Early vs. Late Readmission following Percutaneous Coronary Intervention: Predictors and Impact on Long-Term Outcomes
Abstract
1. Introduction
2. Methods
3. Ethics and Informed Consent
4. Data Collection
5. Statistics
6. Results
7. Predictors of Unplanned Readmission
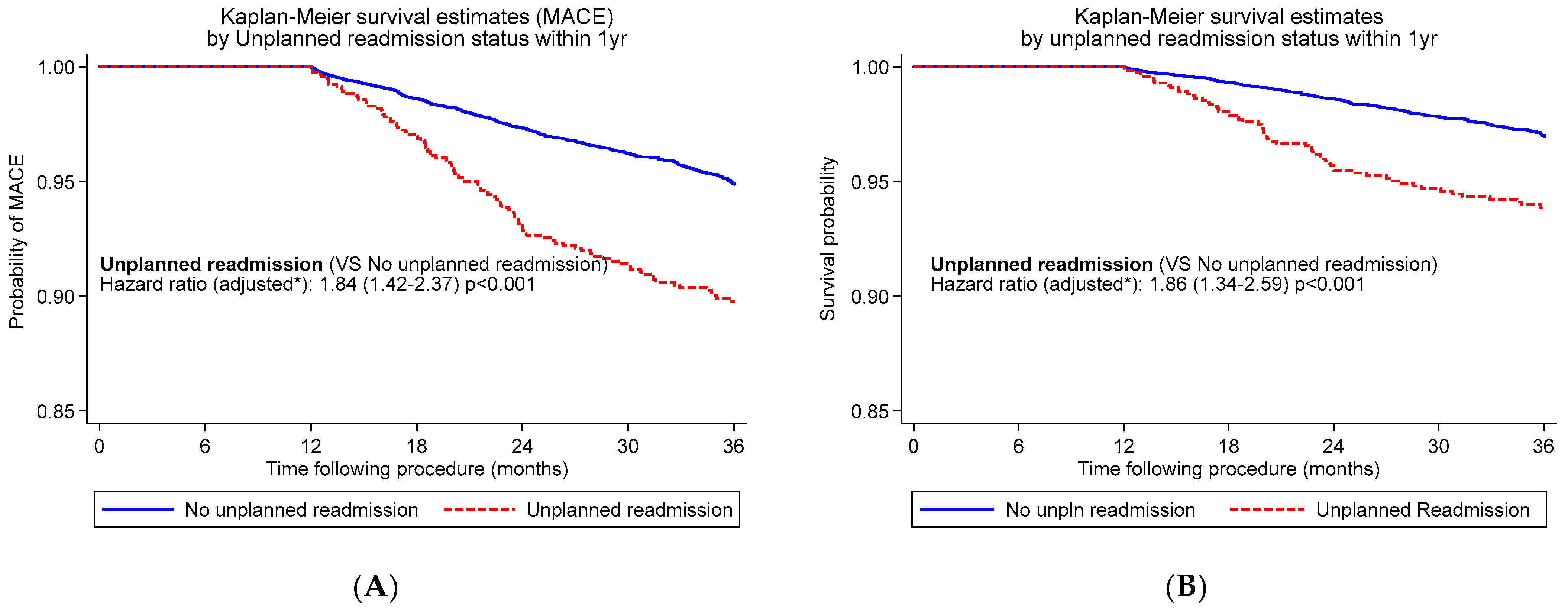
8. Predictors of Early vs. Late Unplanned Readmission
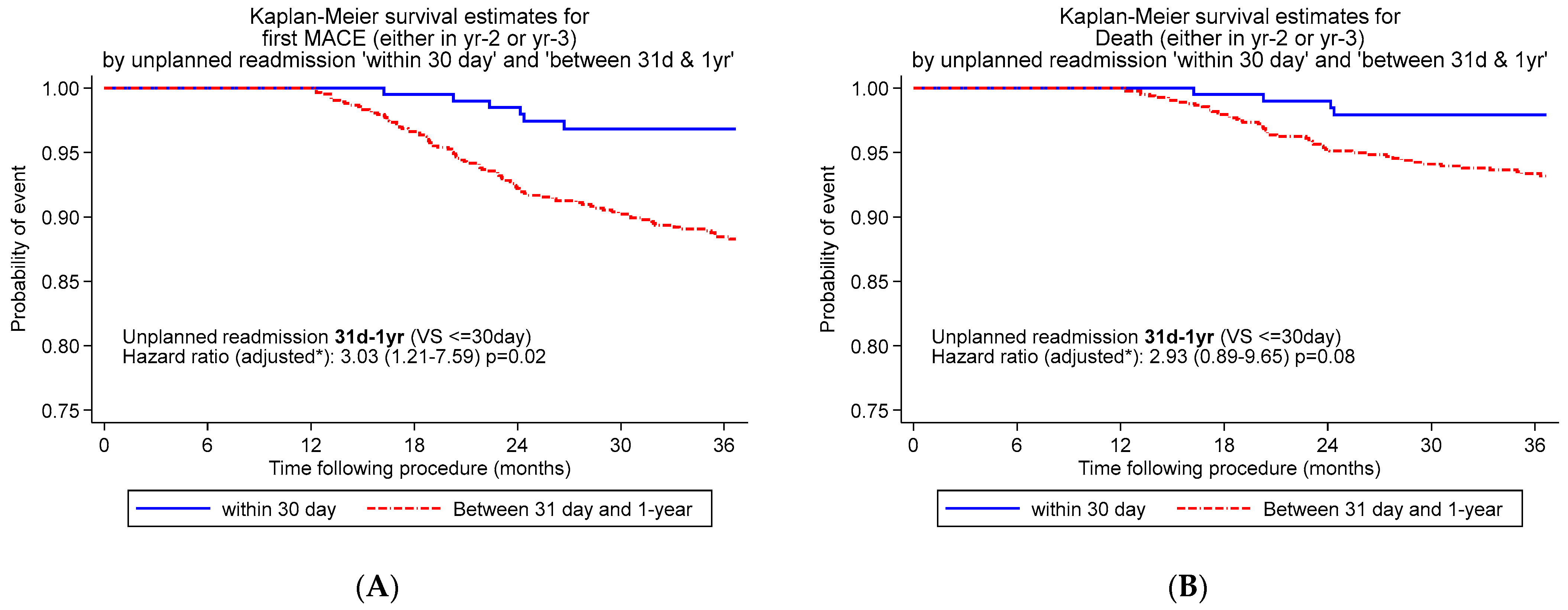
9. Long-Term Outcomes
10. Impact of Early vs. Late Readmission on Long-Term Outcomes
11. Discussion
12. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC); the European Association for Cardio-Thoracic Surgery (EACTS). Guidelines on myocardial revascularization. Eur. Heart J. 2010, 31, 2501–2555. [Google Scholar] [CrossRef] [PubMed]
- Stuntz, M.; Palak, A. Recent trends in percutaneous coronary intervention volume in the United States. Value Health 2016, 19, A641. [Google Scholar] [CrossRef]
- Australian Commission on Safety and Quality in Health Care. Exploring Healthcare Variation in Australia: Analyses Resulting from an OECD Study 2014; Australian Commission on Safety and Quality in Health Care: Sydney, Australia, 2014; ISBN Print: 978-1-921983-67-2; ISBN Online: 978-1-921983-68-9.
- Tripathi, A.; Abbott, J.D.; Fonarow, G.C.; Khan, A.R.; Barry, N.G.; Ikram, S.; Coram, R.; Mathew, V.; Kirtane, A.J.; Nallamothu, B.K.; et al. Thirty-Day Readmission Rate and Costs after Percutaneous Coronary Intervention in the United States: A National Readmission Database Analysis. Circ. Cardiovasc. Interv. 2017, 10, e005925. [Google Scholar] [CrossRef]
- Kwok, C.S.; Rao, S.V.; Potts, J.E.; Kontopantelis, E.; Rashid, M.; Kinnaird, T.; Curzen, N.; Nolan, J.; Bagur, R.; Mamas, M.A. Burden of 30-Day Readmissions After Percutaneous Coronary Intervention in 833,344 Patients in the United States: Predictors, Causes, and Cost Insights From the Nationwide Readmission Database. JACC Interv. 2018, 11, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.S.; Hulme, W.; Olier, I.; Holroyd, E.; Mamas, M.A. Review of early hospitalisation after percutaneous coronary intervention. Int. J. Cardiol. 2017, 227, 370–377. [Google Scholar] [CrossRef]
- Yost, G.W.; Puher, S.L.; Graham, J.; Scott, T.D.; Skelding, K.A.; Berger, P.B.; Blankenship, J.C. Readmission in the 30 days after percutaneous coronary intervention. JACC Cardiovasc. Interv. 2013, 6, 237–244. [Google Scholar] [CrossRef]
- Moretti, C.; D’Ascenzo, F.; Omede, P.; Sciuto, F.; Presutti, D.G.; Di Cuia, M.; Colaci, C.; Giusto, F.; Ballocca, F.; Cerrato, E.; et al. Thirty-day readmission rates after PCI in a metropolitan center in Europe: Incidence and impact on prognosis. J. Cardiovasc. Med. 2015, 16, 238–245. [Google Scholar] [CrossRef]
- Kwok, C.S.; Khan, M.A.; Rao, S.V.; Kinnaird, T.; Sperrin, M.; Buchan, I.; de Belder, M.A.; Ludman, P.F.; Nolan, J.; Loke, Y.K.; et al. Access and non-access site bleeding after percutaneous coronary intervention and risk of subsequent mortality and major adverse cardiovascular events: Systematic review and meta-analysis. Circ. Cardiovasc. Interv. 2015, 8, e001645. [Google Scholar] [CrossRef] [PubMed]
- Patient Protection and Affordable Care Act; Public Law No. 111-148; U.S. Government Publishing Office: Washington, DC, USA, 2010.
- Robinson, P. Hospital Readmissions and the 30-Day Threshold, 2010. ACHKS Market Intelligence Report 2010. Available online: http://www.chks.co.uk/userfiles/files/CHKS%20Report%20Hospital%20readmissions.pdf (accessed on 1 August 2021).
- Tanguturi, V.K.; Temin, E.; Yeh, R.W.; Thompson, R.W.; Rao, S.K.; Mallick, A.; Cavallo, E.; Ferris, T.G.; Wasfy, J.H. Clinical Interventions to Reduce Preventable Hospital Readmission After Percutaneous Coronary Intervention. Circ. Cardiovasc. Qual. Outcomes 2016, 9, 600–604. [Google Scholar] [CrossRef]
- Biswas, S.; Dinh, D.; Lucas, M.; Duffy, S.J.; Brennan, A.L.; Liew, D.; Cox, N.; Nadurata, V.; Reid, C.M.; Lefkovits, J.; et al. Incidence and Predictors of Unplanned Hospital Readmission after Percutaneous Coronary Intervention. J. Clin. Med. 2020, 9, 3242. [Google Scholar] [CrossRef]
- Eccleston, D.; Horrigan, M.; Rafter, T.; Holt, G.; Worthley, S.G.; Sage, P.; Whelan, A.; Reid, C.; Thompson, P.L. Improving Guideline Compliance in Australia With a National Percutaneous Coronary Intervention Outcomes Registry. Heart Lung Circ. 2017, 26, 1303–1309. [Google Scholar] [CrossRef] [PubMed]
- EQ-5DTM. Available online: http://www.euroqol.org/ (accessed on 21 February 2022).
- Morisky, D.; Ang, A.; Krousel-Wood, M.; Ward, H. Predictive Validity of A Medication Adherence Measure in an Outpatient Setting. J. Clin. Hypertens. 2008, 10, 348–354. [Google Scholar] [CrossRef] [PubMed]
- May, L. The National E-Health Transition Authority (NEHTA). Health Inf. Manag. 2005, 34, 19–20. [Google Scholar] [CrossRef]
- Kwok, C.S.; Shah, B.; Al-Suwaidi, J.; Fischman, D.L.; Holmvang, L.; Alraies, C.; Bagur, R.; Nagaraja, V.; Rashid, M.; Mohamed, M.; et al. Timing and Causes of Unplanned Readmissions After Percutaneous Coronary Intervention: Insights From the Nationwide Readmission Database. JACC Cardiovasc. Interv. 2019, 12, 734–748. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.N.; Bendix, K.; Antonsen, L.; Veien, K.T.; Mæng, M.; Junker, A.; Christiansen, E.H.; Kahlert, J.; Terkelsen, C.J.; Christensen, L.B.; et al. One-year rehospitalisation after percutaneous coronary intervention: A retrospective analysis. EuroIntervention 2018, 14, 926–934. [Google Scholar] [CrossRef]
- Kwok, C.W.; Narain, A.; Pacha, H.M.; Lo, T.S.; Holroyd, E.W.; Alraies, M.C.; Nolan, J.; Mamas, M.A. Readmissions to Hospital After Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis of Factors Associated with Readmissions. Cardiovasc. Revascularization Med. 2020, 21, 375–391. [Google Scholar] [CrossRef]
- Khawaja, F.J.; Shah, N.D.; Lennon, R.J.; Slusser, J.P.; Alkatib, A.A.; Rihal, C.S.; Gersh, B.J.; Montori, V.M.; Holmes, D.R.; Bell, M.R.; et al. Factors Associated With 30-Day Readmission Rates After Percutaneous Coronary Intervention. Arch Intern Med. 2012, 172, 112–117. [Google Scholar] [CrossRef]
- Généreux, P.; Giustino, G.; Witzenbichler, B.; Weisz, G.; Stuckey, T.D.; Rinaldi, M.J.; Neumann, F.J.; Metzger, D.C.; Henry, T.D.; Cox, D.A.; et al. Incidence, Predictors, and Impact of Post-Discharge Bleeding After Percutaneous Coronary Intervention. J. Am. Coll. Cardiol. 2015, 66, 1036–1045. [Google Scholar] [CrossRef]
- Masoudi, F.A.; Ponirakis, A.; de Lemos, J.A.; Jollis, J.G.; Kremers, M.; Messenger, J.C.; Moore, J.W.M.; Moussa, I.; Oetgen, W.J.; Varosy, P.D.; et al. Trends in U.S. Cardiovascular Care: 2016 Report From 4 ACC National Cardiovascular Data Registries. J. Am. Coll. Cardiol. 2017, 69, 1427–1450. [Google Scholar] [CrossRef]
- Taylor, J. SWEDEHEART: Sweden’s new online cardiac registry, the first of its kind. Eur. Heart J. 2009, 30, 2165–2173. [Google Scholar]
- Biswas, S.; Dinh, D.; Duffy, S.J.; Brennan, A.; Liew, D.; Chan, W.; Cox, N.; Reid, C.M.; Lefkovits, J.; Stub, D. Characteristics and outcomes of unsuccessful percutaneous coronary intervention. Catheter Cardiovasc Interv. 2022, 99, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Stromberg, A.; Martensson, J.; Fridlund, B.; Levin, L.A.; Karlsson, J.E.; Dahlstrom, U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: Results from a prospective, randomised trial. Eur. Heart J. 2003, 24, 1014–1023. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.S.; Rao, S.V.; Gilchrist, I.; Martinez, S.C.; Al Ayoubi, F.; Potts, J.; Rashid, M.; Kontopantelis, E.; Myint, P.K.; Mamas, M.A. Relation Between Age and Unplanned Readmissions After Percutaneous Coronary Intervention (Findings from the Nationwide Readmission Database). Am. J. Cardiol. 2018, 122, 220–228. [Google Scholar] [CrossRef]
- Wu, C.; Camacho, F.T.; King, I.I.I.S.B.; Walford, G.; Holmes, D.R., Jr.; Stamato, N.J.; Berger, P.B.; Sharma, S.B.; Curtis, J.P.; Venditti, F.J.; et al. Risk Stratification for Long-Term Mortality After Percutaneous Coronary Intervention. Circ. Cardiovasc. Interv. 2014, 7, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Moretti, C.; Meynet, I.; D’Ascenzo, F.; Omede, P.; Barbero, U.; Quadri, G.; Ballocca, F.; Zoccai, G.B.; Gaita, F. Sixty-day readmission rate after percutaneous coronary intervention: Predictors and impact on long-term outcomes. Eur. Heart J. Qual. Care Clin. Outcomes 2015, 1, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, D.; Morton, A.; Chowdhury, E.; Sage, P.; Conradie, A.; Rafter, T.; Delacroix, S.; Duong, M.; Chandrasekhar, J. Do Rural-Urban Disparities in Patient Characteristics Predict Outcomes After Percutaneous Coronary Intervention? Results From a Large Australian Registry. Heart Lung Circ. 2021, 30, S299–S300. [Google Scholar] [CrossRef]
- Murali-Krishnan, R.; Iqbal, J.; Rowe, R.; Hatem, E.; Parviz, Y.; Richardson, J.; Sultan, A.; Gunn, J. Impact of frailty on outcomes after percutaneous coronary intervention: A prospective cohort study. Open Heart 2015, 2, e000294. [Google Scholar] [CrossRef] [PubMed]
| Unplanned Readmission ≤30 Days | Unplanned Readmission 31 Days–1 Year | |||||
|---|---|---|---|---|---|---|
| Characteristics | No | Yes | p-Value | No | Yes | p-Value |
| N (%) | 16,237 | 403 | 12,806 | 1071 | ||
| Age, yr, mean (±SD) | 68.8 (10.5) | 69.7 (11.5) | 0.10 | 68.5 (10.5) | 69.3 (10.6) | 0.02 |
| Male | 12,383 (76.3%) | 291 (72.2%) | 0.045 | 9842 (76.9%) | 782 (73.0%) | 0.004 |
| Diabetes | 4007 (24.7%) | 88 (21.8%) | 0.18 | 3071 (24.0%) | 297 (27.7%) | 0.005 |
| Hypertension | 11,683 (72.0%) | 315 (78.2%) | 0.01 | 9225 (72.0%) | 835 (78.0%) | <0.001 |
| Hypercholesterolaemia 1 | 13,083 (80.6%) | 332 (82.4%) | 0.36 | 10,405 (81.3%) | 899 (83.9%) | 0.06 |
| CAD family history | 5738 (35.3%) | 125 (31.0%) | 0.06 | 4671 (36.5%) | 394 (36.8%) | 0.91 |
| Smoking ever | 8282 (51.0%) | 212 (52.6%) | 0.87 | 6730 (52.6%) | 568 (53.0%) | 0.79 |
| BMI, kg/m2, mean (±SD) | 29.0 (5.0) | 28.7 (5.2) | 0.29 | 28.9 (5.0) | 28.9 (4.7) | 0.76 |
| Heart failure | 1079 (6.6%) | 48 (11.9%) | <0.001 | 831 (6.5%) | 103 (9.6%) | <0.001 |
| Prior MI | 3533 (21.8%) | 106 (26.3%) | 0.04 | 2789 (21.8%) | 285 (26.6%) | <0.001 |
| Prior PCI | 5271 (32.5%) | 140 (34.7%) | 0.30 | 4106 (32.1%) | 410 (38.3%) | <0.001 |
| PVD | 1161 (7.2%) | 37 (9.2%) | 0.14 | 913 (7.1%) | 109 (10.2%) | <0.001 |
| Prior stroke/TIA | 1036 (6.4%) | 32 (7.9%) | 0.24 | 819 (6.4%) | 112 (10.5%) | <0.001 |
| Prior CABG | 1678 (10.3%) | 61 (15.1%) | 0.002 | 1315 (10.3%) | 201 (18.8%) | <0.001 |
| Prior AF | 1791 (14.2%) | 70 (22.2%) | <0.001 | 1282 (13.1%) | 180 (22.8%) | <0.001 |
| Renal failure 2 | 828 (5.8%) | 36 (10.1%) | <0.001 | 623 (5.5%) | 69 (7.2%) | 0.02 |
| Clinical presentation | <0.001 | <0.001 | ||||
| STEMI | 1113 (6.9%) | 30 (7.4%) | 912 (7.1%) | 51 (4.8%) | ||
| NSTEMI | 3452 (21.3%) | 128 (31.8%) | 2720 (21.2%) | 218 (20.4%) | ||
| UAP | 2479 (15.3%) | 72 (17.9%) | 1998 (15.6%) | 232 (21.7%) | ||
| Elective | 8394 (51.7%) | 160 (39.7%) | 6765 (52.8%) | 537 (50.1%) | ||
| Cardiogenic shock | 58 (0.4%) | 1 (0.2%) | 0.72 | 44 (0.3%) | 2 (0.2%) | 0.39 |
| Unplanned Readmission ≤30 Days | Unplanned Readmission 31 Days–1 Year | |||||
|---|---|---|---|---|---|---|
| Characteristics | No | Yes | p-Value | No | Yes | p-Value |
| N (%) | 16,237 | 403 | 12,806 | 1071 | ||
| Lesion access site | 0.54 | <0.001 | ||||
| Brachial | 48 (0.3%) | 0 (0.0%) | 40 (0.3%) | 3 (0.3%) | ||
| Radial | 7177 (44.2%) | 178 (44.2%) | 5125 (40.0%) | 341 (31.8%) | ||
| Femoral | 8824 (54.3%) | 222 (55.1%) | 7580 (59.2%) | 720 (67.2%) | ||
| Lesion type | 0.10 | <0.001 | ||||
| De novo | 13,496 (83.1%) | 332 (82.4%) | 10,914 (85.2%) | 891 (83.2%) | ||
| In stent restenosis | 748 (4.6%) | 29 (7.2%) | 579 (4.5%) | 88 (8.2%) | ||
| Restenosis | 90 (0.6%) | 3 (0.7%) | 50 (0.4%) | 6 (0.6%) | ||
| Other | 1903 (11.7%) | 39 (9.6%) | 1263 (9.7%) | 86 (8.0%) | ||
| ACC/AHA morphology | 0.85 | 0.88 | ||||
| A | 1834 (14.1) | 50 (15.2%) | 1452 (13.4%) | 118 (12.9%) | ||
| B1 | 4528 (34.7%) | 113 (34.2%) | 3846 (35.6%) | 323 (35.3%) | ||
| B2/C | 6685 (51.2%) | 167 (50.6%) | 5511 (50.9%) | 472 (51.6%) | ||
| Target vessel | 0.12 | <0.001 | ||||
| RCA | 4312 (26.6%) | 107 (26.6%) | 3480 (27.2%) | 248 (23.2%) | ||
| LMCA | 227 (1.4%) | 8 (2.0%) | 171 (1.3%) | 17 (1.6%) | ||
| LAD | 6025 (37.1%) | 127 (31.5%) | 4796 (37.5%) | 385 (35.9%) | ||
| LCx | 2960 (18.2%) | 84 (20.8%) | 2346 (18.3%) | 205 (19.1%) | ||
| Bypass | 400 (2.5%) | 14 (3.5%) | 312 (2.4%) | 61 (5.7%) | ||
| Other | 2313 (14.2%) | 63 (15.6%) | 1701 (13.3%) | 155 (14.5%) | ||
| Total occlusion | 664 (4.6%) | 19 (5.1%) | 0.61 | 532 (4.5%) | 53 (5.3%) | 0.29 |
| Multivessel disease | 7258 (44.7%) | 202 (50.1%) | 0.03 | 5633 (44.0%) | 499 (46.6%) | 0.12 |
| Bifurcation lesion | 1449 (10.0%) | 43 (11.7%) | 0.29 | 1139 (9.8%) | 105 (10.5%) | 0.45 |
| Stent length, mm (mean ± SD) | 19.2 (6.7) | 18.5 (6.7) | 0.04 | 19.1 (6.6) | 18.8 (6.4) | 0.26 |
| Stent diam., mm (mean ± SD) | 3.0 (0.5) | 3.0 (0.5) | 0.54 | 3.0 (0.5) | 2.9 (0.5) | <0.001 |
| Major bleeding (BARC 3–5) | 50 (0.3%) | 2 (0.5%) | 0.50 | 47 (0.4%) | 0 (0.0%) | 0.047 |
| Unplanned Readmission ≤30 Days | Unplanned Readmission 31 Days–1 Year | |||||
|---|---|---|---|---|---|---|
| Characteristics | No | Yes | p-Value | No | Yes | p-Value |
| N (%) | 16,237 | 403 | 12,806 | 1071 | ||
| Aspirin | 15,437 (96.5%) | 382 (96.7%) | 0.88 | 12,326 (97.1%) | 1021 (96.0%) | 0.06 |
| P2Y12 * | 14,498 (90.5%) | 369 (92.9%) | 0.11 | 11,653 (91.7%) | 990 (93.2%) | 0.08 |
| Statin | 14,647 (93.1%) | 354 (91.0%) | 0.18 | 11,796 (93.6%) | 973 (92.1%) | 0.15 |
| Statin contra-indicated | 112 (0.7%) | 5 (1.2%) | 86 (0.7%) | 8 (0.7%) | ||
| Beta-blocker | 8983 (55.3%) | 219 (54.3%) | 0.55 | 7270 (56.8%) | 607 (56.7%) | 0.99 |
| ACEI/ARB | 10,625 (65.4%) | 268 (66.5%) | 0.48 | 8567 (66.9%) | 714 (66.7%) | 0.72 |
| Characteristic | Unplanned Readmission ≤30 Days | Unplanned Readmission 31 Days–1 Year | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value | |
| Clinical | ||||||
| Age (years) | 1.00 | 0.98–1.01 | 0.55 | 0.99 | 0.98–1.0 | 0.046 |
| Male | 0.70 | 0.54–0.96) | 0.03 | 0.80 | 0.64–0.98 | 0.03 |
| Diabetes mellitus | - | - | - | 0.94 | 0.76–1.16 | 0.58 |
| Hypertension | 1.13 | 0.80–1.60 | 0.47 | 1.22 | 0.97–1.52 | 0.09 |
| Hypercholesterolemia | - | - | - | 1.11 | 0.84–1.46 | 0.47 |
| Heart failure | 1.37 | 0.82–2.20 | 0.20 | 1.08 | 0.77–1.50 | 0.67 |
| Previous MI | 0.99 | 0.70–1.40 | 0.95 | 0.93 | 0.74–1.18 | 0.56 |
| Previous PCI | - | - | - | 0.97 | 0.78–1.21 | 0.79 |
| Peripheral vascular disease | - | - | - | 1.37 | 1.01–1.85 | 0.04 |
| Previous CABG | 1.31 | 0.84–2.03 | 0.24 | 1.83 | 1.36–2.46 | <0.001 |
| Atrial fibrillation | 1.74 | 1.33–2.49 | 0.002 | 1.91 | 1.51–2.40 | <0.001 |
| Renal impairment | 1.54 | 0.95–2.5 | 0.08 | 1.30 | 0.92–1.84 | 0.13 |
| Presentation | ||||||
| NSTEMI | 1.18 | 0.67–2.10 | 0.57 | 1.23 | 0.80–1.90 | 0.35 |
| UAP | 1.23 | 0.67–2.25 | 0.50 | 1.61 | 1.03–2.50 | 0.03 |
| Elective | 0.69 | 0.39–1.21 | 0.20 | 1.13 | 0.74–1.71 | 0.58 |
| Procedural | ||||||
| In-stent restenosis | 1.29 | 0.70–2.37 | 0.42 | 1.55 | 1.06–2.27 | 0.03 |
| LAD | - | - | - | 1.29 | 1.03–1.61 | 0.03 |
| Bypass | - | - | - | 1.97 | 1.22–3.18 | 0.01 |
| Multivessel disease | 1.33 | 1.0–1.76 | 0.05 | |||
| Stent diameter (per unit) | - | - | - | 0.77 | 0.63–0.93 | 0.01 |
| Aspirin use at discharge | - | - | - | 0.70 | 0.41–1.20 | 0.20 |
| P2Y12 inhib. at discharge | - | - | - | 0.50 | 0.27–0.93 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eccleston, D.; Duong, M.-N.; Chowdhury, E.; Schwarz, N.; Reid, C.; Liew, D.; Conradie, A.; Worthley, S.G. Early vs. Late Readmission following Percutaneous Coronary Intervention: Predictors and Impact on Long-Term Outcomes. J. Clin. Med. 2023, 12, 1684. https://doi.org/10.3390/jcm12041684
Eccleston D, Duong M-N, Chowdhury E, Schwarz N, Reid C, Liew D, Conradie A, Worthley SG. Early vs. Late Readmission following Percutaneous Coronary Intervention: Predictors and Impact on Long-Term Outcomes. Journal of Clinical Medicine. 2023; 12(4):1684. https://doi.org/10.3390/jcm12041684
Chicago/Turabian StyleEccleston, David, My-Ngan Duong, Enayet Chowdhury, Nisha Schwarz, Christopher Reid, Danny Liew, Andre Conradie, and Stephen G. Worthley. 2023. "Early vs. Late Readmission following Percutaneous Coronary Intervention: Predictors and Impact on Long-Term Outcomes" Journal of Clinical Medicine 12, no. 4: 1684. https://doi.org/10.3390/jcm12041684
APA StyleEccleston, D., Duong, M.-N., Chowdhury, E., Schwarz, N., Reid, C., Liew, D., Conradie, A., & Worthley, S. G. (2023). Early vs. Late Readmission following Percutaneous Coronary Intervention: Predictors and Impact on Long-Term Outcomes. Journal of Clinical Medicine, 12(4), 1684. https://doi.org/10.3390/jcm12041684





