Investigation of the Relationship between Right Coronary Artery–Aorta Angle and Coronary Artery Disease and Associated Risk Factors
Abstract
1. Introduction
2. Materials and Methods
2.1. Sampling and Data Collection
2.2. CCTA Scanning Protocols and Image Reconstruction
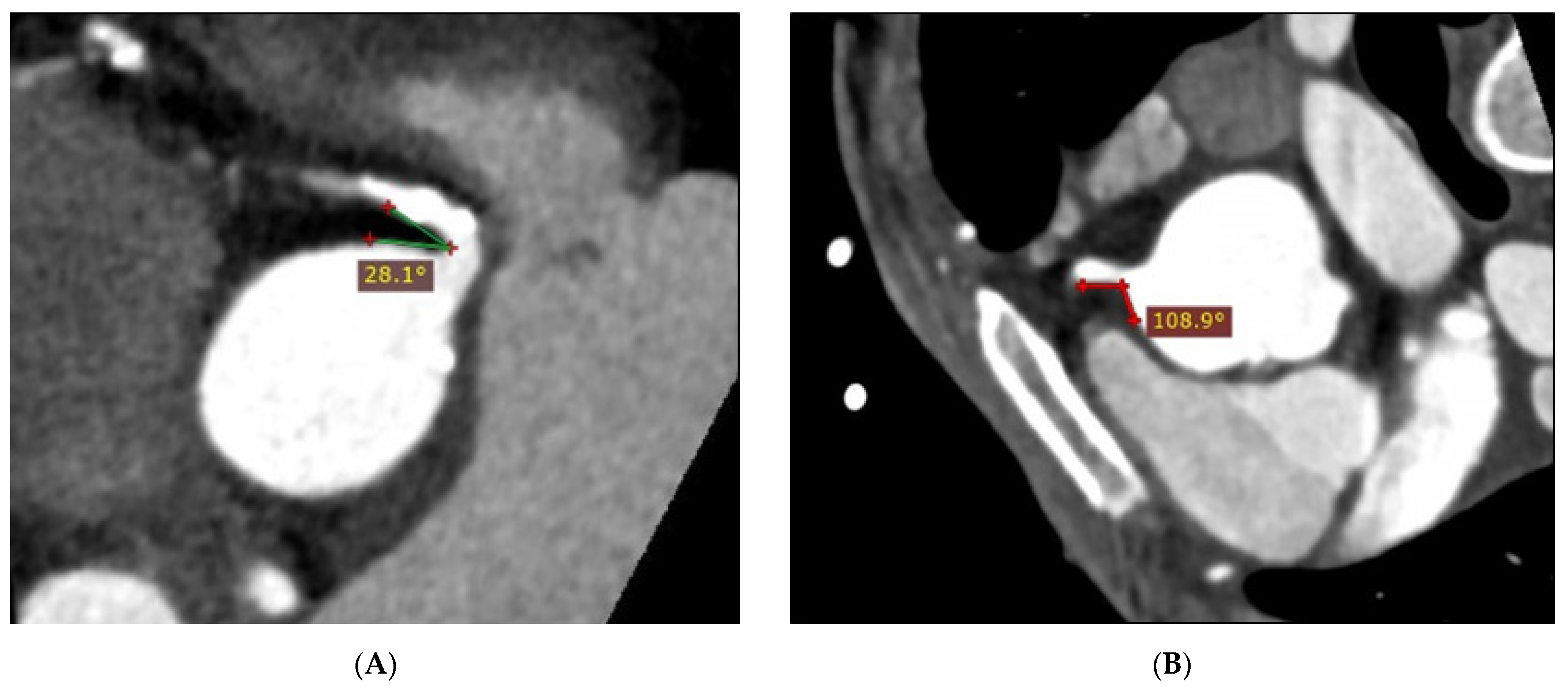
2.3. Coronary Angle Measurement
2.4. Statistical Analysis
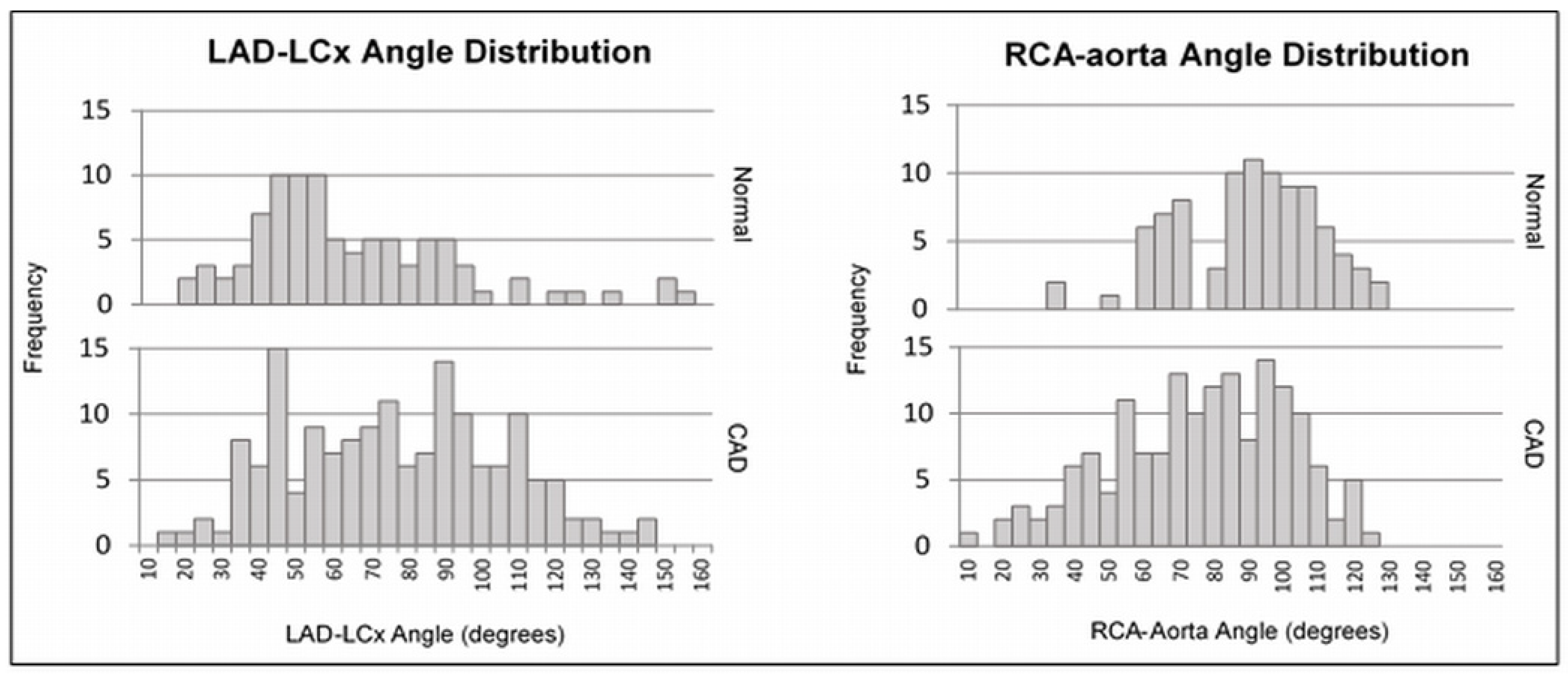
3. Results
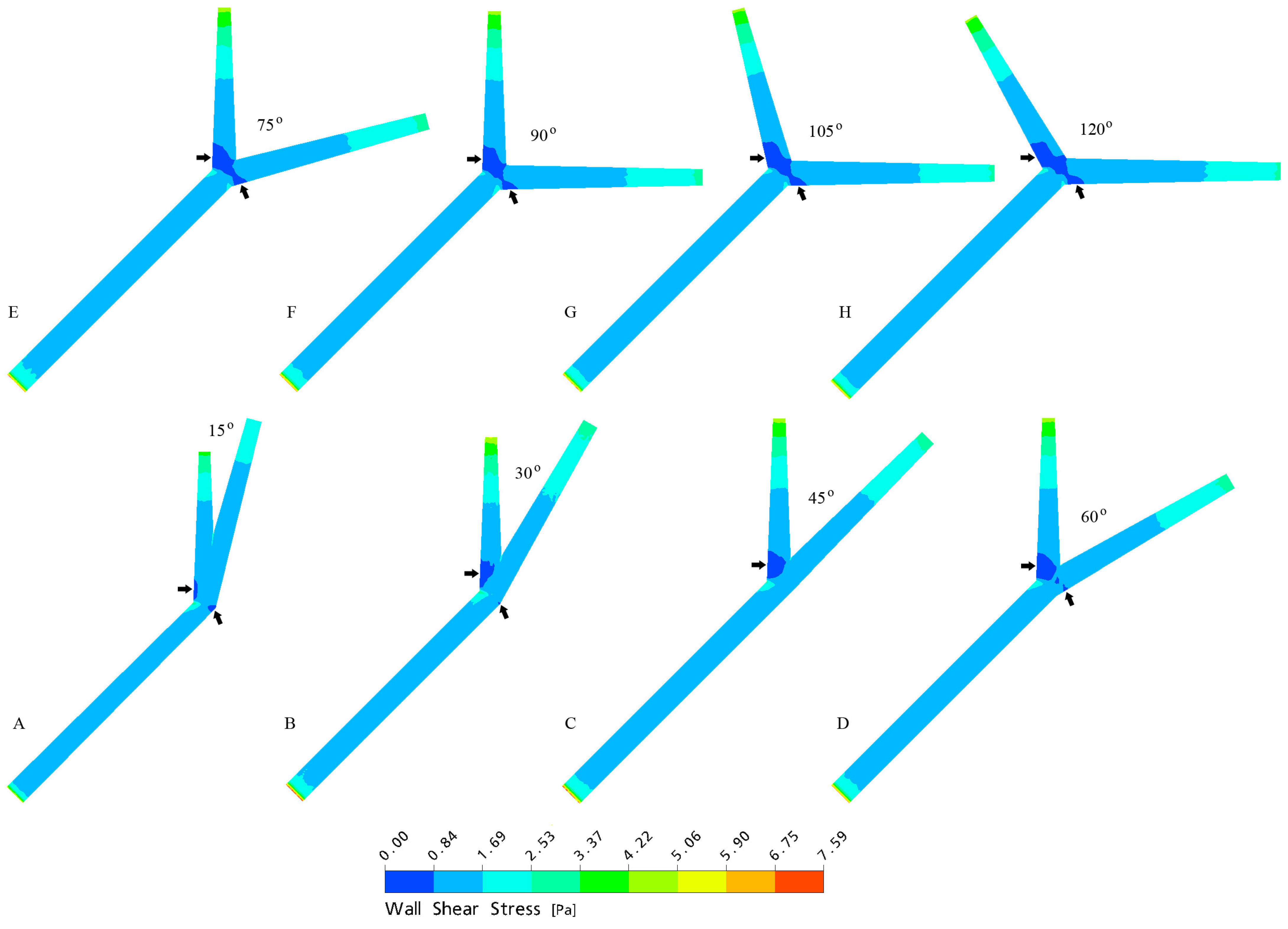
4. Discussion
4.1. Relationship between RCA–Aorta Angle and CAD
4.2. RCA–Aorta Angle and CAD Risk Factors
4.3. Relationship between LAD–LCx Angle and CAD
4.4. LAD–LCx Angle and CAD Risk Factors
4.5. Study Limitations and Directions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Australian Government. Australia’s Health; Australian Institute of Health and Welfare: Sydney, Australia, 2020.
- National Heart Foundation of Australia. Economic Cost of Acute Coronary Syndrome in Australia: The Cost to Individuals and Their Families; National Heart Foundation of Australia: Melbourne, Australia, 2018. [Google Scholar]
- Buckley, T. Alterations of cardiovascular function across the life span. In Understanding Pathophysiology; Craft, J., Gordon, C., Huether, S., McCance, K., Brashers, V., Rote, N., Eds.; Elsevier: Chatswood, Australia, 2017; pp. 610–679. [Google Scholar]
- Juan, Y.; Tsay, P.; Shen, W.; Yeh, C.; Wen, M.; Wan, Y. Comparison of the left main coronary bifurcating angle among patients with normal, non-significantly and significantly stenosed left coronary arteries. Sci. Rep. 2017, 7, 1515–1518. [Google Scholar] [CrossRef]
- Moon, S.; Byun, J.; Kim, J.; Kim, S.; Kim, K.; Jung, J.; Kang, D.; Yang, J.; Choi, J.; Jang, I.; et al. Clinical usefulness of the angle between left main coronary artery and left anterior descending coronary artery for the evaluation of obstructive coronary artery disease. PLoS ONE 2018, 13, e0202249. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Granillo, G.; Rosales, M.; Degrossi, E.; Durbano, I.; Rodriguez, A. Multislice CT coronary angiography for the detection of burden, morphology and distribution of atherosclerotic plaques in the left main bifurcation. Int. J. Cardiovasc. Imaging 2007, 23, 389–392. [Google Scholar] [CrossRef]
- Sun, Z. Coronary CT angiography in coronary artery disease: Correlation between virtual intravascular endoscopic appearances and left bifurcation angulation and coronary plaques. BioMed Res. Int. 2013, 2013, 732059. [Google Scholar] [CrossRef]
- Sun, Z.; Cao, Y. Multislice CT angiography assessment of left coronary artery: Correlation between bifurcation angle and dimensions and development of coronary artery disease. Eur. J. Radiol. 2011, 79, e90–e95. [Google Scholar] [CrossRef] [PubMed]
- Chaichana, T.; Sun, Z.; Jewkes, J. Computation of hemodynamics in the left coronary artery with variable angulations. J. Biomech. 2011, 44, 1869–1878. [Google Scholar] [CrossRef]
- Liu, Z.; Zhao, S.; Li, Y.; Shen, F.; Qi, Y.; Wang, Q. Influence of coronary bifurcation angle on atherosclerosis. Acta Mech. Sin. 2019, 35, 1269–1278. [Google Scholar] [CrossRef]
- Sun, Z.; Chaichana, T. An investigation of correlation between left coronary bifurcation angle and hemodynamic changes in coronary stenosis by coronary computed tomography angiography-derived computational fluid dynamics. Quant. Imaging Med. Surg. 2017, 7, 537–548. [Google Scholar] [CrossRef]
- Zhang, B.; Jin, Y.; Wang, X.; Zeng, T.; Wang, L. Numerical simulation of transient blood flow through the left coronary artery with varying degrees of bifurcation angles. J. Mech. Med. Biol. 2017, 17, 1750005. [Google Scholar] [CrossRef]
- Sun, Z.; Xu, L.; Fan, Z. Coronary CT angiography in calcified coronary plaques: Comparison of diagnostic accuracy between bifurcation angle measurement and coronary lumen assessment for diagnosing significant coronary stenosis. Int. J. Cardiol. 2016, 203, 78–86. [Google Scholar] [CrossRef]
- Geerlings-Batt, J.; Sun, Z. Evaluation of the relationship between left coronary artery bifurcation angle and coronary artery disease: A systematic review. J. Clin. Med. 2022, 11, 5143. [Google Scholar] [CrossRef]
- Temov, K.; Sun, Z. Coronary computed tomography angiography investigation of the association between left main coronary artery bifurcation angle and risk factors of coronary artery disease. Int. J. Cardiovasc. Imaging 2016, 32, S129–S137. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Zeng, W.; Yu, J.; Lu, J.; Hu, Y.; Diao, N.; Liang, B.; Han, P.; Shi, H. Quantification of left coronary bifurcation angles and plaques by coronary computed tomography angiography for prediction of significant coronary stenosis: A preliminary study with dual-source CT. PLoS ONE 2017, 12, e0174352. [Google Scholar] [CrossRef] [PubMed]
- Ziyrek, M.; Sertdemir, A.; Duran, M. Effect of coronary artery bifurcation angle on atherosclerotic lesion localization distance to the bifurcation site. J. Saudi Heart Assoc. 2020, 32, 399–407. [Google Scholar] [CrossRef]
- Geerlings-Batt, J.; Sun, Z. Coronary computed tomography angiography assessment of relationship between right coronary artery-aorta angle and the development of coronary artery disease. Quant. Imaging Med. Surg. 2022, accepted. [Google Scholar]
- Virmani, R.; Chun, P.; Goldstein, R.; Robinowitz, M.; MacAllister, H. Acute takeoffs of the coronary arteries along the aortic wall and congenital coronary ostial valve-like ridges: Association with sudden death. J. Am. Coll. Cardiol. 1984, 3, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Loukas, M.; Andall, R.; Khan, A.; Patel, K.; Muresian, H.; Spicer, D.; Tubbs, R. The clinical anatomy of high take-off coronary arteries. Clin. Anat. 2016, 29, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, U.; Ferencik, M.; Cury, R.; Pena, A. Coronary CT angiography. J. Nucl. Med. 2006, 47, 797–806. [Google Scholar]
- Kruk, M.; Noll, D.; Achenbach, S.; Mintz, G.; Pręgowski, J.; Kaczmarska, E.; Kryczka, K.; Pracoń, R.; Dzielińska, Z.; Śleszycka, J.; et al. Impact of coronary artery calcium characteristics on accuracy of CT angiography. JACC Cardiovasc. Imaging 2014, 7, 49–58. [Google Scholar] [CrossRef]
- Yan, R.; Miller, J.; Rochitte, C.; Dewey, M.; Niinuma, H.; Clouse, M.; Vavere, A.; Brinker, J.; Lima, J.; Arbab-Zadeh, A. Predictors of inaccurate coronary arterial stenosis assessment by CT angiography. JACC Cardiovasc. Imaging 2013, 6, 963–972. [Google Scholar] [CrossRef]
- Koo, B.; Erglis, A.; Doh, J.; Daniels, D.; Jegere, S.; Kim, H.; Dunning, A.; de France, T.; Lansky, A.; Leipsic, J.; et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter discover-flow (diagnosis of ischemia-causing stenoses obtained via noninvasive fractional flow reserve) study. J. Am. Coll. Cardiol. 2011, 58, 1989–1997. [Google Scholar] [CrossRef] [PubMed]
- Ko, B.; Cameron, J.; Munnur, R.; Wong, D.; Fujisawa, Y.; Sakaguchi, T.; Hirohata, K.; Hislop-Jambrich, J.; Fujimoto, S.; Takamura, K.; et al. Noninvasive CT-derived FFR based on structural and fluid analysis: A comparison with invasive FFR for detection of functionally significant stenosis. J. Am. Coll. Cardiol. 2017, 10, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Tintoiu, I.; Elefteriades, J.; Ursulescu, A.; Underwood, M.; Droc, I. New Approaches to Aortic Diseases from Valve to Abdominal Bifurcation; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Faarvang, A.; Preil, S.; Nielsen, P.; Beck, H.; Kristensen, L.; Rasmussen, L. Smoking is associated with lower amounts of arterial type I collagen and decorin. Atherosclerosis 2016, 247, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Miyama, N.; Dua, M.; Yeung, J.; Schultz, G.; Asagami, T.; Sho, E.; Sho, M.; Dalman, R. Hyperglycemia limits experimental aortic aneurysm progression. J. Vasc. Surg. 2010, 52, 975–983. [Google Scholar] [CrossRef]
- Rabkin, S. Epicardial fat: Properties, function and relationship to obesity. Obes. Rev. 2006, 8, 253–261. [Google Scholar] [CrossRef]
- Cuspidi, C.; Rescaldani, M.; Sala, C.; Grassi, G. Left-ventricular hypertrophy and obesity: A systematic review and meta-analysis of echocardiographic studies. J. Hypertens. 2014, 32, 16–25. [Google Scholar] [CrossRef]
- Chahal, H.; McClelland, R.; Tandri, H.; Jain, A.; Turkbey, E.; Hundley, W.; Barr, R.; Kizer, J.; Lima, J.; Bluemke, D.; et al. Obesity and right ventricular structure and function: The MESA-right ventricle study. Chest 2012, 141, 388–395. [Google Scholar] [CrossRef]
- Miller, N.; Steptoe, A. Association between depressive symptoms and pericardial fat in healthy older men and women. Sci. Rep. 2022, 12, 13959. [Google Scholar] [CrossRef]


| Variables | Normal (n = 91) | CAD (n = 159) | |
|---|---|---|---|
| Age | 52.56 11.27 | 60.25 10.04 | |
| BMI | 28.24 6.40 | 30.83 6.94 | |
| LAD–LCx angle | 67.48 28.73° | 79.39 28.58° | |
| RCA–aorta angle | 19.51° | 79.07 24.88° | |
| Sex | Female | 54 (59.34%) | 66 (41.51%) |
| Male | 37 (40.66%) | 93 (58.49%) | |
| Smoking status | Non-smoker | 75 (82.42%) | 133 (83.65%) |
| Smoker | 16 (17.58%) | 26 (16.35%) | |
| Diabetes | Non-diabetic | 80 (87.91%) | 119 (74.84%) |
| Diabetic | 11 (12.09%) | 40 (25.16%) | |
| Blood pressure | Normal | 53 (58.24%) | 51 (32.08%) |
| Hypertensive | 38 (41.76%) | 108 (67.92%) | |
| Blood cholesterol | Normal | 67 (73.63%) | 80 (50.31%) |
| High blood cholesterol | 24 (26.37%) | 79 (49.69%) | |
| Dependent | Groups | Mean Standard Deviation | p-Value |
|---|---|---|---|
| LAD–LCx | Normal | 67.49 28.73 | 0.002 |
| CAD | 79.39 28.57 | ||
| LAD–LCx | Female | 69.54 28.48 | 0.004 |
| Male | 80.15 58.93 | ||
| LAD–LCx | Non-smoker | 75.36 28.09 | 0.750 |
| Smoker | 73.58 34.24 | ||
| LAD–LCx | Non-diabetic | 73.04 28.65 | 0.037 |
| Diabetic | 82.92 30.00 | ||
| LAD–LCx | Normal | 75.20 30.54 | 0.949 |
| Hypertensive | 74.95 28.22 | ||
| LAD–LCx | Normal | 74.46 29.95 | 0.694 |
| High cholesterol | 75.92 28.07 | ||
| RCA–aorta | Normal | 92.08 19.51 | <0.001 |
| CAD | 79.07 24.88 | ||
| RCA–aorta | Female | 87.15 23.64 | 0.016 |
| Male | 80.71 23.75 | ||
| RCA–aorta | Non-smoker | 85.25 23.84 | 0.016 |
| Smoker | 76.63 22.94 | ||
| RCA–aorta | Non-diabetic | 84.79 23.50 | 0.110 |
| Diabetic | 79.96 25.12 | ||
| RCA–aorta | Normal | 84.99 20.97 | 0.246 |
| Hypertensive | 82.95 25.77 | ||
| RCA–aorta | Normal | 84.80 23.16 | 0.218 |
| High blood-cholesterol | 82.37 24.89 |
| Dependent | Independent | Coefficient | p-Value |
|---|---|---|---|
| LAD–LCx | Age | 0.010 | 0.873 |
| LAD–LCx | BMI | 0.138 | 0.030 |
| LAD–LCx | Calcium score | 0.008 | 0.925 |
| RCA–aorta | Age | 0.018 | 0.771 |
| RCA–aorta | BMI | −0.229 | <0.001 |
| RCA–aorta | Calcium score | 0.012 | 0.852 |
| RCA–aorta | LAD–LCx | −0.053 | 0.407 |
| Dependent | Independents | p-Value |
|---|---|---|
| LAD–LCx | CAD | 0.033 |
| Sex | 0.024 | |
| Age | 0.874 | |
| BMI | 0.101 | |
| CAD * Sex | 0.771 | |
| RCA–aorta | CAD | 0.001 |
| Sex | 0.140 | |
| Age | 0.553 | |
| BMI | 0.010 | |
| CAD * Sex | 0.321 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geerlings-Batt, J.; Gupta, A.; Sun, Z. Investigation of the Relationship between Right Coronary Artery–Aorta Angle and Coronary Artery Disease and Associated Risk Factors. J. Clin. Med. 2023, 12, 1051. https://doi.org/10.3390/jcm12031051
Geerlings-Batt J, Gupta A, Sun Z. Investigation of the Relationship between Right Coronary Artery–Aorta Angle and Coronary Artery Disease and Associated Risk Factors. Journal of Clinical Medicine. 2023; 12(3):1051. https://doi.org/10.3390/jcm12031051
Chicago/Turabian StyleGeerlings-Batt, Jade, Ashu Gupta, and Zhonghua Sun. 2023. "Investigation of the Relationship between Right Coronary Artery–Aorta Angle and Coronary Artery Disease and Associated Risk Factors" Journal of Clinical Medicine 12, no. 3: 1051. https://doi.org/10.3390/jcm12031051
APA StyleGeerlings-Batt, J., Gupta, A., & Sun, Z. (2023). Investigation of the Relationship between Right Coronary Artery–Aorta Angle and Coronary Artery Disease and Associated Risk Factors. Journal of Clinical Medicine, 12(3), 1051. https://doi.org/10.3390/jcm12031051







