Head-Mounted Displays for Upper Limb Stroke Rehabilitation: A Scoping Review
Abstract
:1. Introduction
- To collect all the available information on the clinical feasibility and effectiveness of HMD use for improving UE motor recovery in people after stroke in a bio-psycho-social view;
- To map relevant data related to the software and hardware characteristics of HMD interventions applied to UE treatment in stroke survivors so far;
- To track information on treatment protocols applied and therapeutic modalities proposed for HMD applications for UE rehabilitation in this population type;
- To identify stroke patients subgroups who could be more responsive to HMD use for increasing UE function.
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Types of Participants
2.4. Types of Interventions and Outcome Measures
2.5. Search Strategy
2.6. Study Selection
2.7. Data Extraction
3. Results

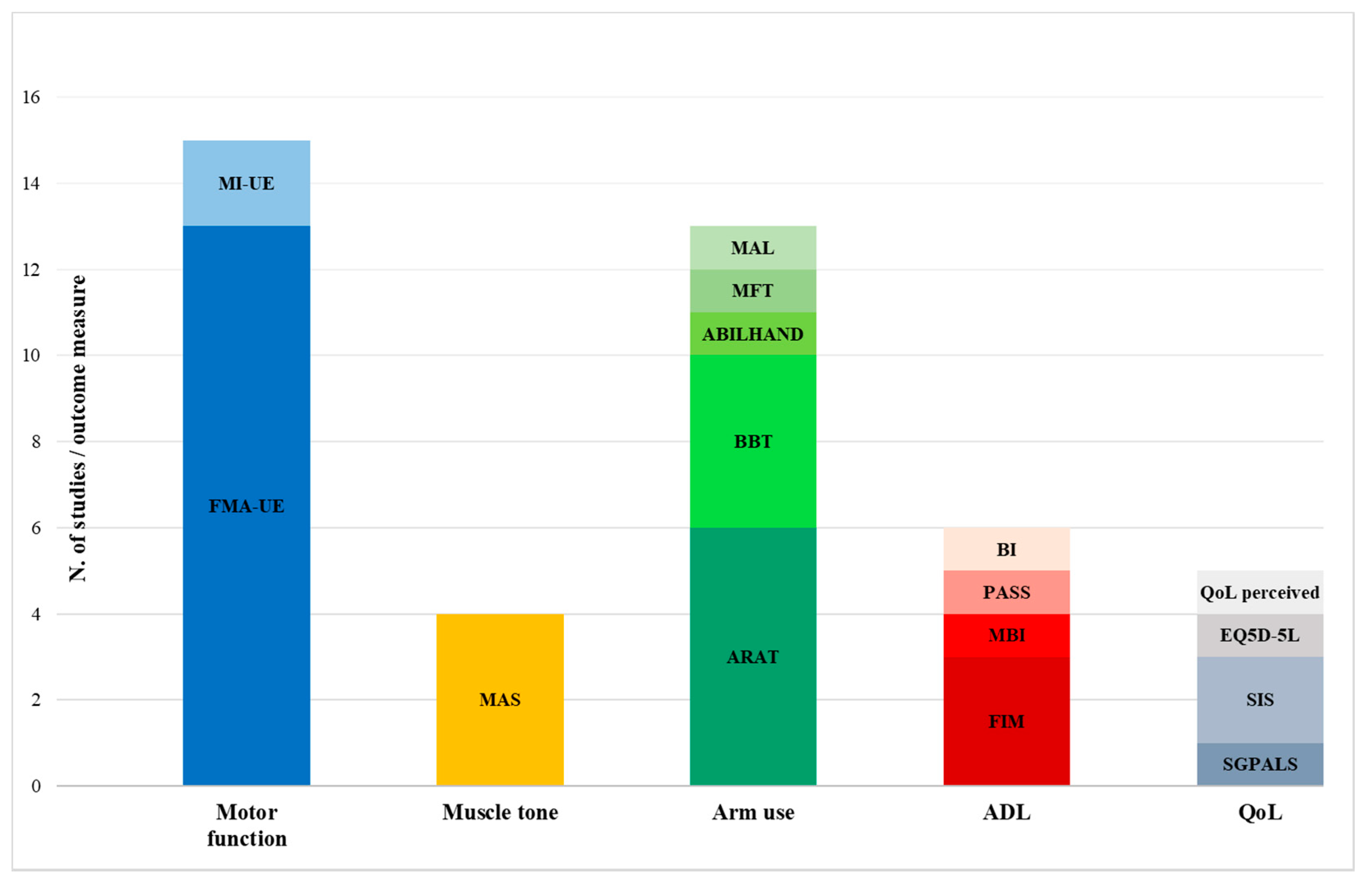
3.1. Motor Function
3.2. Arm Use
3.3. ADL
3.4. Participation
3.5. Side-Effects and Sense of Presence
3.6. Risk of Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviation
References
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.; Sacco, R.L.; Hacke, W.; Fisher, M.; Pandian, J.; Lindsay, P. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int. J. Stroke Off. J. Int. Stroke Soc. 2022, 17, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.-Y. Determinants of the Health-Related Quality of Life for Stroke Survivors. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2015, 24, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Lima, M.J.M.; Brasileiro, I.d.C.; de Lima, T.L.; Braga-Neto, P. Quality of Life after Stroke: Impact of Clinical and Sociodemographic Factors. Clin. Sao Paulo Braz. 2018, 73, e418. [Google Scholar] [CrossRef]
- Gresham, G.E.; Duncan, P.W.; Stason, W.B.; Adams, H.P.; Adelman, A.M.; Alexander, D.N.; Bishop, D.S.; Diller, L.; Donaldson, N.E.; Granger, C.V.; et al. Post-Stroke Rehabilitation: Assessment, Referral and Patient Management. Am. Fam. Physician 1995, 52, 461–470. [Google Scholar]
- Pollock, A.; Farmer, S.E.; Brady, M.C.; Langhorne, P.; Mead, G.E.; Mehrholz, J.; van Wijck, F. Interventions for Improving Upper Limb Function after Stroke. Cochrane Database Syst. Rev. 2014, 2014, CD010820. [Google Scholar] [CrossRef]
- Sampaio-Baptista, C.; Sanders, Z.-B.; Johansen-Berg, H. Structural Plasticity in Adulthood with Motor Learning and Stroke Rehabilitation. Annu. Rev. Neurosci. 2018, 41, 25–40. [Google Scholar] [CrossRef] [PubMed]
- Rossini, P.M.; Calautti, C.; Pauri, F.; Baron, J.-C. Post-Stroke Plastic Reorganisation in the Adult Brain. Lancet Neurol. 2003, 2, 493–502. [Google Scholar] [CrossRef]
- French, B.; Thomas, L.H.; Coupe, J.; McMahon, N.E.; Connell, L.; Harrison, J.; Sutton, C.J.; Tishkovskaya, S.; Watkins, C.L. Repetitive Task Training for Improving Functional Ability after Stroke. Cochrane Database Syst. Rev. 2016, 11, CD006073. [Google Scholar] [CrossRef]
- Kwakkel, G. Intensity of Practice after Stroke: More Is Better. Schweiz. Arch. Neurol. Psychiatr. 2009, 160, 295–298. [Google Scholar]
- Dobkin, B.H. Strategies for Stroke Rehabilitation. Lancet Neurol. 2004, 3, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Lohse, K.R.; Lang, C.E.; Boyd, L.A. Is More Better? Using Metadata to Explore Dose-Response Relationships in Stroke Rehabilitation. Stroke 2014, 45, 2053–2058. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.; Kim, B.; Kim, S.; Martinez, C.; Schweighofer, N. Dosage Matters. Stroke 2019, 50, 1831–1837. [Google Scholar] [CrossRef] [PubMed]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke Rehabilitation. Lancet Lond. Engl. 2011, 377, 1693–1702. [Google Scholar] [CrossRef] [PubMed]
- Rohrbach, N.; Chicklis, E.; Levac, D.E. What Is the Impact of User Affect on Motor Learning in Virtual Environments after Stroke? A Scoping Review. J. Neuroeng. Rehabil. 2019, 16, 79. [Google Scholar] [CrossRef]
- Gutiérrez, R.O.; Galán Del Río, F.; Cano de la Cuerda, R.; Alguacil Diego, I.M.; González, R.A.; Page, J.C.M. A Telerehabilitation Program by Virtual Reality-Video Games Improves Balance and Postural Control in Multiple Sclerosis Patients. NeuroRehabilitation 2013, 33, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Luna-Oliva, L.; Ortiz-Gutiérrez, R.M.; Cano-de la Cuerda, R.; Piédrola, R.M.; Alguacil-Diego, I.M.; Sánchez-Camarero, C.; Martínez Culebras, M.D.C. Kinect Xbox 360 as a Therapeutic Modality for Children with Cerebral Palsy in a School Environment: A Preliminary Study. NeuroRehabilitation 2013, 33, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Gutiérrez, R.; Cano-de-la-Cuerda, R.; Galán-del-Río, F.; Alguacil-Diego, I.M.; Palacios-Ceña, D.; Miangolarra-Page, J.C. A Telerehabilitation Program Improves Postural Control in Multiple Sclerosis Patients: A Spanish Preliminary Study. Int. J. Environ. Res. Public. Health 2013, 10, 5697–5710. [Google Scholar] [CrossRef] [PubMed]
- Campos, E.; Hidrogo, I.; Zavala, G. Impact of Virtual Reality Use on the Teaching and Learning of Vectors. Front. Educ. 2022, 7, 702. [Google Scholar] [CrossRef]
- Mat Rosly, M.; Mat Rosly, H.; Davis Oam, G.M.; Husain, R.; Hasnan, N. Exergaming for Individuals with Neurological Disability: A Systematic Review. Disabil. Rehabil. 2017, 39, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Rüth, M.; Schmelzer, M.; Burtniak, K.; Kaspar, K. Commercial Exergames for Rehabilitation of Physical Health and Quality of Life: A Systematic Review of Randomized Controlled Trials with Adults in Unsupervised Home Environments. Front. Psychol. 2023, 14, 1155569. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual Reality for Stroke Rehabilitation. Cochrane Database Syst. Rev. 2017, 11, CD008349. [Google Scholar] [CrossRef] [PubMed]
- Gelineau, A.; Perrochon, A.; Daviet, J.-C.; Mandigout, S. Compliance with Upper Limb Home-Based Exergaming Interventions for Stroke Patients: A Narrative Review. J. Rehabil. Med. 2022, 54, jrm00325. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; Adey-Wakeling, Z.; Crotty, M.; Lannin, N.A.; George, S.; Sherrington, C. Telerehabilitation Services for Stroke. Cochrane Database Syst. Rev. 2020, 1, CD010255. [Google Scholar] [CrossRef] [PubMed]
- Sardi, L.; Idri, A.; Fernández-Alemán, J.L. A Systematic Review of Gamification in E-Health. J. Biomed. Inform. 2017, 71, 31–48. [Google Scholar] [CrossRef]
- Yavuzer, G.; Senel, A.; Atay, M.B.; Stam, H.J. “Playstation Eyetoy Games” Improve Upper Extremity-Related Motor Functioning in Subacute Stroke: A Randomized Controlled Clinical Trial. Eur. J. Phys. Rehabil. Med. 2008, 44, 237–244. [Google Scholar]
- Cano-Mañas, M.J.; Collado-Vázquez, S.; Rodríguez Hernández, J.; Muñoz Villena, A.J.; Cano-de-la-Cuerda, R. Effects of Video-Game Based Therapy on Balance, Postural Control, Functionality, and Quality of Life of Patients with Subacute Stroke: A Randomized Controlled Trial. J. Healthc. Eng. 2020, 2020, 5480315. [Google Scholar] [CrossRef]
- Slater, M.; Sanchez-Vives, M.V. Enhancing Our Lives with Immersive Virtual Reality. Front. Robot. AI 2016, 3, 74. [Google Scholar] [CrossRef]
- Bohil, C.J.; Alicea, B.; Biocca, F.A. Virtual Reality in Neuroscience Research and Therapy. Nat. Rev. Neurosci. 2011, 12, 752–762. [Google Scholar] [CrossRef]
- Combe, T.; Chardonnet, J.-R.; Merienne, F.; Ovtcharova, J. CAVE and HMD: Distance Perception Comparative Study. Virtual Real. 2023, 27, 2003–2013. [Google Scholar] [CrossRef]
- Helou, S.; Khalil, N.; Daou, M.; El Helou, E. Virtual Reality for Healthcare: A Scoping Review of Commercially Available Applications for Head-Mounted Displays. Digit. Health 2023, 9, 20552076231178619. [Google Scholar] [CrossRef]
- Baashar, Y.; Alkawsi, G.; Wan Ahmad, W.N.; Alomari, M.A.; Alhussian, H.; Tiong, S.K. Towards Wearable Augmented Reality in Healthcare: A Comparative Survey and Analysis of Head-Mounted Displays. Int. J. Environ. Res. Public. Health 2023, 20, 3940. [Google Scholar] [CrossRef] [PubMed]
- Fregna, G.; Schincaglia, N.; Baroni, A.; Straudi, S.; Casile, A. A Novel Immersive Virtual Reality Environment for the Motor Rehabilitation of Stroke Patients: A Feasibility Study. Front. Robot. AI 2022, 9, 906424. [Google Scholar] [CrossRef]
- Casile, A.; Fregna, G.; Boarini, V.; Paoluzzi, C.; Manfredini, F.; Lamberti, N.; Baroni, A.; Straudi, S. Quantitative Comparison of Hand Kinematics Measured with a Markerless Commercial Head-Mounted Display and a Marker-Based Motion Capture System in Stroke Survivors. Sensors 2023, 23, 7906. [Google Scholar] [CrossRef] [PubMed]
- Demeco, A.; Zola, L.; Frizziero, A.; Martini, C.; Palumbo, A.; Foresti, R.; Buccino, G.; Costantino, C. Immersive Virtual Reality in Post-Stroke Rehabilitation: A Systematic Review. Sensors 2023, 23, 1712. [Google Scholar] [CrossRef] [PubMed]
- Patsaki, I.; Dimitriadi, N.; Despoti, A.; Tzoumi, D.; Leventakis, N.; Roussou, G.; Papathanasiou, A.; Nanas, S.; Karatzanos, E. The Effectiveness of Immersive Virtual Reality in Physical Recovery of Stroke Patients: A Systematic Review. Front. Syst. Neurosci. 2022, 16, 880447. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; He, Z.; Yu, X.; Remis, A. Comparison of Immersive and Non-Immersive Virtual Reality for Upper Extremity Functional Recovery in Patients with Stroke: A Systematic Review and Network Meta-Analysis. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2023, 44, 2679–2697. [Google Scholar] [CrossRef] [PubMed]
- Marek, K.; Zubrycki, I.; Miller, E. Immersion Therapy with Head-Mounted Display for Rehabilitation of the Upper Limb after Stroke-Review. Sensors 2022, 22, 9962. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- JBI Critical Appraisal Tools|JBI. Available online: https://jbi.global/critical-appraisal-tools (accessed on 2 August 2023).
- Crosbie, J.H.; Lennon, S.; McGoldrick, M.C.; McNeill, M.D.J.; McDonough, S.M. Virtual Reality in the Rehabilitation of the Arm after Hemiplegic Stroke: A Randomized Controlled Pilot Study. Clin. Rehabil. 2012, 26, 798–806. [Google Scholar] [CrossRef]
- Hsu, H.-Y.; Kuo, L.-C.; Lin, Y.-C.; Su, F.-C.; Yang, T.-H.; Lin, C.-W. Effects of a Virtual Reality-Based Mirror Therapy Program on Improving Sensorimotor Function of Hands in Chronic Stroke Patients: A Randomized Controlled Trial. Neurorehabil. Neural Repair 2022, 36, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-Y.; Chiang, W.-C.; Yeh, Y.-C.; Fan, S.-C.; Yang, W.-H.; Kuo, H.-C.; Li, P.-C. Effects of Virtual Reality-Based Motor Control Training on Inflammation, Oxidative Stress, Neuroplasticity and Upper Limb Motor Function in Patients with Chronic Stroke: A Randomized Controlled Trial. BMC Neurol. 2022, 22, 21. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.W.; Kuo, L.C.; Lin, Y.C.; Su, F.C.; Lin, Y.A.; Hsu, H.Y. Development and Testing of a Virtual Reality Mirror Therapy System for the Sensorimotor Performance of Upper Extremity: A Pilot Randomized Controlled Trial. IEEE Access 2021, 9, 14725–14734. [Google Scholar] [CrossRef]
- Mekbib, D.B.; Debeli, D.K.; Zhang, L.; Fang, S.; Shao, Y.; Yang, W.; Han, J.; Jiang, H.; Zhu, J.; Zhao, Z.; et al. A Novel Fully Immersive Virtual Reality Environment for Upper Extremity Rehabilitation in Patients with Stroke. Ann. N. Y. Acad. Sci. 2021, 1493, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Ögün, M.N.; Kurul, R.; Yaşar, M.F.; Turkoglu, S.A.; Avci, Ş.; Yildiz, N. Effect of Leap Motion-Based 3D Immersive Virtual Reality Usage on Upper Extremity Function in Ischemic Stroke Patients. Arq. Neuropsiquiatr. 2019, 77, 681–688. [Google Scholar] [CrossRef]
- Song, Y.-H.; Lee, H.-M. Effect of Immersive Virtual Reality-Based Bilateral Arm Training in Patients with Chronic Stroke. Brain Sci. 2021, 11, 1032. [Google Scholar] [CrossRef]
- Ma, M.; Bechkoum, K. Serious Games for Movement Therapy after Stroke. In Proceedings of the 2008 IEEE International Conference on Systems, Man and Cybernetics, Singapore, 12–15 October 2008; pp. 1872–1877. [Google Scholar]
- Chen, C.-H.; Kreidler, T.; Ochsenfahrt, A. Rehago—A Home-Based Training App Using Virtual Reality to Improve Functional Performance of Stroke Patients with Mirror Therapy and Gamification Concept: A Pilot Study. Stud. Health Technol. Inform. 2022, 292, 91–95. [Google Scholar] [CrossRef]
- Connelly, L.; Stoykov, M.E.; Jia, Y.; Toro, M.L.; Kenyon, R.V.; Kamper, D.G. Use of a Pneumatic Glove for Hand Rehabilitation Following Stroke. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 2434–2437. [Google Scholar] [CrossRef]
- Erhardsson, M.; Alt Murphy, M.; Sunnerhagen, K.S. Commercial Head-Mounted Display Virtual Reality for Upper Extremity Rehabilitation in Chronic Stroke: A Single-Case Design Study. J. Neuroeng. Rehabil. 2020, 17, 154. [Google Scholar] [CrossRef]
- Lee, S.H.; Jung, H.-Y.; Yun, S.J.; Oh, B.-M.; Seo, H.G. Upper Extremity Rehabilitation Using Fully Immersive Virtual Reality Games With a Head Mount Display: A Feasibility Study. PM R 2020, 12, 257–262. [Google Scholar] [CrossRef]
- Mekbib, D.B.; Zhao, Z.; Wang, J.; Xu, B.; Zhang, L.; Cheng, R.; Fang, S.; Shao, Y.; Yang, W.; Han, J.; et al. Proactive Motor Functional Recovery Following Immersive Virtual Reality-Based Limb Mirroring Therapy in Patients with Subacute Stroke. Neurother. J. Am. Soc. Exp. Neurother. 2020, 17, 1919–1930. [Google Scholar] [CrossRef]
- Sramka, M.; Lacko, J.; Ruzicky, E.; Masan, J. Combined Methods of Rehabilitation of Patients after Stroke: Virtual Reality and Traditional Approach. Neuro Endocrinol. Lett. 2020, 41, 123–133. [Google Scholar] [PubMed]
- Vourvopoulos, A.; Pardo, O.M.; Lefebvre, S.; Neureither, M.; Saldana, D.; Jahng, E.; Liew, S.-L. Effects of a Brain-Computer Interface With Virtual Reality (VR) Neurofeedback: A Pilot Study in Chronic Stroke Patients. Front. Hum. Neurosci. 2019, 13, 210. [Google Scholar] [CrossRef]
- Weber, L.M.; Nilsen, D.M.; Gillen, G.; Yoon, J.; Stein, J. Immersive Virtual Reality Mirror Therapy for Upper Limb Recovery After Stroke: A Pilot Study. Am. J. Phys. Med. Rehabil. 2019, 98, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Vourvopoulos, A.; Jorge, C.; Abreu, R.; Figueiredo, P.; Fernandes, J.-C.; Bermúdez i Badia, S. Efficacy and Brain Imaging Correlates of an Immersive Motor Imagery BCI-Driven VR System for Upper Limb Motor Rehabilitation: A Clinical Case Report. Front. Hum. Neurosci. 2019, 13, 244. [Google Scholar] [CrossRef]
- Vourvopoulos, A.; Marin-Pardo, O.; Neureither, M.; Saldana, D.; Jahng, E.; Liew, S.-L. Multimodal Head-Mounted Virtual-Reality Brain-Computer Interface for Stroke Rehabilitation. In Virtual, Augmented and Mixed Reality. Multimodal Interaction, Proceedings of the 11th International Conference, VAMR 2019, Held as Part of the 21st HCI International Conference, HCII 2019, Orlando, FL, USA, 26–31 July 2019; Chen, J.Y.C., Fragomeni, G., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 165–179. [Google Scholar]
- Huang, L.-L.; Chen, M.-H. Effectiveness of the Immersive Virtual Reality in Upper Extremity Rehabilitation. In Cross-Cultural Design. Applications in Health, Learning, Communication, and Creativity, Proceedings of the 12th International Conference, CCD 2020, Held as Part of the 22nd HCI International Conference, HCII 2020, Copenhagen, Denmark, 19–24 July 2020; Proceedings, Part II. Springer: Berlin/Heidelberg, Germany, 2020; pp. 89–98. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Pau, M.; Cocco, E.; Arippa, F.; Casu, G.; Porta, M.; Menascu, S.; Achiron, A.; Kalron, A. An Immersive Virtual Kitchen Training System for People with Multiple Sclerosis: A Development and Validation Study. J. Clin. Med. 2023, 12, 3222. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.J.; Hyun, S.E.; Oh, B.-M.; Seo, H.G. Fully Immersive Virtual Reality Exergames with Dual-Task Components for Patients with Parkinson’s Disease: A Feasibility Study. J. Neuroeng. Rehabil. 2023, 20, 92. [Google Scholar] [CrossRef]
- Kim, A.; Schweighofer, N.; Finley, J.M. Locomotor Skill Acquisition in Virtual Reality Shows Sustained Transfer to the Real World. J. Neuroeng. Rehabil. 2019, 16, 113. [Google Scholar] [CrossRef]
- Levac, D.E.; Huber, M.E.; Sternad, D. Learning and Transfer of Complex Motor Skills in Virtual Reality: A Perspective Review. J. Neuroeng. Rehabil. 2019, 16, 121. [Google Scholar] [CrossRef]
- Chen, J.; Or, C.K.; Chen, T. Effectiveness of Using Virtual Reality-Supported Exercise Therapy for Upper Extremity Motor Rehabilitation in Patients With Stroke: Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Med. Internet Res. 2022, 24, e24111. [Google Scholar] [CrossRef]
- Geed, S.; Feit, P.; Edwards, D.F.; Dromerick, A.W. Why Are Stroke Rehabilitation Trial Recruitment Rates in Single Digits? Front. Neurol. 2021, 12, 674237. [Google Scholar] [CrossRef]
- Saes, M.; Mohamed Refai, M.I.; van Beijnum, B.J.F.; Bussmann, J.B.J.; Jansma, E.P.; Veltink, P.H.; Buurke, J.H.; van Wegen, E.E.H.; Meskers, C.G.M.; Krakauer, J.W.; et al. Quantifying Quality of Reaching Movements Longitudinally Post-Stroke: A Systematic Review. Neurorehabil. Neural Repair 2022, 36, 183–207. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, J.W.; Mazzoni, P.; Ghazizadeh, A.; Ravindran, R.; Shadmehr, R. Generalization of Motor Learning Depends on the History of Prior Action. PLoS Biol. 2006, 4, e316. [Google Scholar] [CrossRef] [PubMed]
- Kiper, P.; Przysiężna, E.; Cieślik, B.; Broniec-Siekaniec, K.; Kucińska, A.; Szczygieł, J.; Turek, K.; Gajda, R.; Szczepańska-Gieracha, J. Effects of Immersive Virtual Therapy as a Method Supporting Recovery of Depressive Symptoms in Post-Stroke Rehabilitation: Randomized Controlled Trial. Clin. Interv. Aging 2022, 17, 1673–1685. [Google Scholar] [CrossRef]
- Tosto-Mancuso, J.; Tabacof, L.; Herrera, J.E.; Breyman, E.; Dewil, S.; Cortes, M.; Correa-esnard, L.; Kellner, C.P.; Dangayach, N.; Putrino, D. Gamified Neurorehabilitation Strategies for Post-Stroke Motor Recovery: Challenges and Advantages. Curr. Neurol. Neurosci. Rep. 2022, 22, 183–195. [Google Scholar] [CrossRef] [PubMed]
| Study | Sample | Population | VR Dosage | Hardware& Software | Comparison | Outcome | Outcome Measures | Participants Analyzed |
|---|---|---|---|---|---|---|---|---|
| RCTS | ||||||||
| Crosbie, 2012 [41] | 18 (M = 10, F = 8) VRG: 9 CG: 9 | Chronic stroke patients VRG age 56.1 ± 14, MI-UE score 81.7 ± 9.4, ARAT score 51.3 ± 8.2 CG age 64.6 ± 7.4, MI-UE score 77.4 ± 19.5, ARAT score 47.3 ± 18.1 | Three sessions/week for 3 weeks of 30–45 min each | HMD (model not mentioned), desktop computer, motion tracking system, sensors _________ - | CT | Motor function | MI-UE, ARAT | 100% |
| Hsu, 2022 [42] | 54 (M = 20, F = 32) VRG: 18 UMT: 18 COT: 18 | Chronic stroke patients VRG age 52.9 ± 11.8, FMA-UE score 42.3 ± 14.3 UMT age 56.7 ± 11.5, FMA-UE score 32.1 ± 15.2; COT age 56.9 ± 13.0, FMA-UE score 34.5 ± 17.4 | Two sessions/week for 9 weeks comprised of 30 min of VR mirror therapy + 20 min of CT | HMD Oculus Rift, personal computer-based desktop, Leap Motion Controller, two camera sensors _________ Unity software | UMT or COT | Motor function | FMA-UE, MAL, BBT, SWM, MAS | 96% |
| Huang, 2020 [59] | 18 (M = 15, F = 3). VRG: 9 CT: 9 | Subacute/chronic stroke patients VRG age 59.5 ± 15.0, FMA-UE score 38.2 ± 19.6 CT age 55.3 ± 10.5, FMA-UE score 52.4 ± 10.1 | Total of 20 sessions over 8 weeks of 30 min of VR + 60 min of CT + 60 min of OT each. | HMD HTC Vive, hand controllers, pc station _________ - | CT | Motor function, ADL | FMA-UE, BBT, FIM | 100% |
| Huang, 2022 [43] | 30 (M = 10, F = 20) VRG: 15 CG: 15 | Chronic stroke patients VRG age 50.8± 12.3, FMA-UE score 49.4 ± 9.0; CG age 58.3 ± 11.2, FMA-UE score 44.5 ± 16.6 | Total of 16 sessions of 60 min each, 2–3 days/week | HMD HTC Vive, hand controllers, two infrared laser emittent units _________ Steam or VIVE platform | COT | Motor function, biomarkers analysis, usability | FMA-UE, AROM, BDNF proteins, SSQ, Borg Scale of Perceived Exertion and self-reported measures on satisfaction and safety | 100% |
| Lin, 2021 [44] | 18 (M = 13; F = 5) VRG: 9 CG: 9 | Chronic stroke patients VRG age 49.7 ± 13.4, FMA-UE score 43.4 ± 14.5 CG age 58.8 ± 9.6, FMA-UE score 28.3 ± 18.1 | Two sessions/week for 9 weeks of 30 min of VR mirror therapy + 20 min of CT each | HMD Oculus Rift, Leap Motion controller _________ Unity software | UMT + CT | Motor function | FMA-UE | 100% |
| Mekbib, 2021 [45] | 23 (M = 17, F = 6) VRG: 12 CG: 11 | Subacute stroke patients (<3 months) VRG age 52.2 ± 13.3, FMA-UE score 9.3 ± 3.8 CG age 61.0 ± 7.7, FMA-UE score 6.6 ± 2.2 | Four sessions/week for 2 weeks of 60 min of VR training + 60 of OT each | HMD HTC Vive, Leap Motion controller, PC; HTC Vive tracking technology, HTC Vive link box _________ Unity software | OT | Motor function, ADL, Cerebral Activity | FMA-UE, BI, fMRI | 100% |
| Ögün, 2019 [46] | 65 (M = 51, F = 14) VRG: 33 CG: 32 | Chronic stroke patients VRG age 61.5 ± 10.9, FMA-UE score 39.6 ± 8.8 CG age 59.8 ± 8.1, FMA-UE score 38.6 ± 8.8 | Three sessions/week for 6 weeks of 60 min each | HMD Oculus Rift, Leap Motion controller, TV screen _________ - | CT + VR equipment without motor interaction | Motor function, ADL | FMA-UE, ARAT, FIM, PASS-IADL, PASS-BADL | 100% |
| Song, 2021 [47] | 10 (M = 6, F = 4) VRG: 5 CG: 5 | Chronic stroke patients VRG age 64.2 ± 7.1 CG age 60.0 ± 10.9 | Five sessions/week for 4 weeks of 30 min each of VR bilateral arm training + 60 min of CT at every session | HMD Oculus Rift, hand controllers, Notebook _________ Tion, Human IT Solution | Usual bilateral arm training + CT | Motor function, Proprioception, Muscle Activity, Cerebral Activity | MFT, two-point discrimination test, Proprioception test, Stereognosis test, EMG, EEG | 100% |
| NRCTs | ||||||||
| Ma, 2008 [48] | 8 (M = 4, F = 4) VRG: 2 CG: 2 | Chronic stroke patients VRG age 59.5 ± 19.6, ARAT score 47.0 ± 11.2, MI score 84.0 ± 14.3 CG age 58.0 ± 16.4, ARAT score 55.5 ± 1.7, MI score 78.8 ± 3.5 | Total of 10 sessions | HMD VR1280, desktop computer _________ - | CT | Motor function | MI-UE, ARAT | 100% |
| NCCTs | ||||||||
| Chen, 2022 [49] | 48 (M = 34, F = 14) | Subacute/chronic stroke patients | Total of 42 sessions, 30 min each | HMD Pico Neo 2, hand controllers _________ Rehago software | - | ADL, QoL | FIM, EQ5D-5L | 100% |
| Case Series | ||||||||
| Connelly, 2009 [50] | 7 Sex data not reported | Chronic stroke patients age 57 ± 18, stage 4 or 5 of the Hand Stage of Recovery of the Chedoke–McMaster Stroke Assessment, FMA-UE score 37 ± 8.8 | Three sessions/week for 6 weeks of 30 min each | HMD Wide5, magnetic tracker, Pneuglove _________ Coin3D, CAVELib, Trackd-tool softwares | - | Motor function | FMA-UE | 100% |
| Erhardsson, 2020 [51] | 7 (M = 5, F = 2) | Chronic stroke patients age 60.6 ± 9.9 | Total of 4–27 sessions in 10 weeks | HMD HTC Vive _________ Steam software | - | Motor function | ARAT, BBT and ABILHAND questionnaire, FMA-UE, MAS, SGPALS, Kinematics data | 100%. Kinematics data from four patients |
| Lee, 2020 [52] | 12 (M = 7, F = 5) | Chronic Stroke patients age 40.2 ± 17.8, ARAT score 23.9 ± 18.6 | Total of 10 sessions, 2–3 sessions/week of 30 min each | HMD HTC Vive + hand controller _________ - | - | Motor function, usability | ARAT, BBT, MBI, self-reported usability questionnaire | 100% (usability) 75% (Motor function) |
| Mekbib, 2020 [53] | 8 (M = 6, F = 2) | Subacute stroke patients (<3 months) age 57.1 ± 4.5, FMA-UE score 7.5 ± 3.7 | Total of 60 min of VR training + 60 min of CT per day (4 days/week) for 2 weeks | HMD HTC Vive, Leap Motion controller, PC; HTC Vive tracking technology, HTC Vive link box _________ | - | Motor function, Cerebral Activity | FMA-UE, MRI | 100% |
| Sramka, 2020 [54] | 6 (4 for UE training) Sex data not reported | Not reported | Total of 11–12 sessions | HMD HTC Vive and Oculus Rift, hand controllers, Leap Motion controller _________ - | - | Motor function | Quantitative parameters (i.e., movement accuracy, limb orientation, movement speed) | 100% |
| Vourvopoulos, 2019 [55] | 4 (M = 3, F = 1) | Chronic stroke patients age 60.0 ± 5.8, FMA-UE score 31.8 ± 13.1 | Eight sessions of 90 min each | HMD Oculus Rift _________ REINVENT system (VR-BCI intervention) | - | Motor function, quality of life, usability, Muscle Activity, Cerebral Activity | FMA-UE, MAS, SIS, SSQ, self-reported data on enjoyment and ease of use, EEG, EMG, MRI, TMS | 100% |
| Weber, 2019 [56] | 10 (M = 6, F = 4) | Chronic stroke patients age 54.1 ± 13.0, FMA-UE score 21.7 ± 8.2 | Twelve sessions of 30 min each | HMD Oculus Rift, hand controllers, laptop computer, two tabletop infrared LED sensors _________ WiseMind | - | Motor function, usability | SSQ, SUS, FMA-UE, ARAT | 100% |
| Case Reports | ||||||||
| Vourvopoulus, 2019 (2) [57] | 1 male | A 60-year-old chronic stroke patient FMA-UE score 31 | Ten sessions of 15 min each for 3 weeks | Oculus Rift + haptic feedback tools _________ NeuRow system (VR-BCI intervention) | - | Motor function, quality of life, motor-imagery capability, cognitive function, Cerebral Activity | FMA-UE, MAS, SIS, MoCA, VMIQ-2 questionnaire, EEG, fMRI | 100% |
| Vourvopoulos, 2019 (3) [58] | 1 male | A 69-year-old chronic stroke patient FMA-UE score 13 | Sixteen sessions of 90 min each | HMD Oculus Rift; _________ REINVENT system (VR-BCI intervention) | - | Motor function, quality of life, Embodiment, Presence, Usability, Cerebral Activity | FMA-UE, SIS, SSQ, Presence Questionnaire, Embodiment Questionnaire, EEG data | 100% |
| ICF Domain | Study | Intervention | Within Groups Results | Between Groups Results | Sample |
|---|---|---|---|---|---|
| BODY FUNCTIONS | |||||
| Motor Function (FMA-UE, MI-UE) | |||||
| RCTs | |||||
| Crosbie, 2012 [41] | HMD VS CT | MI-UE: VRG from 81.7 to 84.9. CG from 77.4 to 85 | No significant differences (p = 0.48) | 18 VRG: 9 CG: 9 | |
| Hsu, 2022 [42] | Oculus Rift + Leap Motion or UMT or COT | FMA-UE: VRG from 42.3 to 46.1 (p < 0.05) UMT from 32.1 to 34.4 (p < 0.05) COT from 34.5 to 35.1 (not significant) | Significant difference between VRG and COT (p = 0.03) in favor of VRG, not between VGR and UMT | 52 VRG: 18 UMT: 17 COT: 17 | |
| Huang, 2020 [59] | HTC Vive + hand controllers VS CT | FMA-UE: VRG from 38.22 to 46.78 (p = 0.01). CG from 52.44 to 55.56 (p = 0.02). | No significant differences (p = 0.08) | 18 VRG: 9 CG: 9 | |
| Huang, 2022 [43] | HTC Vive + hand controllers VS COT | FMA-UE: VRG from 49.40 to 52.47 (p < 0.05) COT from 44.47 to 45.53 (p < 0.05) | Significant difference in favor of VRG (p ≤ 0.05) | 30 VRG: 15 CG: 15 | |
| Lin, 2021 [44] | Oculus Rift + Leap Motion VRMT VS UMT | FMA-UE: VRG from 43.4 to 46.7 (p < 0.05) CG from 28.3 to 29.2 (not significant) | Significant difference in favor of VRG (p = 0.03) | 18 VRG: 9 CG: 9 | |
| Mekbib, 2021 [45] | HTC Vive + Leap Motion VS OT | FMA-UE: VRG from 9.25 to 12.25 (p < 0.01) CG from 6.60 to 7.70 (not significant) | Significant difference in favor of VRG (p = 0.01) | 23 VRG: 12 CG: 11 | |
| Ögün, 2019 [46] | Oculus Rift + Leap Motion VS CT + only VR scenery | FMA-UE: VRG from 39.63 to 46.54 (p < 0.01) CG from 38.56 to 40.06 (p < 0.01) | Significant difference in favor of VRG (p < 0.01) | 65 VRG: 33 CG: 32 | |
| NRCTs | |||||
| Ma, 2008 [48] | VR 1280 + functional training VS functional training only | MI-UE: VRG improvement in all patients (p = 0.04) CG improvement in 2/4 patients (p = 0.14) | 8 VRG: 4 CG: 4 | ||
| Case Series | |||||
| Connelly, 2009 [50] | Wide5 + Pneuglove | FMA-UE: From 37 to 43.1 (p < 0.01) | 7 | ||
| Erhardsson, 2020 [51] | HTC Vive | FMA-UE: Improvements in 5/7 patients, gains between 3–5 points | 7 | ||
| Mekbib, 2020 [53] | HTC Vive | FMA-UE: Improvements in 5/8 patients, gains between 1–11 points (p = 0.04) | 8 | ||
| Vourvopoulus, 2019 [55] | Oculus Rift 1 | FMA-UE: Improvements in 3/4 patients, gains between 1–6 points (not significant) | 4 | ||
| Weber, 2019 [56] | Oculus Rift + hand controllers | FMA-UE: Improvements in 5/10 patients, gains between 1–5 points (not significant) | 10 | ||
| Case Reports | |||||
| Vourvopoulos, 2019 (2) [57] | BCI through Oculus Rift + haptic feedback tools | FMA-UE: Gain of 9 points | 1 | ||
| Vourvopoulos, 2019 (3) [58] | Oculus Rift | FMA-UE: Gain of 1 point | 1 | ||
| Muscle tone (MAS) | |||||
| RCTs | |||||
| Hsu, 2022 [42] | Oculus Rift + Leap Motion VS UMT VS COT | MAS: No significant differences in all groups | Significant difference in wrist hypertonia between VRG and COT after treatment (p = 0.03) in favor of VRG | 52 VRG: 18 UMT: 17 COT: 17 | |
| Case Series | |||||
| Erhardsson, 2020 [51] | HTC Vive | MAS: No significant differences | 7 | ||
| Vourvopoulus, 2019 [55] | Oculus Rift 1 | MAS: No differences | 4 | ||
| Case Reports | |||||
| Vourvopoulus, 2019 (2) [57] | BCI through Oculus Rift + haptic feedback tools | MAS: From 1+ to 2 | 1 | ||
| ACTIVITIES | |||||
| Arm use (ARAT, BBT, MAL, MFT, ABILHAND) | |||||
| RCTs | |||||
| Crosbie, 2012 [41] | HMD VS CT | ARAT: VRG from 51.3 to 52.8. CG from 47.3 to 50.2. | No significant differences (p = 0.14) | 18 VRG: 9 CG: 9 | |
| Hsu, 2022 [42] | Oculus Rift + Leap Motion VS UMT VS COT | BBT: Significant difference only in VRG, from 19.7 to 22.6 (p < 0.05) | Significant difference between VRG and UMT (p = 0.02) in favor of VRG | 52 VRG: 18 UMT: 17 COT: 17 | |
| MAL-AOU: Significant difference only in UMT, from 0.84 to 0.89 (p < 0.05) | No significant differences | ||||
| MAL-QOM: Significant difference in UMT, from 0.91 to 0.95 (p < 0.05) and in VRG, from 1.19 to 1.31 (p < 0.05) | Significant difference between UMT and VRG (p = 0.05) in favor of VRG | ||||
| Huang, 2020 [59] | HTC Vive + hand controllers VS CT | BBT: VRG from 17.44 to 29.67 (p = 0.12) CG from 29.67 to 35.44 (p = 0.10) | No significant differences (p = 0.42) | 18 VRG; 9 CG: 9 | |
| Ögün, 2019 [46] | Oculus Rift + Leap Motion VS CT + only VR scenery | ARAT: VRG from 32.81 to 41.15 (p < 0.01) CG from 30.84 to 32.09 (p < 0.01) | Significant difference in favor of VRG (p < 0.01) | 65 VRG: 33 CG: 32 | |
| Song, 2021 [47] | Oculus Rift + hand controllers VS conventional rehabilitation | MFT: Improvements in both VRG (p = 0.04) and CG (p = 0.04) | No significant differences | 10 VRG: 5 CG: 5 | |
| NRCTs | |||||
| Ma, 2008 [48] | VR 1280 + functional training VS functional training only | ARAT: Improvement in 1/4 patient (3 points) in VRG and in 2/4 patients of the CG (1 and 2 points) | 8 VRG: 4 CG: 4 | ||
| Case Series | |||||
| Erhardsson, 2020 [51] | HTC Vive | ARAT: Improvements in 6/7 patients | 7 | ||
| BBT: Improvements in 2/7 patients | |||||
| ABILHAND: Improvements in 4/7 patients | |||||
| Lee, 2020 [52] | HTC Vive + hand controllers | ARAT: From 22.3 to 31.1 (p = 0.03) | 9 | ||
| BBT: From 11.2 to 19.6 (p = 0.01) | |||||
| Weber, 2019 [56] | Oculus Rift + hand controllers | ARAT: Improvements in 2/10 patients, gains of 3 and 6 points (not significant) | 10 | ||
| ADL (FIM, (M)BI, PASS-BADL, PASS-IADL) | |||||
| RCTs | |||||
| Huang, 2020 [59] | FIM: VRG from 112.67 to 108.56 (p = 0.25) CG from 99.33 to 104.11 (p = 0.12) | No significant differences (p = 0.06) | 18 VRG: 9 CG: 9 | ||
| Mekbib, 2021 [45] | HTC Vive + Leap Motion + OT VS OT only | BI: VRG from 28.18 to 32.27 (p = 0.01) CG from 24.00 to 28.00 (p = 0.01) | No significant differences (p = 0.19) | 23 VR: 12 CG: 11 | |
| Ögün, 2019 [46] | Oculus Rift + Leap Motion VS CT + only VR scenery | FIM: VRG from 84.81 to 89.60 (p < 0.01) CG from 84.25 to 84.96 (p < 0.01) | Significant difference in favor of VRG (p < 0.01) | 65 VRG: 33 CG: 32 | |
| PASS-BADL: VRG from 1.46 to 1.84 (p < 0.01) CG from 1.53 to 1.56 (p = 0.51) | Significant difference in favor of VRG (p < 0.01) | ||||
| PASS-IADL: VRG from 1.58 to 1.98 (p < 0.01) CG from 1.57 to 1.61 (p = 0.54) | Significant difference in favor of VRG (p < 0.01) | ||||
| NCCTs | |||||
| Chen, 2022 [49] | Pico Neo 2 + Rehago | FIM: From 101.48 to 107.02, (p < 0.01) | 48 | ||
| Case Series | |||||
| Lee, 2020 [52] | HTC Vive + hand controllers | MBI: From 90.4 to 93.0 (p = 0.04) | 9 | ||
| PARTICIPATION | |||||
| QoL and Free time (EQ5D-5L, SGPALS, SIS) | |||||
| NCCTs | |||||
| Chen, 2022 [49] | Pico Neo 2 | EQ5D-5L: From 12.52 to 11.62 (p < 0.03) | 48 | ||
| QoL perceived: From 69.65 to 76.38 (p < 0.01) | |||||
| Case Series | |||||
| Erhardsson, 2020 [51] | HTC Vive | SGPALS: No difference | 7 | ||
| Vourvopoulos, 2019 [55] | Oculus Rift | SIS: Improvements in 1/4 patients, gain of 10 points (not significant) | 4 | ||
| Case Reports | |||||
| Vourvopoulos, 2019 (3) [58] | Oculus Rift 1 | SIS: Improvements of 30 points | 1 | ||
| OTHERS: Feasibility (SSQ, SUS), Presence, Embodiment | |||||
| RCTs | |||||
| Huang, 2022 [43] | HTC Vive + hand controllers VS COT | SSQ: Mean score of 0.39. Total of 46.7% of patients experienced eye strain and 46.67% sweating, 26.6% of subjects experienced both symptoms | 30 VRG: 15 CG: 15 | ||
| Case Series | |||||
| Vourvopoulos, 2019 [55] | Oculus Rift | SSQ: Changes after treatment: nausea subscale MD 0.13 (SD 1.46), oculomotor subscale MD -0.25 (SD 1.67) (not significant) | 4 | ||
| Weber, 2019 [56] | Oculus Rift + hand controllers | SUS: Mean score of 76/100 (40–100) | 10 | ||
| SSQ: From 1 to 1.6 after the first and the last session | |||||
| Case Reports | |||||
| Vourvopoulos, 2019 (3) [58] | Oculus Rift 1 | SSQ: No increases in nausea or oculo-motor sickness. | 1 | ||
| Presence: Increasing trend across sessions | |||||
| Embodiment: Increasing trend across sessions mostly for body ownership feeling | |||||
| RCTs (Cochrane RoB) | |||||||||||
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | Overall Score | |||
| Crosbie, 2012 [41] | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | 6/7 | |||
| Hsu, 2022 [42] | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | 6/7 | |||
| Huang, 2020 [59] | ? | ? | × | ? | ✓ | ✓ | ✓ | 3/7 | |||
| Huang, 2022 [43] | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | 6/7 | |||
| Lin, 2021 [44] | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | 6/7 | |||
| Mekbib, 2021 [45] | ✓ | ✓ | × | ✓ | × | ✓ | ✓ | 5/7 | |||
| Ögün, 2019 [46] | ✓ | ? | ✓ | ✓ | × | ✓ | ✓ | 5/7 | |||
| Song, 2021 [47] | ? | ✓ | × | ? | ? | ✓ | ✓ | 3/7 | |||
| NRCTs (JBI checklist) | |||||||||||
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Overall Score |
| Ma, 2008 [48] | ✓ | ? | ? | ? | ? | ✓ | × | ✓ | × | ✓ | 4/10 |
| NCCT (JBI checklist) | |||||||||||
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Overall Score | |
| Chen, 2022 [49] | ✓ | NA | NA | × | ✓ | ✓ | NA | ✓ | ✓ | 5/9 | |
| Case Series (JBI checklist) | |||||||||||
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Overall Score |
| Connelly, 2009 [50] | ✓ | ✓ | ✓ | ? | ? | × | ✓ | × | × | × | 4/10 |
| Erhardsson, 2020 [51] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | 9/10 |
| Lee, 2020 [52] | × | ? | ? | ✓ | ? | ✓ | × | ✓ | ? | ✓ | 4/10 |
| Mekbib, 2020 [53] | × | ? | ? | ? | ? | ✓ | × | ✓ | × | × | 2/10 |
| Sramka, 2020 [54] | × | × | × | ? | ? | × | × | × | × | × | 0/10 |
| Vourvopoulos, 2019 [55] | ✓ | ? | ? | ? | ? | × | × | ✓ | × | × | 2/10 |
| Weber, 2019 [56] | ✓ | ✓ | ✓ | ? | × | ✓ | × | ✓ | ✓ | ✓ | 7/10 |
| Case Reports (JBI checklist) | |||||||||||
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Overall Score | ||
| Vourvopoulos, 2019 (2) [57] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | 6/7 | ||
| Vourvopoulos, 2019 (3) [58] | × | × | × | ✓ | ✓ | ✓ | ✓ | ✓ | 5/7 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fregna, G.; Paoluzzi, C.; Baroni, A.; Cano-de-la-Cuerda, R.; Casile, A.; Straudi, S. Head-Mounted Displays for Upper Limb Stroke Rehabilitation: A Scoping Review. J. Clin. Med. 2023, 12, 7444. https://doi.org/10.3390/jcm12237444
Fregna G, Paoluzzi C, Baroni A, Cano-de-la-Cuerda R, Casile A, Straudi S. Head-Mounted Displays for Upper Limb Stroke Rehabilitation: A Scoping Review. Journal of Clinical Medicine. 2023; 12(23):7444. https://doi.org/10.3390/jcm12237444
Chicago/Turabian StyleFregna, Giulia, Chiara Paoluzzi, Andrea Baroni, Roberto Cano-de-la-Cuerda, Antonino Casile, and Sofia Straudi. 2023. "Head-Mounted Displays for Upper Limb Stroke Rehabilitation: A Scoping Review" Journal of Clinical Medicine 12, no. 23: 7444. https://doi.org/10.3390/jcm12237444
APA StyleFregna, G., Paoluzzi, C., Baroni, A., Cano-de-la-Cuerda, R., Casile, A., & Straudi, S. (2023). Head-Mounted Displays for Upper Limb Stroke Rehabilitation: A Scoping Review. Journal of Clinical Medicine, 12(23), 7444. https://doi.org/10.3390/jcm12237444








