Tricuspid Valve Geometrical Changes in Patients with Functional Tricuspid Regurgitation: Insights from a CT Scan Analysis Focusing on Commissures
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. CT Scan Acquisition
2.3. CT Data Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. CT Assessment of TV Components
4.2. TV Annulus Remodelling
4.3. TR Grade Correlation
4.4. Clinical Implications
4.5. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Taramasso, M.; Gavazzoni, M.; Pozzoli, A.; Dreyfus, G.D.; Bolling, S.F.; George, I.; Kapos, I.; Tanner, F.C.; Zuber, M.; Maisano, F.; et al. Tricuspid Regurgitation: Predicting the Need for Intervention, Procedural Success, and Recurrence of Disease. JACC Cardiovasc. Imaging 2019, 12, 605–621. [Google Scholar] [CrossRef] [PubMed]
- Topilsky, Y.; Nkomo, V.T.; Vatury, O.; Michelena, H.I.; Letourneau, T.; Suri, R.M.; Pislaru, S.; Park, S.; Mahoney, D.W.; Biner, S.; et al. Clinical Outcome of Isolated Tricuspid Regurgitation. JACC Cardiovasc. Imaging 2014, 7, 1185–1194. [Google Scholar] [CrossRef] [PubMed]
- Zack, C.J.; Fender, E.A.; Chandrashekar, P.; Reddy, Y.N.; Bennett, C.E.; Stulak, J.M.; Miller, V.M.; Nishimura, R.A. National Trends and Outcomes in Isolated Tricuspid Valve Surgery. J. Am. Coll. Cardiol. 2017, 70, 2953–2960. [Google Scholar] [CrossRef] [PubMed]
- Cammalleri, V.; Mega, S.; Ussia, G.P.; Grigioni, F. Mitral and Tricuspid Valves Percutaneous Repair in Patients with Advanced Heart Failure: Panacea, or Pandora’s Box? Heart Fail Clin. 2021, 17, 607–618. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., 3rd; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2021, 77, 450–500. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Praz, F.; Muraru, D.; Kreidel, F.; Lurz, P.; Hahn, R.T.; Delgado, V.; Senni, M.; von Bardeleben, R.S.; Nickenig, G.; Hausleiter, J.; et al. Transcatheter Treat. Tricuspid Valve Disease. EuroIntervention 2021, 17, 791–808. [Google Scholar] [CrossRef]
- Cammalleri, V.; Carpenito, M.; Bono, M.C.; Mega, S.; Ussia, G.P.; Grigioni, F. Transcatheter Tricuspid Valve Therapy: From Anatomy to Intervention. Front Cardiovasc. Med. 2021, 8, 778445. [Google Scholar] [CrossRef]
- Schlossbauer, S.A.; Faletra, F.F.; Paiocchi, V.L.; Leo, L.A.; Franciosi, G.; Bonanni, M.; Angelini, G.; Pavon, A.G.; Ferrari, E.; Ho, S.Y.; et al. Multimodality Imaging of the Anatomy of Tricuspid Valve. J. Cardiovasc. Dev. Dis. 2021, 8, 107. [Google Scholar] [CrossRef]
- Romeo, F.; Cammalleri, V.; Ruvolo, G.; Quadri, A.; De Vico, P.; Muscoli, S.; Marchei, M.; Meloni, S.; Conti, F.; Ussia, G.P. Trans-Catheter Mitral Valve Implantation for Mitral Regurgitation: Clinical Case Description and Literature Review. J. Cardiovasc. Med. 2016, 17, 85–91. [Google Scholar] [CrossRef]
- Van Rosendael, P.J.; Joyce, E.; Katsanos, S.; Debonnaire, P.; Kamperidis, V.; van Der Kley, F.; Schalij, M.J.; Bax, J.J.; Ajmone Marsan, N.; Delgado, V. Tricuspid Valve Remodelling in Functional Tricuspid Regurgitation: Multidetector Row Computed Tomography Insights. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 96–105. [Google Scholar] [CrossRef]
- Ranard, L.S.; Vahl, T.P.; Chung, C.J.; Sadri, S.; Khalique, O.K.; Hamid, N.; Nazif, T.; George, I.; Ng, V.; Patel, A.; et al. Impact of Inferior Vena Cava Entry Characteristics on Tricuspid Annular Access during Transcatheter Interventions. Catheter. Cardiovasc. Interv. 2022, 99, 1268–1276. [Google Scholar] [CrossRef]
- Khalique, O.K.; Jelnin, V.; Hueske, A.; Lawlor, M.; Leon, M.B.; Kodali, S.K.; Akkoc, D.; Pettway, E.; Hahn, R.T.; Hamid, N.B.; et al. Right Heart Morphology of Candidate Patients for Transcatheter Tricuspid Valve Interventions. Cardiovasc. Eng. Technol. 2022, 13, 573–589. [Google Scholar] [CrossRef]
- Cammalleri, V.; Carpenito, M.; De Stefano, D.; Ussia, G.P.; Bono, M.C.; Mega, S.; Nusca, A.; Cocco, N.; Nobile, E.; De Filippis, A.; et al. Novel Computed Tomography Variables for Assessing Tricuspid Valve Morphology: Results from the TRIMA (Tricuspid Regurgitation IMAging) Study. J. Clin. Med. 2022, 11, 2825. [Google Scholar] [CrossRef] [PubMed]
- Hell, M.M.; Emrich, T.; Kreidel, F.; Kreitner, K.F.; Schoepf, U.J.; Münzel, T.; von Bardeleben, R.S. Computed Tomography Imaging Needs for Novel Transcatheter Tricuspid Valve Repair and Replacement Therapies. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Van Der Wall, E.E.; Schuijf, J.D.; Bax, J.J. Triple Rule-out CT Coronary Angiography: Three of a Kind? Int. J. Cardiovasc. Imaging 2009, 25, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Palmisano, A.; Vignale, D.; Tadic, M.; Moroni, F.; De Stefano, D.; Gatti, M.; Boccia, E.; Faletti, R.; Oppizzi, M.; Peretto, G.; et al. Myocardial Late Contrast Enhancement CT in Troponin-Positive Acute Chest Pain Syndrome. Radiology 2022, 302, 545–553. [Google Scholar] [CrossRef]
- Bernardini, F.; Gelfusa, M.; Celeski, M.; Coletti, F.; Nusca, A.; De Stefano, D.; Piccirillo, F.; Mangiacapra, F.; Gallo, P.; Cammalleri, V.; et al. Beyond the Calcium Score: What Additional Information from a CT Scan Can Assist in Cardiovascular Risk Assessment? Appl. Sci. 2023, 13, 241. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef]
- Hahn, R.T.; Zamorano, J.L. The Need for a New Tricuspid Regurgitation Grading Scheme. Eur. Heart J.-Cardiovasc. Imaging 2017, 18, 1342–1343. [Google Scholar] [CrossRef]
- Hahn, R.T.; Badano, L.P.; Bartko, P.E.; Muraru, D.; Maisano, F.; Zamorano, J.L.; Donal, E. Tricuspid regurgitation: Recent advances in understanding pathophysiology, severity grading and outcome. Eur. Heart J. Cardiovasc. Imaging 2022, 23, 913–929. [Google Scholar] [CrossRef] [PubMed]
- Praz, F.; Khalique, O.K.; Macedo, L.G.D.R.; Pulerwitz, T.C.; Jantz, J.; Wu, I.Y.; Kantor, A.; Patel, A.; Vahl, T.; Bapat, V.; et al. Comparison between Three-Dimensional Echocardiography and Computed Tomography for Comprehensive Tricuspid Annulus and Valve Assessment in Severe Tricuspid Regurgitation: Implications for Tricuspid Regurgitation Grading and Transcatheter Therapies. J. Am. Soc. Echocardiogr. 2018, 31, 1190–1202.E3. [Google Scholar] [CrossRef] [PubMed]
- Pulerwitz, T.C.; Khalique, O.K.; Leb, J.; Hahn, R.T.; Nazif, T.; Leon, M.B.; George, I.; Vahl, T.P.; D’Souza, B.; Bapat, V.N.; et al. Optimizing Cardiac CT Protocols for Comprehensive Acquisition Prior to Percutaneous MV and TV Repair/Replacement. JACC Cardiovasc. Imaging 2020, 13, 836–850. [Google Scholar] [CrossRef] [PubMed]
- Silver, M.D.; Lam, J.H.; Ranganathan, N.; Wigle, E.D. Morphology of the Human Tricuspid Valve. Circulation 1971, 43, 333–348. [Google Scholar] [CrossRef]
- Joudinaud, T.M.; Flecher, E.M.; Duran, C.M.G. Functional Terminology for the Tricuspid Valve. J. Heart Valve Dis. 2006, 15, 382–388. [Google Scholar]
- Hołda, M.K.; Zhingre Sanchez, J.D.; Bateman, M.G.; Iaizzo, P.A. Right Atrioventricular Valve Leaflet Morphology Redefined. JACC Cardiovasc. Interv. 2019, 12, 169–178. [Google Scholar] [CrossRef]
- Tretter, J.T.; Sarwark, A.E.; Anderson, R.H.; Spicer, D.E. Assessment of the Anatomical Variation to Be Found in the Normal Tricuspid Valve. Clin. Anat. 2016, 29, 399–407. [Google Scholar] [CrossRef]
- Victor, S.; Nayak, V.M. The Tricuspid Valve Is Bicuspid. J. Heart Valve Dis. 1994, 3, 27–36. [Google Scholar] [CrossRef]
- Hahn, R.T.; Weckbach, L.T.; Noack, T.; Hamid, N.; Kitamura, M.; Bae, R.; Lurz, P.; Kodali, S.K.; Sorajja, P.; Hausleiter, J.; et al. Proposal for a Standard Echocardiographic Tricuspid Valve Nomenclature. JACC Cardiovasc. Imaging 2021, 14, 1299–1305. [Google Scholar] [CrossRef]
- Sugiura, A.; Tanaka, T.; Kavsur, R.; Öztürk, C.; Vogelhuber, J.; Wilde, N.; Becher, M.U.; Zimmer, S.; Nickenig, G.; Weber, M. Leaflet Configuration and Residual Tricuspid Regurgitation After Transcatheter Edge-to-Edge Tricuspid Repair. JACC Cardiovasc. Interv. 2021, 14, 2260–2270. [Google Scholar] [CrossRef]
- Kitamura, M.; Kresoja, K.P.; Besler, C.; Leontyev, S.; Kiefer, P.; Rommel, K.P.; Otto, W.; Forner, A.F.; Ender, J.; Holzhey, D.M.; et al. Impact of Tricuspid Valve Morphology on Clinical Outcomes After Transcatheter Edge-to-Edge Repair. JACC Cardiovasc. Interv. 2021, 14, 1616–1618. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, S.; Saracino, G.; Matsumura, Y.; Daimon, M.; Tran, H.; Greenberg, N.L.; Hozumi, T.; Yoshikawa, J.; Thomas, J.D.; Shiota, T. Three-Dimensional Geometry of the Tricuspid Annulus in Healthy Subjects and in Patients with Functional Tricuspid Regurgitation: A Real-Time, 3-Dimensional Echocardiographic Study. Circulation 2006, 114, I492–I498. [Google Scholar] [CrossRef] [PubMed]
- Ton-Nu, T.T.; Levine, R.A.; Handschumacher, M.D.; Dorer, D.J.; Yosefy, C.; Fan, D.; Hua, L.; Jiang, L.; Hung, J. Geometric Determinants of Functional Tricuspid Regurgitation: Insights from 3-Dimensional Echocardiography. Circulation 2006, 114, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Tei, C.; Pilgrim, J.P.; Shah, P.M.; Ormiston, J.A.; Wong, M. The Tricuspid Valve Annulus: Study of Size and Motion in Normal Subjects and in Patients with Tricuspid Regurgitation. Circulation 1982, 66, 665–671. [Google Scholar] [CrossRef]
- Badano, L.P.; Muraru, D.; Enriquez-Sarano, M. Assessment of Functional Tricuspid Regurgitation. Eur. Heart J. 2013, 34, 1875–1885. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Song, J.M.; Lee, E.Y.; Kim, Y.J.; Kang, D.H.; Song, J.K. Geometric and Hemodynamic Determinants of Functional Tricuspid Regurgitation: A Real-Time Three-Dimensional Echocardiography Study. Int. J. Cardiol. 2008, 124, 160–165. [Google Scholar] [CrossRef]
- Guta, A.C.; Badano, L.P.; Tomaselli, M.; Mihalcea, D.; Bartos, D.; Parati, G.; Muraru, D. The Pathophysiological Link between Right Atrial Remodeling and Functional Tricuspid Regurgitation in Patients with Atrial Fibrillation: A Three-Dimensional Echocardiography Study. J. Am. Soc. Echocardiogr. 2021, 34, 585–594.E1. [Google Scholar] [CrossRef] [PubMed]
- Muraru, D.; Addetia, K.; Guta, A.C.; Ochoa-Jimenez, R.C.; Genovese, D.; Veronesi, F.; Basso, C.; Iliceto, S.; Badano, L.P.; Lang, R.M. Right Atrial Volume Is a Major Determinant of Tricuspid Annulus Area in Functional Tricuspid Regurgitation: A Three-Dimensional Echocardiographic Study. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Carpenito, M.; Cammalleri, V.; Vitez, L.; De Filippis, A.; Nobile, E.; Bono, M.C.; Mega, S.; Bunc, M.; Grigioni, F.; Ussia, G.P. Edge-to-Edge Repair for Tricuspid Valve Regurgitation. Preliminary Echo-Data and Clinical Implications from the Tricuspid Regurgitation IMAging (TRIMA) Study. J. Clin. Med. 2022, 11, 5609. [Google Scholar] [CrossRef]
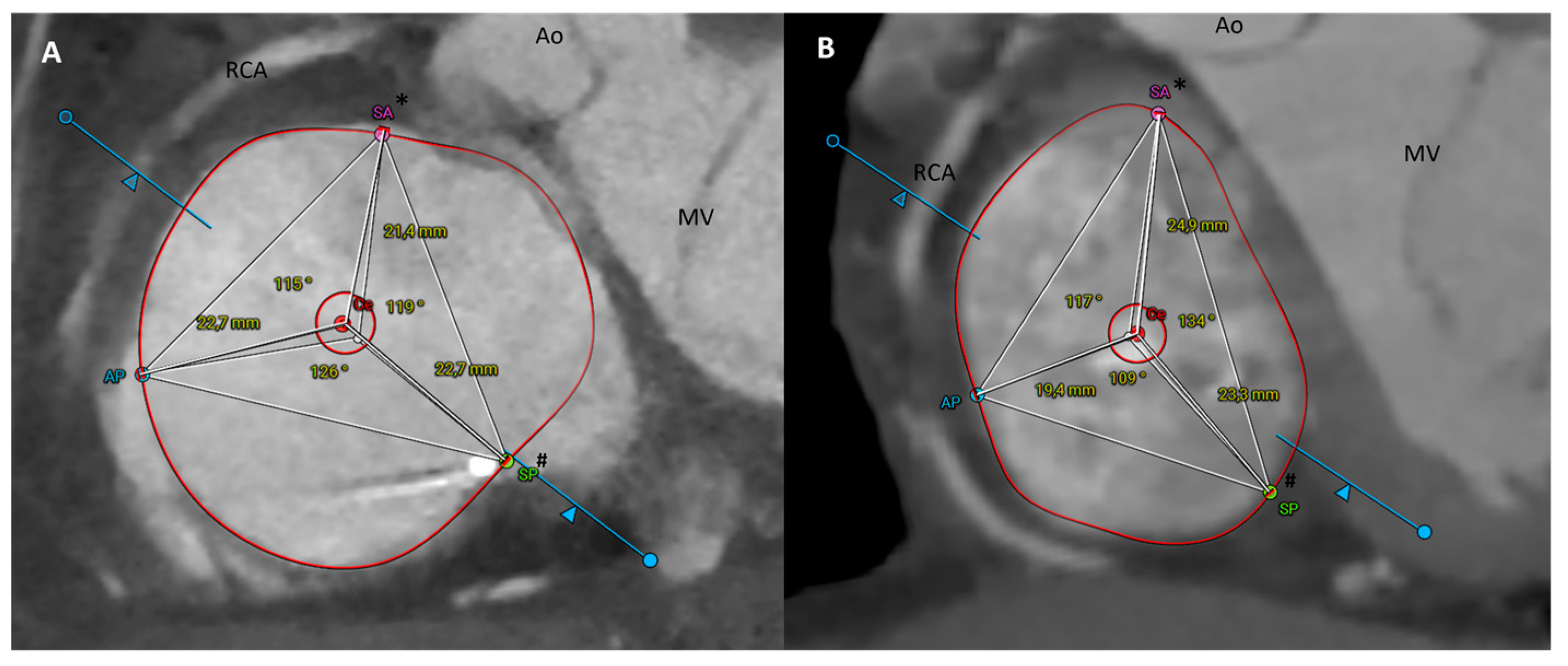


| Parameter | Method | Description |
|---|---|---|
| TV annulus area | Semi-automated | TV annulus area (cm2) |
| TV annulus perimeter | Semi-automated | TV annulus perimeter (mm) |
| Septal-lateral diameter | Manual | Septal-lateral dimension of the TV annulus (mm), measured as the maximal distance in septal to lateral direction and coinciding with the annulus measurement in the four-chamber view |
| Antero-posterior diameter | Manual | Antero-posterior dimension of the TV annulus (mm), obtained orthogonally to the septal-lateral diameter and corresponding with the measurement in the two-chamber view |
| Eccentricity index | Manual | Ratio between the antero-posterior/septal-lateral diameter, it expresses the shape of the TV annulus |
| AS-PS | Automated | Distance between the antero-septal and postero-septal commissure (mm) |
| PS-AP | Automated | Distance between the postero-septal and antero-posterior commissure (mm) |
| AP-AS | Automated | Distance between the antero-posterior and antero-septal commissure (mm) |
| Ce-AS | Manual | Segment between the centroid and the antero-septal commissure (mm) |
| Ce-PS | Manual | Segment between the centroid and the postero-septal commissure (mm) |
| Ce-AP | Manual | Segment between the centroid and the antero-posterior commissure (mm) |
| α | Manual | Angle between the segments Ce-AS and Ce-PS (°) |
| β | Manual | Angle between the segments Ce-PS and Ce-AP (°) |
| γ | Manual | Angle between the segments Ce-AP and Ce-AS (°) |
| TR ≥ 3+ (n = 43) | Control (n = 43) | p | |
|---|---|---|---|
| Age, years ± SD | 78.07 ± 7.69 | 71.65 ± 13.67 | 0.009 |
| Male, n (%) | 12 (28) | 24 (56) | 0.009 |
| BMI, kg/m2 ± SD | 24.4 ± 3.89 | 23.22 ± 4.12 | 0.176 |
| Atrial fibrillation, n (%) | 39 (91) | 7 (16) | <0.001 |
| Hypertension, n (%) | 25 (58) | 22 (51) | 0.665 |
| Diabetes, n (%) | 10 (23) | 7 (16) | 0.588 |
| Dyslipidemia, n (%) | 22 (51) | 18 (42) | 0.51 |
| LVEF, % ± SD | 51.28 ± 3.89 | 53.87 ± 8.53 | 0.074 |
| Permanent PM/ICD/CRT | 18 (41) | 0 | <0.001 |
| TR ≥ 3+ (n = 43) | Control (n = 43) | Difference (95% CI) | p | |
|---|---|---|---|---|
| Annulus area (cm2 ± SD) | 16.84 ± 3.55 | 12.09 ± 2.37 | 4.75 (3.45 to 6.05) | <0.001 |
| Annulus perimeter (mm ± SD) | 147.77 ± 17.15 | 129.47 ± 13.24 | 18.29 (11.72 to 24.86) | <0.001 |
| SL diameter (mm ± SD) | 46.80 ± 6.44 | 36.80 ± 5.21 | 10 (7.49 to 12.51) | <0.001 |
| AP diameter (mm ± SD) | 45.67 ± 5.05 | 39.39 ± 4.97 | 6.28 (4.13 to 8.43) | <0.001 |
| Eccentricity (index ± SD) | 0.99 ± 0.12 | 1.11 ± 0.31 | −0.12 (−0.22 to −0.02) | 0.022 |
| AS-PS (mm ± SD) | 38.64 ± 5.67 | 35.06 ± 6.83 | 3.58 (0.89 to 6.27) | 0.010 |
| PS-AP (mm ± SD) | 40.71 ± 5.74 | 35.23 ± 6.59 | 5.49 (2.83 to 8.14) | <0.001 |
| AP-AS (mm ± SD) | 38.80 ± 5.83 | 31.77 ± 4.36 | 7.03 (4.50 to 9.06) | <0.001 |
| Ce-AS (mm ± SD) | 21.98 ± 2.90 | 18.32 ± 3.12 | 3.66 (2.37 to 4.96) | <0.001 |
| Ce-PS (mm ± SD) | 23.02 ± 3.77 | 20.88 ± 3.04 | 2.14 (0.67 to 3.61) | 0.005 |
| Ce-AP (mm ± SD) | 22.94 ± 2.84 | 19.22 ± 3.03 | 3.73 (2.46 to 4.98) | <0.001 |
| α (° ± SD) | 117.91 ± 9.43 | 121.81 ± 9.49 | −3.91 (−7.96 to 0.15) | 0.09 |
| β (° ± SD) | 123.49 ± 8.05 | 124.05 ± 13.16 | −0.56 (−5.31 to 4.19) | 0.815 |
| γ (° ± SD) | 118.14 ± 8.69 | 114.14 ± 8.33 | 4.00 (0.35 to 7.66) | 0.032 |
| Coefficient | 95% CI | p | |
|---|---|---|---|
| AS-PS | 0.146 | 0.105 to 0.188 | <0.001 |
| PS-AP | 0.215 | 0.174 to 0.256 | <0.001 |
| AP-AS | 0.349 | 0.299 to 0.399 | <0.001 |
| Ce-AS | 0.497 | 0.415 to 0.578 | <0.001 |
| Ce-PS | 0.273 | 0.181 to 0.366 | <0.001 |
| Ce-AP | 0.479 | 0.385 to 0.573 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cammalleri, V.; Nobile, E.; De Stefano, D.; Carpenito, M.; Mega, S.; Bono, M.C.; De Filippis, A.; Nusca, A.; Quattrocchi, C.C.; Grigioni, F.; et al. Tricuspid Valve Geometrical Changes in Patients with Functional Tricuspid Regurgitation: Insights from a CT Scan Analysis Focusing on Commissures. J. Clin. Med. 2023, 12, 1712. https://doi.org/10.3390/jcm12051712
Cammalleri V, Nobile E, De Stefano D, Carpenito M, Mega S, Bono MC, De Filippis A, Nusca A, Quattrocchi CC, Grigioni F, et al. Tricuspid Valve Geometrical Changes in Patients with Functional Tricuspid Regurgitation: Insights from a CT Scan Analysis Focusing on Commissures. Journal of Clinical Medicine. 2023; 12(5):1712. https://doi.org/10.3390/jcm12051712
Chicago/Turabian StyleCammalleri, Valeria, Edoardo Nobile, Domenico De Stefano, Myriam Carpenito, Simona Mega, Maria Caterina Bono, Aurelio De Filippis, Annunziata Nusca, Carlo Cosimo Quattrocchi, Francesco Grigioni, and et al. 2023. "Tricuspid Valve Geometrical Changes in Patients with Functional Tricuspid Regurgitation: Insights from a CT Scan Analysis Focusing on Commissures" Journal of Clinical Medicine 12, no. 5: 1712. https://doi.org/10.3390/jcm12051712
APA StyleCammalleri, V., Nobile, E., De Stefano, D., Carpenito, M., Mega, S., Bono, M. C., De Filippis, A., Nusca, A., Quattrocchi, C. C., Grigioni, F., & Ussia, G. P. (2023). Tricuspid Valve Geometrical Changes in Patients with Functional Tricuspid Regurgitation: Insights from a CT Scan Analysis Focusing on Commissures. Journal of Clinical Medicine, 12(5), 1712. https://doi.org/10.3390/jcm12051712








