1. Introduction
Falls are a common cause of morbidity and functional impairment in older people and represent a significant health problem that requires preventive action.
It is estimated that approximately one in three people aged 65 years and over and half of those aged 80 and over experience at least one fall per year [
1]. As the frequency of this event increases with increasing age, the magnitude of the problem will increase as the population ages [
2].
Injuries resulting from falls are often not serious, but 10% to 20% of fallers aged 65 years and older sustain bone fractures [
3]. Globally, among people aged ≥ 70 years, falls result in more than 6 million years lived with disability, and 1.6% (95% CI 1.32–1.79) of falls result in death [
4]. Falls in the elderly represent a major concern because of their impact on public health and can result in a significant economic burden because of the substantial associated medical expenditures [
5,
6].
Among older people, experiencing falls has been identified as a risk factor for nursing-home admission [
7], and repeated falls are a common reason for admission to the hospital [
8]. Loss of confidence following a fall can have psychological consequences for older people, who may be afraid of falling again. This change can lead to reduction in physical activity, depression and social isolation, accelerating functional decline [
9].
Recognized fall risk factors related to the health status of the elderly include poor health [
10], conditions due to cardiovascular diseases [
11,
12], depression [
13], dementia [
14], arthritis [
15], epilepsy [
16] and visual impairment [
17]. Polypharmacy and the use of certain medications, such as benzodiazepine, psychotropics and some classes of cardiovascular drugs, can also increase the risk of falling [
12,
18,
19,
20].
In addition to individual health-related risk factors, environmental hazards also play a role in many falls. These hazards include slippery floors or stairs; inadequate, irregular or excessive lighting; and lack of handholds [
21].
The ongoing Silver Steps (Passi d’Argento) survey, promoted by the Italian National Institute of Health (ISS), provides an overview of the situation in Italy [
22]. In 2012–2013, 11.2% (CI 95% 10.64–11.69%) of respondents aged 65 years and over (
n = 24.000) reported having fallen in the 30 days prior to the interview, with 14% (CI 95% 12.4–15.8%) of cases requiring at least one day of hospitalization [
23]. Most falls occurred in the home (60.5%, CI 95% 58.2–62.7%), with falls representing the leading cause of home accidents. Falls occurred less frequently in the street (19.5%, CI 95% 17.8–21.2%) or elsewhere. The survey also found that only one in six respondents said they had received advice from their doctor or other healthcare professional about how to prevent falls in the 12 months prior to the survey, suggesting a need for greater awareness and preventive interventions. Multivariate analysis identified several factors that showed statistically significant associations with increased risk of falling, including age, female gender, disability, polypharmacy, visual impairment, economic difficulties and living in a house with structural problems.
Falls are caused by multiple factors, so any prevention strategy should be based on interventions with multiple components [
24]. The recent global guidelines for fall prevention in older adults recommend multicomponent interventions, defined as “fixed combinations of two or more intervention components that are not individually tailored following a multifactorial falls risk assessment. Multicomponent interventions vary widely: for illustration, an example could be a medication review, home modifications and generic exercise advice” [
25]. Recommendations for healthy nutrition should be included, as both nutritional status and BMI are associated with the risk of falls and recurrent falls [
26].
General practitioners (GPs) are the first point of contact for health issues. They are in the best position to assess the presence of risk factors for falls, to provide fall-prevention interventions to community-dwelling older adults, and to evaluate the impact of prevention strategies. In Italy, GPs are present in the community, their clinics are easily accessible to patients, and they conduct clinical practice both in their clinic and in the patient’s home. The GP thus has easy access to the home environment to assess safety conditions and daily habits. In addition, GPs can provide continuity of care over time and have the capacity to follow up on long-term multicomponent interventions.
The PREMIO study (Primary Prevention Study of Domiciliary Falls in Elderly Patients at Risk, in Italian: Studio di PREvenzione PriMaria delle Cadute DomIciliari in Pazienti Anziani a rischiO) was launched in 2015 by one of the largest Italian federations of GPs (in Italian: Federazione Italiana Medici di Medicina Generale-FIMMG). The aim of the study was to implement a multicomponent preventive intervention program coordinated by the GPs and to evaluate its impact on the rate of reported falls and their serious complications such as fractures and fall-related healthcare utilization. The effect of this intervention was compared with the effect of simple dietary recommendations.
2. Materials and Methods
2.1. Participants
The first 20 consecutive patients who met the inclusion criteria and agreed to participate in the study were recruited by their respective GPs during clinic or home visits. Inclusion criteria required the presence of at least five of the following fall risk factors: history of previous falls, fear of falling, polypharmacy (≥5 medications), treatment with medications that increase the risk of falling (
Table S1), impaired mobility, altered vision, social isolation, major cerebro- or cardiovascular disease, difficulty extending the knees, mental confusion, creatinine clearance < 65 mL/min and arthritis and/or arthrosis. The five-factor threshold was arbitrarily defined as a reliable compromise for sample enrichment that was helpful in identifying a population who were at high risk for falls but also fit enough to actively participate in a low-intensity program of physical activity.
Other inclusion criteria were age ≥ 65 years, living at home regularly and signing the informed consent. Individuals with a life expectancy of <1 year; those with Parkinson’s disease, epilepsy or depression (under antidepressant treatment); bedridden patients and, in general, all subjects with serious psychophysical conditions that prevented their participation in the study were excluded from the selection procedures.
2.2. Study Design
The PREMIO study was a two-arm, pragmatic, randomized controlled trial. All GPs identified through their membership in the national medical organization FIMMG were invited to participate in the study through presentations, e-mails, letters and face-to-face interviews. A total of 117 GPs agreed to participate, and each doctor committed to enrolling 20 patients who were considered at risk of falling, according to the then-current Italian guidelines for the prevention of falls at home among the elderly [
27].
Patients were randomized using a sealed-envelope system. Participating GPs received randomly generated treatment allocations in sealed opaque envelopes. The envelope was opened once a patient who met the inclusion criteria agreed to participate in the program.
All patients randomized to the intervention group received a booklet with physical-activity recommendations (
Table S2).
They also received a Fall Diary (
Table S3) and a Physical Activity Diary (
Table S4), both to be completed daily and sent to the GP every three months. To complete the intervention, the patients received a set of dietary recommendations (
Table S5).
The patients in the control arm received the same set of dietary recommendations (as required by the ethics committee) and the Fall Diary.
For each enrolled patient, the GP completed a patient data sheet with demographic and medical data based on the patient’s clinical records. These data and the information from the fall and physical-activity diaries were centralized through a web platform for the creation and management of the PREMIO database at NETMEDICA (
www.netmedicaitalia.it, accessed on 20 October 2023).
Within 2 weeks of enrollment, the GP was to visit each patient’s home, identify home risks and provide recommendations to address them, and complete the environmental risk survey module (
Table S6). All GPs contacted the patients monthly to monitor compliance and reinforce motivation to participate in the study.
The intervention lasted 12 months. At the end of the study, all participating patients were asked to complete a customer-satisfaction questionnaire based on a 7-item Likert scale (
Table S7) to assess the acceptability of the program.
2.3. Intervention
The intervention plan was multicomponent and included the following:
medical review of treatments, with the aim of limiting medications that increase the risk of falling (
Table S1)
recommendation of 1–2 daily training sessions with gentle physical exercise (5 min of stationary exercise plus 5 min of slow walking and 5 min of fast walking, gradually increasing up to 30 min, followed by 5 min of slow walking. See
Table S2)
inspection of patients’ homes, followed by recommendations of home modifications to reduce structural hazards (e.g., installing a handrail on stairs or equipping the shower stall or bathtub with non-slip mats. See
Table S6).
Minor interventions added to the program at the discretion of the GP included, for example, management of orthostatic hypotension, podiatry, diet and practical recommendations (e.g., safe shoe models).
2.4. Outcomes
The primary outcome was the rate of falls over 12 months. To investigate different characteristics of fallers, fall rates were expressed as both the mean number of falls and the proportion of individuals reporting at least one fall.
Secondary outcomes included the direct consequences of falls, i.e., fractures, admissions to the hospital or emergency department and visits to their GP’s clinic.
2.5. Ethical Compliance
The study protocol was approved by the Ethics Committee of the coordinating center at the IRCCS San Raffaele Roma (PR n. 06/16; 10 March 2016) and by the ethics committees of the local health districts where the GPs were located (over 40 ethics committees were contacted).
All participating subjects signed an informed-consent form after receiving detailed information about the aims of the study and the protocol.
2.6. Statistical Methods
The study was designed to show a significant (5%) reduction in falls in the intervention group, that is, a change from an expected frequency of 27% per year to 22%, considering a type-I error of 0.05 and a statistical power of 80%. The estimated number of patients to recruit was 953 per group. The G*power statistical software was used for power analysis.
The primary statistical analysis was based on 1757 individuals who started the study. The protocol, which required participants to keep records of physical activity and falls over the whole duration of the study, was completed by 1225 individuals (69.7%).
A flow chart describing patient dropout and withdrawal is provided in
Supplementary Figure S1. The mean age, sex ratio, and the mean of fall risk factors were compared between the subjects who left the study and those who completed the program. No significant difference was found for any parameters evaluated.
The presence of differences in clinical and demographic characteristics between treatment arms was tested with Student’s t-test for continuous variables and with the χ2 test for categorical variables.
The effect of the intervention on the number of falls was evaluated with a log-normal multiple regression model and with logistic regression models for binary variables.
Risks for all endpoints were evaluated as mean ratio (MR) and odds ratio (OR), depending on the model fitted, and reported with their 95% confidence intervals (95% CI).
All statistical analyses were performed using SPSS version 23 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, version 23.0. Armonk, NY, USA: IBM Corp), and Stata version 15.1 (StataCorp. 2017. College Station, TX, USA: StataCorp LLC).
3. Results
The PREMIO study involved 117 GPs who enrolled 1757 patients at high risk of falling. Half of the patients were randomized to intervention and half to the control group, as shown in
Table 1.
Patients were predominantly female (63.5%), and the mean age of the entire study group was 77.5 years. Three out of four patients were overweight or obese (45.2% and 29.4%, respectively), while only 0.9% were underweight.
Current smokers constituted 17.1% of the total study group, although information on smoking habits was largely underreported in the medical records (47.7% missing). Smoking habits was the only variable with such a high proportion of missing values. There were no statistically significant differences between the two study groups in these selected characteristics, confirming the effectiveness of randomization. The difference in the number of patients randomized to the intervention and control groups resulted from an unequal distribution of patients recruited by each GP.
The distribution of fall risk factors among the patients is shown in
Table 2.
One of the inclusion criteria was having at least 5 risk factors from the predefined list. The mean number of risk factors was 6; the most common number was 5 (66%), followed by 6 (19%). The use of medications that increase the risk of falling was the most common risk factor (93.5%), followed by cerebro- or cardiovascular disease (87.6%), polypharmacy (85.5%) and the presence of arthritis or arthrosis (85.5%), this last being the only factor that showed a small but statistically significant difference between the intervention and control groups.
To test whether selection bias was introduced by differential attrition of subjects from the multicomponent intervention group versus the control group, the proportions of subjects who completed the protocol and recorded physical activity and falls for the full 12 months of the study were compared in the two groups and were found to substantially overlap (68.6% and 66%, respectively). The main reason for patient withdrawal was the progressive loss of interest in the study. Other common reasons included the GP’s decision to leave the study, health reasons including death and practical reasons such as change of residence or change of GP.
Table 3 shows the distribution of patients according to selected characteristics of the 117 GPs who participated in the study.
Three out of four patients had male GPs (76.4%). The mean age of the GPs was 59.4 years. Almost half were from southern Italy (52.5%), and the rest were from central-northern Italy. On average, each doctor enrolled 15 patients. No statistically significant difference was found between the two study groups for any of these characteristics.
In the intervention group, most patients had their GPs make the two planned home visits (81.4%), while the rest made only one; 80% had regular telephone contact with patients.
Table 4 shows the results of the univariate analysis of primary endpoints.
Subjects who received the multicomponent intervention had a lower mean number of falls (−26.0%, p < 0.02). The reduction was more dramatic in the subgroup of domestic falls, the target of the intervention (−31.2%, p < 0.02) but did not reach statistical significance in the subgroup of falls outside. In the subgroup of domestic falls, the number of fallers was also slightly lower in the intervention group than in the control group (p = 0.05).
Multivariate models were used to account for residual confounding and to test for the presence of interactions. The log-normal multivariate model fitted to the mean number of falls showed a significantly lower mean number of domestic falls in the multicomponent-intervention group compared with the controls (mean ratio 0.70, 95% CI: 0.54–0.90; p = 0.032) after adjustment for the potential confounders of age, sex, BMI and smoking habits.
Binary logistic regression analysis of the risk of falling at least once per year showed an odds ratio (OR) of 0.76 (95% CI: 0.57–1.02; p = 0.068), which was estimated from a model including age and sex.
No interaction was found between the effect of the multicomponent intervention and other covariates, although some covariates were closely associated with the risk of falling.
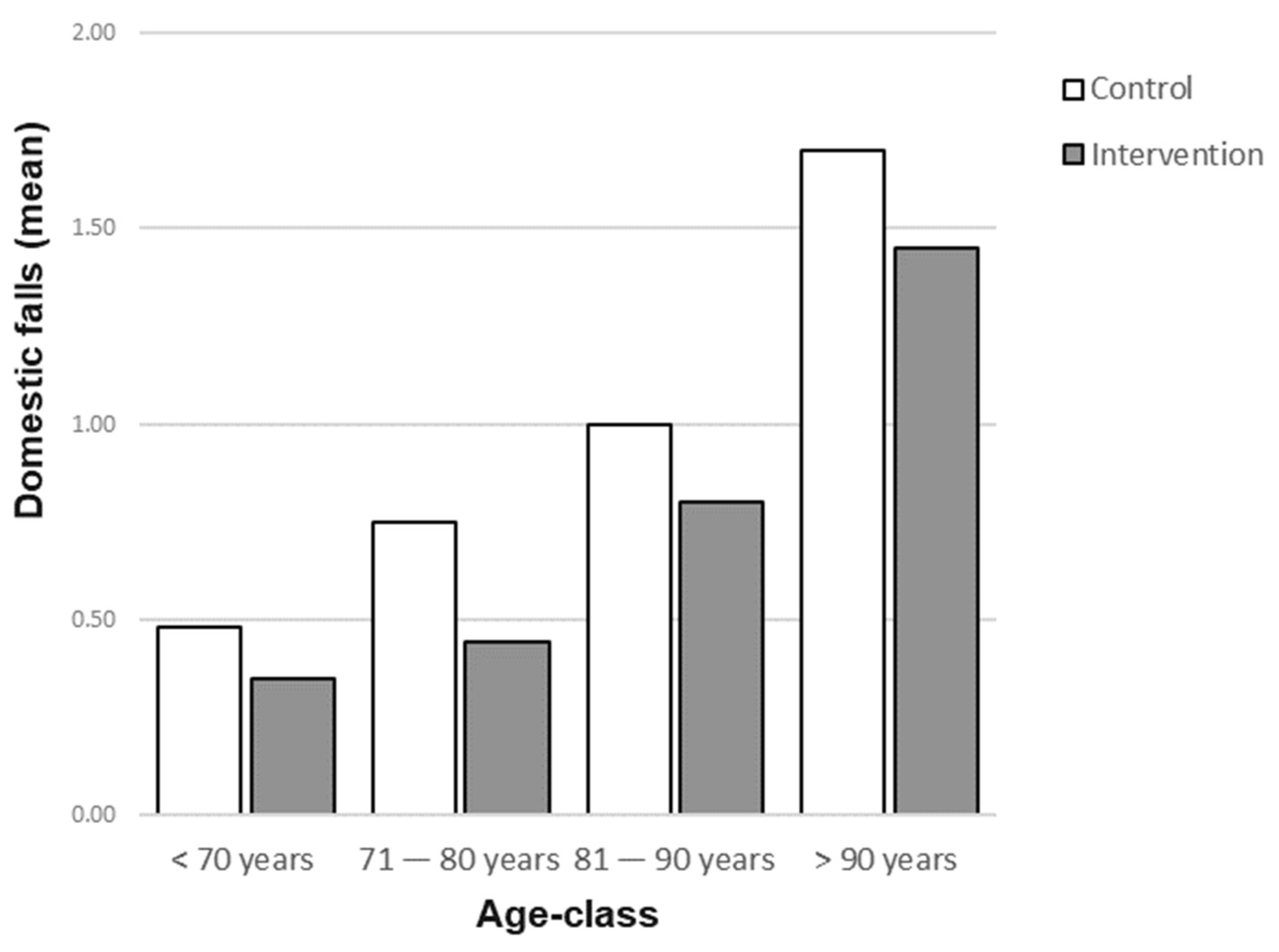
Figure 1 shows that the mean number of domestic falls increased with age in both the intervention and control groups but was consistently lower in the intervention group than in the control group across all age classes.
The study included several secondary endpoints, as summarized in
Table 5.
The overall frequency of fractures due to falls was 2.7%, and, unexpectedly, subjects in the intervention group showed a higher risk compared to controls (OR = 2.39, p = 0.023).
No statistically significant differences were observed for the other endpoints, although subjects in the intervention arm were less likely to be admitted to hospitals or to emergency departments and were less likely to visit the GPs’ clinics (16.5% of subjects overall, for a total of 764 visits).
Patients in the intervention arms were given a questionnaire to assess their level of satisfaction with the fall-prevention program. The mean score was 6.4 (SD 1.3), which corresponds to complete satisfaction on a 0–7 Likert scale.
4. Discussion
The PREMIO study involved engaging many GPs across the country to raise awareness of the problem of falls in older adults and propose an active role for the primary care physician. The multicomponent intervention proposed here was supported by extensive evidence, and our results confirm the validity and effectiveness of this approach.
Patients randomized to the multicomponent intervention experienced a statistically significant reduction in the mean number of falls recorded during 12 months of follow-up (−26.0% overall). The reduction was particularly dramatic for domestic falls, which were reduced by 31.2% (mean number of falls per year: 0.80 in the control group vs. 0.55 in the intervention group). The overall number of fallers was reduced by 3.9% (p = 0.05).
Limited improvement was also seen in other secondary outcomes of great importance for public health, such as admission to a general hospital (2.3% in the intervention group vs. 2.6% in the controls) or to the emergency department (5.7% and 7.3% respectively) because of a fall.
The result regarding fractures was unexpected, with a significantly higher risk in the intervention group than among the controls (OR = 2.39, p = 0.023).
Interventions for the prevention of falls in older people living in the community are the object of great scientific interest and intense clinical research, including a series of Cochrane reviews aimed at better understanding “what might work and for whom… (while) the evidence story continues to evolve, exploring ever more precise components of these interventions” [
28].
A Cochrane review analyzed the effect of multicomponent interventions on fall-related outcomes [
24]. Meta-analysis of the four trials with participants selected by high risk of falling at baseline showed a protective effect of these interventions, with the rate of falls decreased by 21% (95% CI 7% to 32%), a result comparable to that of the PREMIO study. The number of people who sustained at least one fall was reduced by 17% (95% CI 10% to 26%).
Another more recent Cochrane review evaluated interventions with an environmental approach to reducing the risk of falling [
29]. In their review, the category of interventions to reduce home fall hazards included studies with an assessment, advice and guidance approach similar to one of the components of the PREMIO multicomponent intervention: a healthcare professional visited participants in their own home one or two times, with telephone follow-up; fall hazards were assessed and a problem-solving strategy was proposed. This strategy raised awareness of falling risk, and assistive technologies were provided in some cases. The results of the meta-analysis (9 studies on older people selected for high risk at baseline) were similar to those of the PREMIO study, with the rate of falls reduced by 38% (95% CI 30% to 44%). The proportion of fallers who had at least one fall was reduced by 26% in the meta-analysis (95% CI 15% to 35%).
The third Cochrane review found that the difference related to the effect of exercise (all types) on the rate of falls in trials in which all participants were at an increased risk of falling was 20% (95% CI 12% to 28%). The difference in the number of people experiencing at least one fall (35 studies) was 13% (95% CI 9% to 17%) [
30].
Overall, these reviews showed comparable reductions in fall rates but a greater reduction in the number of fallers compared to the PREMIO study. This relatively small reduction in the number of fallers may be tentatively explained by the fact that a large proportion of patients in PREMIO were overweight or obese (three out of four subjects overweight; three out of ten obese). A systematic literature review of studies of community-dwelling older adults found a U-shaped association between BMI and fall risk, with an increased risk for those with extreme values of BMI relative to those with intermediate values [
26].
The multivariate statistical analysis showed that the benefit of the multicomponent intervention was not modified by external factors. For example, the reduction in the mean number of falls in the intervention group is consistent across all age-classes.
Few studies in the Cochrane reviews reported on falls requiring medical attention or hospitalization, yielding uncertain evidence that multicomponent interventions, exercise and home fall-hazard interventions made little or no difference, as in PREMIO [
24,
29,
30,
31].
Our unexpected finding of an increased risk of fracture in the multicomponent-intervention group compared with the controls is relevant from a clinical, quality-of-life and socioeconomic perspective. There is a paucity of data and low certainty in the literature on this topic.
Both the Cochrane reviews of home fall-hazard interventions and of the effect of exercise found that such interventions made little or no difference in the risk of people experiencing a fall-related fracture compared with usual care [
29,
30], while the review of multicomponent interventions included only two trials with one fracture event each, making it inconclusive [
24].
In addition, in a component-network meta-analysis of interventions to prevent falls and fall-related fractures in community-dwelling older adults, no single intervention was associated with a reduction in the number of fall-related fractures, while one of the intervention components, assistive technology, was significantly associated with an increase in the number of fall-related fractures (RR 1.66; 95% CI 1.07–2.59) [
32].
Finally, in a large trial conducted in the UK among community-dwelling older adults, the fracture-rate ratio was 1.20 (95% CI 0.91 to 1.59) for exercise and 1.30 (95% CI, 0.99 to 1.71) for multifactorial fall prevention compared with mailed advice [
33]. No explanation was provided by the authors of that study.
Bone health and fall prevention are often considered separately in public-health settings. The PREMIO study was designed to address the individual risk of falls, not the risk of fractures. A possible explanation for the unexpected increased risk of fractures in PREMIO could be a differential distribution of patients by fracture-related conditions between the intervention and control groups. A higher prevalence of subjects with arthritis/arthrosis was observed in the intervention group (87.2% vs. 83.8%,
p < 0.05), and this condition is often associated with osteoporosis and higher risk of fractures [
34]. Bone mineral density and osteoporosis were also not taken into account, as in other similar studies, although their association with fractures, falls and fear of falling is well known. Another possible explanation is that overtraining or increased confidence may lead to a higher risk of serious consequences of falls. A detailed analysis of all fracture events is planned to investigate this finding in more detail.
The PREMIO study was conducted at the practice level, involving GPs from all over the country, with the aim of incorporating a multifactorial fall-prevention intervention as a regular procedure for each GP. In Italy, general practice is managed by the National Health System, and the relationships between the GP and their patients are therefore quite stable over the patients’ lifetimes, creating an excellent opportunity for this kind of intervention. In PREMIO, the high rate of record completion (72%) demonstrated the possibility of involving primary care professionals in research, linking routine clinical practice to science. The heterogeneity resulting from such a broad and fragmented approach was addressed with methodological tools such as block randomization at the GP level. The high score on the Likert scale used to assess the acceptability of the intervention to patients showed that this type of approach is highly appreciated by older subjects living in the community.
The study has several strengths, starting with the randomized and controlled design, the nationwide distribution of investigators, and especially the practice-oriented intervention model, which was designed to be systematically offered to elderly patients in the practice who were at risk of falling.
Limitations include an overly high expectation of the frequency of falls, which, together with the number of patients who withdrew before the start of the study, reduced the statistical power and resulted in non-significant findings for some of the secondary endpoints. The use of non-probability samples may have increased the risk of sampling bias. Nevertheless, the relatively large number of patients, the wide geographical distribution and the randomized study design provided reliable and relatively robust quantitative estimates that can help guide future studies or public-health interventions in terms of the best strategies to prevent falls among the elderly, especially at home. Furthermore, the lack of a longer follow-up did not allow the authors to evaluate the duration of the benefits and adherence to the intervention program in the long term.
Additional risk factors for falls should be considered in future studies. Such risk factors include substance abuse and excessive alcohol consumption [
25]. Smartphone use is also becoming ubiquitous among the elderly. There is a gap in scientific knowledge regarding the risk of fall and neurological and orthopedic disorders associated with smartphone use, but some studies show that it can slow movement, induce systematic imbalance and alter turning behavior, thereby increasing the risk of falling [
35,
36].
5. Conclusions
The PREMIO study, which was based on the classic working model of general practice, demonstrated the ability of GPs to manage intervention studies with large numbers of patients.
The study showed a significant reduction in falls by one in four falls and up to 31% fewer falls at home, although the reduction in the number of fallers was limited. Among the secondary endpoints, admissions to a general hospital or to the emergency room and visits to the GP’s clinic showed marginal improvements. The increased risk of fractures in the intervention group was unexpected and warrants further analyses, given the paucity and uncertainty of published evidence on this topic.
In conclusion, this study confirms that a multicomponent intervention at the primary-care level has the potential to prevent a significant proportion of domestic falls among community-dwelling older people at high risk of falling. The involvement of the GPs is critical because of their role in monitoring adherence to the program. The secondary benefits of the intervention are more difficult to interpret because the study was not specifically designed to measure these outcomes. Non-significant benefits in terms of hospital and emergency-department admissions were offset by an increase in fractures in the intervention group, a finding that may be related to residual confounding after randomization.
Future studies and public-health interventions to prevent falls could benefit from a multicomponent approach including medication review, physical exercise and home risk assessment and should include assessment of risk factors for fractures.
Supplementary Materials
The following supporting information can be downloaded at:
https://www.mdpi.com/article/10.3390/jcm12227134/s1, Supplementary Table S1. Risk of falling associated to the use of selected drugs known to increase the risk of falling. Supplementary Table S2. Description of the physical activity prescribed as part of the intervention. Supplementary Table S3. Evaluation grid of falling risk environmental factors, to be filled by the General Practitioner. Supplementary Table S4. Monthly fall diary to be completed by participants and sent to the General Practitioner. Supplementary Table S5. Monthly diary of physical activity to be completed by participants and sent to the General Practitioner. Supplementary Table S6. Dietary Recommendations. Supplementary Table S7. Customer satisfaction questionnaire completed by all participants. Figure S1. Patients flow.
Author Contributions
Conceptualization, W.M.; Methodology, W.M., C.T. and S.B.; Formal analysis, S.B.; Investigation, G.M., A.P.D. and A.P.; Participant enrolment, Intervention administration, Data collection, F.I.M.M.G Research PREMIO Group; Data curation, N.C., P.M. and A.D.V.; Writing—original draft, W.M. and A.G.; Supervision, S.S. and M.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study has been approved by the ethics committee of the IRCCS San Raffaele Roma (Coordinating Center) on 4 March 2016 (Protocol Code PREMIO; RP02/16) and thereafter by all
ethics committees of the local health districts where the GPs were located.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Acknowledgments
The authors thank Monica Neri (Neri Monica EI, Annet sur Marne, France) for providing medical writing support. Contributing Authors: F.I.M.M.G Research PREMIO Group: F.I.M.M.G Research PREMIO Group: Abbonato Francesco (Roma), Amedeo Riccardo (Trapani), Auriemma Lucia (Napoli), Baranzini Franco (Varese), Barba Ettore (Brescia), Bedoni Alfredo (Bergamo), Belotti Cecilia (Bergamo), Benincasa Santi (Ragusa), Bettino Gino (Caserta), Bombardiere Giuseppe Nicodemo (Crotone), Bruschelli Carla (Roma), Burresi Andrea (Siena), Caccamo Orazio Antonio (Caltanissetta), Cagia Michele (Bari), Caldarola Giuseppe (Bari), Calderone Rosa Maria (Palermo), Calì Claudia (Palermo), Caliari Serena (Firenze), Calore Marco (Rovigo), Campisi Daniele (Roma), Carità Vincenzo (Agrigento), Carpentieri Ambrogio (Potenza), Carrano Francesco (Frosinone), Carraro Andrea (Genova), Castellano Giovanna (Palermo), Cella Luigi (Piacenza), Chiriatti Alberto (Roma), Ciaccia Angela (Bari), Colosimo Francesco (Crotone), Contaldi Pasquale (Salerno), Cupiraggi Enrico Ernesto (Catanzaro), Curreri Antonio (Agrigento), Cusumano Mariano (Trapani), D’Alessandro Rosario (Palermo), D’Anna Giuseppe (Caltanissetta), De Angeli Daniele (Milano), De Vita Maria Teresa (Foggia), Del Sole Anna Rita (Bari), Denora Antonio Maria (Bari), Di Bari Nicola (Barletta-Andria-Trani), Di Carlo Vittorio (Palermo), Di Lascio Giacomo (Potenza), Di Macco Erasmo (Latina), Di Maggio Edoardo (Enna), Di Modugno Nicola (Barletta-Andria-Trani), Drago Pietro (Barletta-Andria-Trani), Fanciullacci Antonio (Firenze), Fasulo Serenella (Palermo), Ferri Luana (Roma), Ferri Sergio (Terni), Fiorillo Alfonso (Roma), Francucci Massimo (Perugia), Galasso Vincenzo (Roma), Giobbe Maria Rosaria (Bari), Gioè Vincenza Maria (Trapani), Gurgone Francesco (Enna), Imburgia Giovanni (Palermo), Legrottaglie Francesco (Brindisi), Lembo Aurelio (Messina), Lentini Patrizia (Roma), Lerede Modesto (Bari), Levato Gabriella (Milano), Lippa Luciano (L’Aquila), Lisco Michele Giuseppe (Brindisi), Livadiotti Daniela (Roma), Lo Bue Giuseppe (Palermo), Lo Russo Nicola Antonio (Bari), Lombardo Trifone (Bari), Lorusso Pasquale (Bari), Luciani Vincenzo (Benevento), Madami Lallo (Bari), Madurno Donato (Bari), Mahajne Ibrahim (Firenze), Malatesta Marco (Genova), Mannina Santa Maria Antonina (Palermo), Maracchione Nicoletta (Bari), Martino Michele (Bari), Marulli Carlo Fedele (Teramo), Mastrosimone Giuseppe (Caltanissetta), Merlino Giovanni (Palermo), Mocerino Maria Felicia (Napoli), Monopoli Donato (Brindisi), Morciano Maria Rosaria (Brindisi), Natale Pasquale (Bologna), Panzera Tiziana (Sondrio), Pascucci Francesco (Roma), Perrone Antonio (Foggia), Pirro Maurizio (Roma), Porcelli Donato (Bari), Pozzi Anna Carla (Milano), Reina Giovanni Paolo (Palermo), Roccatagliata Ubaldo (Genova), Rosati Giovanni (Salerno), Rubino Tommaso (Pistoia), Rulli Nicola (Reggio Calabria), Salamone Francesco (Palermo), Salvati Alessandra (Roma), Santivetti Paolo (Roma), Santoro Giuseppe (Enna), Scalera Pietro (Bari), Schiavone Ciro (Foggia), Sciarra Federico (Roma), Segreto Baldassarre (Agrigento), Sessa Pasquale (Napoli), Siciliano Salvatore (Torino), Sirico Luigi (Salerno), Siviero Guido Alberto (Rovigo), Stirpe Maria Cristina (Roma), Stranges Saverio (Caserta), Taormina Francesca (Palermo), Tarì Michele (Bari), Tiberio Giovanni (Roma), Toscano Luciano (Matera), Travaglio Pasquale (Bari), Valletta Domenico Giuseppe (L’Aquila), Verginelli Antonio (Roma), Vissani Luca (Macerata), Zafonte Rita (Palermo), Zamparella Maria (Bari). All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- NHS Falls Overview. Available online: www.nhs.uk/conditions/falls/ (accessed on 12 October 2023).
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef]
- Moreland, B.; Kakara, R.; Henry, A. Trends in nonfatal falls and fall related injuries among adults aged ≥ 65 years—United States, 2012–2018. Morb. Mortal. Wkly. Rep. 2020, 69, 875–881. [Google Scholar] [CrossRef] [PubMed]
- 2019 Global Burden of Diseases. Available online: https://vizhub.healthdata.org/gbd-results/ (accessed on 12 October 2023).
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.R.; Stevens, J.A.; Drake, C. Medical costs of fatal and nonfatal falls in older adults. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Haagsma, J.A.; Olij, B.F.; Majdan, M.; van Beeck, E.F.; Vos, T.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Liu, Z.; et al. Falls in older aged adults in 22 European countries: Incidence, mortality and burden of disease from 1990 to 2017. Inj Prev. 2020, 26 (Supp. 1), i67–i74. [Google Scholar] [CrossRef]
- Berete, F.; Demarest, S.; Charafeddine, R.; De Ridder, K.; Vanoverloop, J.; Van Oyen, H.; Bruyère, O.; Van der Heyden, J. Predictors of nursing home admission in the older population in Belgium: A longitudinal follow-up of health interview survey participants. BMC Geriatr. 2022, 22, 807. [Google Scholar] [CrossRef] [PubMed]
- Prabhakaran, K.; Gogna, S.; Pee, S.; Samson, D.J.; Con, J.; Latifi, R. Falling again? Falls in geriatric adults—Risk factors and outcomes associated with recidivism. J. Surg. Res. 2020, 247, 66–76. [Google Scholar] [CrossRef]
- Pin, S.; Spini, D. Impact of falling on social participation and social support trajectories in a middle-aged and elderly European sample. SSM Popul. Health 2016, 2, 382–389. [Google Scholar] [CrossRef]
- Mackenzie, L.; Byles, J.; Mishra, G. An occupational focus of fall with serious injury among older women in Australia. Aust. Occup. Ther. J. 2004, 51, 144–154. [Google Scholar] [CrossRef]
- Jorgensen, L.; Engastand, T.; Jacobsen, B.K. High incidence of falls in long term stroke survivors than in population control: Depressive symptom predict falls after stroke. Stroke 2002, 33, 542–547. [Google Scholar] [CrossRef]
- de Vries, M.; Seppala, L.J.; Daams, J.G.; van de Glind, E.M.; Masud, T.; van der Velde, N.; Blain, H.; Bousquet, J.; Bucht, G.; Caballero-Mora, M.A.; et al. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-Analysis: I Cardiovascular drugs. J. Am. Med. Dir. Assoc. 2018, 19, e1–e371. [Google Scholar] [CrossRef]
- Gambaro, E.; Gramaglia, C.; Azzolina, D.; Campani, D.; Dal Molin, A.; Zeppegno, P. The complex associations between late life depression, fear of falling and risk of falls. A systematic review and meta-analysis. Aging Res. Rev. 2022, 73, 101532. [Google Scholar] [CrossRef]
- Lach, H.W.; Harrison, B.E.; Phongphanngam, S. Falls and fall prevention in older adults with early-stage dementia: An integrative Review. Res. Gerontol. Nurs. 2017, 10, 139–148. [Google Scholar] [CrossRef]
- Byun, M.; Kim, J.; Kim, M. Physical and Psychological Factors Affecting Falls in Older Patients with Arthritis. Int. J. Environ. Res. Public. Health 2020, 17, 1098. [Google Scholar] [CrossRef]
- Haasum, Y.; Johnell, K. Use of anti epileptic drugs and risk of falls in old age. A Syst. Rev. Epilepsy Res. 2017, 138, 98–104. [Google Scholar] [CrossRef]
- Terheyden, J.H.; Gerhards, J.; Ost, R.A.D.; Wintergerst, M.W.M.; Holz, F.G.; Finger, R.P. Patient-reported vision impairment in low luminance predicts multiple falls. BMC Geriatr. 2023, 23, 583. [Google Scholar] [CrossRef]
- van der Velde, N.; Seppala, L.J.; Hartikainen, S.; Kamkar, N.; Mallet, L.; Masud, T.; Montero-Odasso, M.; van Poelgeest, E.P.; Thomsen, K.; Ryg, J.; et al. European position paper on polypharmacy and fall-risk-increasing drugs recommendations in the World Guidelines for Falls Prevention and Management: Implications and implementation. Eur. Geriatr. Med. 2023, 14, 649–658. [Google Scholar] [CrossRef]
- Seppala, L.J.; van de Glind, E.M.M.; Daams, J.G.; Ploegmakers, K.J.; de Vries, M.; Wermelink, A.; van der Velde, N.; EUGMS Task and Finish Group on Fall-Risk-Increasing Drugs. FallRisk-Increasing Drugs: A Systematic Review and Meta-analysis: III. Others. J. Am. Med. Dir. Assoc. 2018, 19, 372.e1–372.e8. [Google Scholar]
- Seppala, L.J.; Wermelink, A.; de Vries, M.; Ploegmakers, K.J.; van de Glind, E.M.M.; Daams, J.G.; van der Velde, N.; EUGMS task and Finish group on fall-risk-increasing drugs. FallRisk-Increasing Drugs: A Systematic Review and Meta-Analysis: II. Psychotropics. J. Am. Med. Dir. Assoc. 2018, 19, 371.e11–371.e17. [Google Scholar]
- Pighills, A.; Clemson, L. Environmental risk factors for falls. In Falls in Older People: Risk Factors, Strategies for Prevention and Implications for Practice, 3rd ed.; Lord, S., Sherrington, C., Naganathan, V., Eds.; Cambridge University Press: Cambridge, UK, 2021; pp. 202–210. [Google Scholar]
- Passi d’Argento. Epicentro, ISS. Available online: https://www.epicentro.iss.it/passi-argento/dati/cadute#dati (accessed on 13 October 2023).
- Cristofori, M.; Biscaglia, L.; Contoli, B.; Bianco, E.; De Luca, A.; Baldi, A.; Carrozzi, G.; Chiti, L.; Antoniotti, M.C.; Ferrelli, R.; et al. Falls in people over 64 years: Results from the nationwide surveillance system PASSI d’Argento, Italy 2012–13. Not. Ist. Super. Sanità 2013, 26, III–IV. [Google Scholar]
- Hopewell, S.; Adedire, O.; Copsey, B.J.; Boniface, G.J.; Sherrington, C.; Clemson, L.; Close, J.C.; Lamb, S.E. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2018, 7, CD012221. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing. 2022, 51, afac205. [Google Scholar] [CrossRef]
- Trevisan, C.; Crippa, A.; Ek, S.; Welmer, A.K.; Sergi, G.; Maggi, S.; Manzato, E.; Bea, J.W.; Cauley, J.A.; Decullier, E.; et al. Nutritional Status, Body Mass Index, and the Risk of Falls in Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2019, 20, 569–582.e7. [Google Scholar] [CrossRef]
- Piano Nazionale Linee Guida (PNLG), ISS, Prevenzione delle cadute da incidente domestico negli anziani, Doc 13 May 2007. Available online: salute.gov.it (accessed on 12 October 2023).
- Lewis, S.R.; Griffin, X.L. Preventing falls in older people: The evidence for environmental interventions and why history matters. Cochrane Database Syst. Rev. 2023, 3, ED000162. [Google Scholar] [CrossRef]
- Clemson, L.; Stark, S.; Pighills, A.C.; Fairhall, N.J.; Lamb, S.E.; Ali, J.; Sherrington, C. Environmental interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2023, 3, CD013258. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2019, 1, CD012424. [Google Scholar] [CrossRef]
- Caristia, S.; Campani, D.; Cannici, C.; Frontera, E.; Giarda, G.; Pisterzi, S.; Terranova, L.; Payedimarri, A.B.; Faggiano, F.; Dal Molin, A. Physical exercise and fall prevention: A systematic review and meta-analysis of experimental studies included in Cochrane reviews. Geriatr. Nurs. 2021, 42, 1275–1286. [Google Scholar] [CrossRef]
- Dautzenberg, L.; Beglinger, S.; Tsokani, S.; Zevgiti, S.; Raijmann, R.C.M.A.; Rodondi, N.; Scholten, R.J.P.M.; Rutjes, A.W.S.; Di Nisio, M.; Emmelot-Vonk, M.; et al. Interventions for preventing falls and fall-related fractures in community-dwelling older adults: A systematic review and network meta-analysis. J. Am. Geriatr. Soc. 2021, 69, 2973–2984. [Google Scholar] [CrossRef]
- Lamb, S.E.; Bruce, J.; Hossain, A.; Ji, C.; Longo, R.; Lall, R.; Bojke, C.; Hulme, C.; Withers, E.; Finnegan, S.; et al. Screening and Intervention to Prevent Falls and Fractures in Older People. N. Engl. J. Med. 2020, 383, 1848–1859. [Google Scholar] [CrossRef]
- Fardellone, P.; Salawati, E.; Le Monnier, L.; Goëb, V. Bone Loss, Osteoporosis, and Fractures in Patients with Rheumatoid Arthritis: A Review. J. Clin. Med. 2020, 9, 3361. [Google Scholar] [CrossRef]
- Bianchini, E.; Warmerdam, E.; Romijnders, R.; Stürner, K.H.; Baron, R.; Heinzel, S.; Pontieri, F.E.; Hansen, C.; Maetzler, W. Turning When Using Smartphone in Persons With and Those Without Neurologic Conditions: Observational Study. J. Med. Internet Res. 2023, 25, e41082. [Google Scholar] [CrossRef]
- Bruyneel, A.V.; Duclos, N.C. Effects of the use of mobile phone on postural and locomotor tasks: A scoping review. Gait Posture. 2020, 82, 233–241. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).