Indirect Insulin Resistance Indices and Their Cut-Off Values for the Prediction of Post-Transplantation Diabetes Mellitus in Kidney Transplant Recipients
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Data Collection
2.3. Outcome Definition
2.4. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. Cross-Sectional Associations
3.3. Prospective Analyses of Insulin Resistance Index and Incident PTDM in KTRs
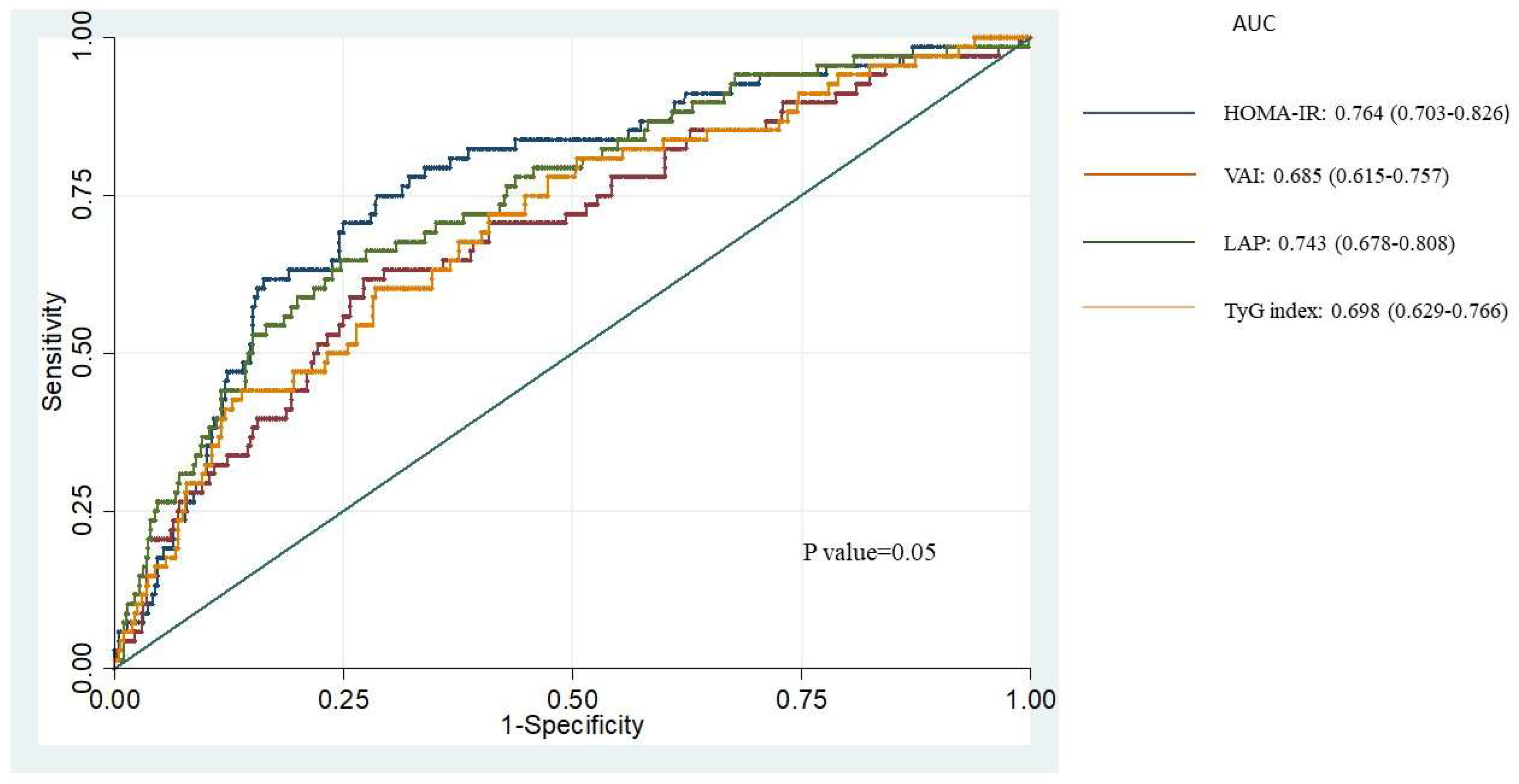
3.4. ROC Curves and Cut-Off Values of Indirect Insulin Resistance Indices for Incident PTDM
3.5. Cut-Off Values of Indirect Insulin Resistance Indices Combined with TyG Index for Incident PTDM
3.6. Validation of Cox-Regression Model and Cut-Off Value of HOMA-IR
4. Discussion
5. Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kuypers, D.R.J.; Claes, K.; Bammens, B.; Evenepoel, P.; Vanrenterghem, Y. Early Clinical Assessment of Glucose Metabolism in Renal Allograft Recipients: Diagnosis and Prediction of Post-Transplant Diabetes Mellitus (PTDM). Nephrol. Dial. Transplant. 2008, 23, 2033–2042. [Google Scholar] [CrossRef] [PubMed]
- Conte, C.; Secchi, A. Post-Transplantation Diabetes in Kidney Transplant Recipients: An Update on Management and Prevention. Acta Diabetol. 2018, 55, 763–779. [Google Scholar] [CrossRef] [PubMed]
- Montori, V.M.; Basu, A.; Erwin, P.J.; Velosa, J.A.; Gabriel, S.E.; Kudva, Y.C. Posttransplantation Diabetes A Systematic Review of the Literature. Diabetes Care 2002, 25, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Langsford, D. Dysglycemia after Renal Transplantation: Definition, Pathogenesis, Outcomes and Implications for Management. World J. Diabetes 2015, 6, 1132. [Google Scholar] [CrossRef] [PubMed]
- Bloom, R.D.; Crutchlow, M.F. New-Onset Diabetes Mellitus in the Kidney Recipient: Diagnosis and Management Strategies. Clin. J. Am. Soc. Nephrol. 2008, 3, S38. [Google Scholar] [CrossRef] [PubMed]
- Hjelmesaeth, J.; Midtvedt, K.; Jenssen, T.; Hartmann, A. Insulin Resistance After Renal Transplantation Impact of Immunosuppressive and Antihypertensive Therapy. Diabetes Care 2001, 24, 2121–2126. [Google Scholar] [CrossRef] [PubMed]
- Mayer-Davis, E.J.; D’agostino, R., Jr.; Karter, A.J.; Haffner, S.M.; Rewers, M.J.; Saad, M.; Bergman, R.N. Intensity and Amount of Physical Activity in Relation to Insulin Sensitivity The Insulin Resistance Atherosclerosis Study. JAMA 1998, 279, 669–674. [Google Scholar] [CrossRef]
- Luan, F.L.; Steffick, D.E.; Ojo, A.O. New-Onset Diabetes Mellitus in Kidney Transplant Recipients Discharged on Steroid-Free Immunosuppression. Transplantation 2011, 91, 334–341. [Google Scholar] [CrossRef]
- Defronzo, R.A.; Tobin, J.D.; Andres, R. Glucose Clamp Technique: A Method for Quantifying Insulin Secretion and Resistance. Am. J. Physiol. 1979, 273, 214–223. [Google Scholar] [CrossRef]
- Greenfield, M.S.; Doberne, L.; Kraemer, F.; Tobey, T.; Reaven, G. Assessment of Insulin Resistance with the Insulin Suppression Test and the Euglycemic Clamp. Diabetes 1981, 30, 387–392. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis Model Assessment: Insulin Resistance and Beta-Cell Function from Fasting Plasma Glucose and Insulin Concentrations in Man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Katz, A.; Nambi, S.S.; Mather, K.; Baron, A.D.; Follmann, D.A.; Sullivan, G.; Quon, M.J. Quantitative Insulin Sensitivity Check Index: A Simple, Accurate Method for Assessing Insulin Sensitivity In Humans. J. Clin. Endocrinol. Metab. 2000, 85, 2402–2410. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Romero, F.; Simental-Mendía, L.E.; González-Ortiz, M.; Martínez-Abundis, E.; Ramos-Zavala, M.G.; Hernández-González, S.O.; Jacques-Camarena, O.; Rodríguez-Morán, M. The Product of Triglycerides and Glucose, a Simple Measure of Insulin Sensitivity. Comparison with the Euglycemic-Hyperinsulinemic Clamp. J. Clin. Endocrinol. Metab. 2010, 95, 3347–3351. [Google Scholar] [CrossRef] [PubMed]
- Mazidi, M.; Kengne, A.P.; Katsiki, N.; Mikhailidis, D.P.; Banach, M. Lipid Accumulation Product and Triglycerides/Glucose Index Are Useful Predictors of Insulin Resistance. J. Diabetes Complicat. 2018, 32, 266–270. [Google Scholar] [CrossRef]
- Cai, R.; Wu, M.; Lin, M.; Guo, X.; Xing, Y. Pretransplant Homeostasis Model Assessment of Insulin Resistance and Fasting Plasma Glucose Predict New-Onset Diabetes After Renal Transplant in Chinese Patients. Transplant. Proc. 2019, 51, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, P.; Mukhopadhyay, P.; Roychowdhary, A.; Chowdhury, S.; Ghosh, S. Prevalence and Predictors of “New-Onset Diabetes after Transplantation” (NODAT) in Renal Transplant Recipients: An Observational Study. Ind. J. Endocrinol. Metab. 2019, 23, 273. [Google Scholar] [CrossRef]
- Dedinská, L.; Baltesová, T.; Beňa; Čellár, M.; Galajda, P.; Chrastina, M.; Jurčina, A.; Kováčiková, L.; Laca, L.; Lacková, E.; et al. Incidence of Diabetes Mellitus After Kidney Transplantation in Slovakia: Multicentric, Prospective Analysis. Transplant. Proc. 2016, 48, 3292–3298. [Google Scholar] [CrossRef]
- Tokodai, K.; Amada, N.; Haga, I.; Takayama, T.; Nakamura, A.; Kashiwadate, T. Insulin Resistance as a Risk Factor for New-Onset Diabetes after Kidney Transplantation. Transplant. Proc. 2014, 46, 537–539. [Google Scholar] [CrossRef]
- Xiaojie, N.; Bicheng, C.; Yongling, L.; Tingting, H.; Yi, Z.; Chen, Z. Metabolic-Related Index to Predict Post-Transplantation Diabetes Mellitus after Kidney Transplantation. Horm. Metab. Res. 2023, 55, 343–354. [Google Scholar] [CrossRef]
- De Vries, A.P.J.; Bakker, S.J.L.; Van Son, W.J.; Van Der Heide, J.J.H.; Ploeg, R.J.; The, H.T.; De Jong, P.E.; Gans, R.O.B. Metabolic Syndrome Is Associated with Impaired Long-Term Renal Allograft Function; Not All Component Criteria Contribute Equally. Am. J. Transplant. 2004, 4, 1675–1683. [Google Scholar] [CrossRef]
- Zelle, D.M.; Corpeleijn, E.; Deinum, J.; Stolk, R.P.; Gans, R.O.B.; Navis, G.; Bakker, S.J.L. Pancreatic β- Cell Dysfunction and Risk of New-Onset Diabetes after Kidney Transplantation. Diabetes Care 2013, 36, 1926–1932. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Iii, A.F.C.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T. A New Equation to Estimate Glomerular Filtration Rate Andrew. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Bala, C.; Gheorghe-Fronea, O.; Pop, D.; Pop, C.; Caloian, B.; Comsa, H.; Bozan, C.; Matei, C.; Dorobantu, M. The Association Between Six Surrogate Insulin Resistance Indexes and Hypertension: A Population-Based Study. Metab. Syndr. Relat. Disord. 2019, 17, 328–333. [Google Scholar] [CrossRef]
- Fan, J.; Gao, S.T.; Wang, L.J.; Qian, Z.L.; Zhou, Z.Q.; Liu, X.Z. Association of Three Simple Insulin Resistance Indexes with Prehypertension in Normoglycemic Subjects. Metab. Syndr. Relat. Disord. 2019, 17, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Sharif, A.; Hecking, M.; de Vries, A.P.J.; Porrini, E.; Hornum, M.; Rasoul-Rockenschaub, S. Proceedings from an International Consensus Meeting on Posttransplantation Diabetes Mellitus: Recommendations and Future Directions. Am. J. Transpl. 2014, 14, 1992–2000. [Google Scholar] [CrossRef] [PubMed]
- Eisenga, M.F.; Zelle, D.M.; Sloan, J.H.; Gaillard, C.A.J.M.; Bakker, S.J.L.; Dullaart, R.P.F. High Serum PCSK9 Is Associated with Increased Risk of New-Onset Diabetes after Transplantation in Renal Transplant Recipients. Diabetes Care 2017, 40, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Akobeng, A.K. Understanding Diagnostic Tests 3: Receiver Operating Characteristic Curves. Acta Paediatr. Int. J. Paediatr. 2007, 96, 644–647. [Google Scholar] [CrossRef]
- Kahn, S.E.; Cooper, M.E.; Del Prato, S. Pathophysiology and Treatment of Diabetes. Nutr. Diabetes 2014, 383, 1068–1083. [Google Scholar] [CrossRef]
- Laakso, M. How Good a Marker Is Insulin Level for Insulin Resistance? Am. J. Epidemiol. 1993, 137, 959–965. [Google Scholar] [CrossRef]
- Oterdoom, L.H.; De Vries, A.P.J.; Van Son, W.J.; Homan Van Der Heide, J.J.; Ploeg, R.J.; Gansevoort, R.T.; De Jong, P.E.; Gans, R.O.B.; Bakker, S.J.L. Validation of Insulin Resistance Indexes in a Stable Renal Transplant Population. Diabetes Care 2005, 28, 2424–2429. [Google Scholar] [CrossRef][Green Version]
- Szili-Torok, T.; Sokooti, S.; Osté, M.C.J.; Gomes-Neto, A.W.; Dullaart, R.P.F.; Bakker, S.J.L.; Tietge, U.J.F. Remnant Lipoprotein Cholesterol Is Associated with Incident New Onset Diabetes after Transplantation (NODAT) in Renal Transplant Recipients: Results of the Transplant Lines Biobank and Cohort Studies. Cardiovasc. Diabetol. 2022, 21, 41. [Google Scholar] [CrossRef] [PubMed]
- Sokooti, S.; Szili-Torok, T.; Flores-Guerrero, J.L.; Osté, M.C.J.; Gomes-Neto, A.W.; Kootstra-Ros, J.E.; Heerspink, H.J.L.; Connelly, M.A.; Bakker, S.J.L.; Dullaart, R.P.F. High-Density Lipoprotein Particles and Their Relationship to Posttransplantation Diabetes Mellitus in Renal Transplant Recipients. Biomolecules 2020, 10, 481. [Google Scholar] [CrossRef]
- Oterdoom, L.H.; De Vries, A.P.J.; Gansevoort, R.T.; Van Son, W.J.; Van Der Heide, J.J.H.; Ploeg, R.J.; De Jong, P.E.; Gans, R.O.B.; Bakker, S.J.L. Determinants of Insulin Resistance in Renal Transplant Recipients. Transplantation 2007, 83, 29–35. [Google Scholar] [CrossRef][Green Version]
- Martin, B.C.; Warram, J.H.; Krolewski, A.S.; Soeldner, J.S.; Kahn, C.R.; Martin, B.C.; Bergman, R.N. Role of Glucose and Insulin Resistance in Development of Type 2 Diabetes Mellitus: Results of a 25-Year Follow-up Study. Lancet 1992, 340, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.; Park, J.H.; Jang, E.J.; Park, Y.K.; Yu, J.M.; Park, J.S.; Ahn, Y.; Choi, S.H.; Yoo, H.J. The Cut-off Values of Surrogate Measures for Insulin Sensitivity in a Healthy Population in Korea According to the Korean National Health and Nutrition Examination Survey (KNHANES) 2007–2010. J. Korean Med. Sci. 2018, 33, e197. [Google Scholar] [CrossRef] [PubMed]
- Placzkowska, S.; Pawlik-Sobecka, L.; Kokot, I.; Piwowar, A. Indirect Insulin Resistance Detection: Current Clinical Trends and Laboratory Limitations. Biomed. Pap. 2019, 163, 187–199. [Google Scholar] [CrossRef]
- Muniyappa, R.; Lee, S.; Chen, H.; Quon, M.J. Current Approaches for Assessing Insulin Sensitivity and Resistance in Vivo: Advantages, Limitations, and Appropriate Usage. Am. J. Physiol. Endocrinol. Metab. 2008, 294, 15–26. [Google Scholar] [CrossRef]
- Harano, Y.; Hidaka, H.; Ohgaku, S.; Haneda, M.; Motoi, S.; Kawagoe, K.; Shigeta, Y.; Abe, H. Glucose, Insulin, and Somatostatin Infusion for the Determination of Insulin Sensitivity In Vivo. Metabolism 1978, 27, 1449–1452. [Google Scholar] [CrossRef]
- Kim, B.; Choi, H.Y.; Kim, W.; Ahn, C.; Lee, J.; Kim, J.G.; Kim, J.; Shin, H.; Yu, J.M.; Moon, S. The Cut-off Values of Surrogate Measures for Insulin Resistance in the Korean Population According to the Korean Genome and Epidemiology Study (KOGES). PLoS ONE 2018, 13, e0206994. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Villalobos-Molina, R.; Jiménez-Flores, J.R.; Simental-Mendia, L.E.; Méndez-Cruz, R.; Murguía-Romero, M.; Rodríguez-Morán, M. Fasting Triglycerides and Glucose Index as a Diagnostic Test for Insulin Resistance in Young Adults. Arch. Med. Res. 2016, 47, 382–387. [Google Scholar] [CrossRef]
- Rao, N.; Rathi, M.; Sharma, A.; Ramachandran, R.; Kumar, V.; Kohli, H.S.; Gupta, K.L.; Sakhuja, V. Pretransplant HbA1c and Glucose Metabolism Parameters in Predicting Posttransplant Diabetes Mellitus and Their Course in the First 6 Months after Living-Donor Renal Transplant. Exp. Clin. Transplant. 2018, 16, 446–454. [Google Scholar] [CrossRef]
- Demirci, M.S.; Toz, H.; Yilmaz, F.; Ertilav, M.; Asci, G.; Ozkahya, M.; Zeytinoglu, A.; Nart, D.; Ok, E. Risk Factors and Consequences of Post-Transplant Diabetes Mellitus. Clin. Transplant. 2010, 24, E170–E177. [Google Scholar] [CrossRef] [PubMed]
- Chakkera, H.A.; Weil, E.J.; Swanson, C.M.; Dueck, A.C.; Heilman, R.L.; Reddy, K.S.; Hamawi, K.; Khamash, H.; Moss, A.A.; Mulligan, D.C.; et al. Pretransplant Risk Score for New-Onset Diabetes after Kidney Transplantation. Diabetes Care 2011, 34, 2141–2145. [Google Scholar] [CrossRef] [PubMed]
- Raimi, T.H.; Dele-Ojo, B.F.; Dada, S.A.; Fadare, J.O.; Ajayi, D.D.; Ajayi, E.A.; Ajayi, O.A. Triglyceride-Glucose Index and Related Parameters Predicted Metabolic Syndrome in Nigerians. Metab. Syndr. Relat. Disord. 2021, 19, 76–82. [Google Scholar] [CrossRef]
- Mirr, M.; Skrypnik, D.; Bogdański, P.; Owecki, M. Newly Proposed Insulin Resistance Indexes Called TyG-NC.Pdf. J. Endocrinol. Investig. 2021, 44, 2831–2843. [Google Scholar] [CrossRef] [PubMed]
- Hedblad, B.; Nilsson, P.; Janzon, L.; Berglund, G. Relation between Insulin Resistance and Carotid Intima-Media Thickness and Stenosis in Non-Diabetic Subjects. Diabet. Med. 2000, 17, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Esteghamati, A.; Ashraf, H.; Esteghamati, A.R.; Meysamie, A.; Khalilzadeh, O.; Nakhjavani, M.; Abbasi, M. Optimal Threshold of Homeostasis Model Assessment for Insulin Resistance in an Iranian Population: The Implication of Metabolic Syndrome to Detect Insulin Resistance. Diabetes Res. Clin. Pract. 2009, 84, 279–287. [Google Scholar] [CrossRef]
- Marques-Vidal, P.; Mazoyer, E.; Bongard, V.; Gourdy, P.; Ruidavets, J.-B.; Drouet, L.; Ferrières, J. Prevalence of Insulin Resistance Syndrome in Southwestern France and Its Relationship with Inflammatory and Hemostatic Markers. Diabetes Care 2002, 25, 1371–1377. [Google Scholar] [CrossRef]
- Ghasemi, A.; Tohidi, M.; Derakhshan, A.; Hasheminia, M.; Azizi, F.; Hadaegh, F. Cut-off Points of Homeostasis Model Assessment of Insulin Resistance, Beta-Cell Function, and Fasting Serum Insulin to Identify Future Type 2 Diabetes: Tehran Lipid and Glucose Study. Acta Diabetol. 2015, 52, 905–915. [Google Scholar] [CrossRef]
- Lee, C.H.; Shih, A.Z.L.; Woo, Y.C.; Fong, C.H.Y.; Leung, O.Y.; Janus, E.; Cheung, B.M.Y.; Lam, K.S.L. Optimal Cut-Offs of Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) to Identify Dysglycemia and Type 2 Diabetes Mellitus: A15-Year Prospective Study in Chinese. PLoS ONE 2016, 11, e0163424. [Google Scholar] [CrossRef]
- Ekstrand, A.V.; Eriksson, J.G.; Grönhagen-Riska, C.; Ahonen, P.J.; Groop, L.C. Insulin Resistance and Insulin Deficiency in the Pathogenesis of Posttransplantation Diabetes in Man. Transplantation 1992, 53, 563–659. [Google Scholar] [CrossRef] [PubMed]
| Variables | |
| Participants, n | 472 |
| General characteristics | |
| Men, % | 56.4 |
| Age, year | 50.4 ± 12.1 |
| Current smoker, % | 40.9 |
| Alcohol use, never, % | 45.1 |
| Weight, kg | 76.3 ± 13.5 |
| Height, cm | 172.5 ± 9.7 |
| BMI, kg/m2 | 25.6 ± 4.1 |
| Transplant demographics | |
| Time since renal transplantation, year | 6.1 (2.6–11.7) |
| Donor age, year | 39.5 (23.0–51.0) |
| Living donor, % | 15.0 |
| Dialysis duration, months | 27 (13–49) |
| Rejection, % | 45.5 |
| Blood pressure | |
| Systolic blood pressure, mmHg | 151.4 ± 22.4 |
| Diastolic blood pressure, mmHg | 898.8 ± 9.9 |
| Metabolic variables | |
| Total cholesterol, mmol/L | 5.6 (5.0–6.2) |
| LDL cholesterol, mmol/L | 3.6 (3.0–4.1) |
| HDL cholesterol, mmol/L | 1.1 (0.9–1.3) |
| Triglycerides, mmol/L | 1.9 (1.4–2.6) |
| Glucose Homeostasis | |
| Glucose, mmol/L | 4.5 ± 0.5 |
| HbA1c, % | 6.3 ± 0.8 |
| Insulin, μU/mL | 10.3 (7.7–14.1) |
| hs-CRP, mg/L | 1.9 (0.7–4.6) |
| Renal function | |
| Serum Creatinin mmol/L | 137.0 (113.0–171.0) |
| eGFR, mL/min per 1.73 m2 | 46.7 (35.7–57.6) |
| UAE, g/24 h | 0.2 (0.0–0.50) |
| CMV infection, % | 29.2 |
| Medication use | |
| Statin use, % | 47.9 |
| Anti-hypertensive medication, % | 85.4 |
| Prednisolone, mg/day | 9.2 ± 1.3 |
| Calcineurin inhibitor, % | 77.3 |
| Cyclosporine, % | 63.8 |
| Tacrolimus, % | 13.6 |
| Proliferation inhibitor, % | 55.8 |
| Azathioprine,% | 33.9 |
| Mycophenolic acid, % | 41.9 |
| HOMA-IR, n = 68 | HR (95% CI) Per 1 SD | p Value |
|---|---|---|
| Crude | 2.61 (1.99–3.42) | <0.001 |
| Model 1+ | 2.79 (2.07–3.76) | <0.001 |
| +BMI | 2.26 (1.62–3.14) | <0.001 |
| +HbA1C | 2.37 (1.75–3.22) | <0.001 |
| +TG, HDL-C | 2.35 (1.71–3.22) | <0.001 |
| +VAI | 2.30 (1.68–3.16) | <0.001 |
| VAI, n = 68 | HR (95% CI) Per 1 SD | p Value |
| Crude | 1.97 (1.53–2.53) | <0.001 |
| Model 1+ | 2.09 (1.62–2.70) | <0.001 |
| +Glucose | 1.92 (1.49–2.47) | <0.001 |
| +HbA1c | 2.12 (1.61–2.79) | <0.001 |
| +HOMA-IR | 1.57 (1.20–2.04) | 0.001 |
| LAP, n = 68 | HR (95% CI) Per 1 SD | p Value |
| Crude | 2.39 (1.84–3.10) | <0.001 |
| Model 1+ | 2.62 (1.98–3.46) | <0.001 |
| +glucose | 2.40 (1.82–3.16) | <0.001 |
| +HbA1c | 2.67 (1.99–3.57) | <0.001 |
| +HDL-C | 2.62 (1.95–3.51) | <0.001 |
| +HOMA-IR | 1.94 (1.44–2.63) | <0.001 |
| TyG index, n = 68 | HR (95% CI) Per 1 SD | p Value |
| Crude | 2.38 (1.83–3.10) | <0.001 |
| Model 1 | 2.58 (1.96–3.39) | <0.001 |
| +BMI | 2.10 (1.57–2.83) | <0.001 |
| +HbA1C | 2.48 (1.85–3.31) | <0.001 |
| +HDL-C | 2.52 (1.89–3.36) | <0.001 |
| Insulin Resistance Index | Cut-Off Value | Sensitivity | Specificity | HR (95% CI) |
|---|---|---|---|---|
| HOMA-IR | 2.47 | 75.0 | 71.3 | 6.42 (3.67–11.25) |
| VAI | 4.01 | 61.8 | 72.8 | 4.10 (2.48–6.77) |
| LAP | 87.04 | 64.7 | 75.2 | 5.82 (3.46–9.80) |
| TyG index | 4.94 | 51.5 | 83.9 | 5.73 (3.45–9.52) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sokooti, S.; Szili-Török, T.; Heerspink, H.J.L.; Dullaart, R.P.F.; Bakker, S.J.L. Indirect Insulin Resistance Indices and Their Cut-Off Values for the Prediction of Post-Transplantation Diabetes Mellitus in Kidney Transplant Recipients. J. Clin. Med. 2023, 12, 7296. https://doi.org/10.3390/jcm12237296
Sokooti S, Szili-Török T, Heerspink HJL, Dullaart RPF, Bakker SJL. Indirect Insulin Resistance Indices and Their Cut-Off Values for the Prediction of Post-Transplantation Diabetes Mellitus in Kidney Transplant Recipients. Journal of Clinical Medicine. 2023; 12(23):7296. https://doi.org/10.3390/jcm12237296
Chicago/Turabian StyleSokooti, Sara, Tamás Szili-Török, Hiddo J. L. Heerspink, Robin P. F. Dullaart, and Stephan J. L. Bakker. 2023. "Indirect Insulin Resistance Indices and Their Cut-Off Values for the Prediction of Post-Transplantation Diabetes Mellitus in Kidney Transplant Recipients" Journal of Clinical Medicine 12, no. 23: 7296. https://doi.org/10.3390/jcm12237296
APA StyleSokooti, S., Szili-Török, T., Heerspink, H. J. L., Dullaart, R. P. F., & Bakker, S. J. L. (2023). Indirect Insulin Resistance Indices and Their Cut-Off Values for the Prediction of Post-Transplantation Diabetes Mellitus in Kidney Transplant Recipients. Journal of Clinical Medicine, 12(23), 7296. https://doi.org/10.3390/jcm12237296