Ten-Year Single-Center Study Examining Patient Survival after Commencing Long-Term Peritoneal Dialysis
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Naorungroj, T.; Neto, A.S.; Wang, A.; Gallagher, M.; Bellomo, R. Renal outcomes according to renal replacement therapy modality and treatment protocol in the ATN and RENAL trials. Crit. Care 2022, 26, 269. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.; Bello, A.K.; Levin, A.; Lunney, M.; Osman, M.A.; Ye, F.; Ashuntantang, G.E.; Bellorin-Font, E.; Gharbi, M.B.; Davison, S.N.; et al. Peritoneal Dialysis Use and Practice Patterns: An International Survey Study. Am. J. Kidney Dis. 2021, 77, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Sukul, N.; Zhao, J.; Fuller, D.S.; Karaboyas, A.; Bieber, B.; Sloand, J.A.; Subramanian, L.; Johnson, D.W.; Oliver, M.J.; Tungsanga, K.; et al. Patient-reported advantages and disadvantages of peritoneal dialysis: Results from the PDOPPS. BMC Nephrol. 2019, 20, 116. [Google Scholar] [CrossRef] [PubMed]
- Tekkarismaz, N.; Torun, D. Long-term clinical outcomes of peritoneal dialysis patients: 9-year experience of a single centre in Turkey. Turk. J. Med. Sci. 2020, 50, 386–397. [Google Scholar] [CrossRef] [PubMed]
- De Sousa-Amorim, E.; Bajo-Rubio, M.A.; del Peso-Gilsanz, G.; Castro, M.J.; Celadilla, O.; Selgas-Gutierrez, R. Thirty years in a peritoneal dialysis unit: Long-term survival. Nefrologia 2013, 33, 546–551. [Google Scholar] [CrossRef]
- Xia, X.; Qiu, Y.; Yu, J.; Lin, T.; Lu, M.; Yi, C.; Lin, J.; Ye, H.; Chen, W.; Mao, H.; et al. Ten-year survival of patients treated with peritoneal dialysis: A prospective observational cohort study. Perit. Dial. Int. 2020, 40, 573–580. [Google Scholar] [CrossRef]
- Abe, M.; Hamano, T.; Hoshino, J.; Wada, A.; Nakai, S.; Hanafusa, N.; Masakane, I.; Nitta, K.; Nakamoto, H. Predictors of outcomes in patients on peritoneal dialysis: A 2-year nationwide cohort study. Sci. Rep. 2019, 9, 3967. [Google Scholar] [CrossRef]
- Kang, M.; Kim, Y.L.; Kang, E.; Ryu, H.; Kim, Y.C.; Kim, D.K.; Lee, H.; Han, S.S.; Joo, K.W.; Kim, Y.S.; et al. Evolving outcomes of peritoneal dialysis: Secular trends at a single large center over three decades. Kidney Res. Clin. Pract. 2021, 40, 472–483. [Google Scholar] [CrossRef]
- Guzman-Ventura, W.; Caballero-Alvarado, J. Survival of patients on chronic hemodialysis versus chronic peritoneal dialysis. Rev. Peru. Med. Exp. Salud Publica 2022, 39, 161–169. [Google Scholar] [CrossRef]
- Gunawan, A.; Sakti, P.T. Five-Year Survival Rate of Patients with End-Stage Renal Disease on Continuous Ambulatory Peritoneal Dialysis (CAPD) at Malang CAPD Center, Indonesia. Acta Med. Indones. 2023, 55, 4–9. [Google Scholar]
- Leanos-Miranda, A. Factors predicting survival in patients on peritoneal dialysis. Rev. Investig. Clin. 1997, 49, 355–360. [Google Scholar]
- Cueto-Manzano, A.M.; Quintana-Pina, E.; Correa-Rotter, R. Long-term CAPD survival and analysis of mortality risk factors: 12-year experience of a single Mexican center. Perit. Dial. Int. 2001, 21, 148–153. [Google Scholar] [CrossRef]
- Rojas-Campos, E.; Alcantar-Medina, M.; Cortes-Sanabria, L.; Martinez-Ramirez, H.R.; Camarena, J.L.; Chavez, S.; Flores, A.; Nieves, J.J.; Monteon, F.; Gomez-Navarro, B.; et al. Patient and technique survival in continuous ambulatory peritoneal dialysis in a single center of the west of Mexico. Rev. Investig. Clin. 2007, 59, 184–191. [Google Scholar]
- Garcia-Garcia, G.; Briseno-Renteria, G.; Luquin-Arellan, V.H.; Gao, Z.; Gill, J.; Tonelli, M. Survival among patients with kidney failure in Jalisco, Mexico. J. Am. Soc. Nephrol. 2007, 18, 1922–1927. [Google Scholar] [CrossRef] [PubMed]
- Agudelo-Botero, M.; Valdez-Ortiz, R.; Giraldo-Rodriguez, L.; Gonzalez-Robledo, M.C.; Mino-Leon, D.; Rosales-Herrera, M.F.; Cahuana-Hurtado, L.; Rojas-Russell, M.E.; Davila-Cervantes, C.A. Overview of the burden of chronic kidney disease in Mexico: Secondary data analysis based on the Global Burden of Disease Study 2017. BMJ Open 2020, 10, e035285. [Google Scholar] [CrossRef] [PubMed]
- Kosnik, M.B.; Reif, D.M.; Lobdell, D.T.; Astell-Burt, T.; Feng, X.; Hader, J.D.; Hoppin, J.A. Associations between access to healthcare, environmental quality, and end-stage renal disease survival time: Proportional-hazards models of over 1,000,000 people over 14 years. PLoS ONE 2019, 14, e0214094. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, A.R.; Madonia, C.; Rascon-Pacheco, R.A. Improved patient/technique survival and peritonitis rates in patients treated with automated peritoneal dialysis when compared to continuous ambulatory peritoneal dialysis in a Mexican PD center. Kidney Int. 2008, 73, S76–S80. [Google Scholar] [CrossRef] [PubMed]
- Kwak, D.; Thompson, L.V. Frailty: Past, present, and future? Sport. Med. Health Sci. 2021, 3, 1–10. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, T.J.; Joosten, H.; van Buren, M.; Vinen, K.; Brown, E.A. A review of supportive care for older people with advanced chronic kidney disease. Clin. Kidney J. 2023, 16, 635–646. [Google Scholar] [CrossRef]
- Luo, P.T.; Li, W.; Li, X.Y.; Zhang, Y.; Du, B.; Cui, W.P. Impact of peritoneal dialysis modality on patient and PD survival: A systematic review. Perit. Dial. Int. 2023, 43, 128–138. [Google Scholar] [CrossRef]
- Rabindranath, K.S.; Nessim, S.J.; Bargman, J.M. Small Solute Clearance in Peritoneal Dialysis. Evid.-Based Nephrol. 2022, 2, 91–112. [Google Scholar]
- Arzhan, S.; Lew, S.Q.; Ing, T.S.; Tzamaloukas, A.H.; Unruh, M.L. Dysnatremias in Chronic Kidney Disease: Pathophysiology, Manifestations, and Treatment. Front. Med. 2021, 8, 769287. [Google Scholar] [CrossRef]
- Hassanein, M.; Arrigain, S.; Schold, J.D.; Nakhoul, G.N.; Navaneethan, S.D.; Mehdi, A.; Sekar, A.; Tabbara, J.; Taliercio, J.J.; Investigators, C. Dysnatremias, Mortality, and Kidney Failure in CKD: Findings From the Chronic Renal Insufficiency Cohort (CRIC) Study. Kidney Med. 2022, 4, 100554. [Google Scholar] [CrossRef]
- Domenici, A.; Giuliani, A. Automated Peritoneal Dialysis: Patient Perspectives and Outcomes. Int. J. Nephrol. Renov. Dis. 2021, 14, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Bitar, W.; Helve, J.; Kanerva, M.; Honkanen, E.; Rauta, V.; Haapio, M.; Finne, P. Severe infections in peritoneal dialysis and home hemodialysis patients: An inception cohort study. PLoS ONE 2023, 18, e0286579. [Google Scholar] [CrossRef]
- Shi, X.; Du, H.; Zhang, Z.; Zhou, Y. Clinical outcomes of automated versus continuous ambulatory peritoneal dialysis for end-stage kidney disease: Protocol of a systematic review and meta-analysis. BMJ Open 2022, 12, e065795. [Google Scholar] [CrossRef]
- Vesga, J.I.; Rodriguez, N.; Sanabria, R.M. Peritoneal dialysis modality failure in a middle-income country: A retrospective cohort study. Kidney Med. 2021, 3, 335–342.e331. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yang, L.; Zhu, X.; Zhang, X.; Meng, L.; Li, X.; Zhao, J.; Zhuang, X.; Cui, W. Clinical features and risk factors of catheter removal among 1062 episodes of peritoneal dialysis-associated peritonitis: A multicenter 7-year study. Ther. Apher. Dial. 2023, 27, 540–551. [Google Scholar] [CrossRef] [PubMed]
- Guo, Q.; Chen, Y.; Wu, R.; Yang, L.; Zhu, X.; Zhao, Q.; Zhuang, X.; Wu, Y.; Luo, P.; Cui, W. Poorer clinical outcomes of early-onset peritonitis in elderly peritoneal dialysis patients: A longitudinal and multicenter study. Ther. Apher. Dial. 2022, 26, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Pourhosein, E.; Bagherpour, F.; Latifi, M.; Pourhosein, M.; Pourmand, G.; Namdari, F.; Pourmand, N.; Ghaffari, P.; Dehghani, S. The influence of socioeconomic factors on deceased organ donation in Iran. Korean J. Transplant. 2022, 36, 54–60. [Google Scholar] [CrossRef]
- Soylu, D.; Soylu, A.; Yuzbasioglu, M.F. Determination of the factors affecting organ donation: Voluntary organ donors. Transpl. Immunol. 2022, 72, 101568. [Google Scholar] [CrossRef]
- Damar, H.T.; Ordin, Y.S.; Top, F.U. Factors Affecting Attitudes Toward Organ Donation in Health Care Professionals. Transplant. Proc. 2019, 51, 2167–2170. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Garcia, G.; Tonelli, M.; Ibarra-Hernandez, M.; Chavez-Iniguez, J.S.; Oseguera-Vizcaino, M.C. Access to kidney transplantation in Mexico, 2007–2019: A call to end disparities in transplant care. BMC Nephrol. 2021, 22, 99. [Google Scholar] [CrossRef] [PubMed]
- National Autonomous University of Mexico, Global Magazine. More than 22 Thousand People in Mexico Are Waiting to Receive an Organ or Tissue. Available online: https://unamglobal.unam.mx/global_revista/mas-de-22-mil-personas-esperan-recibir-un-organo-o-tejido-en-mexico/ (accessed on 4 October 2023).
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef] [PubMed]
| Failure Event (Fatal Outcome) | p | Person-Time | ||
|---|---|---|---|---|
| No (n = 297) | Yes (n = 73) | |||
| Gender | ||||
| Female | 107 (36.0) | 28 (38.4) | 0.711 | 5269 |
| Male | 190 (64.0) | 45 (61.6) | 10,377 | |
| Age (years) | 59.5 (18.3–89.4) | 62.1 (28.7–78.6) | 0.207 | 15,646 |
| Subjacent cause of ESKD | ||||
| T2DM | 219 (73.7) | 55 (75.4) | 0.812 | 10,741 |
| Hypertension | 45 (15.2) | 9 (12.3) | 2436 | |
| Other | 33 (11.1) | 9 (12.3) | 2469 | |
| Treatment modality | ||||
| APD | 104 (35.0) | 19 (26.0) | 0.144 | 6225 |
| CAPD | 193 (65.0) | 54 (74.0) | 9422 | |
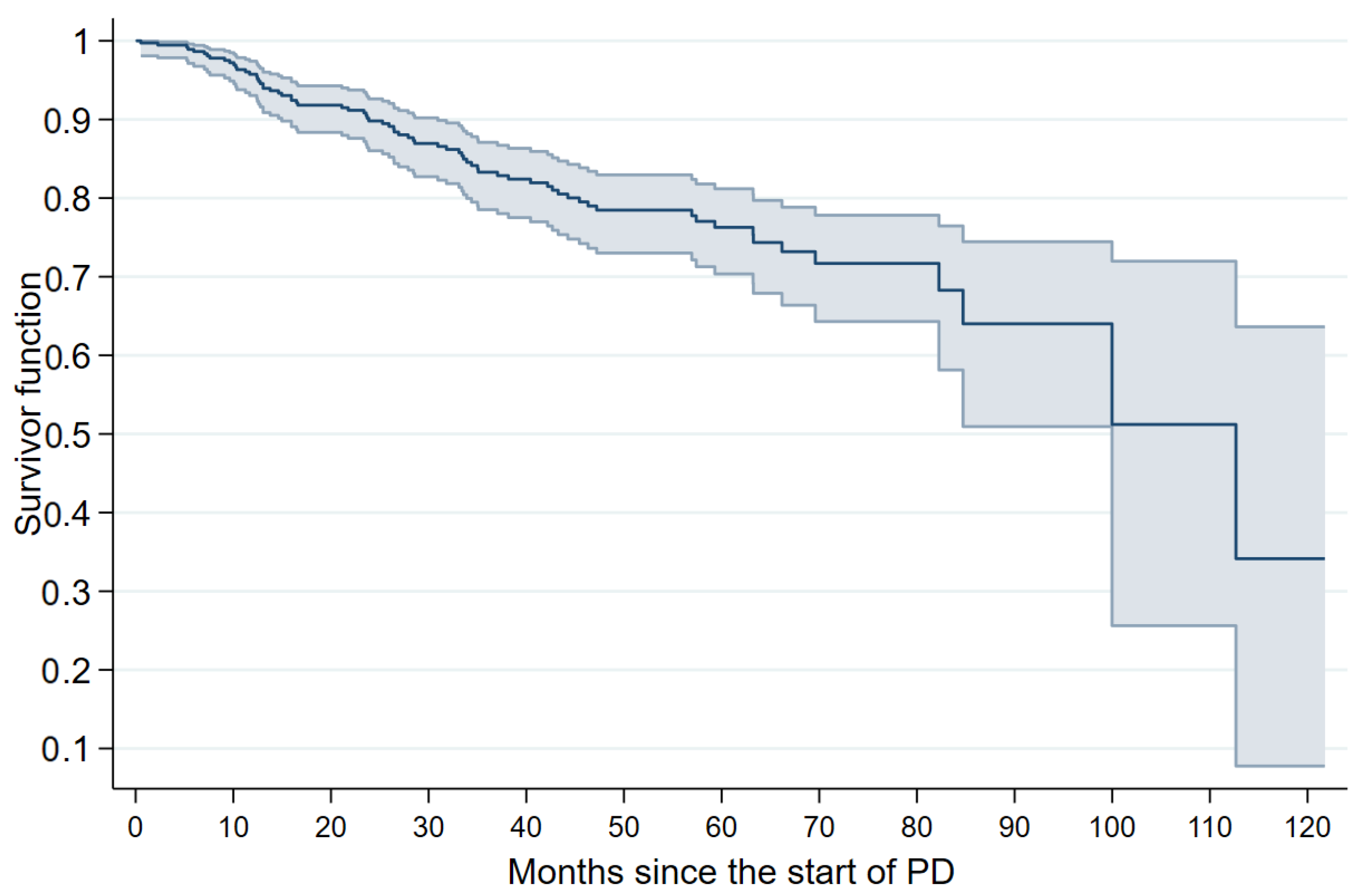
| t (Months) | Patients at Risk (n) | Failures (n) | Survivor Function (95% CI) |
|---|---|---|---|
| 1 | 372 | 1 | 99.7 (98.1–99.9) |
| 3 | 371 | 4 | 99.5 (97.9–99.8) |
| 6 | 365 | 10 | 98.4 (96.5–99.3) |
| 12 | 325 | 13 | 95.5 (92.8–97.2) |
| 18 | 300 | 6 | 91.6 (88.2–94.1) |
| 24 | 267 | 17 | 89.7 (85.8–92.5) |
| 36 | 194 | 10 | 83.2 (78.5–87.0) |
| 48 | 144 | 3 | 78.4 (73.0–82.9) |
| 60 | 96 | 4 | 76.3 (70.4–81.2) |
| 72 | 39 | 1 | 71.9 (64.6–77.9) |
| 84 | 18 | 1 | 68.7 (59.1–76.5) |
| 96 | 9 | 2 | 64.9 (52.8–74.7) |
| 120 | 3 | 1 | 44.5 (19.9–66.6) |
| Characteristic | HR (95% CI), p | |
|---|---|---|
| Bivariate Analysis | Multiple Analysis | |
| Gender | ||
| Female | 1.00 | 1.00 |
| Male | 0.78 (0.48–1.25), 0.300 | 0.74 (0.45–1.20), 0.218 |
| Age (years) | 1.02 (1.01–1.03), 0.014 | 1.02 (1.01–1.03), 0.040 |
| Treatment modality | ||
| APD | 1.00 | 1.00 |
| CAPD | 2.03 (1.18–3.48), 0.010 | 1.89 (1.08–3.01), 0.026 |
| Year of treatment initiation | 1.08 (0.93–1.24), 0.309 | 1.03 (0.89–1.19), 0.708 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Venegas-Ramírez, J.; Barrios-Mora, K.E.; Ríos-Bracamontes, E.F.; Guzmán-Esquivel, J.; Cárdenas-Rojas, M.I.; Murillo-Zamora, E. Ten-Year Single-Center Study Examining Patient Survival after Commencing Long-Term Peritoneal Dialysis. J. Clin. Med. 2023, 12, 7283. https://doi.org/10.3390/jcm12237283
Venegas-Ramírez J, Barrios-Mora KE, Ríos-Bracamontes EF, Guzmán-Esquivel J, Cárdenas-Rojas MI, Murillo-Zamora E. Ten-Year Single-Center Study Examining Patient Survival after Commencing Long-Term Peritoneal Dialysis. Journal of Clinical Medicine. 2023; 12(23):7283. https://doi.org/10.3390/jcm12237283
Chicago/Turabian StyleVenegas-Ramírez, Jesús, Karla Esmeralda Barrios-Mora, Eder Fernando Ríos-Bracamontes, José Guzmán-Esquivel, Martha Irazema Cárdenas-Rojas, and Efrén Murillo-Zamora. 2023. "Ten-Year Single-Center Study Examining Patient Survival after Commencing Long-Term Peritoneal Dialysis" Journal of Clinical Medicine 12, no. 23: 7283. https://doi.org/10.3390/jcm12237283
APA StyleVenegas-Ramírez, J., Barrios-Mora, K. E., Ríos-Bracamontes, E. F., Guzmán-Esquivel, J., Cárdenas-Rojas, M. I., & Murillo-Zamora, E. (2023). Ten-Year Single-Center Study Examining Patient Survival after Commencing Long-Term Peritoneal Dialysis. Journal of Clinical Medicine, 12(23), 7283. https://doi.org/10.3390/jcm12237283






