Clinical and Functional Results of Cementless Unicompartmental Knee Arthroplasty with a Minimum Follow Up of 5 Years—A Consecutive Cohort of 201 Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Clinical Outcome
2.3. Survival
2.4. Statistics
3. Results
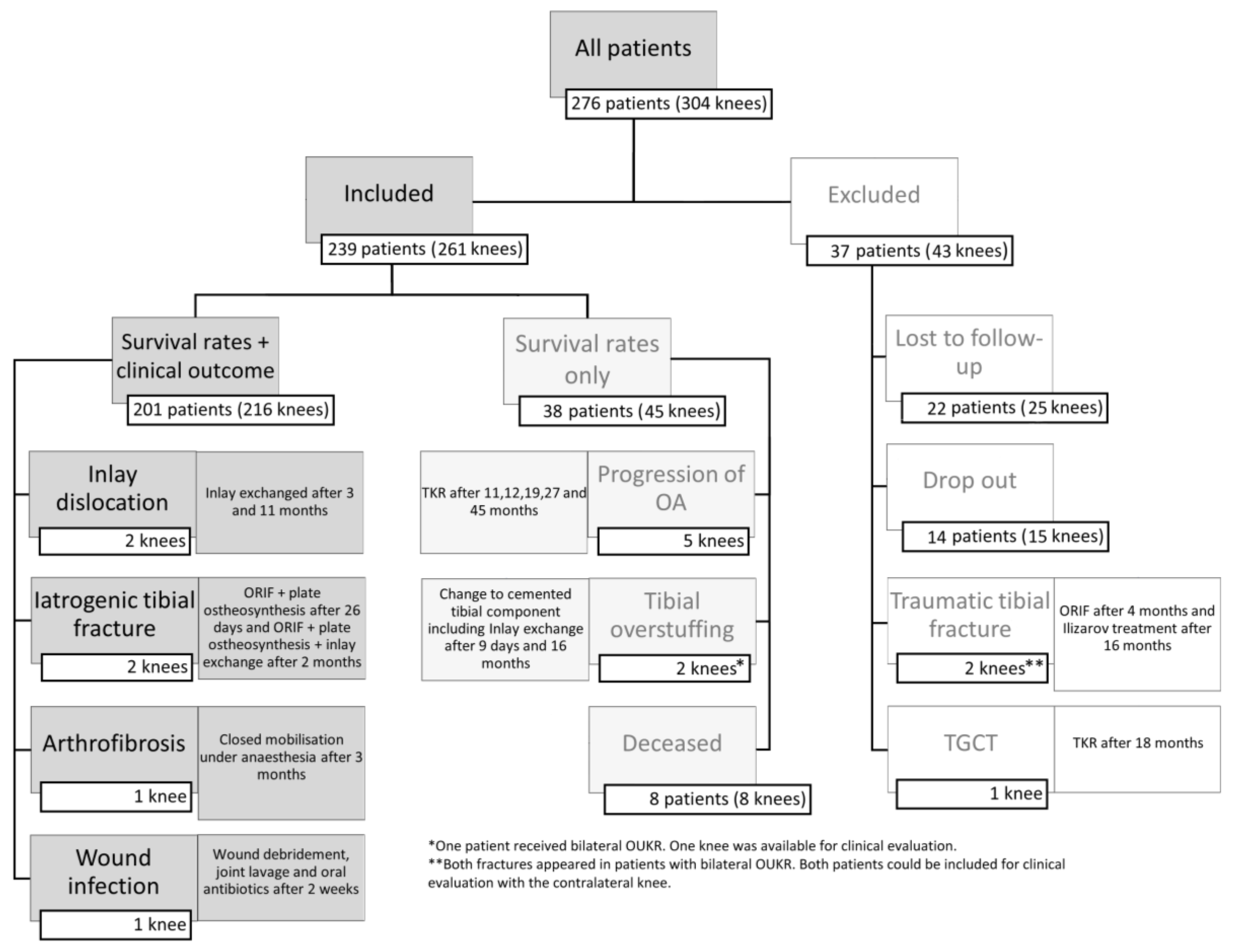
3.1. Patient Cohort
3.2. Revision Surgery and Reoperation
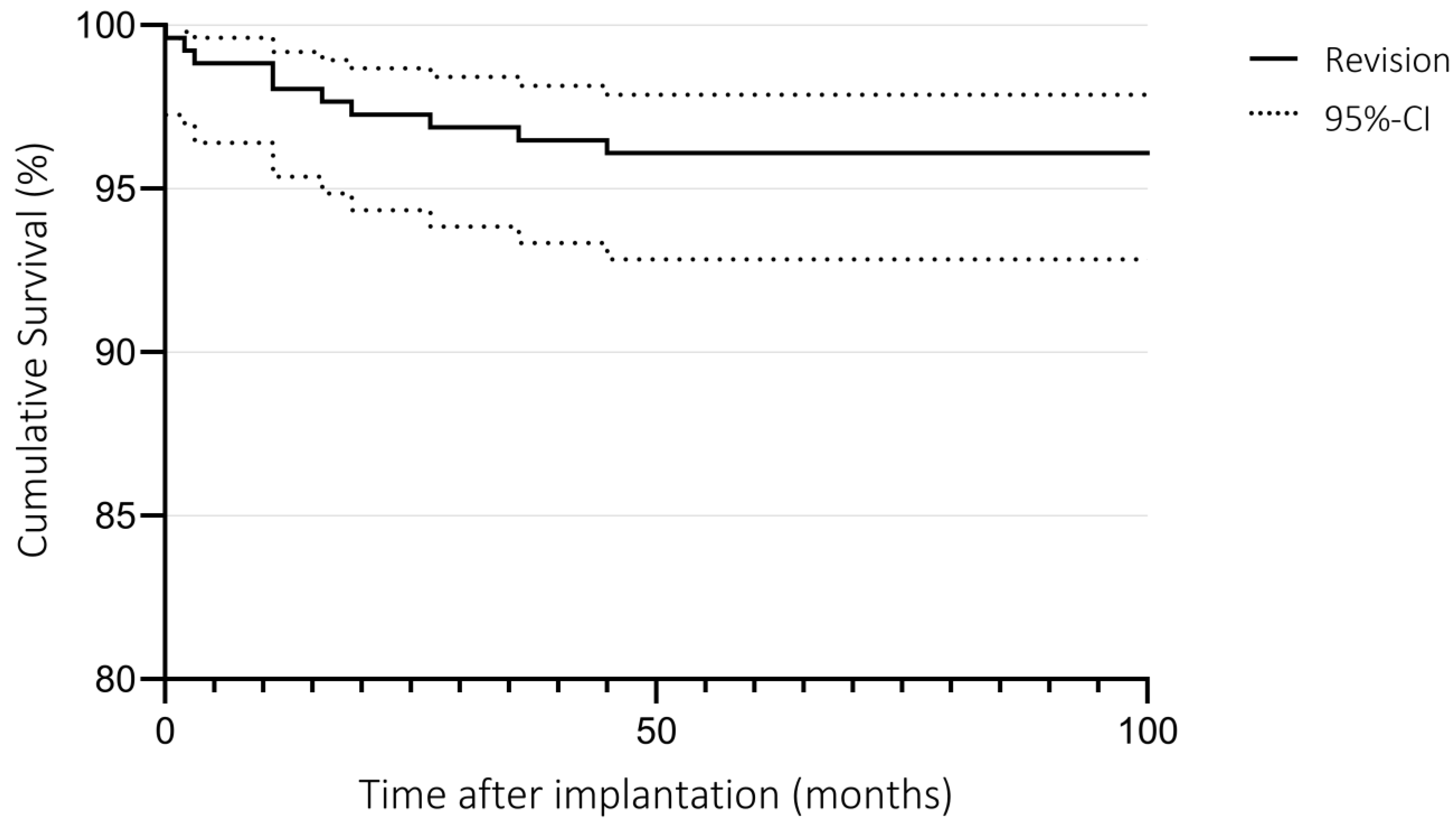
3.3. Survival
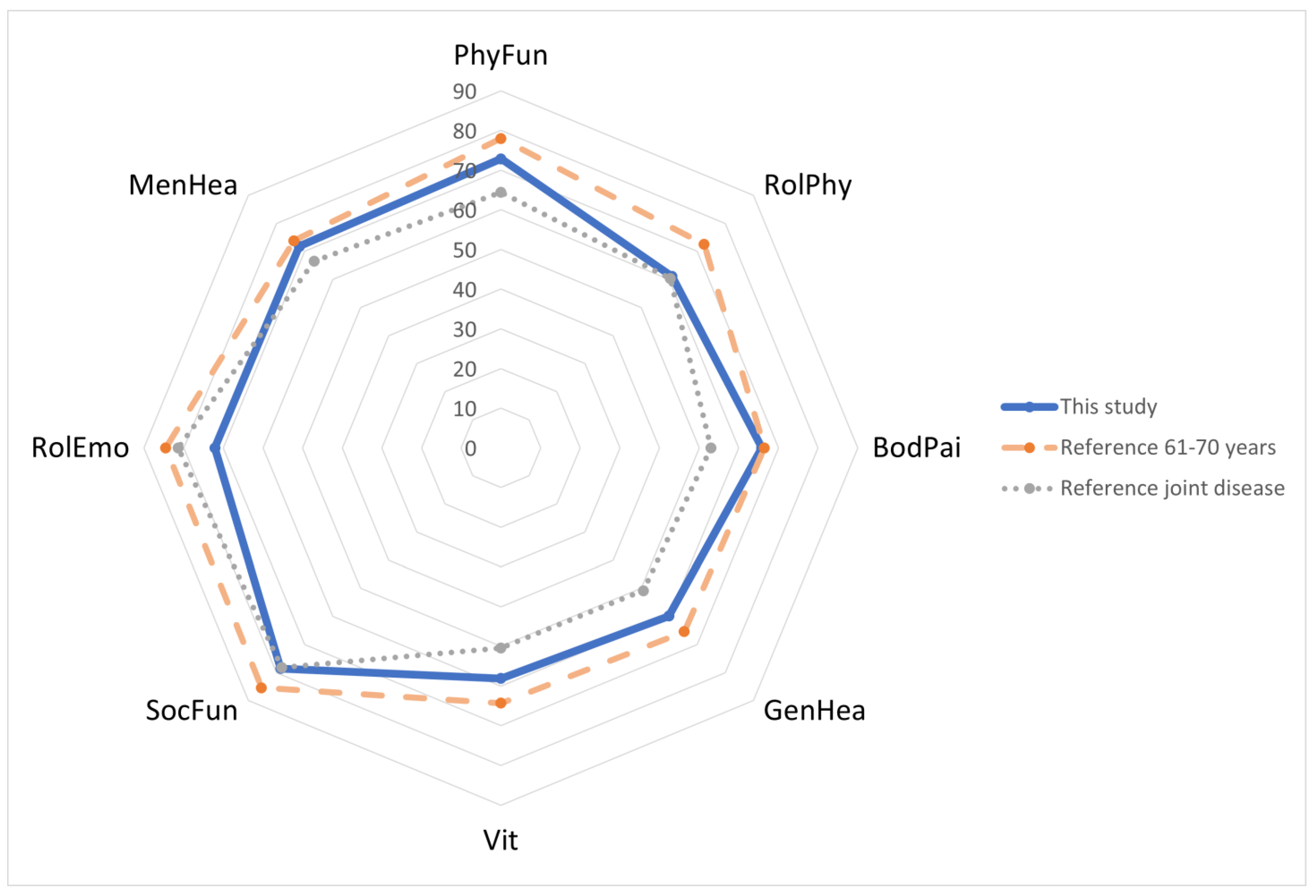
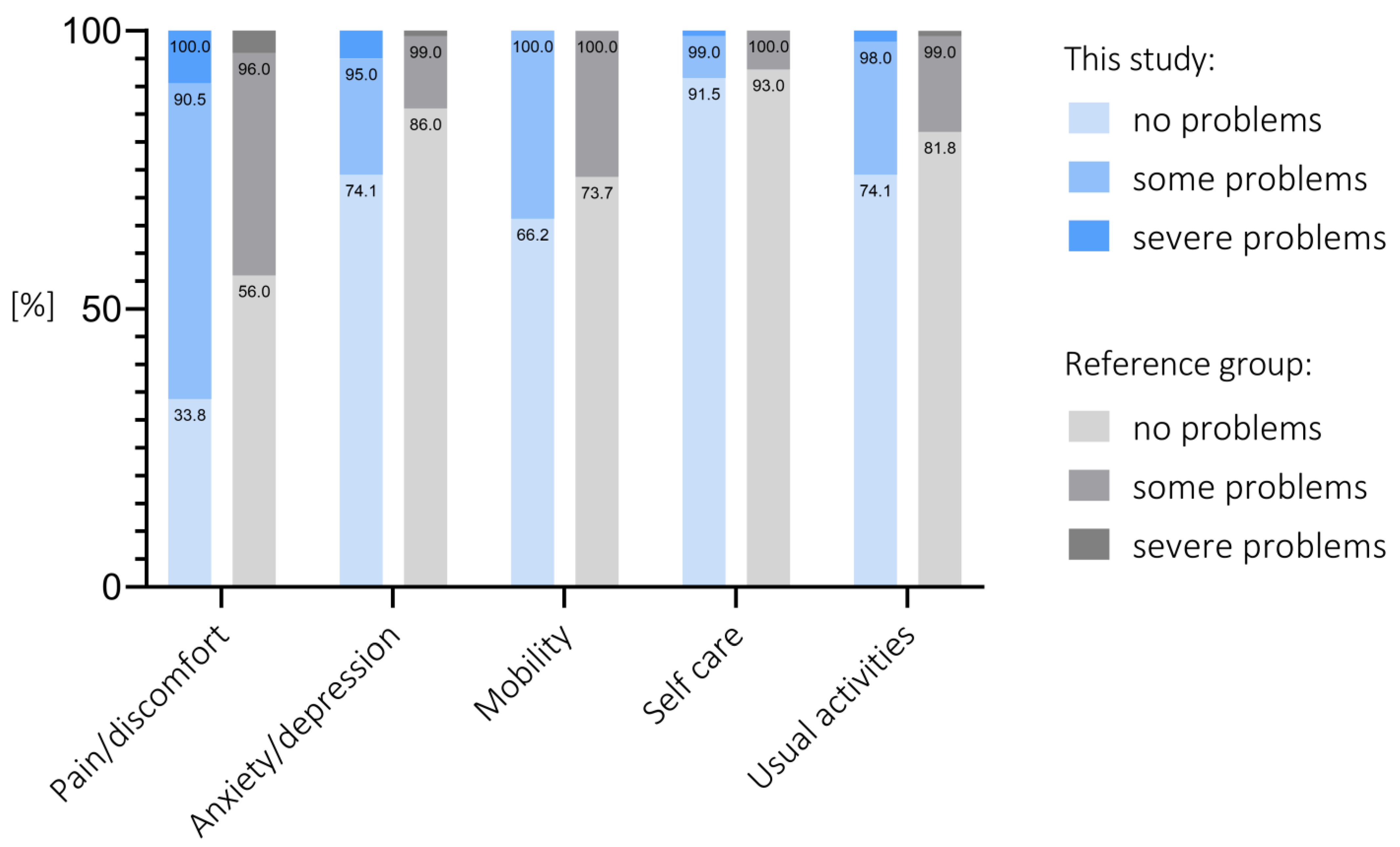
3.4. Functional Scores
| Score | Spalte2 | PreOp | Last Follow-Up | Δ | p-Value |
|---|---|---|---|---|---|
| OKS | Mean | 31.75 | 40.74 | 8.97 | |
| SD | 7.34 | 7.49 | 11.88 | <0.001 | |
| IQR | 26–37 | 37–46 | 2–18 | ||
| AKSS-O | Mean | 50.83 | 82.83 | 31.90 | |
| SD | 12.74 | 16.53 | 18.86 | <0.001 | |
| IQR | 41–59 | 75–95 | 21–46 | ||
| AKSS-F | Mean | 61.09 | 83.73 | 22.46 | |
| SD | 20.26 | 20.99 | 24.17 | <0.001 | |
| IQR | 50–80 | 75–100 | 10–40 | ||
| FFbH-OA | Mean | 65.50 | 82.42 | 16.87 | |
| SD | 17.05 | 19.02 | 19.29 | <0.001 | |
| IQR | 53–78 | 71.25–97 | 6–28 | ||
| UCLA | Mean | 3.28 | 6.33 | 3.14 | |
| SD | 1.84 | 1.77 | 2.37 | <0.001 | |
| IQR | 2–4 | 6–7 | 2–5 | ||
| ROM | Mean | 121.06 | 127.38 | 6.77 | |
| SD | 14.22 | 12.71 | 14.44 | <0.001 | |
| IQR | 111–130 | 120–135 | 0–15 | ||
| Pain | Mean | 7.17 | 1.99 | −5.2 | |
| SD | 1.90 | 2.51 | 2.92 | <0.001 | |
| IQR | 6–9 | 0–3 | −7–(−3) | ||
| FJS | Mean | - | 68.24 | - | |
| SD | - | 30.15 | - | ||
| IQR | - | 45.8–95.8 | - |
3.5. Satisfaction
3.6. BMI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cui, A.; Li, H.; Wang, D.; Zhong, J.; Chen, Y.; Lu, H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. Eclinicalmedicine 2020, 29–30, 100587. [Google Scholar] [CrossRef] [PubMed]
- Long, H.; Liu, Q.; Yin, H.; Wang, K.; Diao, N.; Zhang, Y.; Lin, J.; Guo, A. Prevalence Trends of Site-Specific Osteoarthritis from 1990 to 2019: Findings From the Global Burden of Disease Study 2019. Arthritis Rheumatol. 2022, 74, 1172–1183. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, J.; Rabenberg, M.; Scheidt-Nave, C. Prävalenz ausgewählter muskuloskelettaler Erkrankungen. Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 678–686. [Google Scholar] [CrossRef]
- Stoddart, J.C.; Dandridge, O.; Garner, A.; Cobb, J.; Van Arkel, R.J. The compartmental distribution of knee osteoarthritis—A systematic review and meta-analysis. Osteoarthr. Cartil. 2021, 29, 445–455. [Google Scholar] [CrossRef]
- Ahlback, S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol. Diagn. 1968, S277, 7–72. [Google Scholar]
- The German Arthroplasty Registry—Annual Report 2020. Available online: https://www.eprd.de/fileadmin/user_upload/Dateien/Publikationen/Berichte/Jahresbericht2020-Web_2020-12-11_F.pdf (accessed on 10 June 2022).
- Panzram, B.; Bertlich, I.; Reiner, T.; Walker, T.; Hagmann, S.; Gotterbarm, T. Cementless unicompartmental knee replacement allows early return to normal activity. BMC Musculoskelet Disord 2018, 19, 18. [Google Scholar] [CrossRef]
- Witjes, S.; Gouttebarge, V.; Kuijer, P.P.; van Geenen, R.C.; Poolman, R.W.; Kerkhoffs, G.M. Return to Sports and Physical Activity After Total and Unicondylar Knee Arthroplasty: A Systematic Review and Meta-Analysis. Sports Med. 2016, 46, 269–292. [Google Scholar] [CrossRef]
- Slover, J.; Espehaug, B.; Havelin, L.I.; Engesaeter, L.B.; Furnes, O.; Tomek, I.; Tosteson, A. Cost-effectiveness of unicompartmental and total knee arthroplasty in elderly low-demand patients. A Markov decision analysis. J. Bone Jt. Surg. Am. 2006, 88, 2348–2355. [Google Scholar] [CrossRef]
- Willis-Owen, C.A.; Brust, K.; Alsop, H.; Miraldo, M.; Cobb, J.P. Unicondylar knee arthroplasty in the UK National Health Service: An analysis of candidacy, outcome and cost efficacy. Knee 2009, 16, 473–478. [Google Scholar] [CrossRef]
- Zimmer, B. Partial Knee Health Economics Flyer. 2020. Available online: https://www.zimmerbiomet.com/content/dam/zb-corporate/en/products/specialties/knee/oxford-partial-knee/0060.1-GLBL-en%20Partial%20Knee%20health%20economics%20flyer.pdf (accessed on 15 August 2022).
- Brown, N.M.; Sheth, N.P.; Davis, K.; Berend, M.E.; Lombardi, A.V.; Berend, K.R.; Della Valle, C.J. Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: A multicenter analysis. J. Arthroplast. 2012, S27 (Suppl. S8), 86–90. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Miller, S.; Hadden, W.; Johnston, L.; Wang, W.; Arnold, G.; Abboud, R. Comparison of gait kinematics in total and unicondylar knee replacement surgery. Ann. R. Coll. Surg. Engl. 2019, 101, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Kleeblad, L.J.; Van Der List, J.P.; Zuiderbaan, H.A.; Pearle, A.D. Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: A systematic review. Knee Surg. Sport. Traumatol. Arthrosc. 2018, 26, 1811–1822. [Google Scholar] [CrossRef]
- Soohoo, N.F.; Sharifi, H.; Kominski, G.; Lieberman, J.R. Cost-effectiveness analysis of unicompartmental knee arthroplasty as an alternative to total knee arthroplasty for unicompartmental osteoarthritis. J. Bone Joint Surg. Am. 2006, 88, 1975–1982. [Google Scholar] [PubMed]
- Shankar, S.; Tetreault, M.W.; Jegier, B.J.; Andersson, G.B.; Della Valle, C.J. A cost comparison of unicompartmental and total knee arthroplasty. Knee 2016, 23, 1016–1019. [Google Scholar] [CrossRef]
- Di Martino, A.; Bordini, B.; Barile, F.; Ancarani, C.; Digennaro, V.; Faldini, C. Unicompartmental knee arthroplasty has higher revisions than total knee arthroplasty at long term follow-up: A registry study on 6453 prostheses. Knee Surg. Sport. Traumatol. Arthrosc. 2021, 29, 3323–3329. [Google Scholar] [CrossRef] [PubMed]
- Liddle, A.D.; Pandit, H.; Judge, A.; Murray, D.W. Patient-reported outcomes after total and unicompartmental knee arthroplasty: A study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Jt. J. 2015, 97-B, 793–801. [Google Scholar] [CrossRef]
- Wilson, H.A.; Middleton, R.; Abram, S.G.F.; Smith, S.; Alvand, A.; Jackson, W.F.; Bottomley, N.; Hopewell, S.; Price, A.J. Patient relevant outcomes of unicompartmental versus total knee replacement: Systematic review and meta-analysis. BMJ 2019, 364, l352. [Google Scholar] [CrossRef]
- Mohammad, H.R.; Judge, A.; Murray, D. A matched comparison of cementless unicompartmental and total knee replacement outcomes based on the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Acta Orthop. 2022, 93, 478–487. [Google Scholar] [CrossRef]
- The German Arthroplasty Registry—Annual Report 2021. Available online: https://www.researchgate.net/publication/351515573_The_German_Arthroplasty_Registry_-_Annual_Report_2020 (accessed on 15 August 2022).
- Migliorini, F.; Tingart, M.; Niewiera, M.; Rath, B.; Eschweiler, J. Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 947–955. [Google Scholar] [CrossRef]
- Chawla, H.; van der List, J.P.; Christ, A.B.; Sobrero, M.R.; Zuiderbaan, H.A.; Pearle, A.D. Annual revision rates of partial versus total knee arthroplasty: A comparative meta-analysis. Knee 2017, 24, 179–190. [Google Scholar] [CrossRef] [PubMed]
- The New Zealand Orthopaedic Association. The New Zealand Joint Registry 22 Year Report. 2021. Available online: https://www.nzoa.org.nz/sites/default/files/NZJR_22_Year_Report_Final.pdf (accessed on 15 August 2022).
- Mikkelsen, M.; Price, A.; Pedersen, A.B.; Gromov, K.; Troelsen, A. Optimized medial unicompartmental knee arthroplasty outcome: Learning from 20 years of propensity score matched registry data. Acta Orthop. 2022, 93, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.; Rahman, A.; Jenkins, C.; Mohammad, H.; Barker, K.; Dodd, C.; Jackson, W.; Price, A.; Mellon, S.; Murray, D. Comparison of five-year clinical outcomes of 524 cemented and cementless medial unicompartmental knee replacements. Knee 2022, 34, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Campi, S.; Pandit, H.G.; Dodd, C.A.F.; Murray, D.W. Cementless fixation in medial unicompartmental knee arthroplasty: A systematic review. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Liddle, A.D.; Pandit, H.; O’Brien, S.; Doran, E.; Penny, I.D.; Hooper, G.J.; Burn, P.J.; Dodd, C.A.; Beverland, D.E.; Maxwell, A.R.; et al. Cementless fixation in Oxford unicompartmental knee replacement: A multicentre study of 1000 knees. Bone Jt. J. 2013, 95-B, 181–187. [Google Scholar] [CrossRef]
- Campi, S.; Pandit, H.; Hooper, G.; Snell, D.; Jenkins, C.; Dodd, C.A.F.; Maxwell, R.; Murray, D.W. Ten-year survival and seven-year functional results of cementless Oxford unicompartmental knee replacement: A prospective consecutive series of our first 1000 cases. Knee 2018, 25, 1231–1237. [Google Scholar] [CrossRef]
- Pandit, H.; Jenkins, C.; Beard, D.J.; Gallagher, J.; Price, A.J.; Dodd, C.A.; Goodfellow, J.W.; Murray, D.W. Cementless Oxford unicompartmental knee replacement shows reduced radiolucency at one year. J. Bone Jt. Surg. Br. 2009, 91, 185–189. [Google Scholar] [CrossRef]
- Mohammad, H.R.; Kennedy, J.A.; Mellon, S.J.; Judge, A.; Dodd, C.A.; Murray, D.W. Ten-year clinical and radiographic results of 1000 cementless Oxford unicompartmental knee replacements. Knee Surg. Sport. Traumatol. Arthrosc. 2020, 28, 1479–1487. [Google Scholar] [CrossRef]
- Panzram, B.; Mandery, M.; Reiner, T.; Gotterbarm, T.; Schiltenwolf, M.; Merle, C. Cementless Oxford Medial Unicompartmental Knee Replacement-Clinical and Radiological Results of 228 Knees with a Minimum 2-Year Follow-Up. J. Clin. Med. 2020, 9, 1476. [Google Scholar] [CrossRef]
- Pandit, H.; Jenkins, C.; Barker, K.; Dodd, C.A.; Murray, D.W. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J. Bone Jt. Surg. Br. 2006, 88, 54–60. [Google Scholar] [CrossRef]
- Pandit, H.; Jenkins, C.; Gill, H.S.; Smith, G.; Price, A.J.; Dodd, C.A.; Murray, D.W. Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. J. Bone Jt. Surg. Br. 2011, 93, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.F.; Pickard, A.; Shaw, J. General population normative data for the EQ-5D-3L in the five largest European economies. Eur. J. Health Econ. 2021, 22, 1467–1475. [Google Scholar] [CrossRef] [PubMed]
- Ellert, U.; Kurth, B.M. Gesundheitsbezogene Lebensqualität bei Erwachsenen in Deutschland. Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Bullinger, M.; Kirchberger, I.; Ware, J. SF-36 Fragebogen zum Gesundheitszustand; Hogrefe-Verlag GmbH & Co KG: Göttingen, Germany, 1998. [Google Scholar]
- Tripathy, S.K.; Varghese, P.; Srinivasan, A.; Goyal, T.; Purudappa, P.P.; Sen, R.K.; Chandrappa, M.H. Joint awareness after unicompartmental knee arthroplasty and total knee arthroplasty: A systematic review and meta-analysis of cohort studies. Knee Surg. Sport. Traumatol. Arthrosc. 2021, 29, 3478–3487. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.K.; Lin, W.; Yang, G.M.; Lu, J.F.; Wang, F. Joint Awareness after Unicompartmental Knee Arthroplasty Evaluated with the Forgotten Joint Score. Orthop. Surg. 2020, 12, 218–223. [Google Scholar] [CrossRef]
- Manara, J.R.; Bristol Knee, G.; White, P.; Bray, R.; Davies, H.; Eldridge, J.; Porteous, A.; Murray, J.R. Medium term results of the cementless Oxford mobile bearing medial unicompartmental knee replacement. Eur. J. Orthop. Surg. Traumatol. 2022, 1–6. [Google Scholar] [CrossRef]
- Hefny, M.H.; Smith, N.; Waite, J. Cementless medial Oxford unicompartmental knee replacement. Five-year results from an independent series. Knee 2020, 27, 1219–1227. [Google Scholar] [PubMed]
- Nandra, R.; Rajgor, H.D.; Winkworth, C.; Aslam, N. Regional five-year clinical outcomes of 289 consecutive cementless oxford uni-compartmental knee replacements at a non-inventor centre. J. Clin. Orthop. Trauma 2021, 17, 176–181. [Google Scholar] [CrossRef]
- Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: 2021 Annual Report 2021. Available online: https://aoanjrr.sahmri.com/annual-reports-2021 (accessed on 30 August 2022).
- Seeger, J.B.; Haas, D.; Jager, S.; Rohner, E.; Tohtz, S.; Clarius, M. Extended sagittal saw cut significantly reduces fracture load in cementless unicompartmental knee arthroplasty compared to cemented tibia plateaus: An experimental cadaver study. Knee Surg. Sport. Traumatol. Arthrosc. 2012, 20, 1087–1091. [Google Scholar] [CrossRef] [PubMed]
- Campi, S.; Mellon, S.J.; Ridley, D.; Foulke, B.; Dodd, C.A.F.; Pandit, H.G.; Murray, D.W. Optimal interference of the tibial component of the cementless Oxford Unicompartmental Knee Replacement. Bone Jt. Res. 2018, 7, 226–231. [Google Scholar] [CrossRef]
- Mohammad, H.R.; Campi, S.; Murray, D.; Mellon, S. Instruments to reduce the risk of tibial fracture following cementless unicompartmental knee replacement. Knee 2018, 25, 988–996. [Google Scholar] [CrossRef] [PubMed]
- Keppler, L.; Klingbeil, S.; Keppler, A.M.; Becker, J.; Fulghum, C.; Michel, B.; Voigts, K.; Reng, W. Impact of keel saw blade design and thickness on the incidence of tibial plateau fracture and tibial implant-loosening in cementless medial UKR. BMC Musculoskelet Disord. 2022, 23, 597. [Google Scholar] [CrossRef] [PubMed]
- Burger, J.A.; Jager, T.; Dooley, M.S.; Zuiderbaan, H.A.; Kerkhoffs, G.; Pearle, A.D. Comparable incidence of periprosthetic tibial fractures in cementless and cemented unicompartmental knee arthroplasty: A systematic review and meta-analysis. Knee Surg. Sport. Traumatol. Arthrosc. 2022, 30, 852–874. [Google Scholar] [CrossRef] [PubMed]
- Pandit, H.G.; Campi, S.; Hamilton, T.W.; Dada, O.D.; Pollalis, S.; Jenkins, C.; Dodd, C.A.F.; Murray, D.W. Five-year experience of cementless Oxford unicompartmental knee replacement. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Zuiderbaan, H.A.; van der List, J.P.; Khamaisy, S.; Nawabi, D.H.; Thein, R.; Ishmael, C.; Paul, S.; Pearle, A.D. Unicompartmental knee arthroplasty versus total knee arthroplasty: Which type of artificial joint do patients forget? Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Kahlenberg, C.A.; Nwachukwu, B.U.; McLawhorn, A.S.; Cross, M.B.; Cornell, C.N.; Padgett, D.E. Patient Satisfaction After Total Knee Replacement: A Systematic Review. HSS J. 2018, 14, 192–201. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panzram, B.; Barbian, F.; Reiner, T.; Hariri, M.; Renkawitz, T.; Walker, T. Clinical and Functional Results of Cementless Unicompartmental Knee Arthroplasty with a Minimum Follow Up of 5 Years—A Consecutive Cohort of 201 Patients. J. Clin. Med. 2023, 12, 1694. https://doi.org/10.3390/jcm12041694
Panzram B, Barbian F, Reiner T, Hariri M, Renkawitz T, Walker T. Clinical and Functional Results of Cementless Unicompartmental Knee Arthroplasty with a Minimum Follow Up of 5 Years—A Consecutive Cohort of 201 Patients. Journal of Clinical Medicine. 2023; 12(4):1694. https://doi.org/10.3390/jcm12041694
Chicago/Turabian StylePanzram, Benjamin, Frederik Barbian, Tobias Reiner, Mustafa Hariri, Tobias Renkawitz, and Tilman Walker. 2023. "Clinical and Functional Results of Cementless Unicompartmental Knee Arthroplasty with a Minimum Follow Up of 5 Years—A Consecutive Cohort of 201 Patients" Journal of Clinical Medicine 12, no. 4: 1694. https://doi.org/10.3390/jcm12041694
APA StylePanzram, B., Barbian, F., Reiner, T., Hariri, M., Renkawitz, T., & Walker, T. (2023). Clinical and Functional Results of Cementless Unicompartmental Knee Arthroplasty with a Minimum Follow Up of 5 Years—A Consecutive Cohort of 201 Patients. Journal of Clinical Medicine, 12(4), 1694. https://doi.org/10.3390/jcm12041694




