospital IRCCS, Italy. Patients were identified from hospital clinical records using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD9-CM) procedure codes (00.70, 00.71,00.72, 00.73, 00.74, 00.75, 00.76, 00.77 for revision THA and 80.06,81.55, 00.80, 00.81, 00.82, 00.83, 00.84 for revision TKA). The patients included were divided into two groups based on age at the time of surgery: < 80 years old (Group 1) and those geriatrics ≥80 years old (Group 2). Participant exclusion criteria were sequelae of periprosthetic infections, malignancy, patients under 18 years old, and less than 1 year of follow-up. Patients were matched by gender, diseased joint, preoperative diagnosis, type, and period of surgery.
Femoral stem revision was performed using uncemented monoblock splined tapered gritblasted stems (Wagner-SL stem; Zimmer, Warsaw, Indiana, US) or uncemented Arcos Modular Femoral Revision System (Zimmer Biomet Inc., Warsaw, Indiana, US) in cases of major defect in order to avoid leg length discrepancy (LLD). Acetabular revision was performed using Trabecular Metal shell (TM Modular, Trilogy TM and augment or TM Revision shell, Zimmer Biomet, Warsaw, Indiana, US); for major acetabular defect, a dual mobility cup (DMC Avantage; Zimmer Biomet, Warsaw, Indiana, US) cemented into a larger shell was used. Revision knee arthroplasty was performed using NexGen® Legacy® Constrained Condylar Knee (LCCK) with or without Trabecular Metal™ Cones augments (Zimmer Biomet, Warsaw, Indiana, US).
Data regarding patient demographic characteristics, body mass index (BMI) in kg/m2, clinical variables, American Society of Anesthesia (ASA) classification, comorbid conditions, perioperative medical complications, length of stay (LOS), use of thromboprophylaxis, and inflammatory indicators were obtained from medical file records. During hospitalization, all complications and their management were documented in the clinical file records that were analyzed for the purposes of this study. Perioperative complications that emerged from the first perioperative day to the day before discharge home or transfer to the rehabilitation department were recorded. Perioperative local complications are those occurring at the level of the surgical site, including hematomas, superficial infections, deep infections, fractures, dislocations, and contact dermatitis associated with compression stockings. Perioperative systemic complications include deep vein thrombosis, pulmonary embolism and other pulmonary complications, gastrointestinal disorders, and neurological and genitourinary complications. The occurrence of postoperative anemia was measured: the postoperative Hb (hemoglobin) values, the number of patients who underwent blood transfusions, and the number of blood units transfused were recorded. Postoperative anemia is defined by a postoperative Hb ≤ 8 g/dL on the third day after surgery or blood transfusions performed within the second postoperative day. The threshold values for transfusing were based on the PBM (Patient Blood Management) guidelines: Hb < 7 g/dL or Hb < 8 g/dL in cardiopathic or symptomatic patients (thoracic pain, orthostatic hypotension, tachycardia) [18]. The 30-day, 90-day, and 1-year readmission rates of these two groups were recorded.
2.2. Statistical Analysis
Data were described as number and percentage for categorical variables, or mean and standard deviation for continuous variables. Differences between Group 1 and Group 2 were explored with the chi-square test if categorical, with Student’s t test if continuous Gaussian distributed, or with Mann–Whitney if otherwise. Association between risk factors and early mobilization at day 0 and risk factors and postoperative anemia were explored with univariable logistic regression. All independent factors with a p value under 0.1 were then submitted to a backward multivariable logistic regression. An explorative analysis was performed for association of age groups and for systemic complications, 30-day, 90-day, and 1-year readmission rate. A p value under 0.05 was considered significant. All analyses were performed with stata15.
3. Results
3.1. Selection of Study Population
Patients were divided into two groups based on age at the time of surgery. Demographic results are reported in Table 1. A total of 312 patients were identified; 266 patients underwent revision THA, and 46 underwent revision TKA. Among 266 patients who underwent RTHA (revision total hip arthroplasty), 118 were affected by periprosthetic infections, and 20 were lost during follow-up. Therefore, only 128 patients were eligible for the study: 66 patients ≥ 80 years old, and 62 < 80 years old. Among 46 patients who underwent RTKA (revision total knee arthroplasty), 19 were periprosthetic infections, and 6 were lost during follow-up. Therefore, only 21 patients were eligible for the study: 9 patients ≥ 80 years old and 12 < 80 years old. The flow chart of the patient selection and inclusion process is shown in Figure 1.

Table 1.
Characteristics of the patient population in the two groups.
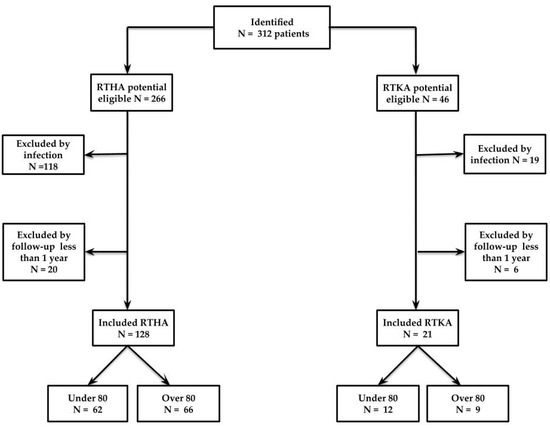
Figure 1.
Flow chart of the patient selection and inclusion process. RTHA, revision total hip arthroplasty; RTKA, revision total knee arthroplasty.
Group 1 (<80 years old) included 74 patients with a mean age of 60.5 (18–78, σ 2.3) years old: there were 34 male (45.95%) and 40 female patients (54.1%); 62 (83.8%) underwent hip revision, and 12 (16.2%) underwent knee revision arthroplasty.
Group 2 (≥80 years old) included 75 patients with a mean age of 82.5 (80–89, σ 11.9) years old: there were 34 male (45.3%) and 41 female patients (54.7%); 66 (88.0%) underwent hip revision, and 9 (12.0%) underwent knee revision arthroplasty.
3.2. Characteristics of Study Population
The two groups significantly differed for some comorbidities (Table 1): arterial hypertension (44.6% and 68.0%, respectively, in Group 1 and 2, p 0.004); cardiovascular diseases, specifically coronary artery disease and atrial fibrillation (10.8% and 29.3%, respectively, in Group 1 and 2, p 0.005); carotid artery stenosis (8.1% and 24%, respectively, in Group 1 and 2, p 0.013); and preoperative anemia (10.8% and 29.3%, respectively, in Group 1 and 2, p 0.005). The ASA (American Society of Anesthesiologists) score for Group 1 and Group 2 was I in 74.3% and 38.7%; II in 24.3% and 49.3%; and III in 1.4% and 12.0%, respectively (p < 0.001). Moreover, serum levels of iron differed significantly in the two groups (86.6 ± 32.7 vs. 73.6 ± 30.0, respectively, in Group 1 and 2, p 0.016). Group 1 mean length of stay (LOS) was 5.4 days (3–16, σ 2.5), and in Group 2, respectively, it was 5.6 days (4–16, σ 2.7), p 0.833.
Perioperative local complications (Figure 2) observed during hospitalization were postoperative anemia, need of blood transfusions, hematomas, superficial infections of surgical site, and dislocations. Postoperative anemia affected 13 patients in Group 1 (17.6%) and 25 in Group 2 (33.3%) (p 0.027). Blood units were transfused in 11 patients (14.9%) of Group 2 and 20 patients (26.7%) of Group 1, but with no significant difference (p 0.076). No hematomas were found in Group 1, but 8 patients (10.7%) presented hematomas in Group 2. Wound infection was observed in 2 patients only in Group 1 (2.7%), and 2 dislocations happened only in Group 2 (2.7%).
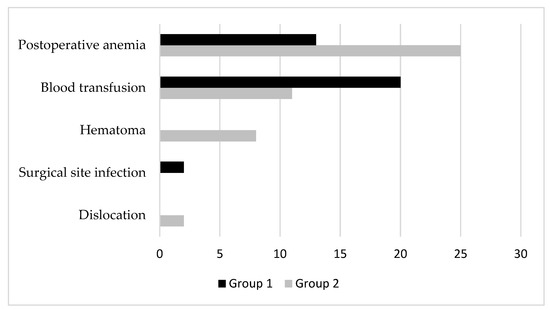
Figure 2.
Perioperative local complications in the two groups.
Perioperative systemic complications in the two groups were recorded in Group 1 and Group 2 (Figure 3): 6 patients (8.1%) and 4 patients (5.3%), respectively, were diagnosed with fever, and 2 patients (2.7%) and 5 patients (6.7%), respectively, were diagnosed with urinary tract infections. In Group 2 only 1 patient was diagnosed with a thromboembolic event (1.3%), 7 patients needed low-flow oxygen therapy (9.3%), 5 patients were diagnosed with new-onset atrial fibrillation and acute myocardial infarction (6.7%), 7 patients were diagnosed with postoperative delirium (9.3%), and only 1 patient was diagnosed with a neurological complication (1.3%).
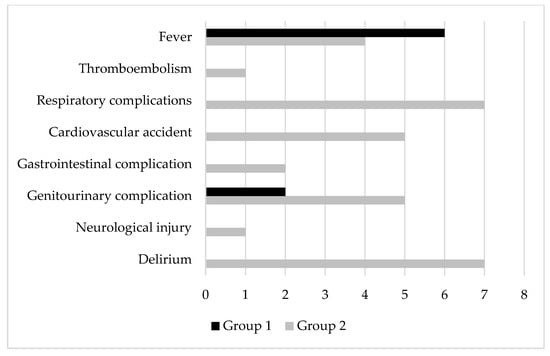
Figure 3.
Perioperative systemic complications in the two groups.
No significant differences in the two groups were observed for the hospital readmission rate at 30 days, 90 days, and 1 year (Figure 4). Readmission at 30 days occurred in 1 patient (1.4%) in Group 1 and 5 patients (6.7%) in Group 2 (p 0.208); 90-day readmission occurred in 2 patients (2.7%) in Group 1 and 6 patients (8.0%) in Group 2 (p 0.273); and 1-year readmission occurred in 8 patients (10.8%) in Group 1 and 7 patients (9.3%) in Group 2 (p 0.784).
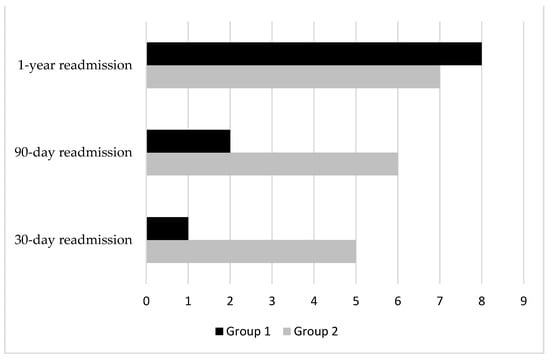
Figure 4.
30-day, 90-day, and 1-year hospital readmission rates in the two groups.
Factors significantly associated with early mobilization after surgery are summarized in Table 2. After multivariable analysis, we observed that early mobilization at day 0 was significantly associated only with preoperative anemia (OR = 5.67, 95% CI 1.63–19.77, p 0.006). The association of risk factors with postoperative anemia is shown in Table 3. After multivariable analysis, postoperative anemia results were associated with preoperative anemia (OR = 8.34, 95% CI 3.24–21.50, p < 0.001) and osteoporosis (OR = 4.10, 95% CI 1.35–12.45, p 0.013). No evidence of association was observed between blood transfusion and antiplatelet therapy (18.0% vs. 21.8% of blood transfusion in antiplatelet therapy or not, respectively, p 0.609) or anticoagulant therapy (23.1% vs. 20.6% of blood transfusion in anticoagulant therapy or not, respectively, p 0.734).

Table 2.
Univariable and multivariable logistic regression assessing risk factors for early mobilization at day 0.

Table 3.
Univariable and multivariable logistic regression assessing risk factors for postoperative anemia.
4. Discussion
The main finding of the present study was that patients ≥ 80 years old who underwent hip and knee revision arthroplasty reported a low rate of perioperative local complications compared to the younger control group. On the other hand, perioperative systemic complications were higher in the elderly population compared to younger patients. Moreover, the older age of patients was not associated with a longer length of stay in the hospital, and it was not related to a higher risk of readmission at 30 days, 90 days, and 1 year after surgery.
The higher risk of urinary tract infections identified can be a target to improve medical care quality. These infections are associated with indwelling catheters, and early removal of the catheters must be recommended. The increased risk of respiratory complications such as postoperative pneumonia in patients ≥ 80 years old compared to younger patients must be highlighted. Postoperative preventive measures such as chest physiotherapy for pneumonia and breathing exercises must be recommended to reduce pneumonia rates, especially in older patients. The high risk of cardiovascular complications in older patients should be treated with medication preoperatively and continued throughout the postoperative period. This study identified risk factors significantly correlated to early mobilization and verticalization: preoperative anemia was the only factor significantly associated with time of verticalization the day of surgery. Patients who suffered from preoperative anemia were treated with iron supplementation (infusion or oral therapy) to increase their iron deposits before surgeries procedures, resulting in an even better postoperative iron profile than nonanemic patients. Unfortunately, this was not supported by laboratory data since not all patients who underwent iron supplementation had repeated preoperative blood tests. Furthermore, multivariable analysis assessing significant associations between risk factors and postoperative anemia identified preoperative anemia as a significant risk factor for postoperative anemia. RTHA and RTKA were safe for patients ≥ 80 years old in our high-volume single center, where all surgeries were performed by senior surgeons experienced in joint replacement surgery. Furthermore, the co-management between the surgeon and the hospitalist, a doctor in the field of internal medicine, during the patient’s hospitalization potentially reduced complications, improving medical care [14,19,20,21,22,23].
The majority of previous studies in the geriatric population, especially case–control studies, were conducted on primary hip and knee arthroplasty and very few on total hip and knee revision arthroplasty. Bovonratwet et al., contrary to our results, reported greater risks in patients aged ≥ 80 years compared with younger patients after aseptic RTHA and highlighted the need for medical optimization in these vulnerable patients [17]. Dugdale et al. found, contrary to our results, that nonagenarian patients had longer length of stay (LOS), higher total charges, and were more likely to develop several more major complications than octogenarians following both PTHA (primary total hip arthroplasty) or RTHA [15]. Birdsall et al. reported a mortality rate of 5% after a knee revision arthroplasty of 119 patients aged ≥ 80 years old [24]. Smith et al. compared perioperative complications after PTKA (primary total knee arthroplasty) and RTKA between octogenarians and nonagenarians. The investigators observed a higher risk of perioperative complications, such as postoperative anemia and need of blood transfusions, in the older patient group [25]. Jauregui et al. have demonstrated the cost–benefit ratio of both primary and revision arthroplasty for the geriatric population: on one hand, octogenarians had a higher risk of perioperative complications which prolong hospital stay and sanitary costs; on the other hand, a good functional outcome and pain control emerged regardless of age [26]. The investigators observed a significantly higher rate of hospital readmission for all causes in the elderly population [15,27,28,29,30,31,32], especially dislocations, which occur in up to 20% of older patients [33,34,35]. Parvizi et al. have demonstrated that preexisting cardiovascular diseases represent a risk factor for intraoperative mortality in over 80 years old patients and a 30-day mortality rate of 0.29% in all age groups [36,37]. Birdsall et al. reported a 1-year mortality rate of 5% in octogenarians [24]. Respiratory and urinary tract infections and delirium are more statistically significant in the older population [38]. Smith et al. compared one group of nonagenarians with one group of octogenarians who underwent either primary or revision arthroplasty: the older group reported a higher risk of needed blood transfusion, urinary tract infection, and acute kidney injury than the younger group [25]. Increases in life expectancy and implant failures have resulted in more elderly patients requiring revision THA and TKA [39,40]. Revision surgery has been projected to increase by 137% between 2005 and 2030 [2]. Previous studies have shown revision arthroplasty to be effective in reducing pain and in increasing function and quality of life in elderly patients.
Wear is the main reason for hip and knee revision arthroplasty [41,42]. Reducing wear is a strategic step in minimizing harmful failures for users. Metal-on-metal bearings also carry the danger of poisoning due to metallosis. The main drawback of this type of bearing is that worn metal particles can spread through the lymphatic system to locations far from the implant, and it has been reported that the metals can accumulate in the liver, spleen, lymph nodes, and bone marrow. Along with the reactive nature of worn metal particles, they have the potential to create local inflammation, contributing to the emergence of osteolysis, or cause cytotoxicity, hypersensitivity, and neoplasia [43,44]. Jamari et al. reported that dimples can reduce contact pressure and wear, indicating that in real use they could reduce failure due to wear and poisoning due to metallosis. The bottom profile dimple ball type is estimated to produce the lowest wear compared to other models; this model demonstrated a promising surface textured parameter and could be used to design the bearing components in a total hip arthroplasty [45].
This study has several limitations. First, it is a retrospective observational study; as with any database, the quality of data and missing data may introduce errors. Second, the study was performed in a high-volume single center with a high level of expertise in elective prosthetic surgery whose results cannot be generalized. Third, the preoperative schedule selection bias selected very healthy patients or patients with stable chronic diseases; therefore, the conclusion of the study may be applicable only to patients with low comorbidities. The main strength of this study is the large number of patients enrolled. Second, it is the only retrospective study that has evaluated perioperative complications and readmission rates after hip and knee revision surgery in patients ≥ 80 years old compared to patients < 80 years old in a high-volume single center. Further research would be necessary to determine the clinical relevance of the higher perioperative systemic complications found in nonagenarian and octogenarian patients, highlighting the need of medical optimization and post-discharge planning following total hip and knee revision arthroplasty.
5. Conclusions
In conclusion, 80-year-old patients are not associated with a higher risk of perioperative complications or readmission rate compared with younger patients undergoing hip and knee revision surgery. Therefore, age could not be considered an absolute contraindication to revision arthroplasty procedures.
Author Contributions
Conceptualization, G.G., M.D.P. and M.L.; methodology, F.L.C. and M.L.; software, F.L.C. and E.M.; validation, M.L.; formal analysis, M.D.P. and E.M.; investigation, V.D.M. and F.L.C.; resources, V.D.M.; data curation, M.D.P., E.M., F.L.C. and G.G.; writing—original draft preparation, V.D.M.; writing—review and editing, V.D.M.; visualization, V.D.M., F.L.C. and M.L.; supervision, F.L.C. and M.L.; project administration, G.G. and M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and good clinical practice guidelines. The study protocol for the development of this registry was approved by Ethics Committee of Humanitas Research Hospital (protocol code 618/17).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study: all individual participants signed a written informed consent before the surgical procedure and a written informed consent to be included in the registry of orthopedic surgical procedures.
Data Availability Statement
The data supporting reported results can be found in a repository (Zenodo).
Acknowledgments
The Livio Sciutto Foundation for Medical Research is gratefully acknowledged. This is a nonprofit social organization that recorded in its database the demographic and surgical data of the patients included in the study, with the previous consent of the patients and respecting the current law on the privacy. Finally, all the patients who participated in the study, together with physicians and nurses of the Humanitas Clinical Laboratory, are gratefully acknowledged.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Inacio, M.C.S.; Graves, S.E.; Pratt, N.L.; Roughead, E.E.; Nemes, S. Increase in Total Joint Arthroplasty Projected from 2014 to 2046 in Australia: A Conservative Local Model with International Implications. Clin. Orthop. Relat. Res. 2017, 475, 2130–2137. [Google Scholar] [CrossRef]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J. Bone Joint Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Ammarullah, M.I.; Afif, I.Y.; Maula, M.I.; Winarni, T.I.; Tauviqirrahman, M.; Bayuseno, A.P.; Basri, H.; Syahrom, A.; Saad, A.P.M. Jamari Deformation Analysis of CoCrMo-on-CoCrMo Hip Implant Based on Body Mass Index Using 2D Finite Element Procedure. J. Phys. Conf. Ser. 2022, 2279, 012004. [Google Scholar] [CrossRef]
- Ozer, A. Computational Wear of Knee Implant Polyethylene Insert Surface under Continuous Dynamic Loading and Posterior Tibial Slope Variation Based on Cadaver Experiments with Comparative Verification. BMC Musculoskelet. Disord. 2022, 23, 871. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Wibowo, D.B.; Kurdi, O.; Tauviqirrahman, M.; Jamari, J. Minimizing Risk of Failure from Ceramic-on-Ceramic Total Hip Prosthesis by Selecting Ceramic Materials Based on Tresca Stress. Sustainability 2022, 14, 13413. [Google Scholar] [CrossRef]
- Parvizi, J.; Mui, A.; Purtill, J.J.; Sharkey, P.F.; Hozack, W.J.; Rothman, R.H. Total Joint Arthroplasty: When Do Fatal or near-Fatal Complications Occur? J. Bone Joint Surg. Am. 2007, 89, 27–32. [Google Scholar] [CrossRef]
- Inacio, M.C.S.; Paxton, E.W.; Graves, S.E.; Namba, R.S.; Nemes, S. Projected Increase in Total Knee Arthroplasty in the United States—An Alternative Projection Model. Osteoarthr. Cartil. 2017, 25, 1797–1803. [Google Scholar] [CrossRef]
- Gaiani, L.; Bertelli, R.; Palmonari, M.; Vicenzi, G. Total Hip Arthroplasty Revision in Elderly People with Cement and Burch-Schneider Anti-Protrusio Cage. Musculoskelet. Surg. 2009, 93, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Bozic, K.J.; Kurtz, S.M.; Lau, E.; Ong, K.; Vail, T.P.; Berry, D.J. The Epidemiology of Revision Total Hip Arthroplasty in the United States. JBJS 2009, 91, 128–133. [Google Scholar] [CrossRef]
- Gasbarra, E.; Perrone, F.L.; Celi, M.; Rao, C.; Feola, M.; Cuozzo, N.; Tarantino, U. Total Hip Arthroplasty Revision in Elderly Patients. Aging Clin. Exp. Res. 2013, 25, 61–63. [Google Scholar] [CrossRef]
- Koroukian, S.M.; Warner, D.F.; Owusu, C.; Given, C.W. Multimorbidity Redefined: Prospective Health Outcomes and the Cumulative Effect of Co-Occurring Conditions. Prev. Chronic Dis. 2015, 12, E55. [Google Scholar] [CrossRef] [PubMed]
- Koroukian, S.M.; Schiltz, N.K.; Warner, D.F.; Klika, A.K.; Higuera-Rueda, C.A.; Barsoum, W.K. Older Adults Undergoing Total Hip or Knee Arthroplasty: Chronicling Changes in Their Multimorbidity Profile in the Last Two Decades. J. Arthroplast. 2018, 33, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Strehle, J.; Del Notaro, C.; Orler, R.; Isler, B. The Outcome of Revision Hip Arthroplasty in Patients Older than Age 80 Years: Complications and Social Outcome of Different Risk Groups. J. Arthroplast. 2000, 15, 690–697. [Google Scholar] [CrossRef]
- Wachter, R.M.; Goldman, L. The Emerging Role of “Hospitalists” in the American Health Care System. N. Engl. J. Med. 1996, 335, 514–517. [Google Scholar] [CrossRef]
- Dugdale, E.M.; Tybor, D.; Kain, M.; Smith, E.L. Comparing Inpatient Complication Rates between Octogenarians and Nonagenarians Following Primary and Revision Total Hip Arthroplasty in a Nationally Representative Sample 2010–2014. Geriatrics 2019, 4, 55. [Google Scholar] [CrossRef] [PubMed]
- Trigueros-Larrea, J.M.; Gonzalez-Bedia, M.A.; Lomo-Garrote, J.M.; Martin-de la Cal, O.; Martin-Ferrero, M.A. Total Knee Arthroplasty in Octogenarians: Should We Still Be so Restrictive? Geriatrics 2021, 6, 67. [Google Scholar] [CrossRef] [PubMed]
- Bovonratwet, P.; Malpani, R.; Ottesen, T.D.; Tyagi, V.; Ondeck, N.T.; Rubin, L.E.; Grauer, J.N. Aseptic Revision Total Hip Arthroplasty in the Elderly: Quantifying the Risks for Patients over 80 Years Old. Bone Jt. J. 2018, 100-B, 143–151. [Google Scholar] [CrossRef]
- Carson, J.L.; Carless, P.A.; Hebert, P.C. Transfusion Thresholds and Other Strategies for Guiding Allogeneic Red Blood Cell Transfusion. Cochrane Database Syst. Rev. 2012, 4, CD002042. [Google Scholar] [CrossRef]
- Phy, M.P.; Vanness, D.J.; Melton, L.J.; Long, K.H.; Schleck, C.D.; Larson, D.R.; Huddleston, P.M.; Huddleston, J.M. Effects of a Hospitalist Model on Elderly Patients with Hip Fracture. Arch. Intern. Med. 2005, 165, 796–801. [Google Scholar] [CrossRef]
- Adesanya, A.O.; Joshi, G.P. Hospitalists and Anesthesiologists as Perioperative Physicians: Are Their Roles Complementary? Bayl. Univ. Med. Cent. Proc. 2007, 20, 140–142. [Google Scholar] [CrossRef]
- Sharma, G.; Kuo, Y.-F.; Freeman, J.; Zhang, D.D.; Goodwin, J.S. Comanagement of Hospitalized Surgical Patients by Medicine Physicians in the United States. Arch. Intern. Med. 2010, 170, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.M.; Mendelson, D.A.; Bingham, K.W.; Kates, S.L. Impact of a Comanaged Geriatric Fracture Center on Short-Term Hip Fracture Outcomes. Arch. Intern. Med. 2009, 169, 1712–1717. [Google Scholar] [CrossRef]
- Zuckerman, J.D.; Sakales, S.R.; Fabian, D.R.; Frankel, V.H. Hip Fractures in Geriatric Patients. Results of an Interdisciplinary Hospital Care Program. Clin. Orthop. Relat. Res. 1992, 274, 213–225. [Google Scholar] [CrossRef]
- Birdsall, P.D.; Hayes, J.H.; Cleary, R.; Pinder, I.M.; Moran, C.G.; Sher, J.L. Health Outcome after Total Knee Replacement in the Very Elderly. J. Bone Joint Surg. Br. 1999, 81, 660–662. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.L.; Dugdale, E.M.; Tybor, D.; Kain, M. Comparing Inpatient Complication Rates between Octogenarians and Nonagenarians Following Primary and Revision Total Knee Arthroplasty in a Nationally Representative Sample, 2010–2014. Geriatrics 2018, 4, 3. [Google Scholar] [CrossRef] [PubMed]
- Jauregui, J.J.; Boylan, M.R.; Kapadia, B.H.; Naziri, Q.; Maheshwari, A.V.; Mont, M.A. Total Joint Arthroplasty in Nonagenarians: What Are the Risks? J. Arthroplast. 2015, 30, 2102–2105.e1. [Google Scholar] [CrossRef]
- Kuperman, E.F.; Schweizer, M.; Joy, P.; Gu, X.; Fang, M.M. The Effects of Advanced Age on Primary Total Knee Arthroplasty: A Meta-Analysis and Systematic Review. BMC Geriatr. 2016, 16, 41. [Google Scholar] [CrossRef]
- Malkani, A.L.; Dilworth, B.; Ong, K.; Baykal, D.; Lau, E.; Mackin, T.N.; Lee, G.-C. High Risk of Readmission in Octogenarians Undergoing Primary Hip Arthroplasty. Clin. Orthop. Relat. Res. 2017, 475, 2878–2888. [Google Scholar] [CrossRef]
- Murphy, B.P.D.; Dowsey, M.M.; Choong, P.F.M. The Impact of Advanced Age on the Outcomes of Primary Total Hip and Knee Arthroplasty for Osteoarthritis: A Systematic Review. JBJS Rev. 2018, 6, e6. [Google Scholar] [CrossRef] [PubMed]
- Murphy, B.P.D.; Dowsey, M.M.; Spelman, T.; Choong, P.F.M. The Impact of Older Age on Patient Outcomes Following Primary Total Knee Arthroplasty. Bone Joint J. 2018, 100-B, 1463–1470. [Google Scholar] [CrossRef]
- Nanjayan, S.K.; Swamy, G.N.; Yellu, S.; Yallappa, S.; Abuzakuk, T.; Straw, R. In-Hospital Complications Following Primary Total Hip and Knee Arthroplasty in Octogenarian and Nonagenarian Patients. J. Orthop. Traumatol. 2014, 15, 29–33. [Google Scholar] [CrossRef]
- Pepper, A.M.; Novikov, D.; Cizmic, Z.; Barrett, J.T.; Collins, M.; Iorio, R.; Schwarzkopf, R.; Long, W.J. Age and Frailty Influence Hip and Knee Arthroplasty Reimbursement in a Bundled Payment Care Improvement Initiative. J. Arthroplast. 2019, 34, S80–S83. [Google Scholar] [CrossRef] [PubMed]
- Pagnano, M.W.; McLamb, L.A.; Trousdale, R.T. Primary and Revision Total Hip Arthroplasty for Patients 90 Years of Age and Older. Mayo Clin. Proc. 2003, 78, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Radcliffe, G.S.; Tomichan, M.C.; Andrews, M.; Stone, M.H. Revision Hip Surgery in the Elderly: Is It Worthwhile? J. Arthroplast. 1999, 14, 38–44. [Google Scholar] [CrossRef]
- Raut, V.V.; Wroblewski, B.M.; Siney, P.D. Revision Hip Arthroplasty. Can the Octogenarian Take It? J. Arthroplast. 1993, 8, 401–403. [Google Scholar] [CrossRef]
- Parvizi, J.; Holiday, A.D.; Ereth, M.H.; Lewallen, D.G. The Frank Stinchfield Award. Sudden Death during Primary Hip Arthroplasty. Clin. Orthop. Relat. Res. 1999, 369, 39–48. [Google Scholar] [CrossRef]
- Parvizi, J.; Johnson, B.G.; Rowland, C.; Ereth, M.H.; Lewallen, D.G. Thirty-Day Mortality after Elective Total Hip Arthroplasty. J. Bone Joint Surg. Am. 2001, 83, 1524–1528. [Google Scholar] [CrossRef]
- Kreder, H.J.; Berry, G.K.; McMurtry, I.A.; Halman, S.I. Arthroplasty in the Octogenarian: Quantifying the Risks. J. Arthroplast. 2005, 20, 289–293. [Google Scholar] [CrossRef]
- Malak, T.T.; Broomfield, J.a.J.; Palmer, A.J.R.; Hopewell, S.; Carr, A.; Brown, C.; Prieto-Alhambra, D.; Glyn-Jones, S. Surrogate Markers of Long-Term Outcome in Primary Total Hip Arthroplasty: A Systematic Review. Bone Joint Res. 2016, 5, 206–214. [Google Scholar] [CrossRef]
- Matharu, G.S.; Nandra, R.S.; Berryman, F.; Judge, A.; Pynsent, P.B.; Dunlop, D.J. Risk Factors for Failure of the 36 Mm Metal-on-Metal Pinnacle Total Hip Arthroplasty System: A Retrospective Single-Centre Cohort Study. Bone Joint J. 2017, 99-B, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Shankar, S.; Nithyaprakash, R.; Sugunesh, P.; Uddin, M.; Pramanik, A. Contact Stress and Wear Analysis of Zirconia Against Alumina for Normal and Physically Demanding Loads in Hip Prosthesis. J. Bionic Eng. 2020, 17, 1045–1058. [Google Scholar] [CrossRef]
- Nithyaprakash, R.; Shankar, S.; Uddin, M.S. Computational Wear Assessment of Hard on Hard Hip Implants Subject to Physically Demanding Tasks. Med. Biol. Eng. Comput. 2018, 56, 899–910. [Google Scholar] [CrossRef]
- Basri, H.; Syahrom, A.; Prakoso, A.T.; Wicaksono, D.; Amarullah, M.I.; Ramadhoni, T.S.; Nugraha, R.D. The Analysis of Dimple Geometry on Artificial Hip Joint to the Performance of Lubrication. J. Phys. Conf. Ser. 2019, 1198, 042012. [Google Scholar] [CrossRef]
- Gao, L.; Dowson, D.; Hewson, R.W. Predictive Wear Modeling of the Articulating Metal-on-Metal Hip Replacements. J. Biomed. Mater. Res. B Appl. Biomater. 2017, 105, 497–506. [Google Scholar] [CrossRef]
- Jamari, J.; Ammarullah, M.I.; Saad, A.P.M.; Syahrom, A.; Uddin, M.; Van der Heide, E.; Basri, H. The Effect of Bottom Profile Dimples on the Femoral Head on Wear in Metal-on-Metal Total Hip Arthroplasty. JFB 2021, 12, 38. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).