Complementary Therapy Learning in the Setting of Lung Transplantation: A Single-Center Observational Study of Appropriation and Efficacy
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Approval
2.2. Study Design, and Setting
2.3. Patient Population
2.4. Study Protocol—Techniques
2.5. Study Protocol—Anesthesia, Surgery, and Postoperative Analgesia
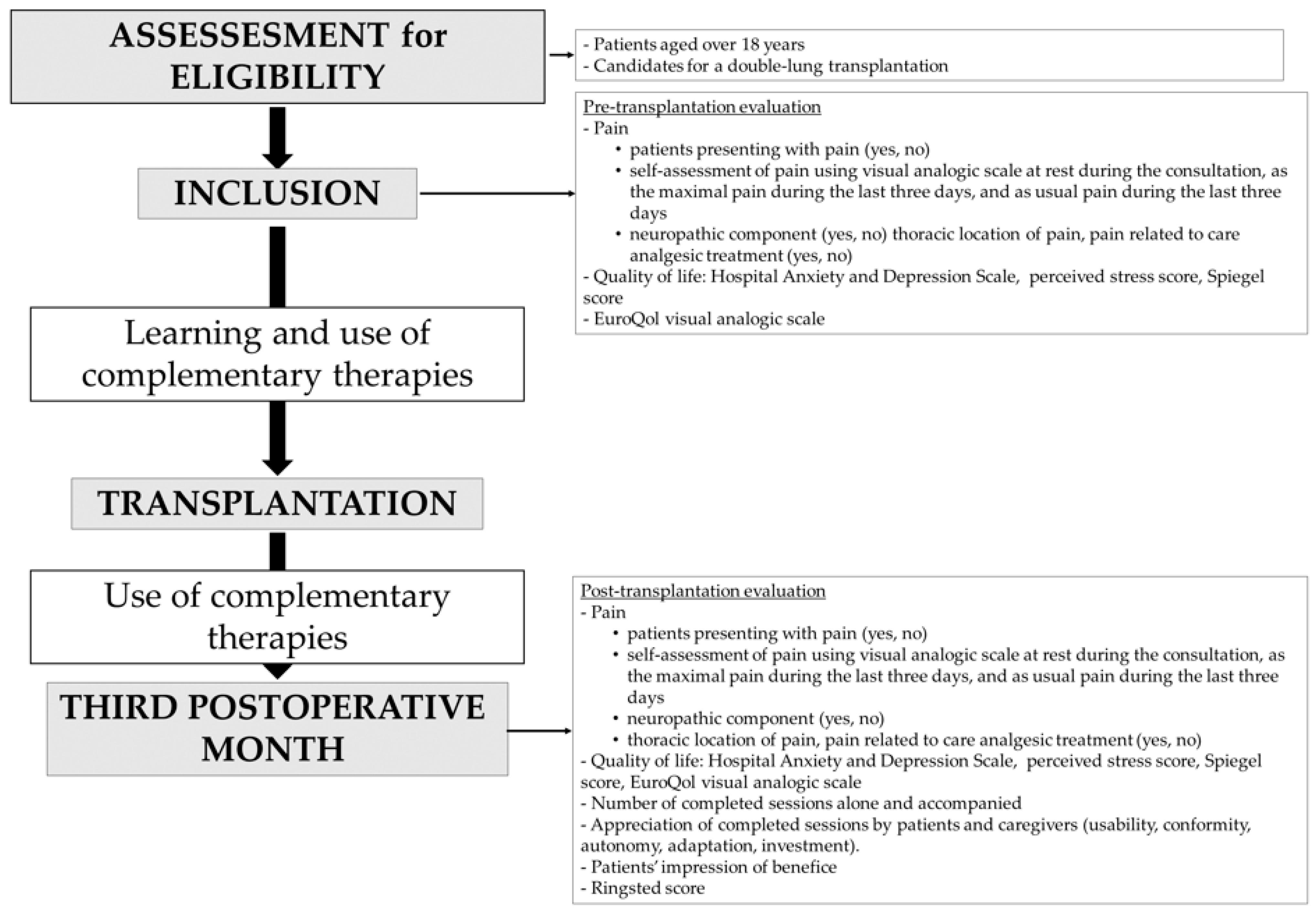
2.6. Data Collection (Figure 1)
- Pain was assessed by (i) the answer to the question “do you think you regularly suffer from pain?”; (ii) self-assessment using a visual analogue scale between 0 (no pain) and 100 (worst pain imaginable) at rest during the consultation, as the maximum pain intensity during the last three days, and as usual pain during the last three days; (iii) the response to the DN4 questionnaire (neuropathic nature of pain) [18]. Thoracic location of pain and its relation to care was noted. Analgesic treatment, including treatment of neuropathic pain, non-medicinal treatment, and benzodiazepine, was specified.
- Anxiety and depression were assessed with the French version of the Hospital Anxiety and Depression Scale (HADS); 14 items rated from 0 to 3, seven questions related to anxiety and seven others to depression; maximum of each score = 21. An anxiety score or a depression score above 7 on this 14-item scale was considered as indicative of a clinical diagnosis of anxiety or depression [19].
- Perceived stress was evaluated with the perceived stress score (ten items rated from 0 to 5; total score < 21 = someone who knows how to manage stress; Total score between 21 and 26 = someone who usually knows how to manage stress, except in certain situations; total score > 27 = someone who does not know how to manage stress) [20].
- Sleep quality was assessed by the Spiegel sleep score (six items rated from 0 to 5: the lower the score, the more serious the sleep disorder [21].
- Quality of life was assessed by the EuroQol visual analog scale (EQ-VAS) which records the respondent’s self-rated health on a vertical scale graduated from 0 to 100 between the two extremes “the best health you can imagine” and “the worst health you can imagine” [22].
- The number of sessions of complementary techniques before and after transplantation was recorded and separated into sessions by the patient, completed by the patient alone or with a therapist (training sessions).
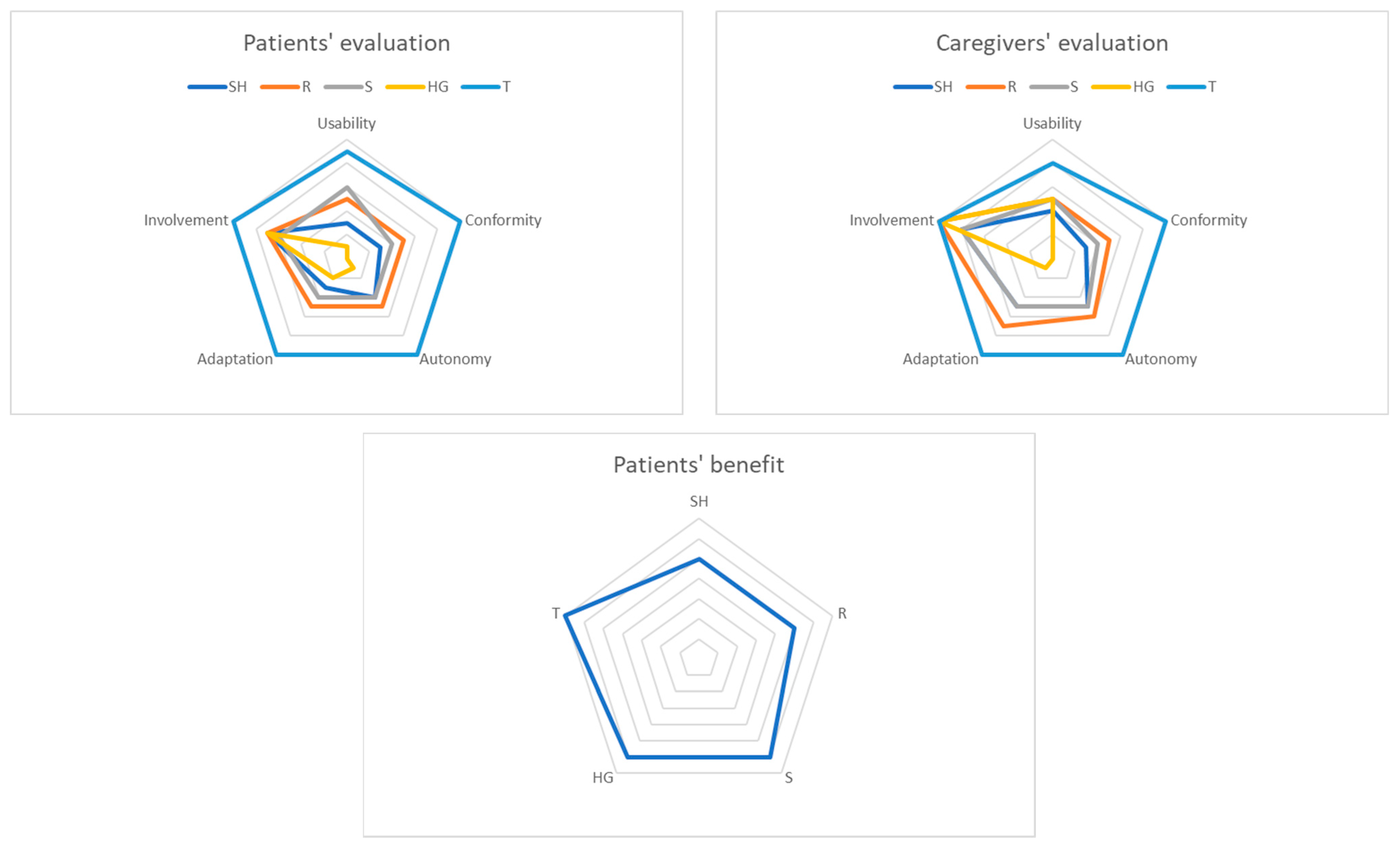
- Patients’ appropriation of the techniques was evaluated by the patients and caregivers using a specific questionnaire. The qualities of the techniques, the patients’ implication and degree of satisfaction were measured by an 11-point numerical rating scale with 0 being “worst possible” and 10 “excellent” on five features (usability, conformity, autonomy, adaptation, and involvement). Patients evaluated their impression of benefit using the same scale.
- Pain-related impairment of daily activities after thoracic surgery was assessed with a specific questionnaire [23] using its French translation [24]. Using this questionnaire, patients scored their pain impairment for each activity from 0 (“no pain or activity never performed”) to 1 (“pain impairs me a little to perform this activity”), 2 (“pain somewhat impairs me”), 3 (“pain impairs me a lot”) or 4 (“pain prevents me from performing this activity”). Activities are separated into daily or routine activities (getting out of bed for example) and chosen or task activities (swimming or carrying heavy bags for example).
2.7. Primary and Secondary Outcomes
2.8. Sample Size Calculation
2.9. Statistical Analyses
3. Results
3.1. Patients’ Characteristics at Inclusion
3.2. Performed Sessions
3.3. Patients’ and Caregivers’ Assessments of the Techniques
3.4. Patients’ Characteristics Three Months after Transplantation
3.5. Relation between the Number of Performed Sessions and Indices of Quality of Life
4. Discussion
Weaknesses and Strengths of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jastrzebski, D.; Kozielski, J.; Banas, A.; Cebula, T.; Gumola, A.; Ziora, D.; Krzywiecki, A. Quality of life during one-year observation of patients with idiopathic pulmonary fibrosis awaiting lung transplantation. J. Physiol. Pharmacol. 2005, 56 (Suppl. 4), 99–105. [Google Scholar]
- Feltrim, M.I.; Rozanski, A.; Borges, A.C.; Cardoso, C.A.; Caramori, M.L.; Pego-Fernandes, P. The quality of life of patients on the lung transplantation waiting list. Transpl. Proc. 2008, 40, 819–821. [Google Scholar] [CrossRef]
- Michel-Cherqui, M.; Ley, L.; Szekely, B.; Dreyfus, J.F.; Fischler, M. Prevalence and characteristics of pain in patients awaiting lung transplantation. J. Pain Symptom Manag. 2015, 49, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Girard, F.; Chouinard, P.; Boudreault, D.; Poirier, C.; Richard, C.; Ruel, M.; Ferraro, P. Prevalence and impact of pain on the quality of life of lung transplant recipients: A prospective observational study. Chest 2006, 130, 1535–1540. [Google Scholar] [CrossRef]
- Forsberg, A.; Claeson, M.; Dahlman, G.B.; Lennerling, A. Pain, fatigue and well-being one to five years after lung transplantation-a nationwide cross-sectional study. Scand. J. Caring Sci. 2018, 32, 971–978. [Google Scholar] [CrossRef]
- Loxe, S.C.; de Mello, L.S.; Camara, L.; de Oliveira Braga Teixeira, R.H.; de Goes Salveti, M.; Gomes Galas, F.B.; Costa Auler Junior, J.O.; de Castro, C.C.B.; Corso Pereira, M.H.; Jardim, J.M. Chronic Pain After Lung Transplantation and Its Impact on Quality of Life: A 4-Year Follow-up. Transpl. Proc. 2020, 52, 1388–1393. [Google Scholar] [CrossRef] [PubMed]
- Shahabeddin Parizi, A.; Krabbe, P.F.M.; Buskens, E.; Bakker, S.J.L.; Vermeulen, K.M. A Scoping Review of Key Health Items in Self-Report Instruments Used Among Solid Organ Transplant Recipients. Patient 2019, 12, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Laurent, Q.; Michel-Cherqui, M.; Szekely, B.; Glorion, M.; Sage, E.; Trichereau, J.; Fischler, M.; Fessler, J.; Guen, M.L. Prevalence, Characteristics and Preoperative Predictors of Chronic Pain After Double-Lung Transplantation: A Prospective Cohort Study. J. Cardiothorac. Vasc. Anesth. 2022, 36, 500–509. [Google Scholar] [CrossRef]
- Taylor, J.L.; Smith, P.J.; Babyak, M.A.; Barbour, K.A.; Hoffman, B.M.; Sebring, D.L.; Davis, R.D.; Palmer, S.M.; Keefe, F.J.; Carney, R.M.; et al. Coping and quality of life in patients awaiting lung transplantation. J. Psychosom. Res. 2008, 65, 71–79. [Google Scholar] [CrossRef]
- Nelson, E.A.; Dowsey, M.M.; Knowles, S.R.; Castle, D.J.; Salzberg, M.R.; Monshat, K.; Dunin, A.J.; Choong, P.F. Systematic review of the efficacy of pre-surgical mind-body based therapies on post-operative outcome measures. Complement. Med. 2013, 21, 697–711. [Google Scholar] [CrossRef]
- Gross, C.R.; Kreitzer, M.J.; Thomas, W.; Reilly-Spong, M.; Cramer-Bornemann, M.; Nyman, J.A.; Frazier, P.; Ibrahim, H.N. Mindfulness-based stress reduction for solid organ transplant recipients: A randomized controlled trial. Altern. Health Med. 2010, 16, 30–38. [Google Scholar]
- Gross, C.R.; Reilly-Spong, M.; Park, T.; Zhao, R.; Gurvich, O.V.; Ibrahim, H.N. Telephone-adapted Mindfulness-based Stress Reduction (tMBSR) for patients awaiting kidney transplantation. Contemp. Clin. Trials 2017, 57, 37–43. [Google Scholar] [CrossRef]
- Tafaj-Reddy, O.; Brar, A.; Markell, M.S. Complementary and integrative medicine in kidney transplantation. Curr. Opin. Organ Transpl. 2019, 24, 87–91. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Babyak, M.A.; Keefe, F.J.; Davis, R.D.; Lacaille, R.A.; Carney, R.M.; Freedland, K.E.; Trulock, E.; Palmer, S.M. Telephone-based coping skills training for patients awaiting lung transplantation. J. Consult. Clin. Psychol. 2006, 74, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Hamza, M.A.; White, P.F.; Ahmed, H.E.; Ghoname, E.A. Effect of the frequency of transcutaneous electrical nerve stimulation on the postoperative opioid analgesic requirement and recovery profile. Anesthesiology 1999, 91, 1232–1238. [Google Scholar] [CrossRef]
- Hamza, M.A.; Ghoname, E.A.; White, P.F.; Craig, W.F.; Ahmed, H.E.; Gajraj, N.M.; Vakharia, A.S.; Noe, C.E. Effect of the duration of electrical stimulation on the analgesic response in patients with low back pain. Anesthesiology 1999, 91, 1622–1627. [Google Scholar] [CrossRef]
- Carli, F. Prehabilitation for the Anesthesiologist. Anesthesiology 2020, 133, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Bouhassira, D.; Attal, N.; Alchaar, H.; Boureau, F.; Brochet, B.; Bruxelle, J.; Cunin, G.; Fermanian, J.; Ginies, P.; Grun-Overdyking, A.; et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 2005, 114, 29–36. [Google Scholar] [CrossRef]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Carskadon, M.A.; Dement, W.C.; Mitler, M.M.; Guilleminault, C.; Zarcone, V.P.; Spiegel, R. Self-reports versus sleep laboratory findings in 122 drug-free subjects with complaints of chronic insomnia. Am. J. Psychiatry 1976, 133, 1382–1388. [Google Scholar] [CrossRef]
- EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [CrossRef]
- Ringsted, T.K.; Wildgaard, K.; Kreiner, S.; Kehlet, H. Pain-related impairment of daily activities after thoracic surgery: A questionnaire validation. Clin. J. Pain 2013, 29, 791–799. [Google Scholar] [CrossRef]
- Dreyfus, J.F.; Kassoul, A.; Michel-Cherqui, M.; Fischler, M.; Le Guen, M. A French version of Ringsted’s questionnaire on pain-related impairment of daily activities after lung surgery: A cohort study. Anaesth. Crit. Care Pain Med. 2019, 38, 615–621. [Google Scholar] [CrossRef]
- Montgomery, G.H.; Hallquist, M.N.; Schnur, J.B.; David, D.; Silverstein, J.H.; Bovbjerg, D.H. Mediators of a brief hypnosis intervention to control side effects in breast surgery patients: Response expectancies and emotional distress. J. Consult. Clin. Psychol. 2010, 78, 80–88. [Google Scholar] [CrossRef]
- Benson, P.E. Suggestion can help. Ann. R. Australas. Coll. Dent. Surg. 2000, 15, 284–285. [Google Scholar]
- Bhasin, M.K.; Dusek, J.A.; Chang, B.H.; Joseph, M.G.; Denninger, J.W.; Fricchione, G.L.; Benson, H.; Libermann, T.A. Relaxation response induces temporal transcriptome changes in energy metabolism, insulin secretion and inflammatory pathways. PLoS ONE 2013, 8, e62817, Erratum in PLoS ONE 2017, 12, e0172873. [Google Scholar] [CrossRef] [PubMed]
- Ju, W.; Ren, L.; Chen, J.; Du, Y. Efficacy of relaxation therapy as an effective nursing intervention for post-operative pain relief in patients undergoing abdominal surgery: A systematic review and meta-analysis. Exp. Med. 2019, 18, 2909–2916. [Google Scholar] [CrossRef] [PubMed]
- Thompson, T.; Terhune, D.B.; Oram, C.; Sharangparni, J.; Rouf, R.; Solmi, M.; Veronese, N.; Stubbs, B. The effectiveness of hypnosis for pain relief: A systematic review and meta-analysis of 85 controlled experimental trials. Neurosci. Biobehav. Rev. 2019, 99, 298–310. [Google Scholar] [CrossRef] [PubMed]
- Tefikow, S.; Barth, J.; Maichrowitz, S.; Beelmann, A.; Strauss, B.; Rosendahl, J. Efficacy of hypnosis in adults undergoing surgery or medical procedures: A meta-analysis of randomized controlled trials. Clin. Psychol. Rev. 2013, 33, 623–636. [Google Scholar] [CrossRef]
- Holler, M.; Koranyi, S.; Strauss, B.; Rosendahl, J. Efficacy of Hypnosis in Adults Undergoing Surgical Procedures: A meta-analytic update. Clin. Psychol. Rev. 2021, 85, 102001. [Google Scholar] [CrossRef] [PubMed]
- van Rangelrooij, K.; Solans-Buxeda, R.; Fernandez-Garcia, M.; Caycedo-Desprez, N.; Selvam, R.; Bulbena, A. Effectiveness of a 4-week sophrology program for primary care patients with moderate to high anxiety levels: A randomised controlled trial. Actas Esp. Psiquiatr. 2020, 48, 200–208. [Google Scholar] [PubMed]
- Ashton, C., Jr.; Whitworth, G.C.; Seldomridge, J.A.; Shapiro, P.A.; Weinberg, A.D.; Michler, R.E.; Smith, C.R.; Rose, E.A.; Fisher, S.; Oz, M.C. Self-hypnosis reduces anxiety following coronary artery bypass surgery. A prospective, randomized trial. J. Cardiovasc. Surg. 1997, 38, 69–75. [Google Scholar]
- Manworren, R.C.B.; Anderson, M.N.; Girard, E.D.; Ruscher, K.A.; Verissimo, A.M.; Palac, H.; Weiss, R.; Rader, C.; Hight, D. Postoperative Pain Outcomes After Nuss Procedures: Comparison of Epidural Analgesia, Continuous Infusion of Local Anesthetic, and Preoperative Self-Hypnosis Training. J. Laparoendosc. Adv. Surg. Tech. 2018, 28, 1234–1242. [Google Scholar] [CrossRef] [PubMed]
- Michel-Cherqui, M.; Szekely, B.; Fessler, J.; Glorion, M.; Sage, E.; Le Guen, M.; Trichereau, J.; Vallée, A.; Fischler, M. Feasibility and Usefulness of Self-Hypnosis in Patients Undergoing Double-Lung Transplantation During the Pre- and Postoperative Periods: A Randomized Study. J. Cardiothorac. Vasc. Anesth. 2022, 36, 2490–2499. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Smith, P.J.; Sherwood, A.; Mabe, S.; Snyder, L.; Frankel, C.; McKee, D.C.; Hamilton, N.; Keefe, F.J.; Shearer, S.; et al. Remote Therapy to Improve Outcomes in Lung Transplant Recipients: Design of the INSPIRE-III Randomized Clinical Trial. Transpl. Direct 2020, 6, e535. [Google Scholar] [CrossRef]
- Johnson, M.I.; Paley, C.A.; Jones, G.; Mulvey, M.R.; Wittkopf, P.G. Efficacy and safety of transcutaneous electrical nerve stimulation (TENS) for acute and chronic pain in adults: A systematic review and meta-analysis of 381 studies (the meta-TENS study). BMJ Open 2022, 12, e051073. [Google Scholar] [CrossRef]
- Zhou, J.; Dan, Y.; Yixian, Y.; Lyu, M.; Zhong, J.; Wang, Z.; Zhu, Y.; Liu, L. Efficacy of Transcutaneous Electronic Nerve Stimulation in Postoperative Analgesia After Pulmonary Surgery: A Systematic Review and Meta-Analysis. Am. J. Phys. Med. Rehabil 2020, 99, 241–249. [Google Scholar] [CrossRef]
- Deng, G. Integrative Medicine Therapies for Pain Management in Cancer Patients. Cancer J. 2019, 25, 343–348. [Google Scholar] [CrossRef]
- Patel, N.; Pierson, J.; Lee, T.; Mast, B.; Lee, B.T.; Estores, I.; Singhal, D. Utilization and Perception of Integrative Medicine Among Plastic Surgery Patients. Ann. Plast. Surg. 2017, 78, 557–561. [Google Scholar] [CrossRef]
- Downe, S.; Finlayson, K.; Melvin, C.; Spiby, H.; Ali, S.; Diggle, P.; Gyte, G.; Hinder, S.; Miller, V.; Slade, P.; et al. Self-hypnosis for intrapartum pain management in pregnant nulliparous women: A randomised controlled trial of clinical effectiveness. BJOG 2015, 122, 1226–1234. [Google Scholar] [CrossRef] [PubMed]


| At Entry n = 59 | Three Months after Transplantation n = 59 | p-Value | |||
|---|---|---|---|---|---|
| Age (years) | 34 (28) | ||||
| Sex female/male | 34 (57.6)/ 25 (42.4) | ||||
| Lung disease | |||||
| Cystic fibrosis | 32 (54.2) | ||||
| Emphysema/COPD | 16 (27.2) | ||||
| Lung fibrosis | 9 (15.2) | ||||
| Other | 2 (3.4) | ||||
| Pain | |||||
| Presence of pain | 23 (40.3) {2} | 21 (35.6) | 0.532 | ||
| Intensity of pain, VAS * | |||||
| During the consultation | 0 (18) {3} | 0 (12) | 0.630 | ||
| Maximum pain intensity during the last three days | 16 (52) {3} | 27 (50) | 0.654 | ||
| Usual pain intensity during the last three days | 6 (32) {3} | 4 (25) | 0.320 | ||
| Localization of pain | |||||
| Thoracic pain | 13 (30.9) {17} | 18 (38.3) {12} | 0.439 | ||
| Care related pain | 8 (18.6) {16} | 16 (34.0) {12} | 0.098 | ||
| Neuropathic pain ** | 2 (3.4) {1} | 16 (27.6) {1} | 0.0008 | ||
| Analgesics | |||||
| None | 52 (88.1) | 39 (66.1) | 0.004 | ||
| WHO classification *** | 0.088 | ||||
| Class 1 | 2 (3.4) | 9 (15.2) | |||
| Class 2 | 3 (5.1) | 9 (15.2) | |||
| Class 3 | 2 (3.4) | 2 (3.4) | |||
| Treatment of neuropathic pain | 1 (1.7) | 4 (6.8) | 0.180 | ||
| Non-medicinal treatment | 1 (1.7) | 0 (0) | NA | ||
| Benzodiazepine | 7 (11.9) | 11 (18.6) | 0.206 | ||
| Quality of life | |||||
| HAD score **** | |||||
| A | 8 (8) {2} | 5 (4) | <0.0001 | ||
| D | 6 (6) {2} | 2 (3) | <0.0001 | ||
| Perceived Stress Score | 28 (12) {2} | 22 (9) | <0.0001 | ||
| Spiegel score | 18 (4) {2} | 18 (6) | 0.733 | ||
| EuroQol visual analogic scale | 40 (33) {2} | 75 (20) | <0.0001 | ||
| Ringsted score total | 5 (8) | ||||
| Routine | 2 (5) | ||||
| Task | 2 (5) | ||||
| Number of Sessions Performed | Total Number of Sessions | |||
|---|---|---|---|---|
| Before Transplantation | After Transplantation | |||
| Holistic gymnastics | ||||
| Training Session | 57 | 30 | 87 | |
| Self-Practice | 78 | 127 | 205 | |
| Total | 135 | 157 | 292 | |
| Self-hypnosis | ||||
| Training Session | 59 | 51 | 110 | |
| Self-Practice | 82 | 575 | 657 | |
| Total | 141 | 626 | 767 | |
| Relaxation | ||||
| Training Session | 54 | 23 | 77 | |
| Self-Practice | 613 | 1332 | 1945 | |
| Total | 667 | 1355 | 2022 | |
| Sophrology | ||||
| Training Session | 8 | 1 | 9 | |
| Self-Practice | 28 | 24 | 52 | |
| Total | 36 | 25 | 61 | |
| Transcutaneous electrical nerve stimulation (TENS) | ||||
| Training Session | 10 | 54 | 64 | |
| Self-Practice | 53 | 1100 | 1153 | |
| Total | 63 | 1154 | 1217 | |
| SH n = 50 | R n = 51 | S n = 3 | HG n = 49 | T n = 36 | P Global | P between Techniques | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients | |||||||||||
| Usability | 3 (7) | 5 (10) | 6 (8) | 1 (6) | 9 (4) | <0.0001 | SH vs. T 0.0001 | R vs. T 0.024 | HG vs. T <0.0001 | ||
| Conformity | 3 (6) | 5 (7) | 4 (9) | 0 (6) | 10 (3) | <0.0001 | SH vs. T <0.0001 | R vs. T <0.0001 | HG vs. T <0.0001 | ||
| Autonomy | 4 (7) | 5 (10) | 4 (8) | 1 (6) | 10 (2) | <0.0001 | SH vs. T <0.0001 | R vs. T 0.0003 | HG vs. T <0.0001 | R vs. HG 0.031 | |
| Adaptation | 3 (8) | 5 (10) | 4 (9) | 2 (7) | 10 (4) | <0.0001 | SH vs. T <0.0001 | R vs. T 0.0006 | HG vs. T <0.0001 | ||
| Involvement | 7 (5) | 7 (7) | 6 (9) | 7 (5) | 10 (3) | 0.0299 | SH vs. T 0.0228 | ||||
| Benefit | 5 (10) | 5 (10) | 6 (8) | 6 (10) | 7 (7) | 0.3541 | |||||
| Caregivers | |||||||||||
| Usability | 4 (10) | 5 (10) | 5 (10) | 5 (8) | 8 (5) | 0.0065 | SH vs. T 0.025 | HG vs. T 0.003 | |||
| Conformity | 3 (10) | 5 (8) | 4 (10) | 0 (5) | 10 (5) | <0.0001 | SH vs. T 0.0001 | R vs. T 0.003 | HG vs. T <0.0001 | R vs. GH 0.007 | |
| Autonomy | 5 (9) | 6 (10) | 5 (10) | 0 (5) | 10 (2) | <0.0001 | SH vs. T 0.0002 | R vs. T 0.007 | HG vs. T <0.0001 | R vs. GH 0.007 | |
| Adaptation | 5 (10) | 7 (10) | 5 (10) | 1 (7) | 10 (5) | <0.0001 | SH vs. T 0.0431 | HG vs. T <0.0001 | R vs. GH 0.032 | ||
| Involvement | 8 (5) | 10 (3) | 8 (5) | 10 (3) | 10 (0) | 0.0059 | SH vs. T 0.0020 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michel-Cherqui, M.; Fessler, J.; Szekely, B.; Glorion, M.; Sage, E.; Fischler, M.; Vallée, A.; Le Guen, M. Complementary Therapy Learning in the Setting of Lung Transplantation: A Single-Center Observational Study of Appropriation and Efficacy. J. Clin. Med. 2023, 12, 1722. https://doi.org/10.3390/jcm12051722
Michel-Cherqui M, Fessler J, Szekely B, Glorion M, Sage E, Fischler M, Vallée A, Le Guen M. Complementary Therapy Learning in the Setting of Lung Transplantation: A Single-Center Observational Study of Appropriation and Efficacy. Journal of Clinical Medicine. 2023; 12(5):1722. https://doi.org/10.3390/jcm12051722
Chicago/Turabian StyleMichel-Cherqui, Mireille, Julien Fessler, Barbara Szekely, Matthieu Glorion, Edouard Sage, Marc Fischler, Alexandre Vallée, and Morgan Le Guen. 2023. "Complementary Therapy Learning in the Setting of Lung Transplantation: A Single-Center Observational Study of Appropriation and Efficacy" Journal of Clinical Medicine 12, no. 5: 1722. https://doi.org/10.3390/jcm12051722
APA StyleMichel-Cherqui, M., Fessler, J., Szekely, B., Glorion, M., Sage, E., Fischler, M., Vallée, A., & Le Guen, M. (2023). Complementary Therapy Learning in the Setting of Lung Transplantation: A Single-Center Observational Study of Appropriation and Efficacy. Journal of Clinical Medicine, 12(5), 1722. https://doi.org/10.3390/jcm12051722







