The Fate of Pre-Existing L5-S1 Degeneration following Oblique Lumbar Interbody Fusion of L4-L5 and Above
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Surgery
2.3. Demographic Data and Primary Outcome
2.4. Radiological Assessment
2.5. Statistical Analysis
3. Results
3.1. Demographic Data and Primary Outcome
3.2. Radiological Parameters between ASD Group and Non-ASD Group
3.3. Progression of Spinal Stenosis in Follow-Up MRI
3.4. Risk Factors for Symptomatic ASD
3.5. Interaction Effects between Identified Risk Factors
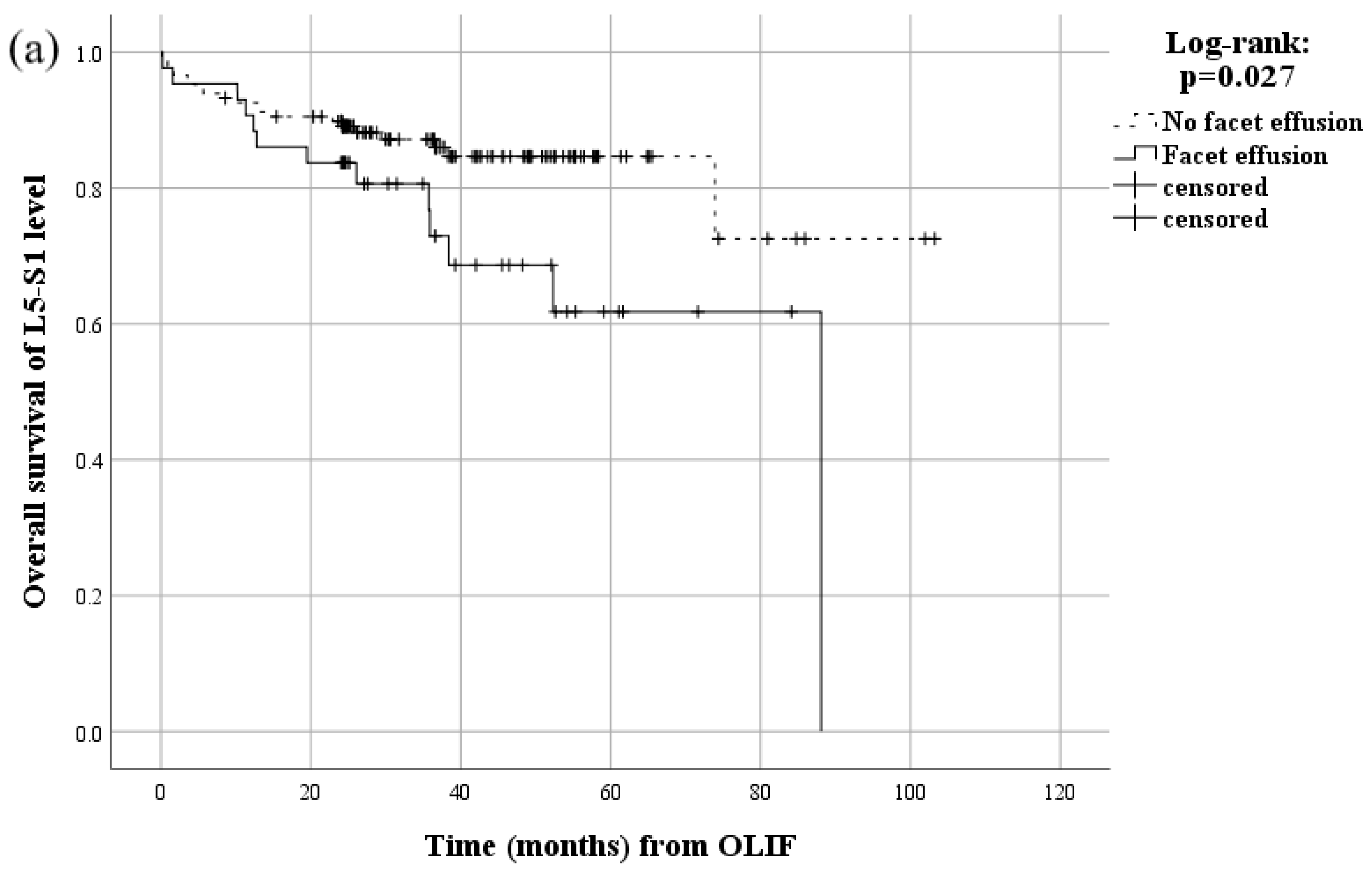
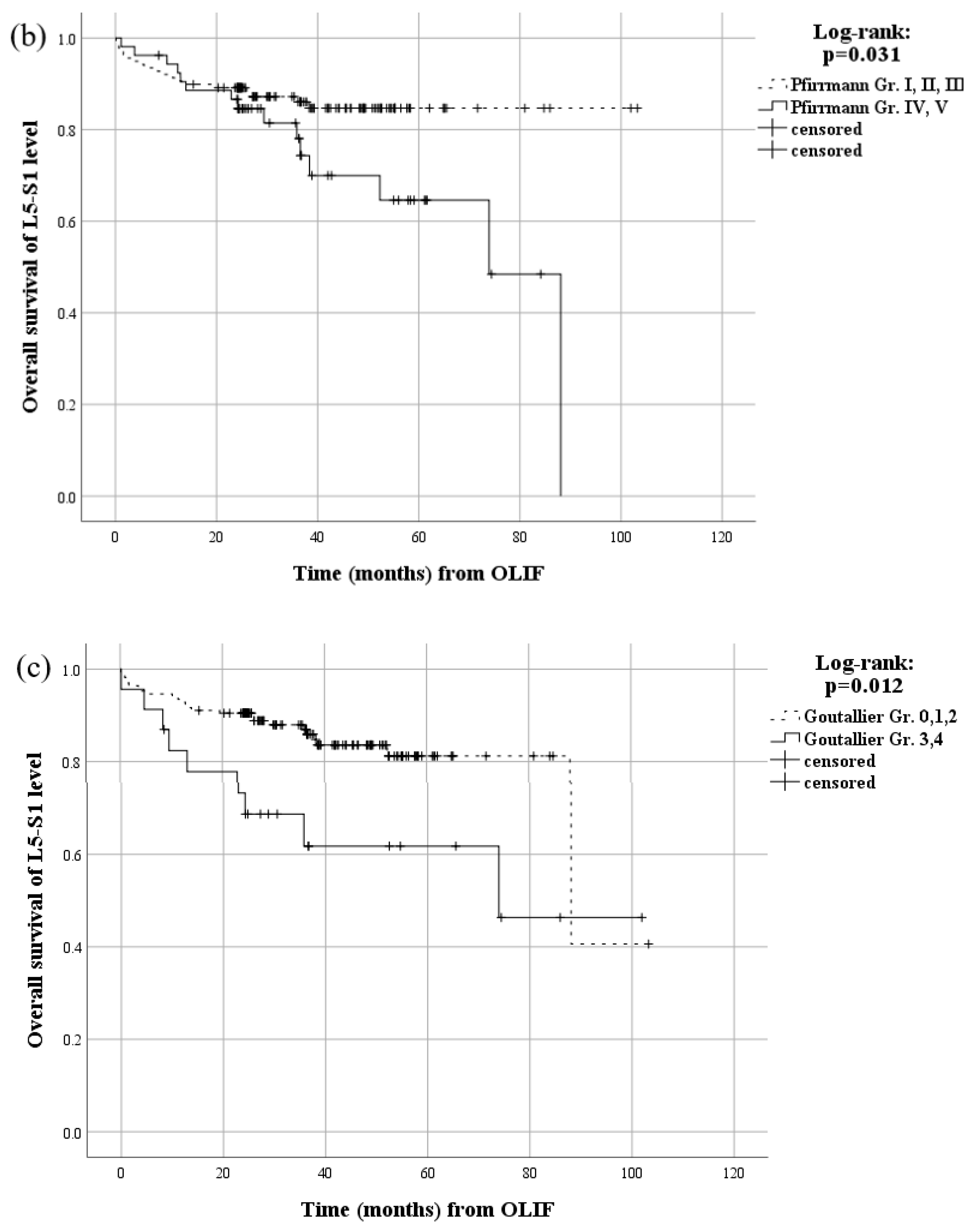
3.6. Survival Analysis of Identified Risk Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Virk, S.S.; Niedermeier, S.; Yu, E.; Khan, S.N. Adjacent segment disease. Orthopedics 2014, 37, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Dekutoski, M.B.; Schendel, M.J.; Ogilvie, J.W.; Olsewski, J.M.; Wallace, L.J.; Lewis, J.L. Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine 1994, 19, 1745–1751. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Du, C.F.; Cai, X.Y.; Gui, W.; Sun, M.S.; Liu, Z.X.; Liu, C.J.; Zhang, C.Q.; Huang, Y.P. Does oblique lumbar interbody fusion promote adjacent degeneration in degenerative disc disease: A finite element analysis. Comput. Biol. Med. 2021, 128, 104122. [Google Scholar] [CrossRef] [PubMed]
- Okuda, S.; Nagamoto, Y.; Matsumoto, T.; Sugiura, T.; Takahashi, Y.; Iwasaki, M. Adjacent segment disease after single segment posterior lumbar interbody fusion for degenerative spondylolisthesis: Minimum 10 years follow-up. Spine 2018, 43, e1384–e1388. [Google Scholar] [CrossRef] [PubMed]
- Miyasaka, K.; Ohmori, K.; Suzuki, K.; Inoue, H. Radiographic analysis of lumbar motion in relation to lumbosacral stability. Investigation of moderate and maximum motion. Spine 2000, 25, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Kim, Y.B.; Park, S.W. Survival Rates and Risk Factors for Cephalad and L5-S1 Adjacent Segment Degeneration after L5 Floating Lumbar Fusion: A Minimum 2-Year Follow-Up. J. Korean Neurosurg. Soc. 2015, 57, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Cheh, G.; Bridwell, K.H.; Lenke, L.G.; Buchowski, J.M.; Daubs, M.D.; Kim, Y.; Baldus, C. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: A minimum 5-year follow-up. Spine 2007, 32, 2253–2257. [Google Scholar] [CrossRef]
- Ghiselli, G.; Wang, J.C.; Bhatia, N.N.; Hsu, W.K.; Dawson, E.G. Adjacent segment degeneration in the lumbar spine. J. Bone Joint Surg. Am. 2004, 86, 1497–1503. [Google Scholar] [CrossRef]
- Ghiselli, G.; Wang, J.C.; Hsu, W.K.; Dawson, E.G. L5-S1 segment survivorship and clinical outcome analysis after L4-L5 isolated fusion. Spine 2003, 28, 1275–1280. [Google Scholar] [CrossRef]
- Li, G.Q.; Tong, T.; Wang, L.F. Comparative analysis of the effects of OLIF and TLIF on adjacent segments after treatment of L4 degenerative lumbar spondylolisthesis. J. Orthop. Res. 2022, 17, 9. [Google Scholar] [CrossRef]
- Takegami, N.; Akeda, K.; Yamada, J.; Imanishi, T.; Fujiwara, T.; Kondo, T.; Takegami, K.; Sudo, A. Incidence and Characteristics of Clinical L5-S1 Adjacent Segment Degeneration after L5 Floating Lumbar Fusion: A Multicenter Study. Asian Spine J. 2022, 9, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, H.; Kanemura, T.; Satake, K.; Ishikawa, Y.; Ouchida, J.; Segi, N.; Yamaguchi, H.; Imagama, S. Comparative Radiographic Outcomes of Lateral and Posterior Lumbar Interbody Fusion in the Treatment of Degenerative Lumbar Kyphosis. Asian Spine J. 2019, 13, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Hyoungmin, K.; Bong-Soon, C.; Sam Yeol, C. Pearls and pitfalls of oblique lateral interbody fusion: A comprehensive narrative review. Neurospine 2022, 19, 163–176. [Google Scholar]
- Kuhns, C.A.; Bridwell, K.H.; Lenke, L.G.; Amor, C.; Lehman, R.A.; Buchowski, J.M.; Edwards, C.; Christine, B. Thoracolumbar deformity arthrodesis stopping at L5—Fate of the L5-S1 disc, minimum 5-year follow-up. Spine 2007, 32, 2771–2776. [Google Scholar] [CrossRef] [PubMed]
- Kasliwal, M.K.; Shaffrey, C.I.; Lenke, L.G.; Dettori, J.R.; Ely, C.G.; Smith, J.S. Frequency, risk factors, and treatment of distal adjacent segment pathology after long thoracolumbar fusion a systematic review. Spine 2012, 37, S165–S179. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.D.; Wang, L.F.; Zhang, J.T.; Wang, P.; Shen, Y. Long fusion arthrodesis stopping at L5 for adult scoliosis fate of L5-S1 disk and risk factors for subsequent disk degeneration. Clin. Spine Surg. 2018, 31, E171–E177. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, B.; Drolet, C.E.; Leveque, J.C.A.; Nemani, V.; Krause, K.L.; Dorsi, M.; Schroerlucke, S.; Shen, J.; Louie, P.K. The impact of interbody approach and lumbar level on segmental, adjacent, and sagittal alignment in degenerative lumbar pathology: A radiographic analysis six months following surgery. Spine J. 2022, 22, 1318–1324. [Google Scholar] [CrossRef] [PubMed]
- Pfirrmann, C.W.; Metzdorf, A.; Zanetti, M.; Hodler, J.; Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001, 26, 1873–1878. [Google Scholar] [CrossRef]
- Weishaupt, D.; Zanetti, M.; Boos, N.; Hodler, J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999, 28, 215–219. [Google Scholar] [CrossRef]
- Goutallier, D.; Postel, J.M.; Bernageau, J.; Lavau, L.; Voisin, M.C. Fatty muscle degeneration in cuff ruptures—preoperative and postoperative evaluation by CT scan. Clin. Orthop. Relat. Res. 1994, 78–83. [Google Scholar]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.-J.; Kim, H.-J.; Chung, S.K.; Kang, H.S. A practical MRI grading system for lumbar foraminal stenosis. AJR Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef] [PubMed]
- Bartynski, W.S.; Lin, L. Lumbar root compression in the lateral recess: MR imaging, conventional myelography, and CT myelography comparison with surgical confirmation. AJNR Am. J. Neuroradiol. 2003, 24, 348–360. [Google Scholar] [PubMed]
- Yilgor, C.; Sogunmez, N.; Boissiere, L.; Yavuz, Y.; Obeid, I.; Kleinstück, F.; Pérez-Grueso, F.J.S.; Acaroglu, E.; Haddad, S.; Mannion, A.F.; et al. Global Alignment and Proportion (GAP) Score: Development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J. Bone Joint Surg. Am. 2017, 99, 1661–1672. [Google Scholar] [CrossRef] [PubMed]
- Lau, K.K.L.; Samartzis, D.; To, N.S.C.; Harada, G.K.; An, H.S.; Wong, A.Y.L. Demographic, surgical, and radiographic risk factors for symptomatic adjacent segment disease after lumbar fusion a systematic review and meta-analysis. J. Bone Joint Surg. Am. 2021, 103, 1438–1450. [Google Scholar] [CrossRef] [PubMed]
- Nachemson, A.L. Instability of the lumbar spine. Pathology, treatment, and clinical evaluation. Neurosurg. Clin. N. Am. 1991, 2, 785–790. [Google Scholar] [CrossRef] [PubMed]
- Bridwell, K.; Edwards, C.; Patel, A.; Rinella, T.; Dellaroca, G.; Berra, A.; Lenke, L. Thoracolumbar deformity arthrodesis to L5 in adult scoliotics: The fate of the L5–S1 disc: Is it protected by a deep-seated L5? Spine J. 2002, 2, 122. [Google Scholar] [CrossRef]
- Chaput, C.; Padon, D.; Rush, J.; Lenehan, E.; Rahm, M. The significance of increased fluid signal on magnetic resonance imaging in lumbar facets in relationship to degenerative spondylolisthesis. Spine 2007, 32, 1883–1887. [Google Scholar] [CrossRef]
- Schizas, C.; Theumann, N.; Burn, A.; Tansey, R.; Wardlaw, D.; Smith, F.W.; Kulik, G. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine 2010, 35, 1919–1924. [Google Scholar] [CrossRef]
- Seok, S.Y.; Cho, J.H.; Lee, H.R.; Lee, D.H.; Hwang, C.J.; Lee, C.S. Risk factors for worsening of sagittal imbalance after revision posterior fusion surgery in patients with adjacent segment disease. World Neurosurg. 2022, 158, E914–E921. [Google Scholar] [CrossRef]
- Sabnis, A.B.; Chamoli, U.; Diwan, A.D. Is L5-S1 motion segment different from the rest? A radiographic kinematic assessment of 72 patients with chronic low back pain. Eur. Spine J. 2018, 27, 1127–1135. [Google Scholar] [CrossRef]
- Hasegawa, K.; Kitahara, K.; Shimoda, H.; Hara, T. Facet joint opening in lumbar degenerative diseases indicating segmental instability. J. Neurosurg. Spine 2010, 12, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Toyoda, H.; Takahashi, S.; Tamai, K.; Suzuki, A.; Hoshino, M.; Terai, H.; Nakamura, H. Relationship between facet joint opening on CT and facet joint effusion on MRI in patients with lumbar spinal stenosis: Analysis of a less invasive decompression procedure. J. Neurosurg. Spine 2022, 36, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, B.D.; Wang, J.; Arnold, P.M.; Hermsmeyer, J.; Norvell, D.C.; Brodke, D.S. Predicting the risk of adjacent segment pathology after lumbar fusion a systematic review. Spine 2012, 37, S123–S132. [Google Scholar] [CrossRef] [PubMed]
- Conaway, W.; Karamian, B.A.; Mao, J.Z.; Kothari, P.; Canseco, J.A.; Bowles, D.R.; DiMaria, S.L.; Semenza, N.C.; Massood, A.J.; Gebeyehu, T.F. The effect of L5-S1 degenerative disc disease on outcomes of L4-L5 fusion. Clin. Spine Surg. 2022, 35, E444–E450. [Google Scholar] [CrossRef] [PubMed]
- Gong, Z.Y.; Li, D.C.; Zou, F.; Liu, S.Y.; Wang, H.L.; Ma, X.S. Low lumbar multifidus muscle status and bone mineral density are important risk factors for adjacent segment disease after lumbar fusion: A case-control study. J. Orthop. Surg. Res. 2022, 17, 8. [Google Scholar] [CrossRef]
- Backhauß, J.-C.; Jansen, O.; Kauczor, H.-U.; Sedaghat, S. Fatty degeneration of the autochthonous muscles is significantly associated with incidental non-traumatic vertebral body fractures of the lower thoracic spine in elderly patients. J. Clin. Med. 2023, 12, 4565. [Google Scholar] [CrossRef]
- Dohzono, S.; Sasaoka, R.; Takamatsu, K.; Nakamura, H. Association between age and trunk muscle area and density in patients with spinal metastases. Asian Spine J. 2022, 16, 677–683. [Google Scholar] [CrossRef]
- Tempel, Z.J.; Gandhoke, G.S.; Bolinger, B.D.; Khattar, N.K.; Parry, P.V.; Chang, Y.F.; Okonkwo, D.O.; Kanter, A.S. The influence of pelvic incidence and lumbar lordosis mismatch on development of symptomatic adjacent level disease following single-level transforaminal lumbar interbody fusion. Neurosurgery 2017, 80, 880–885. [Google Scholar] [CrossRef]
- Dong, S.T.; Li, J.; Jia, X.M.; Zhu, J.Y.; Chen, Y.N.; Yuan, B. Analysis of risk factors for adjacent segment degeneration after minimally invasive transforaminal interbody fusion at lumbosacral spine. Comput. Intell. Neurosci. 2022, 2022, 8. [Google Scholar] [CrossRef]
- Qu, Z.; Deng, B.; Gao, X.; Pan, B.; Sun, W.; Feng, H. The association between Roussouly sagittal alignment type and risk for adjacent segment degeneration following short-segment lumbar interbody fusion: A retrospective cohort study. BMC Musculoskelet. Disord. 2022, 23, 9. [Google Scholar] [CrossRef]
- Takeda, K.; Okada, E.; Shinozaki, Y.; Ozaki, M.; Kono, H.; Yasuda, A.; Suzuki, S.; Tsuji, O.; Nagoshi, N.; Yagi, M.; et al. Risk factors for early-onset radiographical adjacent segment disease in patients with spondylolytic spondylolisthesis after single-level posterior lumbar interbody fusion. Spine J. 2022, 22, 1112–1118. [Google Scholar] [CrossRef] [PubMed]
- Koike, Y.; Kotani, Y.; Terao, H.; Iwasaki, N. Comparison of outcomes of oblique lateral interbody fusion with percutaneous posterior fixation in lateral position and minimally invasive transforaminal lumbar interbody fusion for degenerative spondylolisthesis. Asian Spine J. 2021, 15, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Takaoka, H.; Inage, K.; Eguchi, Y.; Shiga, Y.; Furuya, T.; Maki, S.; Aoki, Y.; Inoue, M.; Fujiyoshi, T.; Miyamoto, T. Comparison between intervertebral oblique lumbar interbody fusion and transforaminal lumbar interbody fusion: A multicenter study. Sci. Rep. 2021, 11, 16673. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.Y.; Tan, J.; Huang, K.; Xie, H.Q. Minimally invasive transforaminal lumbar interbody fusion versus oblique lateral interbody fusion for lumbar degenerative disease: A meta-analysis. BMC Musculoskelet. Disord. 2021, 22, 802. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, H.; Kanemura, T.; Satake, K.; Ishikawa, Y.; Ouchida, J.; Segi, N.; Yamaguchi, H.; Imagama, S. Changes in sagittal alignment following short-level lumbar interbody fusion: Comparison between posterior and lateral lumbar interbody fusions. Asian Spine J. 2019, 13, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Roussouly, P.; Pinheiro-Franco, J.L. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur. Spine J. 2011, 20, 609–618. [Google Scholar] [CrossRef]
- Hu, P.; Yu, M.; Sun, Z.; Li, W.; Jiang, L.; Wei, F.; Liu, X.; Chen, Z.; Liu, Z. Analysis of Global Sagittal Postural Patterns in Asymptomatic Chinese Adults. Asian Spine J. 2016, 10, 282–288. [Google Scholar] [CrossRef]
- Hodges, P.; Holm, A.K.; Hansson, T.; Holm, S. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine 2006, 31, 2926–2933. [Google Scholar] [CrossRef]
- Bagheri, S.R.; Alimohammadi, E.; Zamani Froushani, A.; Abdi, A. Adjacent segment disease after posterior lumbar instrumentation surgery for degenerative disease: Incidence and risk factors. J. Orthop. Surg. 2019, 27, 2309499019842378. [Google Scholar] [CrossRef]
- Lee, J.C.; Kim, Y.; Soh, J.W.; Shin, B.J. Risk factors of adjacent segment disease requiring surgery after lumbar spinal fusion: Comparison of posterior lumbar interbody fusion and posterolateral fusion. Spine 2014, 39, E339–E345. [Google Scholar] [CrossRef]
- Wang, H.; Ma, L.; Yang, D.; Wang, T.; Liu, S.; Yang, S.; Ding, W. Incidence and risk factors of adjacent segment disease following posterior decompression and instrumented fusion for degenerative lumbar disorders. Medicine 2017, 96, e6032. [Google Scholar] [CrossRef]
- Mesregah, M.K.; Yoshida, B.; Lashkari, N.; Abedi, A.; Meisel, H.J.; Diwan, A.; Hsieh, P.T.; Wang, J.C.; Buser, Z.; Yoon, S.T. Demographic, clinical, and operative risk factors associated with postoperative adjacent segment disease in patients undergoing lumbar spine fusions: A systematic review and meta-analysis. Spine J. 2022, 22, 1038–1069. [Google Scholar] [CrossRef]


| Baseline Characteristics | All Patients | ||
|---|---|---|---|
| ASD Group (n = 34) | Non-ASD Group (n = 157) | p-Value | |
| Age (mean ± SD, years) | 69.3 ± 6.8 | 68.5 ± 8.6 | 0.595 |
| Sex, Male (n (%)) | 13 (38.2%) | 59 (37.6%) | 0.943 |
| BMI (mean ± SD, kg/m2) | 25.0 ± 3.4 | 25.1 ± 3.0 | 0.861 |
| Follow-up period (mean ± SD, month) | 45.8 ± 18.4 | 42.1 ± 17.3 | 0.267 |
| Time from OLIF to L5 ESI (mean ± SD, month) | 19.9 ± 20.9 | ||
| Preoperative diagnosis (n (%)) | 0.463 | ||
| Spinal stenosis without SPLT | 11 (32.4) | 38 (24.2) | |
| Degenerative SPLT | 21 (61.8) | 99 (63.1) | |
| Spondylolytic SPLT | 1 (2.9) | 10 (6.4) | |
| Adjacent segment disease | 1 (2.9) | 2 (1.3) | |
| Degenerative lumbar scoliosis | 0 (0.0) | 8 (5.1) | |
| The number of levels that underwent OLIF (n (%)) | 0.297 | ||
| 1 level | 14 (41.2) | 89 (56.7) | |
| 2 levels | 15 (44.1) | 47 (29.9) | |
| 3 levels | 5 (14.7) | 15 (9.6) | |
| 4 levels | 0 (0.0) | 5 (3.2) | |
| 5 levels | 0 (0.0) | 1 (0.6) | |
| Radiologic Parameters | All Patients | ||
|---|---|---|---|
| ASD Group (n = 34) | Non-ASD Group (n = 157) | p-Value | |
| Disc vacuum (n (%)) | 3 (8.8%) | 4 (2.5%) | 0.077 |
| Calcified L5-S1 disc (n (%)) | 3 (9.1%) | 30 (19.1%) | 0.150 |
| Deep-seated L5 (n (%)) | 10 (29.4%) | 55 (35.0%) | 0.531 |
| PI (mean ± SD, degree) | 54.3 ± 8.9 | 54.6 ± 8.6 | 0.850 |
| Preoperative sacral slope (mean ± SD, degree) | 33.2 ± 5.6 | 33.8 ± 7.8 | 0.586 |
| Preoperative pelvic tilt (mean ± SD, degree) | 21.1 ± 8.7 | 21.2 ± 7.5 | 0.936 |
| Preoperative LDI (mean ± SD, percentage) | 70.9 ± 26.9 | 76.0 ± 81.0 | 0.714 |
| Postoperative LDI (mean ± SD, percentage) | 64.0 ± 18.4 | 68.1 ± 36.8 | 0.530 |
| Preoperative PI minus LL (mean ± SD, degree) | 12.2 ± 13.8 | 12.4 ± 13.4 | 0.937 |
| Postoperative PI minus LL (mean ± SD, degree) | 10.2 ± 10.3 | 8.2 ± 9.7 | 0.292 |
| Preoperative SVA (mean ± SD, degree) | 33.8 ± 43.2 | 34.5 ± 47.9 | 0.941 |
| Postoperative SVA (mean ± SD, degree) | 20.6 ± 38.3 | 25.4 ± 33.5 | 0.468 |
| Preoperative flexion–extension ROM in L5-S1 disc (mean ± SD, degree) | 8.0 ± 4.3 | 6.7 ± 4.3 | 0.113 |
| Instability in L5-S1 level (n (%)) | 10 (30.3%) | 39 (24.8%) | 0.514 |
| Lee grade 1 foraminal stenosis (n (%)) | 7 (20.6%) | 33 (21.0%) | 0.955 |
| Bartynski grade 1 lateral recess stenosis (n (%)) | 8 (23.5%) | 24 (15.3%) | 0.243 |
| Pfirrmann grade at L5-S1 disc (n (%)) | 0.102 | ||
| Grade I | 1 (2.9%) | 9 (5.7%) | |
| Grade II | 7 (20.6%) | 30 (19.1%) | |
| Grade III | 11 (32.4%) | 80 (51.0%) | |
| Grade IV | 12 (35.3%) | 31 (19.7%) | |
| Grade V | 3 (8.8%) | 7 (4.5%) | |
| Preoperative grade of facet arthrosis in L5-S1 facet joint (n (%)) | 0.120 | ||
| Grade 0 | 3 (8.8%) | 34 (21.7%) | |
| Grade 1 | 14 (41.2%) | 56 (35.7%) | |
| Grade 2 | 13 (38.2%) | 57 (36.3%) | |
| Grade 3 | 4 (11.8%) | 10 (6.4%) | |
| Facet effusion in L5-S1 level (n (%)) | 13 (38.2%) | 30 (19.1%) | 0.015 |
| Goutallier grade of paraspinal muscle in L5-S1 disc level (n (%)) | 0.014 | ||
| Grade 0 | 0 (0.0%) | 3 (1.9%) | |
| Grade 1 | 4 (11.8%) | 31 (19.7%) | |
| Grade 2 | 21 (61.8%) | 109 (69.4%) | |
| Grade 3 | 6 (17.6%) | 7 (4.5%) | |
| Grade 4 | 3 (8.8%) | 7 (4.5%) | |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p Value | Odds Ratio (95% CI) | p Value | |
| Multi-level OLIF a | 0.103 | 0.098 | ||
| Disc vacuum | 0.097 | 0.563 | ||
| Calcified L5-S1 disc | 0.162 | 0.316 | ||
| Preoperative flexion–extension ROM in L5-S1 disc | 0.115 | 0.082 | ||
| Pfirrmann grade ≥ IV in L5-S1 disc | 2.472 (1.146–5.335) | 0.021 | 2.653 (1.156–6.091) | 0.021 |
| Facet effusion at the L5-S1 level | 2.621 (1.180–5.820) | 0.018 | 2.553 (1.046–6.231) | 0.040 |
| Goutallier grade ≥ 3 of paraspinal muscle at the L5-S1 disc level | 3.677 (1.438–9.404) | 0.007 | 4.473 (1.533–13.047) | 0.006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, D.-H.; Kim, J.H.; Chang, B.-S.; Kim, H.; Kim, D.; Park, S.; Hong, S.H.; Chang, S.Y. The Fate of Pre-Existing L5-S1 Degeneration following Oblique Lumbar Interbody Fusion of L4-L5 and Above. J. Clin. Med. 2023, 12, 7463. https://doi.org/10.3390/jcm12237463
Kang D-H, Kim JH, Chang B-S, Kim H, Kim D, Park S, Hong SH, Chang SY. The Fate of Pre-Existing L5-S1 Degeneration following Oblique Lumbar Interbody Fusion of L4-L5 and Above. Journal of Clinical Medicine. 2023; 12(23):7463. https://doi.org/10.3390/jcm12237463
Chicago/Turabian StyleKang, Dong-Ho, Ji Hwan Kim, Bong-Soon Chang, Hyoungmin Kim, Dongook Kim, Sanghyun Park, Seong Hwa Hong, and Sam Yeol Chang. 2023. "The Fate of Pre-Existing L5-S1 Degeneration following Oblique Lumbar Interbody Fusion of L4-L5 and Above" Journal of Clinical Medicine 12, no. 23: 7463. https://doi.org/10.3390/jcm12237463
APA StyleKang, D.-H., Kim, J. H., Chang, B.-S., Kim, H., Kim, D., Park, S., Hong, S. H., & Chang, S. Y. (2023). The Fate of Pre-Existing L5-S1 Degeneration following Oblique Lumbar Interbody Fusion of L4-L5 and Above. Journal of Clinical Medicine, 12(23), 7463. https://doi.org/10.3390/jcm12237463






