Novel Impedance-pH Parameters in Pre-Bariatric Assessment of Patients: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
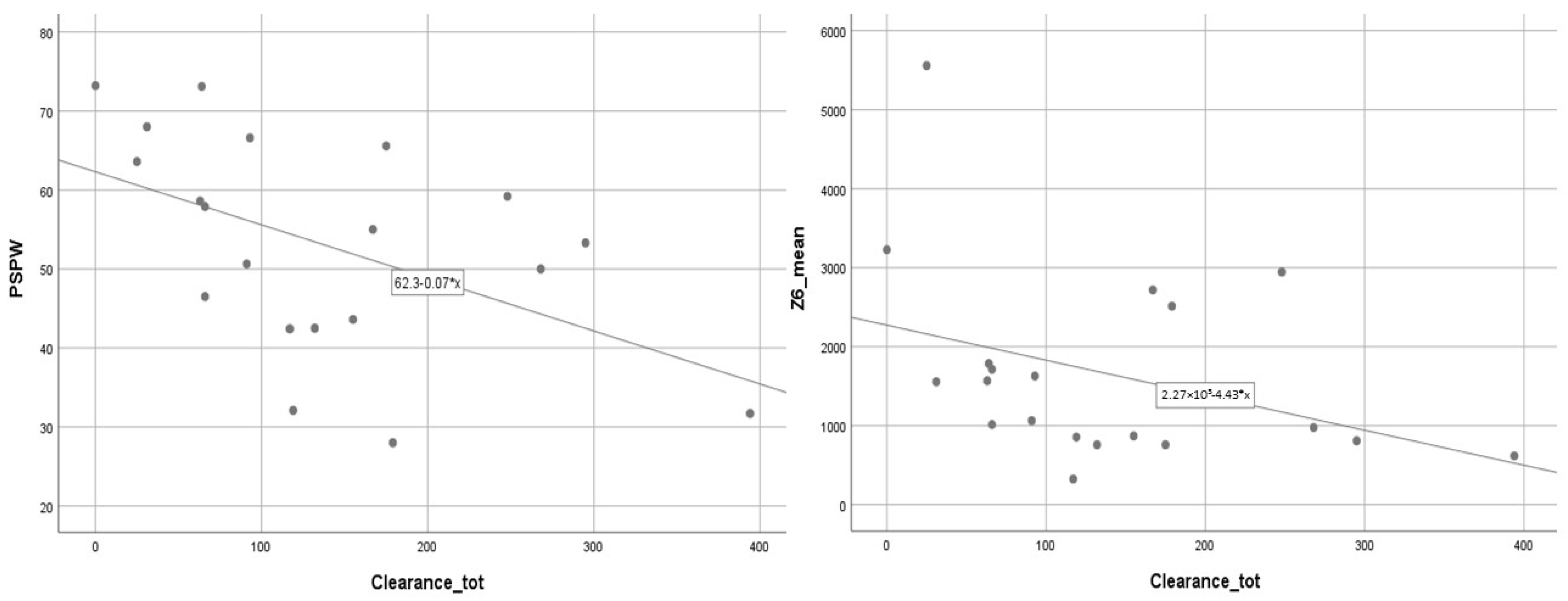
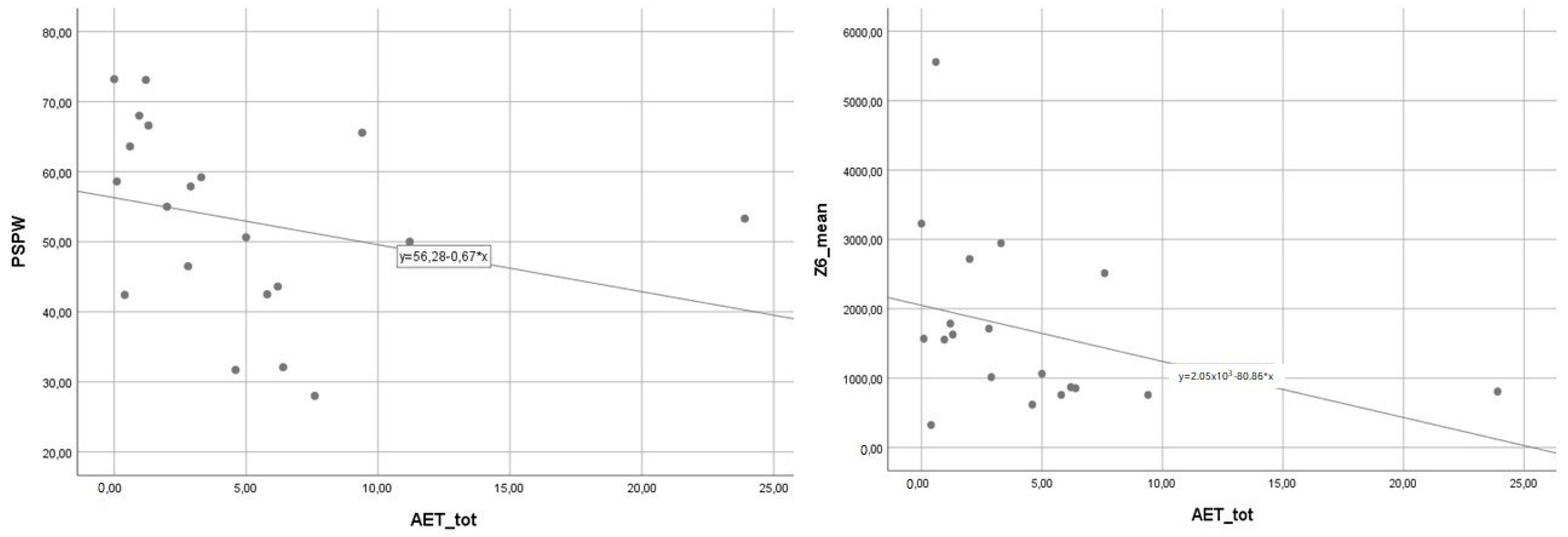
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kristo, I.; Paireder, M.; Jomrich, G.; Felsenreich, D.M.; Fischer, M.; Hennerbichler, F.P.; Langer, F.B.; Prager, G.; Schoppmann, S.F. Silent Gastroesophageal Reflux Disease in Patients with Morbid Obesity Prior to Primary Metabolic Surgery. Obes. Surg. 2020, 30, 4885–4891. [Google Scholar] [CrossRef] [PubMed]
- Lemme, E.M.O.; Alvariz, A.C.; Pereira, G.L.C. Esophageal Functional Disorders in the Pre-Operatory Evaluation of Bariatric Surgery. Arq. Gastroenterol. 2021, 58, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Gyawali, C.P.; Kahrilas, P.J.; Savarino, E.; Zerbib, F.; Mion, F.; Smout, A.; Vaezi, M.; Sifrim, D.; Fox, M.R.; Vela, M.F.; et al. Modern diagnosis of GERD: The Lyon Consensus. Gut 2018, 67, 1351–1362. [Google Scholar] [CrossRef]
- Zentilin, P.; Iiritano, E.; Dulbecco, P.; Bilardi, C.; Savarino, E.; De Conca, S.; Parodi, A.; Reglioni, S.; Vigneri, S.; Savarino, V. Normal values of 24-h ambulatory intraluminal impedance combined with pH-metry in subjects eating a Mediterranean diet. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2006, 38, 226–232. [Google Scholar] [CrossRef]
- Iovino, P.; Theron, B.; Prew, S.; Menon, S.; Trudgill, N. The mechanisms associated with reflux episodes in ambulant subjects with gastro-esophageal reflux disease. Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2021, 33, e14023. [Google Scholar] [CrossRef]
- Blevins, C.H.; Dierkhising, R.A.; Geno, D.M.; Johnson, M.L.; Vela, M.F.; Ravi, K.; Iyer, P.G.; Katzka, D.A. Obesity and GERD impair esophageal epithelial permeability through 2 distinct mechanisms. Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2018, 30, e13403. [Google Scholar] [CrossRef]
- Frazzoni, M.; Savarino, E.; de Bortoli, N.; Martinucci, I.; Furnari, M.; Frazzoni, L.; Mirante, V.G.; Bertani, H.; Marchi, S.; Conigliaro, R.; et al. Analyses of the Post-reflux Swallow-induced Peristaltic Wave Index and Nocturnal Baseline Impedance Parameters Increase the Diagnostic Yield of Impedance-pH Monitoring of Patients with Reflux Disease. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2016, 14, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Frazzoni, L.; Frazzoni, M.; de Bortoli, N.; Tolone, S.; Furnari, M.; Martinucci, I.; Bertani, H.; Marchi, S.; Conigliaro, R.; Fuccio, L.; et al. Postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance can link PPI-responsive heartburn to reflux better than acid exposure time. Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2017, 29, e13116. [Google Scholar] [CrossRef]
- Savarino, E.; Frazzoni, M.; Marabotto, E.; Zentilin, P.; Iovino, P.; Costantini, M.; Tolone, S.; Battaglia, E.; Cicala, M.; Usai-Satta, P.; et al. A SIGE-SINGEM-AIGO technical review on the clinical use of esophageal reflux monitoring. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2020, 52, 966–980. [Google Scholar] [CrossRef]
- Friedenberg, F.K.; Xanthopoulos, M.; Foster, G.D.; Richter, J.E. The association between gastroesophageal reflux disease and obesity. Am. J. Gastroenterol. 2008, 103, 2111–2122. [Google Scholar] [CrossRef]
- El-Serag, H.B.; Tran, T.; Richardson, P.; Ergun, G. Anthropometric correlates of intragastric pressure. Scand. J. Gastroenterol. 2006, 41, 887–891. [Google Scholar] [CrossRef] [PubMed]
- Fisher, B.L.; Pennathur, A.; Mutnick, J.L.; Little, A.G. Obesity correlates with gastroesophageal reflux. Dig. Dis. Sci. 1999, 44, 2290–2294. [Google Scholar] [CrossRef]
- Heimgartner, B.; Herzig, M.; Borbély, Y.; Kröll, D.; Nett, P.; Tutuian, R. Symptoms, endoscopic findings and reflux monitoring results in candidates for bariatric surgery. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2017, 49, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Iovino, P.; Mohammed, I.; Anggiansah, A.; Anggiansah, R.; Cherkas, L.F.; Spector, T.D.; Trudgill, N.J. A study of pathophysiological factors associated with gastro-esophageal reflux disease in twins discordant for gastro-esophageal reflux symptoms. Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2013, 25, 650–656. [Google Scholar] [CrossRef]
- Frazzoni, M.; de Bortoli, N.; Frazzoni, L.; Furnari, M.; Martinucci, I.; Tolone, S.; Farioli, A.; Marchi, S.; Fuccio, L.; Savarino, V.; et al. Impairment of chemical clearance and mucosal integrity distinguishes hypersensitive esophagus from functional heartburn. J. Gastroenterol. 2017, 52, 444–451. [Google Scholar] [CrossRef]
- Frazzoni, M.; Manta, R.; Mirante, V.G.; Conigliaro, R.; Frazzoni, L.; Melotti, G. Esophageal chemical clearance is impaired in gastro-esophageal reflux disease—A 24-h impedance-pH monitoring assessment. Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2013, 25, 399–406.e295. [Google Scholar] [CrossRef] [PubMed]
- Rengarajan, A.; Savarino, E.; Della Coletta, M.; Ghisa, M.; Patel, A.; Gyawali, C.P. Mean Nocturnal Baseline Impedance Correlates with Symptom Outcome When Acid Exposure Time Is Inconclusive on Esophageal Reflux Monitoring. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2020, 18, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Ward, Z.J.; Bleich, S.N.; Cradock, A.L.; Barrett, J.L.; Giles, C.M.; Flax, C.; Long, M.W.; Gortmaker, S.L. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. N. Engl. J. Med. 2019, 381, 2440–2450. [Google Scholar] [CrossRef]
- Santonicola, A.; Cersosimo, G.; Angrisani, L.; Gagliardi, M.; Ferraro, L.; Iovino, P. Nonadherence to Micronutrient Supplementation After Bariatric Surgery: Results from an Italian Internet-Based Survey. J. Am. Nutr. Assoc. 2022, 41, 11–19. [Google Scholar] [CrossRef]
- Iannelli, A.; Sebastianelli, L.; Frey, S.; Vanbiervliet, G.; Santonicola, A.; Angrisani, L.; Schiavo, L.; Iovino, P. Reply to Letter Regarding “Sleeve Gastrectomy, GERD and Barrett’s Esophagus: It is time for objective testing”. Obes. Surg. 2019, 29, 2314–2315. [Google Scholar] [CrossRef]
- Santonicola, A.; Angrisani, L.; Vitiello, A.; Tolone, S.; Trudgill, N.J.; Ciacci, C.; Iovino, P. Hiatal hernia diagnosis prospectively assessed in obese patients before bariatric surgery: Accuracy of high-resolution manometry taking intraoperative diagnosis as reference standard. Surg. Endosc. 2020, 34, 1150–1156. [Google Scholar] [CrossRef]
- Santonicola, A.; Ruggiero, L.; Palma, R.; Angrisani, L.; Iovino, P. Gerd symptoms after laparoscopic Roux-en-Y gastric bypass: An emerging scenario. Int. J. Obes. 2022, 46, 1076–1078. [Google Scholar] [CrossRef] [PubMed]
- Rogers, B.D.; Gyawali, C.P. Editorial: Post-reflux swallow-induced peristaltic wave in eosinophilic oesophagitis-more questions than answers? Aliment. Pharmacol. Ther. 2021, 54, 188–189. [Google Scholar] [CrossRef] [PubMed]
- Sifrim, D.; Roman, S.; Savarino, E.; Bor, S.; Bredenoord, A.J.; Castell, D.; Cicala, M.; de Bortoli, N.; Frazzoni, M.; Gonlachanvit, S.; et al. Normal values and regional differences in oesophageal impedance-pH metrics: A consensus analysis of impedance-pH studies from around the world. Gut 2020, 70, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Frazzoni, L.; Frazzoni, M.; De Bortoli, N.; Ribolsi, M.; Tolone, S.; Russo, S.; Conigliaro, R.L.; Penagini, R.; Fuccio, L.; Zagari, R.M.; et al. Application of Lyon Consensus criteria for GORD diagnosis: Evaluation of conventional and new impedance-pH parameters. Gut 2022, 71, 1062–1067. [Google Scholar] [CrossRef]
| n.9 (45%) OB with GERD | n.11 (55%) OB without GERD | p | |
|---|---|---|---|
| Gender | |||
| 2 (22.2%) | 5 (45.5%) | 0.27 |
| 7 (77.8%) | 6 (54.5%) | |
| Age | 34.56 (27.6–41.45) | 43.27 (36.59–49.96) | 0.06 |
| BMI (Kg/m2) | 45.48 (42–48.95) | 44.86 (41.63–48.09) | 0.74 |
| AET (%) | 6.4 (5.4–10.3) | 1.2 (0.4–2.8) | <0.001 |
| DeMeester score | 24.9 (18.95–29.6) | 3.7 (2–8.9) | <0.001 |
| Acid clearance time (s) | |||
| 175 (125.5–281.5) | 66 (31–117) | 0.003 |
| 113 (55.5–247) | 64 (31–117) | 0.201 |
| 368 (71.5–483) | 0 (0–99) | 0.007 |
| OB Pts with ACT total > 74 s [4] | 9 (100%) | 4 (36.4%) | 0.003 |
| Number of total reflux episodes | |||
| 71 (55.5–80) | 57 (29–71) | 0.080 |
| 59 (43.5–75.5) | 39 (26–62) | 0.152 |
| 10 (3–19) | 5 (1–13) | 0.456 |
| Number of acid reflux episodes | |||
| 47 (39–72.5) | 16 (6–33) | <0.001 |
| 39 (32–68.5) | 14 (6–28) | 0.001 |
| 10 (2.5–17) | 1 (0–4) | 0.038 |
| Number of non-acid reflux episodes | |||
| 8 (6.5–17.5) | 20 (13–56) | 0.020 |
| 8 (4.5–15.5) | 20 (11–39) | 0.020 |
| 1 (0–2.5) | 4 (0–6) | 0.261 |
| MNBI (Ω) | |||
| 3043.2 | 2553.6 | 0.152 |
| (2338.8–4678.3) | (1990.6–3049.5) | ||
| 1976.5 | 1610.4 | 0.261 |
| (1773.35–2924.43) | (1167–2366.5) | ||
| 1427.13 | 1739 | 0.824 |
| (951.95–3017.9) | (1041.8–2851.8) | ||
| 2035.9 | 2321.4 | 0.456 |
| (1295.35–3073.75) | (1634.7–530.9) | ||
| 1146.5 | 1493.7 | 0.80 |
| (837.05–1609.15) | (1346.1–2579.2) | ||
| 855.4 | 1714.1 | 0.010 |
| (758.45–1019.68) | (1555.1–2944.9) | ||
| OB Pts with MNBI < 2292 (Ω) | 8 (89%) | 7 (64%) | 0.2 |
| PSPW index (%) | 43.6 (31.89–51.96) | 59.2 (55–68) | 0.007 |
| OB Pts with PSPW index < 61% | 8 (89%) | 6 (55%) | 0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gagliardi, M.; Santonicola, A.; Palma, R.; Angrisani, L.; Trudgill, N.J.; Iovino, P. Novel Impedance-pH Parameters in Pre-Bariatric Assessment of Patients: A Pilot Study. J. Clin. Med. 2023, 12, 940. https://doi.org/10.3390/jcm12030940
Gagliardi M, Santonicola A, Palma R, Angrisani L, Trudgill NJ, Iovino P. Novel Impedance-pH Parameters in Pre-Bariatric Assessment of Patients: A Pilot Study. Journal of Clinical Medicine. 2023; 12(3):940. https://doi.org/10.3390/jcm12030940
Chicago/Turabian StyleGagliardi, Mario, Antonella Santonicola, Rossella Palma, Luigi Angrisani, Nigel J. Trudgill, and Paola Iovino. 2023. "Novel Impedance-pH Parameters in Pre-Bariatric Assessment of Patients: A Pilot Study" Journal of Clinical Medicine 12, no. 3: 940. https://doi.org/10.3390/jcm12030940
APA StyleGagliardi, M., Santonicola, A., Palma, R., Angrisani, L., Trudgill, N. J., & Iovino, P. (2023). Novel Impedance-pH Parameters in Pre-Bariatric Assessment of Patients: A Pilot Study. Journal of Clinical Medicine, 12(3), 940. https://doi.org/10.3390/jcm12030940









