Fracture of the Lumbar Spine Associated with Ureteral Injury Mimicking Spondylodiscitis Followed by Cervical Spine Fracture in Patient with Ankylosing Hyperostosis
Abstract
1. Introduction
2. Case Report
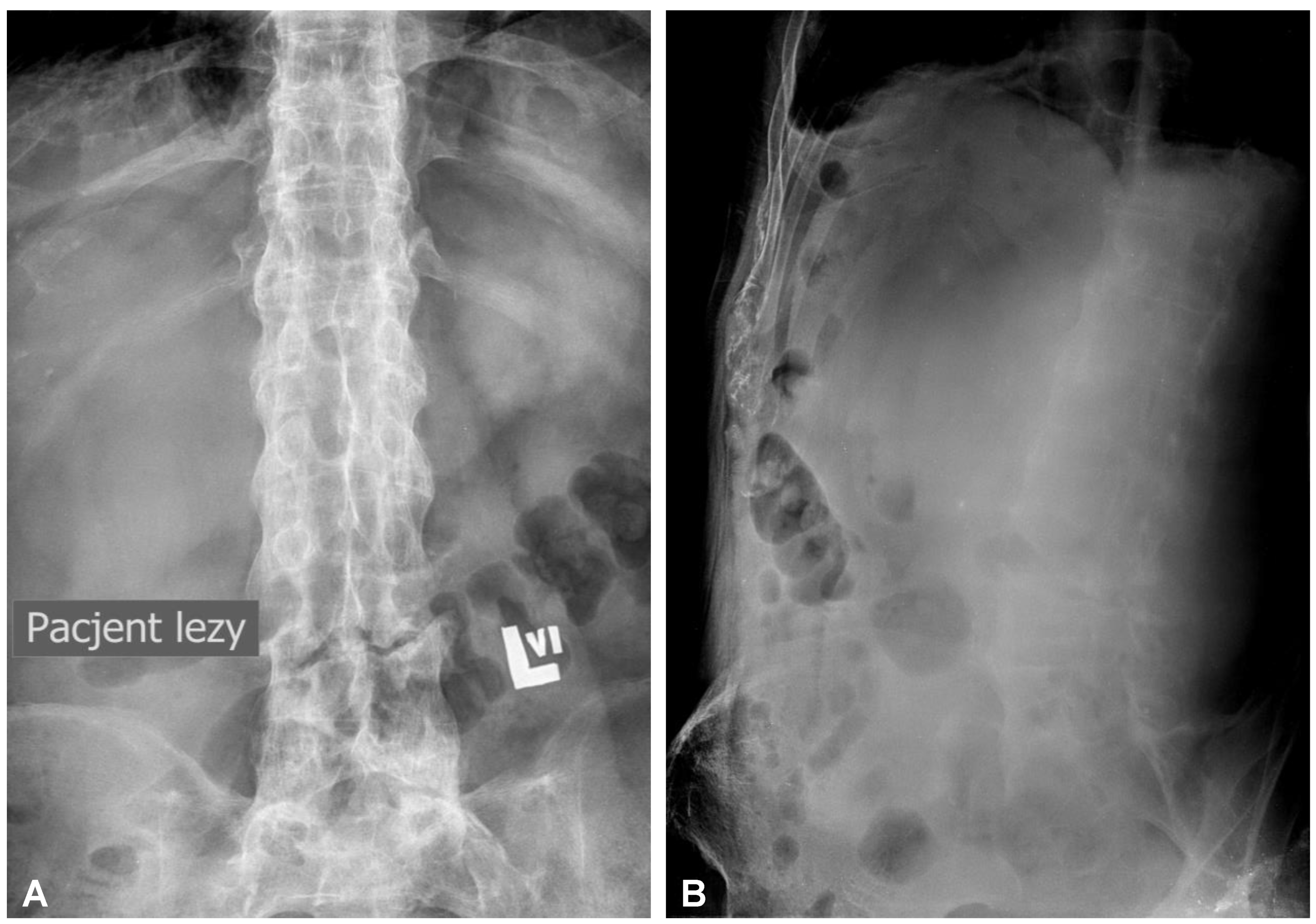
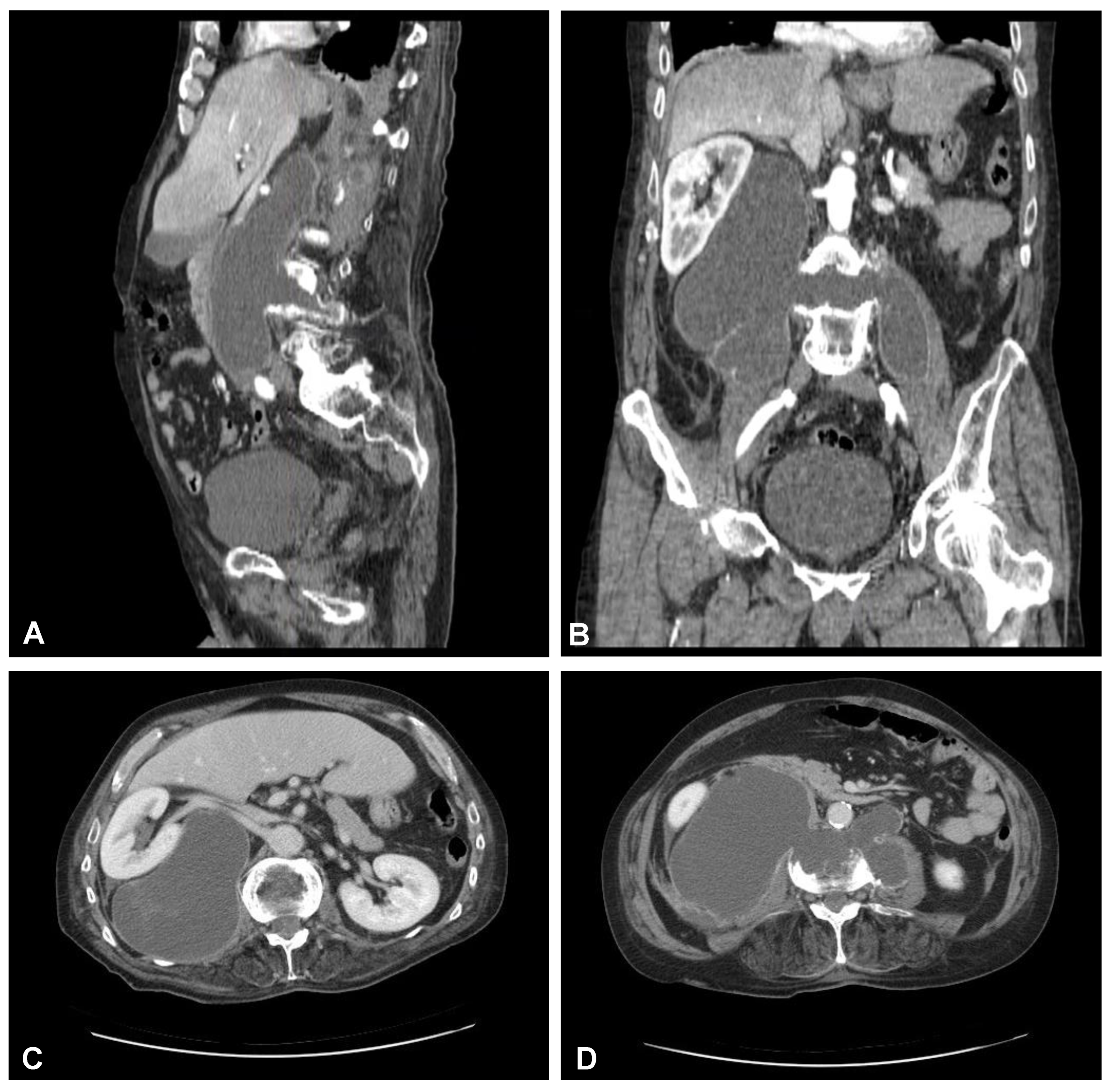
2.1. Clinical Presentation during the First Treatment Episode
2.2. Surgery of the Lumbar Spine Followed by Nephrectomy and Ureter Ligation
2.3. Clinical Presentation during the Second Treatment Episode
2.4. Surgery of the Cervical Spine Due to the Tetraparesis
3. Discussion
3.1. Pathophysiology and Practice Essentials of the Described Disease Entities
3.2. Actual State-of-the-Art
3.3. Clinical Recommendations and Practical Guidelines
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Whang, P.G.; Goldberg, G.; Lawrence, J.P.; Hong, J.; Harrop, J.S.; Anderson, D.G.; Albert, T.J.; Vaccaro, A.R. The management of spinal injuries in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: A comparison of treatment methods and clinical outcomes. J. Spinal Disord. Tech. 2009, 22, 77–85. [Google Scholar] [CrossRef] [PubMed]
- McGonagle, D.; Emery, P. Enthesitis, osteitis, microbes, biomechanics, and immune reactivity in ankylosing spondylitis. J. Rheumatol. 2000, 27, 2302–2304. [Google Scholar] [PubMed]
- Westerveld, L.A.; van Bemmel, J.C.; Dhert, W.J.; Oner, F.C.; Verlaan, J.J. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J. 2014, 14, 729–740. [Google Scholar] [CrossRef] [PubMed]
- Westerveld, L.A.; Verlaan, J.J.; Oner, F.C. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur. Spine J. 2009, 18, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.M.; Ogilvie, M.P.; Gomez-Rodriguez, J.C.; Ryan, M.L.; Peña, D.; Marttos, A.C.; Pizano, L.R.; McKenney, M.G. A review of ureteral injuries after external trauma. Scand. J. Trauma. Resusc. Emerg. Med. 2010, 18, 6. [Google Scholar] [CrossRef] [PubMed]
- Siram, S.M.; Gerald, S.Z.; Greene, W.R.; Hughes, K.; Oyetunji, T.A.; Chrouser, K.; Cornwell, E.E., 3rd; Chang, D.C. Ureteral trauma: Patterns and mechanisms of injury of an uncommon condition. Am. J. Surg. 2010, 199, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Kawasaki, S.; Shigematsu, H.; Matsumori, H.; Maegawa, N.; Tanaka, Y. Ureteral injury as a possible complication of vertebral fracture in a patient with ankylosing spinal hyperostosis. J. Orthop. Sci. 2018, 23, 194–196. [Google Scholar] [CrossRef] [PubMed]
- Oh, I.S.; Chang, D.G.; Kim, Y.H.; Ha, K.Y. Pure hyperextension injury of the lower lumbar spine with an ureteral impingement. Eur. Spine J. 2013, 22 (Suppl. S3), S353–S356. [Google Scholar] [CrossRef] [PubMed]
- Vaishya, R.; Vijay, V.; Nwagbara, I.C.; Agarwal, A.K. Diffuse idiopathic skeletal hyperostosis (DISH)—A common but less known cause of back pain. J. Clin. Orthop. Trauma 2017, 8, 191–196. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fornasier, V.L.; Littlejohn, G.; Urowitz, M.B.; Keystone, E.C.; Smythe, H.A. Spinal entheseal new bone formation: The early changes of spinal diffuse idiopathic skeletal hyperostosis. J. Rheumatol. 1983, 10, 939–947. [Google Scholar] [PubMed]
- Romero-Muñoz, L.M.; Tipper, G.; Segura-Fragoso, A.; Barriga-Martín, A. Outcomes of spinal cord injury following cervical fracture in ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis (DISH): A prospective cohort study. Neurocirugia (Astur. Engl. Ed.) 2022, 33, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Mansouri, A.; Tostivint, V.; Rouvellat, P.; Roumiguié, M.; Gamé, X.; Huyghe, E.; Rischmann, P.; Thanwerdas, J.; Malavaud, P. La longueur de l’uretère est-elle liée à la taille du patient? [Is the ureteral length associated with the patient’s size?]. Prog. Urol. 2019, 29, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Kominsky, H.D.; Shah, N.C.; Beecroft, N.J.; Diab, D.; Crescenze, I.M.; Posid, T.; Baradaran, N. Does Timing of Diagnosis and Management of Iatrogenic Ureter Injuries Affect Outcomes? Experience From a Tertiary Center. Urology 2021, 149, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.J.; Chang, M.Y.; Huang, P.C.; Chu, Y.C. Complete ureter avulsion causing a long defect as a complication of posterior spine fusion: A rare case treated with nonrobotic laparoscopic repair. Res. Rep. Urol. 2019, 11, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Olerud, C.; Frost, A.; Bring, J. Spinal fractures in patients with ankylosing spondylitis. Eur. Spine J. 1996, 5, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Fox, M.W.; Onofrio, B.M.; Kilgore, J.E. Neurological complications of ankylosing spondylitis. J. Neurosurg. 1993, 78, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Taggard, D.A.; Traynelis, V.C. Management of cervical spinal fractures in ankylosing spondylitis with posterior fixation. Spine 2000, 25, 2035–2039. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.Y.; d’Astorg, H.; Rousseau, M.A. Cervical spine surgery in ankylosing spondylitis: Review and current concept. Orthop. Traumatol. Surg. Res. 2015, 101, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Samartzis, D.; Anderson, D.G.; Shen, F.H. Multiple and simultaneous spine fractures in ankylosing spondylitis: Case report. Spine 2005, 30, E711–E715. [Google Scholar] [CrossRef] [PubMed]








Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woźnica, M.; Kaczor, S.; Poniatowski, Ł.A.; Raźniak, M.; Ząbek, M. Fracture of the Lumbar Spine Associated with Ureteral Injury Mimicking Spondylodiscitis Followed by Cervical Spine Fracture in Patient with Ankylosing Hyperostosis. J. Clin. Med. 2023, 12, 6937. https://doi.org/10.3390/jcm12216937
Woźnica M, Kaczor S, Poniatowski ŁA, Raźniak M, Ząbek M. Fracture of the Lumbar Spine Associated with Ureteral Injury Mimicking Spondylodiscitis Followed by Cervical Spine Fracture in Patient with Ankylosing Hyperostosis. Journal of Clinical Medicine. 2023; 12(21):6937. https://doi.org/10.3390/jcm12216937
Chicago/Turabian StyleWoźnica, Michał, Szymon Kaczor, Łukasz A. Poniatowski, Mikołaj Raźniak, and Mirosław Ząbek. 2023. "Fracture of the Lumbar Spine Associated with Ureteral Injury Mimicking Spondylodiscitis Followed by Cervical Spine Fracture in Patient with Ankylosing Hyperostosis" Journal of Clinical Medicine 12, no. 21: 6937. https://doi.org/10.3390/jcm12216937
APA StyleWoźnica, M., Kaczor, S., Poniatowski, Ł. A., Raźniak, M., & Ząbek, M. (2023). Fracture of the Lumbar Spine Associated with Ureteral Injury Mimicking Spondylodiscitis Followed by Cervical Spine Fracture in Patient with Ankylosing Hyperostosis. Journal of Clinical Medicine, 12(21), 6937. https://doi.org/10.3390/jcm12216937




