A Novel Device for Assessment and Treatment of Upper Cervical Spine: Test–Retest Reliability Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.1.1. Part 1: Device Specifications and Calibration
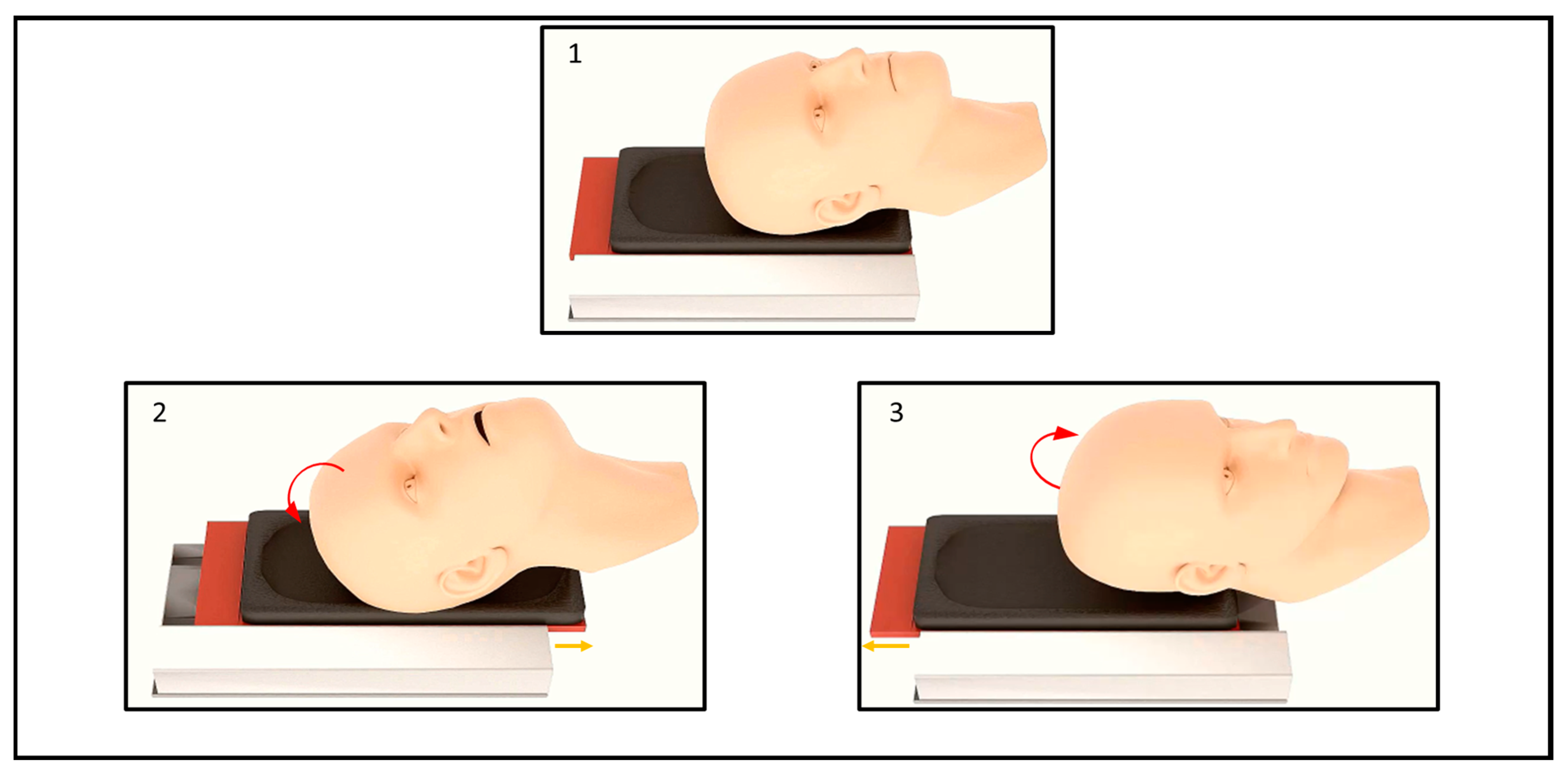
Description of the Technical System
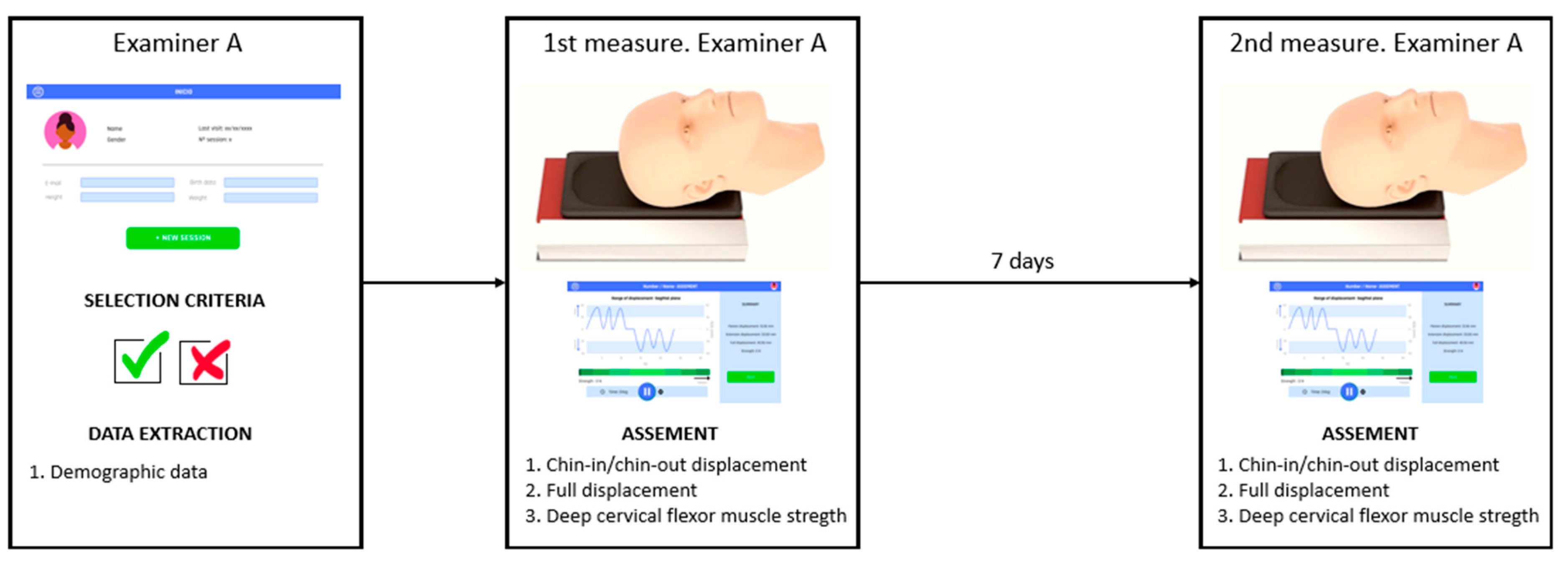
2.1.2. Part 2: Test–Retest Reliability Study
Sample and Selection
Instrumentation and Measures
Testing Procedure
Data Analysis
3. Results
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Safiri, S.; Kolahi, A.A.; Hoy, D.; Buchbinder, R.; Mansournia, M.A.; Bettampadi, D.; Ashrafi-Asgarabad, A.; Almasi-Hashiani, A.; Almasi-Hashiani, A.; Sepidarkish, M.; et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: Systematic analysis of the Global Burden of Disease Study 2017. BMJ 2020, 368, m791. [Google Scholar] [CrossRef] [PubMed]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K. Neck Pain: Revision 2017. J. Orthop. Sport. Phys. Ther. Mov. Sci. Media 2017, 47, A1–A83. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin. Proc. 2015, 90, 284–299. [Google Scholar] [CrossRef]
- Rushton, A.; Carlesso, L.C.; Flynn, T.; Hing, W.A.; Rubinstein, R.; Vogel, S.M.; Kerry, R. International Framework for Examination of the Cervical Region for potential of vascular pathologies of the neck prior to Orthopaedic Manual Therapy (OMT) Intervention: International IFOMPT Cervical Framework. J. Orthop. Sport. Phys. Ther. 2023, 53, 7–22. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Uribarren, A.; Rodriguez-Sanz, J.; López-de-Celis, C.; Pérez-Guillen, S.; Tricás-Moreno, J.M.; Cabanillas-Barea, S. Short-term effects of the traction-manipulation protocol in dizziness intensity and disability in cervicogenic dizziness: A randomized controlled trial. Disabil. Rehabil. 2021, 44, 3601–3609. [Google Scholar] [CrossRef]
- González-Rueda, V.; López-de-Celis, C.; Bueno-Gracia, E.; Rodríguez-Sanz, J.; Pérez-Bellmunt, A.; Barra-López, M.E.; Hidalgo García, C. Short- and mid-term effects of adding upper cervical manual therapy to a conventional physical therapy program in patients with chronic mechanical neck pain. Randomized controlled clinical trial. Clin. Rehabil. 2020, 35, 0269215520965054. [Google Scholar] [CrossRef] [PubMed]
- Ernst, M.J.; Crawford, R.J.; Schelldorfer, S.; Rausch-Osthoff, A.K.; Barbero, M.; Kool, J.; Bauer, C.M. Extension and flexion in the upper cervical spine in neck pain patients. Man. Ther. 2015, 20, 547–552. [Google Scholar] [CrossRef]
- Dhimitri, K.; Brodeur, S.; Croteau, M.; Richard, S.; Seymour, C.J. Reliability of the Cervical Range of Motion Device in Measuring Upper Cervical Motion. J. Man. Manip. Ther. 2013, 6, 31–36. [Google Scholar] [CrossRef]
- Pérez-Fernández, T.; Armijo-Olivo, S.; Liébana, S.; Ortíz, P.J.D.L.T.; Fernández-Carnero, J.; Raya, R.; Martín-Pintado-Zugasti, A. A novel use of inertial sensors to measure the craniocervical flexion range of motion associated to the craniocervical flexion test: An observational study. J. Neuroeng. Rehabil. 2020, 17, 152. [Google Scholar] [CrossRef]
- Falla, D.L.; Campbell, C.D.; Fagan, A.E.; Thompson, D.C.; Jull, G.A. Relationship between cranio-cervical flexion range of motion and pressure change during the cranio-cervical flexion test. Man. Ther. 2003, 8, 92–96. [Google Scholar] [CrossRef]
- Falla, D.; Jull, G.; Dalvalba, P.; Rainoldi, A.; Merletti, R. An Electromyographic Analysis of the Deep Cervical Flexor Muscles in Performance of Craniocervical Flexion. Phys. Ther. 2003, 83, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Mayoux-Benhamou, M.A.; Revel, M.; Vallée, C.; Roudier, R.; Barbet, J.P.; Bargy, F. Longus colli has a postural function on cervical curvature. Surg. Radiol. Anat. 1994, 16, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Jull, G.A.; O’Leary, S.P.; Falla, D.L. Clinical Assessment of the Deep Cervical Flexor Muscles: The Craniocervical Flexion Test. J. Manip. Physiol. Ther. 2008, 31, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Jull, G.; Barrett, C.; Magee, R.; Ho, P. Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia 1999, 19, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Patijn, J. Reproducibility protocol for diagnostic procedures in Manual/Musculoskeletal Medicine: Edition 2019. Man. Medizin. 2019, 57, 451–479. [Google Scholar] [CrossRef]
- O’Leary, S.; Falla, D.; Jull, G. The relationship between superficial muscle activity during the cranio-cervical flexion test and clinical features in patients with chronic neck pain. Man. Ther. 2011, 16, 452–455. [Google Scholar] [CrossRef]
- O’Leary, S.; Falla, D.; Jull, G.; Vicenzino, B. Muscle specificity in tests of cervical flexor muscle performance. J. Electromyogr. Kinesiol. 2007, 17, 35–40. [Google Scholar] [CrossRef]
- Falla, D.; Jull, G.; O’Leary, S.; Dall’Alba, P. Further evaluation of an EMG technique for assessment of the deep cervical flexor muscles. J. Electromyogr. Kinesiol. 2006, 16, 621–628. [Google Scholar] [CrossRef]
- Amiri, M.; Jull, G.; Bullock-Saxton, J. Measurement of Upper Cervical Flexion and Extension with the 3-Space Fastrak Measurement System: A Repeatability Study. J. Man. Manip. Ther. 2003, 11, 198–203. [Google Scholar] [CrossRef]
- Jørgensen, R.; Ris, I.; Falla, D.; Juul-Kristensen, B. Reliability, construct and discriminative validity of clinical testing in subjects with and without chronic neck pain. BMC Musculoskelet. Disord. 2014, 15, 408. [Google Scholar] [CrossRef]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Davis, F.A., Ed.; Prentice Hall: Hoboken, NJ, USA, 2009. [Google Scholar]
- Villanueva-Ruiz, I.; Falla, D.; Lascurain-Aguirrebeña, I. Effectiveness of Specific Neck Exercise for Nonspecific Neck Pain; Usefulness of Strategies for Patient Selection and Tailored Exercise-A Systematic Review with Meta-Analysis. Phys. Ther. 2022, 102, pzab259. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, S.; Vicenzino, B.; Jull, G. A new method of isometric dynamometry for the craniocervical flexor muscles. Phys. Ther. 2005, 85, 556–564. [Google Scholar] [CrossRef] [PubMed]

| 1st Measure Mean ± SD | 2nd Measure Mean ± SD | |
|---|---|---|
| Strength DCF muscle (N) | 21.18 ± 3.15 | 20.78 ± 3.23 |
| Chin-in displacement (mm) | 12.79 ± 3.46 | 13.04 ± 2.56 |
| Chin-out displacement (mm) | 35.99 ± 4.44 | 35.19 ± 3.92 |
| Full displacement (mm) | 48.79 ± 5.99 | 47.23 ± 7.12 |
| Test—Retest Reliability | ICC (95%) |
|---|---|
| Strength DCF muscles (N) | 0.98 (0.91–0.99) |
| Chin-in displacement (mm) | 0.92 (0.63–0.98) |
| Chin-out displacement (mm) | 0.89 (0.58–0.97) |
| Full displacement (mm) | 0.86 (0.43–0.96) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carrasco-Uribarren, A.; Marimon, X.; Portela, A.; Cabanillas-Barea, S.; Rodríguez-Rubio, P.R.; Pérez, R.A. A Novel Device for Assessment and Treatment of Upper Cervical Spine: Test–Retest Reliability Study. J. Clin. Med. 2023, 12, 1954. https://doi.org/10.3390/jcm12051954
Carrasco-Uribarren A, Marimon X, Portela A, Cabanillas-Barea S, Rodríguez-Rubio PR, Pérez RA. A Novel Device for Assessment and Treatment of Upper Cervical Spine: Test–Retest Reliability Study. Journal of Clinical Medicine. 2023; 12(5):1954. https://doi.org/10.3390/jcm12051954
Chicago/Turabian StyleCarrasco-Uribarren, Andoni, Xavier Marimon, Alejandro Portela, Sara Cabanillas-Barea, Pere Ramón Rodríguez-Rubio, and Román A. Pérez. 2023. "A Novel Device for Assessment and Treatment of Upper Cervical Spine: Test–Retest Reliability Study" Journal of Clinical Medicine 12, no. 5: 1954. https://doi.org/10.3390/jcm12051954
APA StyleCarrasco-Uribarren, A., Marimon, X., Portela, A., Cabanillas-Barea, S., Rodríguez-Rubio, P. R., & Pérez, R. A. (2023). A Novel Device for Assessment and Treatment of Upper Cervical Spine: Test–Retest Reliability Study. Journal of Clinical Medicine, 12(5), 1954. https://doi.org/10.3390/jcm12051954










