Abstract
Overweight and moderate obesity confer a survival benefit in chronic diseases such as coronary artery disease and chronic kidney disease, which has been termed the “obesity paradox”. However, whether this phenomenon exists in trauma patients remains controversial. We performed a retrospective cohort study in abdominal trauma patients admitted to a Level I trauma center in Nanjing, China between 2010 and 2020. In addition to the traditional body mass index (BMI) based measures, we further examined the association between body composition-based indices with clinical severity in trauma populations. Body composition indices including skeletal muscle index (SMI), fat tissue index (FTI), and total fat-to-muscle ratio (FTI/SMI) were measured using computed tomography. Our study found that overweight was associated with a four-fold risk of mortality (OR, 4.47 [95% CI, 1.40–14.97], p = 0.012) and obesity was associated with a seven-fold risk of mortality (OR, 6.56 [95% CI, 1.07–36.57], p = 0.032) compared to normal weight. Patients with high FTI/SMI had a three-fold risk of mortality (OR, 3.06 [95% CI, 1.08–10.16], p = 0.046) and double the risk of an intensive care unit length of stay ≥ 5 d (OR, 1.75 [95% CI, 1.06–2.91], p = 0.031) compared to patients with low FTI/SMI. The obesity paradox was not observed in abdominal trauma patients, and high FTI/SMI ratio was independently associated with increased clinical severity.
1. Introduction
Obesity has become a global epidemic, with 39% of adults being overweight and 13% being obese, respectively [1]. Obesity is a well-established risk factor for multiple chronic health conditions including diabetes, hypertension, dyslipidemia, arthritis, heart disease and certain malignancies [2,3]. Despite this, the obesity paradox, which refers to the phenomenon whereby a decreased mortality is present in overweight and moderate obesity compared to normal weight patients, has been observed in various acute and chronic diseases such as sepsis, acute respiratory distress syndrome, coronary artery disease and chronic kidney disease [4,5,6,7]. However, the impact of obesity on trauma patients remains controversial. Hakam et al. and Dvorak et al. have observed the obesity paradox defined by body mass index (BMI) in general trauma patients using the US National Trauma Data Bank (NTDB) [8,9]. However, Cone et al. failed to observe this phenomenon in patients with chest and head trauma using the US Trauma Quality Improvement Program (TQIP) database [10,11]. In the case of abdominal trauma, abdominal adipose, as a direct traumatized organ, might pose more severe metabolic disturbances compared with injuries in other body regions [12].
Nevertheless, BMI is an imprecise measure of adiposity, which fails to differentiate between fat and muscle mass or to quantify adiposity distribution, and patients with the same BMI may have different body composition phenotypes [13,14,15]. It is reported that both low skeletal muscle mass or sarcopenia and high fat mass increased the risk of poor prognosis in trauma patients [16,17]. However, few studies evaluated the combined effects of muscle and fat mass on the clinical outcomes of trauma patients. The fat-to-muscle ratio, a novel index for evaluating the combined effects of muscle and fat mass, has been demonstrated to be associated with a higher risk of metabolic syndrome in healthy adults and a higher risk of mortality in patients with chronic kidney disease [18,19]. Specifically, adults with the highest tertile of fat-to-muscle ratios had a four times higher risk of metabolic syndrome compared with those with the lowest tertile of fat-to-muscle ratios. Hemodialysis patients with higher fat-to-muscle ratios had a three times higher risk of all-cause death than those with lower fat-to-muscle ratios.
However, to our knowledge, the associations between fat-to-muscle ratio and clinical outcomes in trauma patients remain unclear. Studying the relationships between the fat-to-muscle ratio and clinical outcomes would help to take target interventions based on individual body composition at an early stage to improve prognosis. Hence, our study aimed to examine whether the obesity paradox exists in patients with abdominal trauma, and if the fat-to-muscle ratio is independently associated with clinical severity in abdominal trauma patients.
2. Materials and Methods
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline checklist [20].
2.1. Study Design and Patients
We conducted a retrospective cohort study in abdominal trauma patients admitted to the General Surgical Department of the Jinling Hospital Affiliated with Nanjing University Medical School between January 2010 and March 2020. Our hospital has a national Level I abdominal trauma center and is one of the initiating units of the Jiangsu Trauma Treatment Alliance, which could provide high quality data for our research. Abdominal trauma was defined as a blunt or penetrating injury to the abdominal cavity, which is located between the thorax cephalad and the pelvis caudad. Specifically, the upper limit is represented by a horizontal plane passing through the base of the xiphoid appendix and the spinous process of the 12th dorsal vertebra, and the lower limit starts from the pubic symphysis, passes through the entire inguinal arc and iliac crest, and terminates at the spinous process of the 5th lumbar vertebra [21]. During the study period, 963 consecutive patients were admitted to our hospital after abdominal trauma. Among these patients, 516 patients who were admitted to the hospital within 10 days of trauma met the inclusion criteria (Figure 1). After excluding 167 patients who had no abdominal computed tomography (CT) scans or low-quality images within 10 days before or after admission, 349 patients were further assessed for eligibility. Finally, a total of 328 patients were included in the study after excluding 14 patients younger than 18 years, 3 patients who were discharged or died within 24 h, 1 patient without an injury severity score (ISS) record, 1 patient with BMI above 50 kg/m2 and 2 patients with waist circumference (WC) below 30 or above 300 cm.
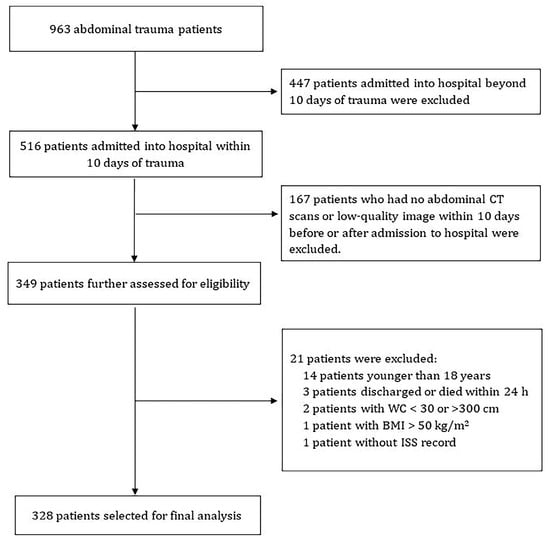
Figure 1.
Flow chart of the included participants. CT, computed tomography; WC, waist circumference; BMI, body mass index; ISS, injury severity score.
2.2. Data Collection
The following variables were extracted from the electronic medical record: demographic characteristics (age, sex, smoking history, alcohol consumption, hypertension, diabetes, height, weight, WC), clinical parameters (Glasgow Coma Scale (GCS), systolic blood pressure (SBP), heart rate (HR), respiratory rate (RR), trauma mechanism, body-region specific abbreviated injury scale (AIS), ISS, laparotomy), and outcomes of mechanical ventilation, death within 28 days of admission, length of stay in hospital and intensive care unit (ICU). Weight, height, and WC were measured on admission for each patient. BMI (defined as the weight in kilograms divided by the square of the height in meters) of less than 18.5 kg/m2, BMI of 18.5–23.9 kg/m2, BMI of 24.0–27.9 kg/m2 and BMI of 28 kg/m2 or higher were defined as underweight, normal weight, overweight and obese, respectively, according to the criteria of the Working Group on Obesity in China (WGOC) for adults [22].
2.3. CT-Based Body Composition Assessment
Body composition indices were measured using contrast-enhanced or unenhanced CT scans at the level of the third lumbar vertebra (L3). The image quality was evaluated by three independent radiologists, who were blinded to all patient information using a 5-point Likert scale with 5 being excellent [23]. All CT scans of acceptable quality were then transferred to the Image J2 software (The National Institutes of Health, Washington, MD, USA) to measure skeletal muscle and adipose tissue areas. The tissue cross-sectional areas were analyzed using tissue-specific Hounsfield Units (HU) attenuation ranges: (1) −29 and +150 HU for skeletal muscle, (2) −150 to −50 HU for viscera adipose tissue, and (3) −190 to −30 HU for subcutaneous and intramuscular adipose tissue [24] (Figure 2). The outer contour of the abdominal wall was automatically delineated and the abdominal muscular wall was manually delineated. Total muscle area (TMA), subcutaneous fat area (SFA) and visceral fat area (VFA) were measured. Total fat area (TFA) was the sum of SFA and VFA.
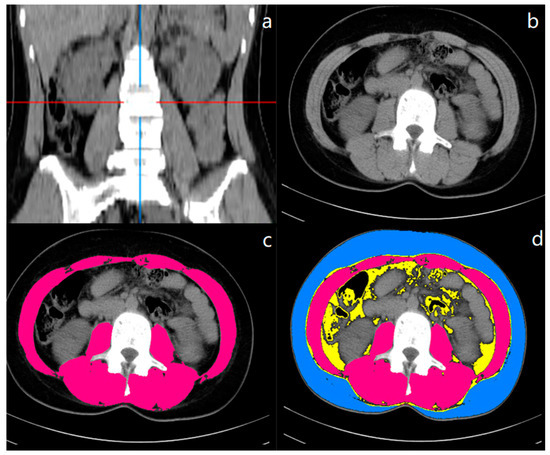
Figure 2.
CT measurement of body composition at the level of the third lumbar vertebra (L3). (a) represented the coronal image and the red and blue lines identified the level of L3 and median coronal dividers, respectively. (b–d) represented the cross-sectional images. In the (c,d) images, different body composition areas were distinguished by different colors (blue: subcutaneous adipose tissue area; red: skeletal muscle area; the yellow area within the inner wall of the muscle: visceral adipose tissue area).
Body composition indices were then normalized by the square of height (cm2/m2) [25,26]. We used TMA, TFA, SFA, and VFA to calculate the skeletal muscle index (SMI, TMA [cm2]/height2 [m2]), fat tissue index (FTI, TFA [cm2]/height2 [m2]), subcutaneous adipose tissue index (SATI, SFA [cm2]/height2 [m2]), visceral adipose tissue index (VATI, VFA [cm2]/height2 [m2]). We further calculated fat-to-muscle area ratios including the total fat-to-muscle area ratio (FTI/SMI), subcutaneous fat-to-muscle area ratio (SATI/SMI), and visceral fat-to-muscle area ratio (VATI/SMI) to assess the combined effects of fat and skeletal muscle on abdominal trauma patients [27]. In addition, the visceral-to-subcutaneous fat area ratio (VATI/SATI) was computed to evaluate the impact of fat distribution on trauma patients [28]. All these indices were divided into low and high groups according to sex-specific median cutoff values [29].
2.4. Outcomes
The primary clinical outcome was 28-day mortality. Secondary clinical outcomes included the use of mechanical ventilation during hospitalization and an ICU length of stay ≥ 5 d.
2.5. Statistical Analysis
Kendall’s coefficient of concordance (Kendall’s W) and intraclass correlation coefficient (ICC) (0 indicates no agreement between raters; 1 indicates perfect agreement between raters) were calculated to assess the consistency of CT image quality assessment among the three radiologists. The normality of distribution was assessed using the Shapiro–Wilk test. Continuous data with a normal distribution were expressed as the means (standard deviations, SDs) and compared by t-test or one-way analysis of variance, as appropriate. Continuous data without a normal distribution were expressed as the medians (interquartile ranges, IQRs) and compared by Mann–Whitney U test or Kruskal–Wallis test as appropriate. Categorical data were expressed as frequencies and percentages and compared by χ2 test or Fisher exact test as appropriate. Correlations between body composition indices were assessed by Pearson correlation analyses.
The associations of the BMI category and fat-to-muscle area ratios with 28-day mortality, mechanical ventilation, and ICU length of stay ≥ 5 d were assessed with univariable and multivariable logistic regression analyses, respectively. We adjusted for potential confounders including age, sex, ISS ≥ 16, hypertension, diabetes, smoking history, alcohol consumption, HR > 120 beats/min, RR > 20 beats/min, SBP < 90 mmHg, GCS < 9 and laparotomy. These variables were chosen based on their clinical relevance to outcomes, and the previous literature [10,11].
In our dataset, there were 7 (2.1%) patients with unknown history of smoking and alcohol consumption and 1 (0.3%) patient without SBP measurement at admission. Missing values were replaced by the mean value for the continuous variable and by the mode (i.e., negative) for the categorical variables, including smoking and alcohol consumption history. All statistical tests were two-sided, and p < 0.05 was considered statistically significant. All analyses were conducted using R version 4.1.1. (R Foundation for Statistical Computing, Vienna, Austria).
3. Results
There was a strong consistency in the evaluation of CT image quality between three radiologists, indicated by 0.836 of Kendall’s W (p < 0.001) and 0.806 of ICC (p < 0.001). The median age was 43 (31–53) years and 266 (81.1%) were males (Table 1). A total of 301 (91.8%) patients suffered from blunt trauma and most patients were severely injured, with 241 (73.5%) of patients having an ISS ≥ 16. 13 (4.0%), 233 (71.0%), 60 (18.3%) and 22 (6.7%) patients were classified as underweight, normal weight, overweight and obese, respectively. The median length of ICU stay was 5 (2–10) days. The need for mechanical ventilation occurred in 101 (30.8%) patients, and 21 (6.4%) patients died within 28 days of admission.

Table 1.
Clinical characteristics and outcomes of abdominal trauma patients stratified by BMI and 28-day mortality of admission.
FTI/SMI, VATI/SMI, and SATI/SMI ratios increased significantly with higher BMI classes (Table 1). Patients with higher classes of BMI had more severe injuries, particularly in the abdomen, indicated by a higher proportion of ISS ≥ 16 and AIS score abdomen ≥ 3 in patients with overweight (88.3% and 81.7%, respectively) and obesity (86.4% and 95.5%, respectively). Patients with overweight (13.3% vs. 4.3%, p = 0.016) and obesity (13.6% vs. 4.3%, p = 0.090) had higher 28-day mortality compared with normal weight patients (Table 1, Figure 3). Patients with overweight and obesity were more likely to require mechanical ventilation (35.0% vs. 27.9%, p = 0.281 and 50.0% vs. 27.9%, p = 0.030, respectively) and to stay in the ICU longer than 5 days (60.0% vs. 47.2%, p = 0.077 and 68.2% vs. 47.2%, p = 0.060, respectively). In the multivariable logistic model, after adjusting for all potential confounders we found that the risk of death within 28 days was around 4.5 times (OR, 4.47 [95% CI, 1.40–14.97]; p = 0.012) and 6.6 times (OR, 6.56 [95% CI, 1.07–36.57]; p = 0.032) higher in patients with overweight and obesity than normal weight patients (Table 2). However, such an association was not observed between overweight or obesity and mechanical ventilation, and ICU length of stay ≥ 5 d.
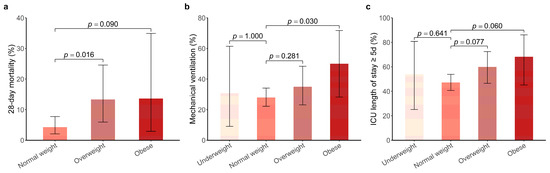
Figure 3.
Comparison of clinical severity including 28-day mortality (a), mechanical ventilation (b) and ICU length of stay ≥ 5 d (c) in abdominal trauma patients with different BMI classifications. p values above each bar plot indicate significance between the respective BMI group of abdominal trauma patients (underweight, overweight, and obese) and the normal weight. The error bars denote the confidence interval, which was calculated based on exact binomial distribution. ICU, intensive care unit.

Table 2.
Associations between different body composition indices and 28-day mortality, mechanical ventilation, and ICU length of stay ≥ 5 d in patients with abdominal trauma.
Patients with high FTI/SMI ratios were more likely to be older (46 vs. 40 years, p = 0.001) compared with low FTI/SMI ratios patients (Table 1). In patients of all ages, females have significantly higher FTI/SMI ratios compared with males (2.02 vs. 1.39, p < 0.001) (Figure 4). After further stratifying patients by age groups, in general, FTI/SMI increased with age and females tended to have higher FTI/SMI across all age groups. Patients with high FTI/SMI ratios had a higher proportion of alcohol consumption (33.5% vs. 22.0%, p = 0.019), with higher prevalence of diabetes (10.4% vs. 3.7%, p = 0.017) and hypertension (23.2% vs. 14.0%, p = 0.033) (Table 1). Moreover, these patients also had higher BMI (22.9 vs. 21.7 kg/m2, p < 0.001) and a higher proportion of ISS ≥ 16 (79.3% vs. 67.7%, p = 0.017). For clinical outcomes, the use of mechanical ventilation (37.2% vs. 24.4%, p = 0.012) and death within 28 days (9.8% vs. 3.0%, p = 0.013) occurred in a significantly higher percentage in patients with high FTI/SMI ratios than in those with low FTI/SMI ratios. Patients with high FTI/SMI ratios also tended to have longer ICU lengths of stay (6 vs. 4 days, p = 0.009). When we stratified patients according to BMI, we found that one (7.7%) patient with underweight, 105 (45.1%) patients with normal weight, 38 (63.3%) patients with overweight and 20 (90.9%) patients with obesity had high FTI/SMI ratios (Figure 5). Furthermore, we found that, among those normal weight patients, eight (79.1%) of the deaths, 38 (58.4%) of the mechanical ventilation users and 57 (51.8%) of ICU stays > 5 d occurred in the high FTI/SMI subgroup.
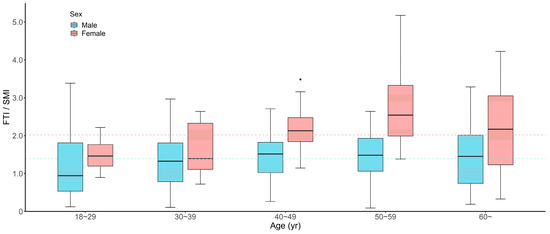
Figure 4.
Box plots showing differences in FTI/SMI according to sex and age. The blue and red dashed lines represent the median FTI/SMI for male (1.39) and female (2.02) patients, respectively. FTI, fat tissue index; SMI, skeletal muscle index.
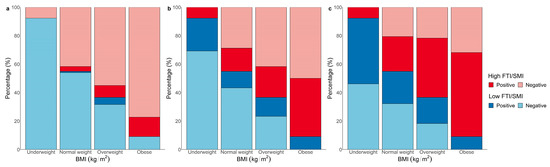
Figure 5.
Bar plots showing the percentage of patients with combinations of low or high FTI/SMI ratios and corresponding positive or negative clinical outcomes in each BMI group. (a): Mortality within 28 days; (b): Mechanical ventilation; (c): ICU length of stay ≥ 5 d. BMI, body mass index; FTI, fat tissue index; SMI, skeletal muscle index.
In multivariable analyses for evaluating the associations between fat-to-muscle area ratios and clinical outcomes, we found that the risk of death within 28 days and ICU length of stay ≥ 5 d was about 3.1 (OR, 3.06 [95% CI, 1.08–10.16]; p = 0.046) and 1.8 (OR, 1.75 [95% CI, 1.06–2.91]; p = 0.031) times higher in high FTI/SMI ratios patients than low FTI/SMI ratios patients (Table 2). After distinguishing adipose tissues in different depots, we found that a high SATI/SMI ratio significantly increased the risk of death within 28 days (OR, 3.33 [95% CI, 1.16–11.13]; p = 0.034), while a high VATI/SMI ratio (OR, 1.99 [95% CI, 1.05–3.82]; p = 0.037) significantly increased the risk of mechanical ventilation. However, there was no significant association between ICU length of stay and the VATI/SMI (OR, 1.39 [95% CI, 0.83–2.33]; p = 0.215) or SATI/SMI ratio (OR, 1.28 [95% CI, 0.79–2.10]; p = 0.321).
4. Discussion
Our study examined whether overweight and obesity confer a survival benefit in abdominal trauma patients and comprehensively assessed the association between skeletal muscle and fat mass and clinical severity by using the fat-to-muscle ratio. We found that patients with overweight and obesity have higher mortality rates than normal weight patients, which indicated that the obesity paradox defined by BMI might not be applied to patients with abdominal trauma. A higher FTI/SMI ratio was independently associated with an increased risk of 28-day mortality and an ICU length of stay ≥ 5 d.
The obesity paradox has been demonstrated in multiple acute and chronic diseases, probably because overweight or moderate obesity was associated with higher energy reserves, anti-inflammatory immune profile, and inflammatory preconditioning, which conferred a survival benefit [4]. Inflammatory preconditioning refers to the fact that increased baseline inflammation caused by obesity triggers multiple anti-inflammatory and antioxidant endogenous pathways to counteract new onset acute inflammatory reactions in critical illness [30,31]. The anti-inflammatory immune profile refers to the anti-inflammatory adipokine profile and M2-type macrophage accumulation in the chronic phase of critical illness [32]. However, the obesity paradox remains conflicting in trauma patients. Dvorak et al. and Farhat et al. have observed this phenomenon in general trauma patients [8,9], while Cone et al. failed to observe it in patients with severe blunt chest trauma and head trauma [10,11]. In the present study, the obesity paradox was not observed in abdominal trauma patients, either. These conflicting results could be attributed to the high heterogeneity of the trauma population and the methodological limitations of using BMI as a proxy for obesity. Abdominal trauma patients have different trauma mechanisms and injury locations, and most of them present with multiple injuries. Delayed diagnosis and treatment were common in this specific trauma population due to their complexity and concealment [33]. Furthermore, several studies have found that the obesity paradox existed in patients with cancer or heart failure when using BMI but it disappeared when using body composition or WC [34,35]. Therefore, more accurate measures to better characterize body composition and fat distribution were warranted instead of BMI alone [4].
CT imaging is easily available in clinical practice and has been evaluated as an accurate method to evaluate skeletal muscle and fat mass. Thus, we used L3 level CT to provide precise estimates of muscle and adipose tissue that are highly correlated with the whole-body volumes of muscle and adipose [36]. Prior studies have examined the associations of skeletal muscle mass and fat mass individually with clinical outcomes in trauma patients, however, their findings were controversial. For skeletal muscle mass, several studies have demonstrated that low skeletal muscle mass was an independent predictor of poor prognosis in patients with trauma [16,37], but this failed to be validated in other studies [38,39]. For fat mass, Shashaty et al. have reported that abdominal adiposity was independently associated with acute kidney injury in critically ill trauma patients [17]. However, no significant associations were observed between fat mass and other clinical outcomes including mortality and hospital or ICU length of stay in other studies [37,38].
Skeletal muscle mass and fat mass should be considered together to avoid the above contradictory results, due to the close correlation between skeletal muscle mass and body fat mass. In this study, there was a positive relationship between FTI and SMI (r = 0.319, p < 0.001) (Supporting information Figure S1), so the assessment of the effect of either SMI or FTI required the simultaneous consideration of both [19].
Therefore, we used the fat-to-muscle ratio to evaluate the effect of the combined muscle and fat mass on abdominal trauma patients. Given gender differences in the FTI/SMI ratio, we grouped patients as high FTI/SMI and low FTI/SMI ratios according to sex-specific medians. The average FTI/SMI were represented as medians in view of non-normality, while as means in a study of trauma patients in Germany [38]. By comparison, we found that males in our study have lower FTI/SMI (1.39 vs. 1.47) but females have higher FTI/SMI (2.02 vs. 1.83), which demonstrated differences in body architecture and body composition among different populations. The fat-to-muscle ratio could be an indicator of sarcopenic obesity, which referred to high fat mass accompanied by low muscle mass. Sarcopenic obesity has been shown as a predictor of metabolic syndrome and cardiovascular diseases, and poor prognosis in patients undergoing hemodialysis [18,19,27]. In our study, we also found that patients with high FTI/SMI ratios had a higher prevalence of diabetes and hypertension, and a high FTI/SMI ratio was significantly associated with poor clinical outcomes after abdominal trauma. There are several biological mechanisms to explain the observed association. Skeletal muscle plays an important role in regulating immune function, glucose disposal and protein synthesis [37]. Therefore, sarcopenic patients have a worse recovery after trauma due to their decreased resilience and physiological reserve [16]. Moreover, obesity is a metabolic syndrome involving hypertension, hyperglycemia, dyslipidemia and a pro-inflammatory state, which has been reported to increase the risk of adverse outcomes after trauma. Specifically, adipose tissue participates in the systematic proinflammatory response to acute trauma, which produces numerous inflammatory mediators such as circulating interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), and leptin [40].
In addition, we explored the combined effect of skeletal muscle mass and fat mass in different depots; however, the results were not consistent for different outcome measures. The SATI/SMI ratio was associated with 28-day mortality, and the VATI/SMI ratio was associated with the use of mechanical ventilation, but neither was associated with the length of ICU stay. The reasons for the apparent differences in these associations were not clear, but may be related to the different effects of visceral and subcutaneous adipose tissue distribution. Two prior studies have shown that visceral to subcutaneous adipose tissue distribution was not associated with increased inflammatory profiles or clinical outcomes after trauma [40,41]. However, a recent study found that lower visceral to subcutaneous adipose tissue distribution was associated with increased inflammatory response and worse clinical outcomes in multiple trauma patients [28]. In this study, we have examined whether body fat distribution by calculating the VATI/SATI ratio has an impact on abdominal trauma patients as well, but no significant associations were found between the VATI/SATI ratio and clinical outcomes (Supporting information Table S1). Therefore, the effect of fat distribution on outcomes in trauma patients needs to be further explored.
Our findings have important clinical implications. Given that muscle and fat are intricately correlated, monitoring the configuration of individual body composition by using the FTI/SMI ratio is critical to improving the prognosis in patients with abdominal trauma. Those patients with high FTI/SMI ratios based on sex-specific medians (1.39 for males, 2.02 for females) may benefit from early appropriate nutritional, pharmacological and exercise interventions. In addition, it is worth noting that up to 45.1% of normal weight patients have high FTI/SMI ratios in the present study, suggesting that these high-risk patients might be overlooked in routine trauma care when using BMI as a risk assessment tool alone.
Our study had several limitations that should be considered. First, this was a single-center retrospective study with a relatively limited sample size, which limits the generalizability of our results to other populations, although we consecutively included abdominal trauma patients admitted to our hospital across the decade. Moreover, the relatively low numbers of underweight patients limited our ability to analyze the relationship between underweight and clinical outcomes in trauma patients, whereas it has been well demonstrated in prior studies [9,10]. Second, as with any observational study, the causalities of the relationship between the FTI/SMI ratio and outcomes were unable to be established, but its value as an independent predictor could be established and further guide clinical practice. Third, 167 patients were excluded due to unavailability or poor image quality of CT scans within 10 days before or after admission to hospital, which might affect the results. However, no significant association was found between the availability of CT scans and BMI or outcome. Fourth, patients admitted within 10 days of trauma might not have the same BMI, FTI or SMI measurements as baseline due to prehospital treatment. However, most patients (73%) were admitted to hospital within three days of trauma, so we believed the impact would be minor. Finally, as we collected body composition measurements at baseline, dynamic changes in body composition during the clinical course were not considered. Future research is needed to investigate the time-dependent dynamic effect of the FTI/SMI ratio on clinical outcomes in patients with abdominal trauma.
5. Conclusions
In conclusion, the obesity paradox was not observed in patients with abdominal trauma. Patients with overweight and obesity have higher mortality rates than normal-weight patients. A higher FTI/SMI ratio was significantly associated with increased 28-day mortality and ICU length of stay, which could be used as a predictor of adverse outcomes in trauma patients. Our findings were particularly useful for patients with high FTI/SMI but normal weight measured by BMI, and early targeted interventions might improve prognosis in this subgroup.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12041503/s1, Figure S1: Scatter plots of different body composition indexes in patients with abdominal trauma. (a): BMI and FTI; (b): BMI and SMI; (c): FTI and SMI; (d): BMI and SATI; (e): BMI and VATI; (f) SATI and VATI; Table S1: Association between abdominal fat distribution and 28-day mortality, mechanical ventilation and ICU length of stay ≥ 5 d in patients with abdominal trauma.
Author Contributions
X.W. and W.Y. conceived, designed, and supervised the study. F.X., Y.H. and C.S. participated in data collection. J.L. carried out the data analysis. J.L. and F.X. prepared the first draft of the manuscript. X.W. and W.Y. interpreted the findings and commented on and revised drafts of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
X.W. is supported by the Three-year Public Health System Construction Program of Shanghai, China (No. GWV-10.2-YQ36). W.Y. is supported by “The 13th Five-Year Plan” Foundation of Jiangsu Province for Medical Key Talents (grant number: ZDRCA2016099) and by the National Major Scientific Research Instruments and Equipments Development Project of the National Natural Science Foundation of China (grant number: 81927808).
Institutional Review Board Statement
This study was approved by the Human Ethics Committee of Jinling Hospital (IRB# 2021NZKY-045-01) and the Institutional Ethics Review Board of the School of Public Health of Fudan University (IRB# 2021-11-0930).
Informed Consent Statement
Informed consent was waived due to the retrospective nature of the study.
Data Availability Statement
The datasets used and/or analyzed during the current study are not publicly available due to patient privacy concerns, but are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Lim, H.J.; Xue, H.; Wang, Y. Global trends in obesity. In Handbook of Eating and Drinking: Interdisciplinary Perspectives; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1217–1235. [Google Scholar]
- Dixon, J.B. The effect of obesity on health outcomes. Mol. Cell. Endocrinol. 2010, 316, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Sarma, S.; Sockalingam, S.; Dash, S. Obesity as a multisystem disease: Trends in obesity rates and obesity-related complications. Diabetes Obes. Metab. 2021, 23 (Suppl. 1), 3–16. [Google Scholar] [CrossRef]
- Karampela, I.; Chrysanthopoulou, E.; Christodoulatos, G.S.; Dalamaga, M. Is There an Obesity Paradox in Critical Illness? Epidemiologic and Metabolic Considerations. Curr. Obes. Rep. 2020, 9, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Wang, M.; Li, S.; Zhang, J.; Ma, Q.; Ding, Y.; Ge, H.; Shen, N.; Zheng, Y.; Sun, Y. Impact of body mass index on survival of medical patients with sepsis: A prospective cohort study in a university hospital in China. BMJ Open 2018, 8, e021979. [Google Scholar] [CrossRef]
- O’Brien, J.M., Jr.; Philips, G.S.; Ali, N.A.; Aberegg, S.K.; Marsh, C.B.; Lemeshow, S. The association between body mass index, processes of care, and outcomes from mechanical ventilation: A prospective cohort study. Crit. Care Med. 2012, 40, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Bucholz, E.M.; Rathore, S.S.; Reid, K.J.; Jones, P.G.; Chan, P.S.; Rich, M.W.; Spertus, J.A.; Krumholz, H.M. Body mass index and mortality in acute myocardial infarction patients. Am. J. Med. 2012, 125, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Farhat, A.; Grigorian, A.; Nguyen, N.T.; Smith, B.; Williams, B.J.; Schubl, S.D.; Joe, V.; Elfenbein, D.; Nahmias, J. Obese trauma patients have increased need for dialysis. Eur. J. Trauma Emerg. Surg. 2020, 46, 1327–1334. [Google Scholar] [CrossRef]
- Dvorak, J.E.; Lester, E.L.W.; Maluso, P.J.; Tatebe, L.; Schlanser, V.; Kaminsky, M.; Messer, T.; Dennis, A.J.; Starr, F.; Bokhari, F. The Obesity Paradox in the Trauma Patient: Normal May not Be Better. World J. Surg. 2020, 44, 1817–1823. [Google Scholar] [CrossRef]
- Cone, J.T.; Benjamin, E.R.; Alfson, D.B.; Biswas, S.; Demetriades, D. The effect of body mass index on outcomes following severe blunt chest trauma. Injury 2020, 51, 2076–2081. [Google Scholar] [CrossRef]
- Cone, J.T.; Benjamin, E.R.; Alfson, D.B.; Demetriades, D. Isolated severe blunt traumatic brain injury: Effect of obesity on outcomes. J. Neurosurg. 2020, 134, 1667–1674. [Google Scholar] [CrossRef] [PubMed]
- Wrba, L.; Halbgebauer, R.; Roos, J.; Huber-Lang, M.; Fischer-Posovszky, P. Adipose tissue: A neglected organ in the response to severe trauma? Cell Mol. Life Sci. 2022, 79, 207. [Google Scholar] [CrossRef]
- Johansen, K.L. Association of body composition with survival among patients on hemodialysis. Clin. J. Am. Soc. Nephrol. 2010, 5, 2144–2145. [Google Scholar] [CrossRef]
- Caan, B.J.; Cespedes Feliciano, E.M.; Kroenke, C.H. The Importance of Body Composition in Explaining the Overweight Paradox in Cancer-Counterpoint. Cancer Res. 2018, 78, 1906–1912. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Pinto, A.; Giusti, A.M.; Lenzi, A.; Poggiogalle, E. Obesity or BMI Paradox? Beneath the Tip of the Iceberg. Front. Nutr. 2020, 7, 53. [Google Scholar] [CrossRef]
- Xia, W.; Barazanchi, A.W.H.; MacFater, W.S.; Hill, A.G. The impact of computed tomography-assessed sarcopenia on outcomes for trauma patients—A systematic review and meta-analysis. Injury 2019, 50, 1565–1576. [Google Scholar] [CrossRef]
- Shashaty, M.G.; Kalkan, E.; Bellamy, S.L.; Reilly, J.P.; Holena, D.N.; Cummins, K.; Lanken, P.N.; Feldman, H.I.; Reilly, M.P.; Udupa, J.K.; et al. Computed tomography-defined abdominal adiposity is associated with acute kidney injury in critically ill trauma patients*. Crit. Care Med. 2014, 42, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Kim, S.G.; Kim, J.K.; Lee, Y.K.; Noh, J.W.; Oh, J.; Kim, H.J.; Song, Y.R. Fat-to-Lean Mass Ratio Can Predict Cardiac Events and All-Cause Mortality in Patients Undergoing Hemodialysis. Ann. Nutr. Metab. 2018, 73, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.N.; Park, M.S.; Lim, K.I.; Yang, S.J.; Yoo, H.J.; Kang, H.J.; Song, W.; Seo, J.A.; Kim, S.G.; Kim, N.H.; et al. Skeletal muscle mass to visceral fat area ratio is associated with metabolic syndrome and arterial stiffness: The Korean Sarcopenic Obesity Study (KSOS). Diabetes Res. Clin. Pract. 2011, 93, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Cirocchi, R.; Boselli, C.; Renzi, C.; Corsi, A.; Cagini, L.; Boccolini, A.; Noya, G.; Fingerhut, A. The surface landmarks of the abdominal wall: A plea for standardization. Arch. Med. Sci. 2014, 10, 566–569. [Google Scholar] [CrossRef]
- Zhou, B.F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—Study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 2002, 15, 83–96. [Google Scholar] [PubMed]
- Kraus, M.S.; Selo, N.; Kiefer, L.S.; Esser, M.; Albtoush, O.M.; Weiss, J.; Wichmann, J.L.; Bamberg, F.; Othman, A.E. Advanced Virtual Monoenergetic Imaging: Improvement of Visualization and Differentiation of Intramuscular Lesions in Portal-Venous-phase Contrast-enhanced Dual-energy CT. Acad. Radiol. 2019, 26, 1457–1465. [Google Scholar] [CrossRef] [PubMed]
- Xi, F.; Tan, S.; Gao, T.; Ding, W.; Sun, J.; Wei, C.; Li, W.; Yu, W. Low skeletal muscle mass predicts poor clinical outcomes in patients with abdominal trauma. Nutrition 2021, 89, 111229. [Google Scholar] [CrossRef] [PubMed]
- Borggreve, A.S.; den Boer, R.B.; van Boxel, G.I.; de Jong, P.A.; Veldhuis, W.B.; Steenhagen, E.; van Hillegersberg, R.; Ruurda, J.P. The Predictive Value of Low Muscle Mass as Measured on CT Scans for Postoperative Complications and Mortality in Gastric Cancer Patients: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 199. [Google Scholar] [CrossRef]
- Kong, M.; Xu, M.; Zhou, Y.; Geng, N.; Lin, N.; Song, W.; Li, S.; Piao, Y.; Han, Z.; Guo, R.; et al. Assessing Visceral Obesity and Abdominal Adipose Tissue Distribution in Healthy Populations Based on Computed Tomography: A Large Multicenter Cross-Sectional Study. Front. Nutr. 2022, 9, 871697. [Google Scholar] [CrossRef]
- Seo, Y.G.; Song, H.J.; Song, Y.R. Fat-to-muscle ratio as a predictor of insulin resistance and metabolic syndrome in Korean adults. J. Cachexia Sarcopenia Muscle 2020, 11, 710–725. [Google Scholar] [CrossRef]
- Chen, Z.; Wittenberg, S.; Auer, T.A.; Bashkuev, M.; Gebert, P.; Fehrenbach, U.; Geisel, D.; Graef, F.; Maerdian, S.; Tsitsilonis, S. The Effect of Fat Distribution on the Inflammatory Response of Multiple Trauma Patients-A Retrospective Study. Life 2021, 11, 1243. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.B.; Choi, M.H.; Song, M.; Lee, J.H.; Lee, I.S.; Lee, M.A.; Hong, T.H.; Jung, E.S.; Choi, M.G. Impact of preoperative body compositions on survival following resection of biliary tract cancer. J. Cachexia Sarcopenia Muscle 2019, 10, 794–802. [Google Scholar] [CrossRef]
- Maia, L.A.; Cruz, F.F.; de Oliveira, M.V.; Samary, C.S.; Fernandes, M.V.S.; Trivelin, S.A.A.; Rocha, N.N.; Gama de Abreu, M.; Pelosi, P.; Silva, P.L.; et al. Effects of Obesity on Pulmonary Inflammation and Remodeling in Experimental Moderate Acute Lung Injury. Front. Immunol. 2019, 10, 1215. [Google Scholar] [CrossRef]
- Kordonowy, L.L.; Burg, E.; Lenox, C.C.; Gauthier, L.M.; Petty, J.M.; Antkowiak, M.; Palvinskaya, T.; Ubags, N.; Rincón, M.; Dixon, A.E.; et al. Obesity is associated with neutrophil dysfunction and attenuation of murine acute lung injury. Am. J. Respir. Cell. Mol. Biol. 2012, 47, 120–127. [Google Scholar] [CrossRef]
- Marques, M.B.; Langouche, L. Endocrine, metabolic, and morphologic alterations of adipose tissue during critical illness. Crit. Care Med. 2013, 41, 317–325. [Google Scholar] [CrossRef]
- Zhen, Y.; Ye, X.; Wang, L. Development of Nursing Rounds Checklist for Patients with Severe Abdominal Trauma. J. Nurs. 2021, 28, 15–19. [Google Scholar] [CrossRef]
- Gonzalez, M.C.; Pastore, C.A.; Orlandi, S.P.; Heymsfield, S.B. Obesity paradox in cancer: New insights provided by body composition. Am. J. Clin. Nutr. 2014, 99, 999–1005. [Google Scholar] [CrossRef]
- Tsujimoto, T.; Kajio, H. Abdominal Obesity Is Associated With an Increased Risk of All-Cause Mortality in Patients With HFpEF. J. Am. Coll. Cardiol. 2017, 70, 2739–2749. [Google Scholar] [CrossRef]
- Cheng, X.; Zhang, Y.; Wang, C.; Deng, W.; Wang, L.; Duanmu, Y.; Li, K.; Yan, D.; Xu, L.; Wu, C.; et al. The optimal anatomic site for a single slice to estimate the total volume of visceral adipose tissue by using the quantitative computed tomography (QCT) in Chinese population. Eur. J. Clin. Nutr. 2018, 72, 1567–1575. [Google Scholar] [CrossRef]
- Moisey, L.L.; Mourtzakis, M.; Cotton, B.A.; Premji, T.; Heyland, D.K.; Wade, C.E.; Bulger, E.; Kozar, R.A. Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit. Care 2013, 17, R206. [Google Scholar] [CrossRef]
- Poros, B.; Irlbeck, T.; Probst, P.; Volkmann, A.; Paprottka, P.; Bocker, W.; Irlbeck, M.; Weig, T. Impact of pathologic body composition assessed by CT-based anthropometric measurements in adult patients with multiple trauma: A retrospective analysis. Eur. J. Trauma Emerg. Surg. 2021, 47, 1089–1103. [Google Scholar] [CrossRef]
- McCusker, A.; Khan, M.; Kulvatunyou, N.; Zeeshan, M.; Sakran, J.V.; Hayek, H.; O’Keeffe, T.; Hamidi, M.; Tang, A.; Joseph, B. Sarcopenia defined by a computed tomography estimate of the psoas muscle area does not predict frailty in geriatric trauma patients. Am. J. Surg. 2019, 218, 261–265. [Google Scholar] [CrossRef]
- Docimo, S., Jr.; Lamparello, B.; Cohen, M.F.; Kopatsis, A.; Vinces, F. Utilizing quantitative measures of visceral adiposity in evaluating trauma patient outcomes. Int. J. Surg. 2015, 21, 51–56. [Google Scholar] [CrossRef]
- Collier, B.; Dossett, L.; Shipman, J.; Day, M.; Lawson, G.; Sawyer, R.; May, A. Visceral adiposity is not associated with inflammatory markers in trauma patients. J. Trauma 2010, 68, 57–61. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).