Cardioplegia in Open Heart Surgery: Age Matters
Abstract
:1. Introduction
2. Data Sources
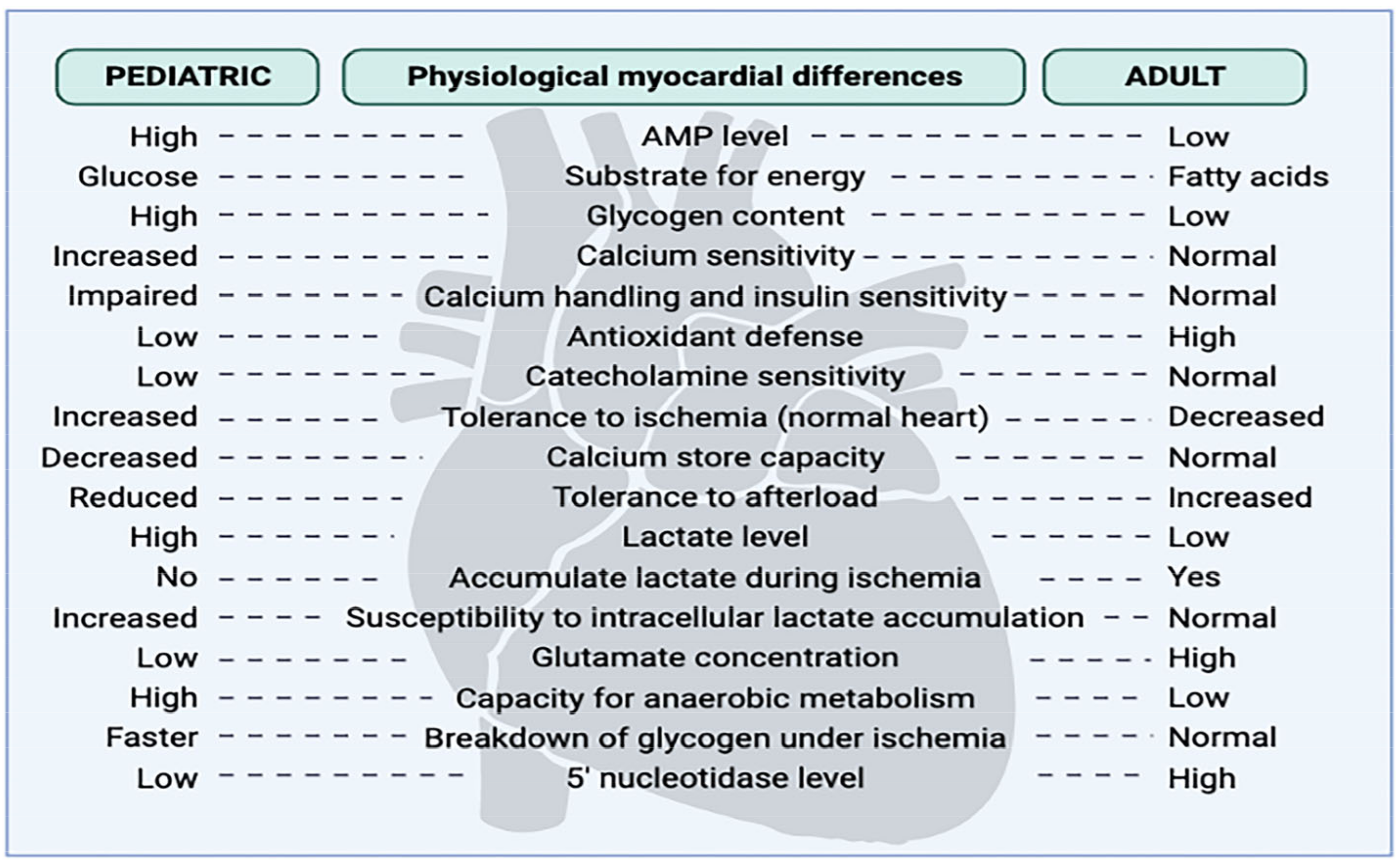
3. Differences in the Response of Adults and Pediatric Hearts to I–R
4. Cardioplegia as a Tool for Heart Preservation throughout History
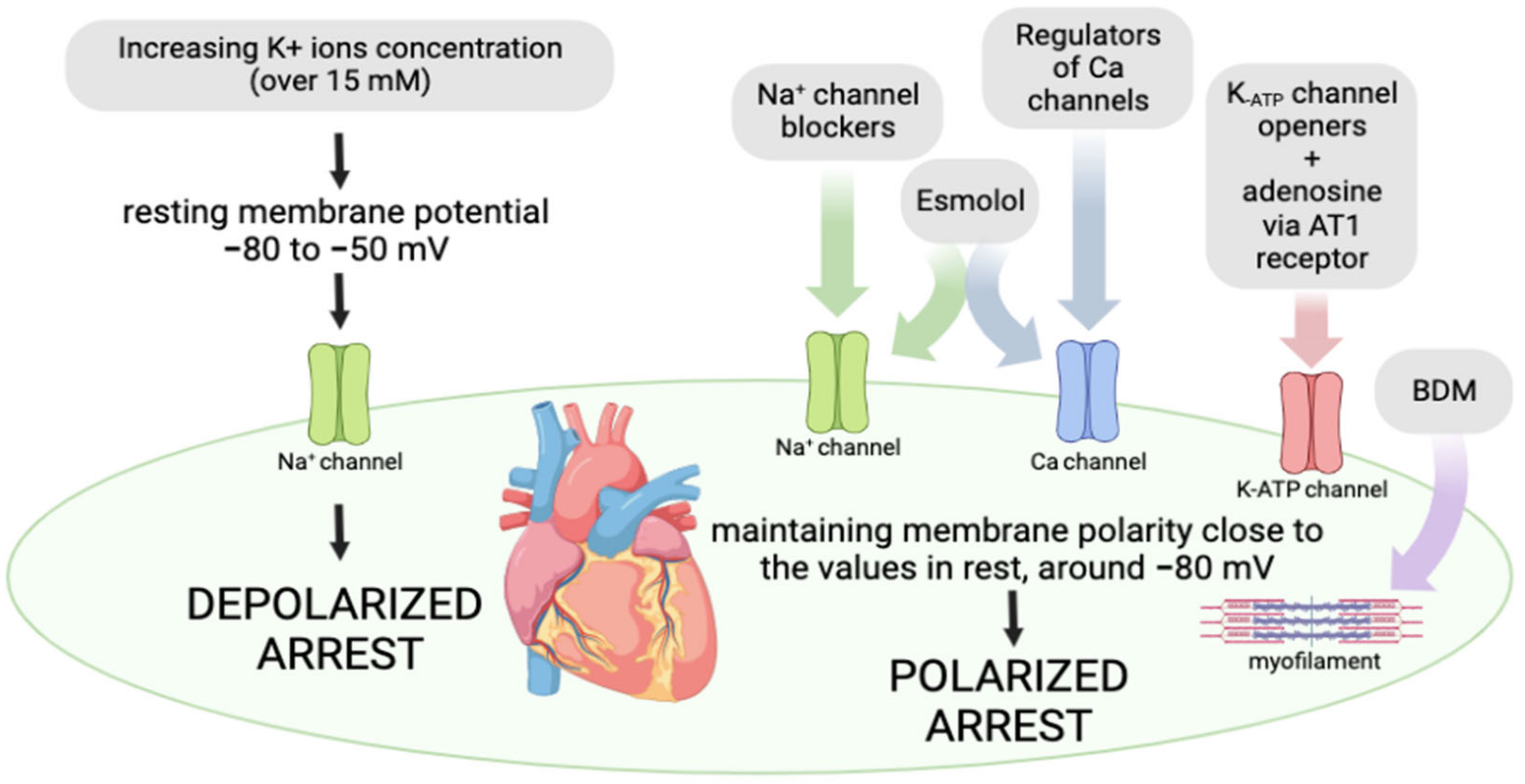
4.1. Membrane Polarity as a Target for Cardioprotection
4.1.1. Depolarized Arrest
4.1.2. Polarized Arrest
4.1.3. Routes of Cardioplegic Solution Application: Advantages and Disadvantages
4.1.4. Different Temperatures of Cardioplegic Solutions: Advantages and Disadvantages
4.1.5. Continuous and Intermittent Cardioplegia: Advantages and Disadvantages
4.1.6. Type of Cardioplegic Solutions
Crystalloid Cardioplegia
Most Commonly Used Crystalloid Cardioplegia in the Pediatric Population
Blood Cardioplegia
5. How Adjuncts in Cardioplegic Solutions Affect the Extent of Myocardial Injury in the Pediatric Population: Data from Clinical Studies
| Surgical Procedure | Patients Age | Applied Cardioplegia | Dosage and Administration | Temperature | Patients Per Group | Parameters of MI Assessment | Conclusion. Study/Year |
|---|---|---|---|---|---|---|---|
| Open cardiac surgery | 1–120 months | STH I | Anterograde administrations of 25 mL/kg/min for 4 min | 4–6 °C | 27 infants | cTnI | STH cardioplegia is associated with MI, with more susceptibility to injury in infants than children. Immura H et al./2001 [55] |
| 31 ≥ 12 months | |||||||
| Elective ventricular septal defect repair in children | 3–48 months | STH I crystalloid cardioplegia | Anterograde administrations of 25 mL/kg for 4 min, followed by a 2 min repeated dose of 15 mL/kg at 20 to 30 min intervals | 4–6 °C | 21 | cTnI | Blood cardioplegia exerted more beneficial effects in heart preservation and significantly attenuated metabolic stress in ischemic conditions. Caputo M et al./2002 [58] |
| 4:1 dilution blood/STH I crystalloid cardioplegia | 19 | ||||||
| Cardiac surgery | 4.5–98 months | STH I crystalloid cardioplegia | Anterograde administrations of induction dose of 110 mL/m2/min for 4 min and maintenance dose of 110 mL/m2/min for 2 min at 20 to 30 min intervals | 4 °C | 32 | cTnI | Cold blood with warm blood cardioplegic solution was the optimal approach for cyanotic patients. Modi P et al./2004 [59] |
| 4:1 dilution blood/STH I crystalloid cardioplegia | 4 °C | 36 | |||||
| Cold blood cardioplegia with terminal warm blood cardioplegic reperfusion | Induction and maintenance doses were the same during aorta cross-clamping, and then, the same dose was administered for 2 min at 37 °C immediately before unclamping | 4 °C and terminal reperfusion at 37 °C | 35 | ||||
| AV septal defects repair surgery | 0–1 year | Plegisol | Anterograde administrations of 20 mL/kg; 10 mL/kg every 20–30 min | 4 °C | 15 15 | CK-MB | Blood cardioplegia preserved myocardial function more effectively than crystalloid. Åmark Ket al/2005 [61] |
| 4:1 crystalloid/blood | |||||||
| Arterial switch operation | <30 days | Intermittent warm blood cardioplegia | 1–1.5 times the physiological coronary flow rate infused anterogradely for 1 min every 10 min | 35–36 °C | 188 | cTn-I | Better myocardial protection was achieved with repeated oxygenated WBC. Bojan M et al./2013 [65] |
| Custodiol | 30 mL/min for 7 min | 4 °C | 30 | ||||
| Arterial switch operation | <30 days | Blood cardioplegia | 5 mL/kg/min, initially for 3 min through ascending aorta and repeated after 20 min | 28 °C | 44 | cTn-I, CK-MB, BNP | Similar extent of myocardial damage and postoperative outcome. Giordano R et al./2016 [67] |
| Custodiol | 1 mL/min/g of heart weight | 5–8 °C | 50 | ||||
| Elective repair of ventricular septal defects and tetralogy of Fallot | ≤12 years | 4:1 dilution blood/STH I crystalloid cardioplegia | 30 mL/kg initially, followed by repeated doses of 15 mL/kg at 25 to 30 min intervals | 4 °C | 50 | cTn-I | del Nido solution exerted more beneficial effects in terms of preservation of cardiac structure, decrease in cTn-I release, and reduced morbidity. Talwar S et al./2017 [68] |
| del Nido cardioplegia solution | 20 mL/kg single dose was administered through the aortic root | 50 | |||||
| Corrective cardiac surgery | 3–69 months | Conventional blood cardioplegia | 30 mL/kg dose was repeated beyond an ischemic time of 90 min for del Nido solution. Additionally, the dose was repeated after 20 min for blood cardioplegia | 8–12 ° C | 30 | cTn-I, CK-MB | Both forms of cardioplegia were associated with similar time-related changes in cTn-I and CK-MB, thus suggesting similar myocardial protection. The advantages of del Nido solution involved decreased necessity for inotropic myocardial support and faster recovery of the heart rhythm. Panigrahi D et al./2018 [69] |
| del Nido cardioplegia solution | 30 | ||||||
| Tetralogy of Fallot | 0–18 years | Standard blood cardioplegia | Anterograde administrations of 20 mL/kg, every 20 min, repeated dose of 10 mL/kg | 8–12 °C | 26 | CK-MB | Similar troponin T release was noticed in both groups, thus suggesting myocardial protection was achieved after blood and del Nido cardioplegic solutions. Negi SL et al./2019 [73] |
| del Nido cardioplegia solution | 20 mL/kg and subsequent dose if cross-clamp time exceeded 75 min | 4–8 °C | 30 | ||||
| Surgical repair of congenital heart disease | 1–120 months | Blood cardioplegia | 30 mL/kg every 4 min | 4–6 °C | 40 | cTn-I | dN cardioplegia enables shorter aortic cross-clamp time and leads to a reduced level of cTn-I. Isildak FU et al./2021 [74] |
| del Nido cardioplegia solution | 20 mL/kg anterogradely, repeated dose for a procedure longer than 60–90 min | 40 | |||||
| Correction of tetralogy of Fallot | 8.3–16.4 months | Modified STH solution | Initially, 30 mL/kg anterogradely and every 40 min at 10 mL/kg | 30 °C | 27 | cTn-I | cTn-I levels were elevated; nevertheless, no significant difference was observed between groups. Gorjipour F et al./2017 [76] |
| del Nido cardioplegia solution | Initially, 20 mL/kg and subsequently, 10 mL/kg after 90 min | 32 |
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghimire, A.; Bisset, E.; Howlett, S. Ischemia and reperfusion injury following cardioplegic arrest is attenuated by age and testosterone deficiency in male but not female mice. Biol. Sex Differ. 2019, 10, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsao, P.C.; Shiau, Y.S.; Chiang, S.H.; Ho, H.C.; Liu, Y.L.; Chung, Y.F.; Lin, L.-J.; Chen, M.R.; Chang, J.K.; Soong, W.J.; et al. Development of a Newborn Screening Program for Critical Congenital Heart Disease (CCHD) in Taipei. PLoS ONE 2016, 11, e0153407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chambers, D.J.; Fallouh, H.B. Cardioplegia and cardiac surgery: Pharmacological arrest and cardioprotection during global ischemia and reperfusion. Pharmacol. Ther. 2010, 127, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Glöckner, A.; Ossmann, S.; Ginther, A.; Kang, J.; Borger, M.A.; Hoyer, A.; Dieterlen, M.T. Relevance and Recommendations for the Application of Cardioplegic Solutions in Cardiopulmonary Bypass Surgery in Pigs. Biomedicines 2021, 9, 1279. [Google Scholar] [CrossRef]
- Drury, N.E.; Horsburgh, A.; Bi, R.; Willetts, R.G.; Jones, T.J. Cardioplegia practice in paediatric cardiac surgery: A UK & Ireland survey. Perfusion 2019, 34, 125–129. [Google Scholar] [CrossRef]
- Yang, X.; An, N.; Zhong, C.; Guan, M.; Jiang, Y.; Li, X.; Zhang, H.; Wang, L.; Ruan, Y.; Gao, Y.; et al. Enhanced cardiomyocyte reactive oxygen species signaling promotes ibrutinib-induced atrial fibrillation. Redox Biol. 2020, 30, 101432. [Google Scholar] [CrossRef]
- Zhu, H.; Zhou, H. Novel Insight into the Role of Endoplasmic Reticulum Stress in the Pathogenesis of Myocardial Ischemia-Reperfusion Injury. Oxidative Med. Cell. Longev. 2021, 2021, 5529810. [Google Scholar] [CrossRef]
- Hausenloy, D.J.; Yellon, D.M. Myocardial ischemia-reperfusion injury: A neglected therapeutic target. J. Clin. Investig. 2013, 123, 92–100. [Google Scholar] [CrossRef] [Green Version]
- Dragasevic, N.; Jakovljevic, V.; Zivkovic, V.; Draginic, N.; Andjic, M.; Bolevich, S.; Jovic, S. The role of aldosterone inhibitors in cardiac ischemia-reperfusion injury. Can. J. Physiol. Pharmacol. 2021, 99, 18–29. [Google Scholar] [CrossRef]
- Rankovic, M.; Krivokapic, M.; Bradic, J.; Petkovic, A.; Zivkovic, V.; Sretenovic, J.; Jeremic, N.; Bolevich, S.; Kartashova, M.; Jeremic, J.; et al. New Insight Into the Cardioprotective Effects of Allium ursinum L. Extract Against Myocardial Ischemia-Reperfusion Injury. Front. Physiol. 2021, 12, 690696. [Google Scholar] [CrossRef]
- Magovern, J.A.; Pae, W.E., Jr.; Miller, C.A.; Waldhausen, J.A. The immature and the mature myocardium. Responses to multidose crystalloid cardioplegia. J. Thorac. Cardiovasc. Surg. 1988, 95, 618–624. [Google Scholar] [CrossRef]
- Ost’ádal, B.; Ost’ádalová, I.; Skárka, L.; Kolár, F.; Kopecký, J. Ischemic injury of the developing heart. Exp. Clin. Cardiol. 2002, 10, 93–98. [Google Scholar]
- Doenst, T.; Schlensak, C.; Beyersdorf, F. Cardioplegia in pediatric cardiac surgery: Do we believe in magic? Ann. Thorac. Surg. 2003, 75, 1668–1677. [Google Scholar] [CrossRef]
- Allen, B.S. Pediatric myocardial protection: Where do we stand? J. Thorac. Cardiovasc. Surg. 2004, 128, 11–13. [Google Scholar] [CrossRef] [Green Version]
- Carvajal, C.; Goyal, A.; Tadi, P. Cardioplegia; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Gerbode, F.; Melrose, D. The use of potassium arrest in open cardiac surgery. Am. J. Surg. 1958, 96, 221–227. [Google Scholar] [CrossRef]
- Effler, D.B.; Groves, L.K.; Sones, F.M., Jr.; Kolff, W.J. Elective cardiac arrest in open-heart surgery; report of three cases. Cleve. Clin. Q. 1956, 23, 105–114. [Google Scholar] [CrossRef]
- Francica, A.; Tonelli, F.; Rossetti, C.; Tropea, I.; Luciani, G.B.; Faggian, G.; Dobson, G.P.; Onorati, F. Cardioplegia between Evolution and Revolution: From Depolarized to Polarized Cardiac Arrest in Adult Cardiac Surgery. J. Clin. Med. 2021, 10, 4485. [Google Scholar] [CrossRef]
- Kirklin, J.W.; Conti, V.R.; Blackstone, E.H. Prevention of myocardial damage during cardiac operations. N. Engl. J. Med. 1979, 301, 135–141. [Google Scholar] [CrossRef]
- Mentzer, R.M., Jr.; Rahko, P.S.; Molina-Viamonte, V.; Canver, C.C.; Chopra, P.S.; Love, R.B.; Cook, T.D.; Hegge, J.O.; Lasley, R.D. Safety, tolerance, and efficacy of adenosine as an additive to blood cardioplegia in humans during coronary artery bypass surgery. Am. J. Cardiol. 1997, 79, 38–43. [Google Scholar] [CrossRef]
- Tyers, G.F.; Todd, G.J.; Niebauer, I.M.; Manley, N.J.; Waldhausen, J.A. The mechanism of myocardial damage following potassium citrate (Melrose) cardioplegia. Surgery 1975, 78, 45–53. [Google Scholar]
- Jynge, P.; Hearse, D.J.; Feuvray, D.; Mahalu, W.; Canković-Darracott, S.; O’Brien, K.; Braimbridge, M.V. The St. Thomas’ hospital cardioplegic solution: A characterization in two species. Scand. J. Thorac. Cardiovasc. Surg. Suppl. 1981, 30, 1–28. [Google Scholar] [PubMed]
- Ledingham, S.J.; Braimbridge, M.V.; Hearse, D.J. The St. Thomas’ Hospital cardioplegic solution. A comparison of the efficacy of two formulations. J. Thorac. Cardiovasc. Surg. 1987, 93, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Bretschneider, H.J. Myocardial protection. Thorac. Cardiovasc. Surg. 1980, 28, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Demmy, T.L.; Molina, J.E.; Ward, H.B.; Gorton, M.E.; Kouchoukos, N.T.; Schmaltz, R.A.; Shennib, H. Custodiol versus Plegisol: A phase 3 multicentre myocardial protection study. Int. J. Angiol. 2008, 17, 149–153. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, A.C.; Asopa, S.; Modi, A.; King, N. HTK versus multidose cardioplegias for myocardial protection in adult cardiac surgery: A meta-analysis. J. Card. Surg. 2021, 36, 1334–1343. [Google Scholar] [CrossRef]
- Dobson, G.P.; Faggian, G.; Onorati, F.; Vinten-Johansen, J. Hyperkalemic cardioplegia for adult and pediatric surgery: End of an era? Front. Physiol. 2013, 4, 228. [Google Scholar] [CrossRef] [Green Version]
- Sternbergh, W.C.; Brunsting, L.A.; Abd-Elfattah, A.S.; Wechsler, A.S. Basal metabolic energy requirements of polarized and depolarized arrest in rat heart. Am. J. Physiol. 1989, 256, H846–H851. [Google Scholar] [CrossRef]
- Tyers, G.F. Metabolic arrest of the ischemic heart. Ann. Thorac. Surg. 1975, 20, 91–94. [Google Scholar] [CrossRef]
- Oliveira, M.A.B.; Godoy, M.F.; Braile, D.M.; Lima-Oliveira, A.P.M. Polarizing cardioplegic solution: State of the art. Braz. J. Cardiovasc. Surg. 2005, 20, 69–74. [Google Scholar] [CrossRef] [Green Version]
- Habertheuer, A.; Kocher, A.; Laufer, G.; Andreas, M.; Szeto, W.Y.; Petzelbauer, P.; Ehrlich, M.; Wiedemann, D.L. Cardioprotection: A review of current practice in global ischemia and future translational perspective. Biomed. Res. Int. 2014, 2014, 325725. [Google Scholar] [CrossRef]
- Gundry, S.R.; Kirsh, M.M. A comparison of retrograde cardioplegia versus antegrade cardioplegia in the presence of coronary artery obstruction. Ann. Thorac. Surg. 1984, 38, 124–127. [Google Scholar] [CrossRef]
- Haan, C.; Lazar, H.L.; Bernard, S.; Rivers, S.; Zallnick, J.; Shemin, R.J. Superiority of retrograde cardioplegia after acute coronary occlusion. Ann. Thorac. Surg. 1991, 51, 408–412. [Google Scholar] [CrossRef]
- Shirai, T.; Rao, V.; Weisel, R.D.; Ikonomidis, J.S.; Hayashida, N.; Ivanov, J.; Carson, S.; Mohabeer, M.K.; Mickle, D.A.G. Antegrade and retrograde cardioplegia: Alternate or simultaneous? J. Thorac. Cardiovasc. Surg. 1996, 112, 787–796. [Google Scholar] [CrossRef] [Green Version]
- Rosenkranz, E.R.; Vinten-Johansen, J.; Buckberg, G.D.; Okamoto, F.; Edwards, H.; Bugyi, H. Benefits of normothermic induction of blood cardioplegia in energy-depleted hearts, with maintenance of arrest by multidose cold blood cardioplegic infusions. J. Thorac. Cardiovasc. Surg. 1982, 84, 667–677. [Google Scholar] [CrossRef]
- Ahmed, A.A.; Mahboobi, S.K. Warm Blood Cardioplegia; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Fan, Y.; Zhang, A.M.; Xiao, Y.B.; Lau, D.H.H.; Morgan, K.; Magni, F.; Harky, A. Warm versus cold cardioplegia for heart surgery: A meta-analysis. Eur. J. Cardiothorac. Surg. 2010, 37, 912–919. [Google Scholar] [CrossRef] [Green Version]
- Martin, T.D.; Craver, J.M.; Gott, J.P.; Weintraub, W.S.; Ramsay, J.; Mora, C.T.; Guyton, R.A. Prospective, randomized trial of retrograde warm blood cardioplegia: Myocardial benefit and neurologic threat. Ann. Thorac. Surg. 1994, 57, 298–304. [Google Scholar] [CrossRef]
- Buckberg, G.D. Normothermic blood cardioplegia. Alternative or adjunct? J. Thorac. Cardiovasc. Surg. 1994, 107, 860–867. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, Y.; Ohtani, M.; Sawa, Y.; Hiraishi, T.; Akedo, H.; Kobayashi, Y.; Nakamura, T.; Matsuda, H. Initial, continuous and intermittent bolus cardioplegia administration: Efficacy of potassium-chloride and magnesium-sulfate as minimal additives for minimally-diluted blood cardioplegia. J. Cardiovasc. Surg. 2005, 46, 61–68. [Google Scholar]
- Lazar, H.L.; Rivers, S.; Cambrils, M.; Bernard, S.; Shemin, R.J. Continuous versus intermittent cardioplegia in the presence of a coronary occlusion. Ann. Thorac. Surg. 1991, 52, 913–917. [Google Scholar] [CrossRef]
- Gunnes, S.; Jynge, P. Fundamentals of the Past: Cardioplegia: The First Period Revisited. In New Solutions for the Heart; Podesser, B.K., Chambers, D.J., Eds.; Springer: Wien, Austria, 2011; pp. 15–40. [Google Scholar]
- Singh, S.; De, D.; Spadaccio, C.; Berry, C.; Al-Attar, N. An overview of different methods of myocardial protection currently employed peri-transplantation. Vessel. Plus 2017, 1, 213–229. [Google Scholar] [CrossRef]
- Sanetra, K.; Pawlak, I.; Cisowski, M. Del Nido cardioplegia–what is the current evidence? Kardiochir Torakochirurgia Pol. 2018, 15, 114–118. [Google Scholar] [CrossRef] [PubMed]
- El-Morsy, G.Z.; Abdullah, H.M.; Abo-Haded, H.M.; Elgamal, M.A.F.; El-Deep, A.M. Does type of cardioplegia affect myocardial and cerebral outcome in pediatric open cardiac surgeries? Ain-Shams J. Anesthesiol. 2014, 7, 242–249. [Google Scholar] [CrossRef]
- Chen, Y.; Shi, J.; Xia, T.C.; Xu, R.; He, X.; Xia, Y. Preservation Solutions for Kidney Transplantation: History, Advances and Mechanisms. Cell Transplant. 2019, 28, 1472–1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aarsaether, E.; Stenberg, T.A.; Jakobsen, Ø.; Busund, R. Mechanoenergetic function and troponin T release following cardioplegic arrest induced by St Thomas’ and histidine-tryptophan-ketoglutarate cardioplegia--an experimental comparative study in pigs. Interact. Cardiovasc. Thorac. Surg. 2009, 9, 635–639. [Google Scholar] [CrossRef]
- Rosenkranz, E.R.; Buckberg, G.D. Myocardial protection during surgical coronary reperfusion. J. Am. Coll. Cardiol. 1983, 1, 1235–1246. [Google Scholar] [CrossRef] [Green Version]
- Follette, D.M.; Mulder, D.G.; Maloney, J.V.; Buckberg, G. Advantages of blood cardioplegia over continuous coronary perfusion or intermittent ischemia. Experimental and clinical study. J. Thorac. Cardiovasc. Surg. 1978, 76, 604–619. [Google Scholar] [CrossRef]
- Shiroishi, M.S. Myocardial protection: The rebirth of potassium-based cardioplegia. Tex. Heart Inst. J. 1999, 26, 71–86. [Google Scholar]
- Øvrum, E.; Tangen, G.; Tølløfsrud, S.; Øystese, R.; Ringdal, M.A.; Istad, R. Cold blood versus cold crystalloid cardioplegia: A prospective randomised study of 345 aortic valve patients. Eur. J. Cardiothorac. Surg. 2010, 38, 745–749. [Google Scholar] [CrossRef]
- Kim, K.; Ball, C.; Grady, P.; Mick, S. Use of del Nido Cardioplegia for Adult Cardiac Surgery at the Cleveland Clinic: Perfusion Implications. J. Extra Corpor. Technol. 2014, 46, 317–323. [Google Scholar]
- Matte, G.S.; del Nido, P.J. History and use of del Nido cardioplegia solution at Boston Children’s Hospital. J. Extra Corpor. Technol. 2012, 44, 98–103, Erratum in J. Extra Corpor. Technol. 2013, 45, 262. [Google Scholar]
- Young, J.N.; Choy, I.O.; Silva, N.K.; Obayashi, D.Y.; Barkan, H.E. Antegrade cold blood cardioplegia is not demonstrably advantageous over cold crystalloid cardioplegia in surgery for congenital heart disease. J. Thorac. Cardiovasc. Surg. 1997, 114, 1002–1009. [Google Scholar] [CrossRef] [Green Version]
- Imura, H.; Caputo, M.; Parry, A.; Pawade, A.; Angelini, G.D.; Suleiman, M.S. Age-dependent and hypoxia-related differences in myocardial protection during pediatric open heart surgery. Circulation 2001, 103, 1551–1556. [Google Scholar] [CrossRef]
- Cyran, S.E.; Phillips, J.; Ditty, S.; Baylen, B.G.; Cheung, J.; LaNoue, K. Developmental differences in cardiac myocyte calcium homeostasis after steady-state potassium depolarization: Mechanisms and implications for cardioplegia. J. Pediatr. 1993, 122, S77–S83. [Google Scholar] [CrossRef]
- Wittnich, C.; Peniston, C.; Ianuzzo, D.; Abel, J.G.; Salerno, T.A. Relative vulnerability of neonatal and adult hearts to ischemic injury. Circulation 1987, 76, V156–V160. [Google Scholar]
- Caputo, M.; Modi, P.; Imura, H.; Pawade, A.; Parry, A.J.; Suleiman, M.S.; Angelini, G.D. Cold blood versus cold crystalloid cardioplegia for repair of ventricular septal defects in pediatric heart surgery: A randomized controlled trial. Ann. Thorac. Surg. 2002, 74, 530–535. [Google Scholar] [CrossRef]
- Modi, P.; Suleiman, M.S.; Reeves, B.; Pawade, A.; Parry, A.J.; Angelini, G.D.; Caputo, M. Myocardial metabolic changes during pediatric cardiac surgery: A randomized study of 3 cardioplegic techniques. J. Thorac. Cardiovasc. Surg. 2004, 128, 67–75. [Google Scholar] [CrossRef] [Green Version]
- Hammon, J.W., Jr.; Graham, T.P., Jr.; Boucek, R.J., Jr.; Parrish, M.D.; Merrill, W.H.; Bender, H.W., Jr. Myocardial adenosine triphosphate content as a measure of metabolic and functional myocardial protection in children undergoing cardiac operation. Ann. Thorac. Surg. 1987, 44, 467–470. [Google Scholar] [CrossRef]
- Amark, K.; Berggren, H.; Björk, K.; Ekroth, A.; Ekroth, R.; Nilsson, K.; Sunnegårdh, J. Blood cardioplegia provides superior protection in infant cardiac surgery. Ann. Thorac. Surg. 2005, 80, 989–994. [Google Scholar] [CrossRef]
- Sinha, P.; Zurakowski, D.; Jonas, R.A. Comparison of two cardioplegia solutions using thermodilution cardiac output in neonates and infants. Ann. Thorac. Surg. 2008, 86, 1613–1619. [Google Scholar] [CrossRef]
- Charette, K.; Gerrah, R.; Quaegebeur, J.; Chen, J.; Riley, D.; Mongero, L.; Corda, R.; Bacha, E. Single dose myocardial protection technique utilizing del Nido cardioplegia solution during congenital heart surgery procedures. Perfusion 2012, 27, 98–103. [Google Scholar] [CrossRef]
- Durandy, Y.D.; Younes, M.; Mahut, B. Pediatric warm open heart surgery and prolonged cross-clamp time. Ann. Thorac. Surg. 2008, 86, 1941–1947. [Google Scholar] [CrossRef] [PubMed]
- Bojan, M.; Peperstraete, H.; Lilot, M.; Tourneur, L.; Vouhé, P.; Pouard, P. Cold histidine-tryptophan-ketoglutarate solution and repeated oxygenated warm blood cardioplegia in neonates with arterial switch operation. Ann. Thorac. Surg. 2013, 95, 1390–1396. [Google Scholar] [CrossRef] [PubMed]
- Qulisy, E.; Fakiha, A.; Debis, R.; Jamjoom, A.A.; Elassalac, A.A.; Al-Radi, O. Custodiol versus blood cardioplegia in pediatric cardiac surgery, two-center study. J. Egypt. Society Cardio-Thoracic Surg. 2016, 24, 38–42. [Google Scholar] [CrossRef] [Green Version]
- Giordano, R.; Arcieri, L.; Cantinotti, M.; Pak, V.; Poli, V.; Maizza, A.; Melo, M.; Assanta, N.; Moschetti, R.; Murzi, B. Custodiol Solution and Cold Blood Cardioplegia in Arterial Switch Operation: Retrospective Analysis in a Single Center. Thorac. Cardiovasc. Surg. 2016, 64, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Talwar, S.; Bhoje, A.; Sreenivas, V.; Makhija, N.; Aarav, S.; Choudhary, S.K.; Airan, B. Comparison of del Nido and St Thomas Cardioplegia Solutions in Pediatric Patients: A Prospective Randomized Clinical Trial. Semin. Thorac. Cardiovasc. Surg. 2017, 29, 366–374. [Google Scholar] [CrossRef]
- Panigrahi, D.; Roychowdhury, S.; Guhabiswas, R. Myocardial protection following del Nido cardioplegia in pediatric cardiac surgery. Asian Cardiovasc. Thorac. Ann. 2018, 26, 267–272. [Google Scholar] [CrossRef]
- O’Brien, J.D.; Howlett, S.E.; Burton, H.J.; O’Blenes, S.B.; Litz, D.S.; Friesen, C.L. Pediatric cardioplegia strategy results in enhanced calcium metabolism and lower serum troponin T. Ann. Thorac. Surg. 2009, 87, 1517–1523. [Google Scholar] [CrossRef]
- Snabaitis, A.K.; Shattock, M.J.; Chambers, D.J. Comparison of polarized and depolarized arrest in the isolated rat heart for long-term preservation. Circulation 1997, 96, 3148–3156. [Google Scholar] [CrossRef]
- Yang, Y.J. Protection of immature myocardium by the addition of mannitol to crystalloid cardioplegic solution. J. Formos. Med. Assoc. 1991, 90, 24–30. [Google Scholar]
- Negi, S.L.; Mandal, B.; Singh, R.S.; Puri, G.D. Myocardial protection and clinical outcomes in Tetralogy of Fallot patients undergoing intracardiac repair: A randomized study of two cardioplegic techniques. Perfusion 2019, 34, 495–502, Erratum in Perfusion 2021, 36, 648. [Google Scholar] [CrossRef]
- Isildak, F.U.; Yavuz, Y. Comparison of Del Nido and Blood Cardioplegia in Pediatric Patients Undergoing Surgical Repair for Congenital Heart Disease. Pediatr. Cardiol. 2021, 42, 1388–1393. [Google Scholar] [CrossRef]
- Mohammed, S.; Menon, S.; Gadhinglajkar, S.V.; Baruah, S.D.; Ramanan, S.V.; Gopalakrishnan, K.A.; Suneel, P.R.; Dharan, B.S. Clinical outcomes of del nido cardioplegia and st thomas blood cardioplegia in neonatal congenital heart surgery. Ann. Card. Anaesth. 2022, 25, 54–60. [Google Scholar] [CrossRef]
- Gorjipour, F.; Dehaki, M.G.; Totonchi, Z.; Hajimiresmaiel, S.J.; Azarfarin, R.; Pazoki-Toroudi, H.; Mahdavi, M.; Korbi, M.; Dehaki, M.G.; Soltani, B.; et al. Inflammatory cytokine response and cardiac troponin I changes in cardiopulmonary bypass using two cardioplegia solutions; del Nido and modified St. Thomas’: A randomized controlled trial. Perfusion 2017, 32, 394–402. [Google Scholar] [CrossRef]
- Stammers, A.H.; Tesdahl, E.A. Does the Type of Cardioplegic Technique Influence Hemodilution and Transfusion Requirements in Adult Patients Undergoing Cardiac Surgery? J. Extra Corpor. Technol. 2017, 49, 231–240. [Google Scholar]
- Günday, M.; Bingöl, H. Is crystalloid cardioplegia a strong predictor of intra-operative hemodilution? J. Cardiothorac. Surg. 2014, 9, 23. [Google Scholar] [CrossRef]

| CRYSTALLOID SOLUTIONS | ||||||
|---|---|---|---|---|---|---|
| Extracellular Solutions | Intracellular Solutions | |||||
| Components (mmol/L) | STH 1 | Plegisol (STH 2) | Celsior | Custodiol | University of Wisconsin | Eurocollins |
| Na+ | 144.00 | 110.00 | 100.00 | 15.00 | 25.00 | 10.00 |
| K+ | 20.00 | 16.00 | 15.00 | 9.00 | 120.0 | 115.00 |
| Mg2+ | 16.00 | 16.00 | 13.00 | 4.00 | 5.00 | / |
| Ca2+ | 2.40 | 1.20 | 0.25 | 0.015 | / | / |
| Procain hidrochloryde | 1.00 | / | / | / | / | / |
| Bicarbonate | / | 10.00 | / | / | / | 10.00 |
| Histidine | / | / | 30.00 | 198.00 | / | / |
| Phosphate buffer | / | / | / | / | 25.00 | 100.00 |
| Mannitol | / | / | 60.00 | 30.00 | / | 60.00 |
| Glucose | / | / | / | / | / | 180.00 |
| Raffinose | / | / | 30.00 | / | 30.00 | / |
| Typtophan | / | / | / | 2.00 | / | / |
| Ketoglutarate | / | / | / | 1.00 | / | / |
| Adenosine | / | / | / | / | 5.00 | / |
| Glutamate | / | / | 20.00 | / | / | / |
| Glutathione | / | / | 3.00 | / | 3.00 | / |
| Allopurinol | / | / | / | / | 1.00 | / |
| Lactobionate | / | / | 80.00 | / | 100.00 | 80.00 |
| Osmolarity | 320 | 300 | 320 | 300 | 330 | 375 |
| Components | Del Nido Solution |
|---|---|
| KCl | 26 mEq |
| Bicarbonates | 13 mL |
| Citrate-phosphate-dextrose | / |
| Mannitol 20% | 16 mL |
| Lidocaine 2% | 6.50 mL |
| Tromethamine 0.3 m | / |
| Crystalloid:blood ratio | 4:1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bradić, J.; Andjić, M.; Novaković, J.; Jeremić, N.; Jakovljević, V. Cardioplegia in Open Heart Surgery: Age Matters. J. Clin. Med. 2023, 12, 1698. https://doi.org/10.3390/jcm12041698
Bradić J, Andjić M, Novaković J, Jeremić N, Jakovljević V. Cardioplegia in Open Heart Surgery: Age Matters. Journal of Clinical Medicine. 2023; 12(4):1698. https://doi.org/10.3390/jcm12041698
Chicago/Turabian StyleBradić, Jovana, Marijana Andjić, Jovana Novaković, Nevena Jeremić, and Vladimir Jakovljević. 2023. "Cardioplegia in Open Heart Surgery: Age Matters" Journal of Clinical Medicine 12, no. 4: 1698. https://doi.org/10.3390/jcm12041698
APA StyleBradić, J., Andjić, M., Novaković, J., Jeremić, N., & Jakovljević, V. (2023). Cardioplegia in Open Heart Surgery: Age Matters. Journal of Clinical Medicine, 12(4), 1698. https://doi.org/10.3390/jcm12041698






