Sensory Information Modulates Voluntary Movement in an Individual with a Clinically Motor- and Sensory-Complete Spinal Cord Injury: A Case Report
Abstract
:1. Introduction
2. Detailed Case Description
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Edgerton, V.R.; Kim, S.J.; Ichiyama, R.M.; Gerasimenko, Y.P.; Roy, R.R. Rehabilitative therapies after spinal cord injury. J. Neurotrauma 2006, 23, 560–570. [Google Scholar] [CrossRef]
- Behrman, A.L.; Ardolino, E.M.; Harkema, S.J. Activity-Based Therapy: From Basic Science to Clinical Application for Recovery after Spinal Cord Injury. J. Neurol. Phys. Ther. 2017, 41 (Suppl. S3), S39–S45. [Google Scholar] [CrossRef] [PubMed]
- Harkema, S.; Behrman, A.; Barbeau, H. Evidence-based therapy for recovery of function after spinal cord injury. Handb. Clin. Neurol. 2012, 109, 259–274. [Google Scholar] [PubMed]
- Cote, M.P.; Murray, M.; Lemay, M.A. Rehabilitation Strategies after Spinal Cord Injury: Inquiry into the Mechanisms of Success and Failure. J. Neurotrauma 2017, 34, 1841–1857. [Google Scholar] [CrossRef]
- Barbeau, H.; Rossignol, S. Recovery of locomotion after chronic spinalization in the adult cat. Brain Res. 1987, 412, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Cai, L.L.; Courtine, G.; Fong, A.J.; Burdick, J.W.; Roy, R.R.; Edgerton, V.R. Plasticity of functional connectivity in the adult spinal cord. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2006, 361, 1635–1646. [Google Scholar] [CrossRef]
- Wolpaw, J.R. What can the spinal cord teach us about learning and memory? Neuroscientist 2010, 16, 532–549. [Google Scholar] [CrossRef]
- Rossignol, S. Locomotion and its recovery after spinal injury in animal models. Neurorehabil. Neural Repair 2002, 16, 201–206. [Google Scholar] [CrossRef]
- Courtine, G.; Gerasimenko, Y.; van den Brand, R.; Yew, A.; Musienko, P.; Zhong, H.; Song, B.; Ao, Y.; Ichiyama, R.M.; Lavrov, I.; et al. Transformation of nonfunctional spinal circuits into functional states after the loss of brain input. Nat. Neurosci. 2009, 12, 1333–1342. [Google Scholar] [CrossRef]
- van de Crommert, H.W.; Mulder, T.; Duysens, J. Neural control of locomotion: Sensory control of the central pattern generator and its relation to treadmill training. Gait Posture 1998, 7, 251–263. [Google Scholar] [CrossRef]
- Khorasanizadeh, M.; Yousefifard, M.; Eskian, M.; Lu, Y.; Chalangari, M.; Harrop, J.S.; Jazayeri, S.B.; Seyedpour, S.; Khodaei, B.; Hosseini, M.; et al. Neurological recovery following traumatic spinal cord injury: A systematic review and meta-analysis. J. Neurosurg. Spine 2019, 30, 683–699. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, J.W.; Curt, A.; Steeves, J.D.; Coleman, W.P.; Tuszynski, M.H.; Lammertse, D.; Bartlett, P.F.; Blight, A.R.; Dietz, V.; Ditunno, J.; et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: Spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord. 2007, 45, 190–205. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Draganich, C.; Thornton, W.A.; Berliner, J.C.; Lennarson, P.J.; Rejc, E.; Sevigny, M.; Charlifue, S.; Tefertiller, C.; Weber, K.A., 2nd. A single dermatome clinical prediction rule for independent walking one year after spinal cord injury. Arch. Phys. Med. Rehabil. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Fisher, C.G.; Noonan, V.K.; Smith, D.E.; Wing, P.C.; Dvorak, M.F.; Kwon, B. Motor recovery, functional status, and health-related quality of life in patients with complete spinal cord injuries. Spine 2005, 30, 2200–2207. [Google Scholar] [CrossRef]
- Kirshblum, S.; Millis, S.; McKinley, W.; Tulsky, D. Late neurologic recovery after traumatic spinal cord injury. Arch. Phys. Med. Rehabil. 2004, 85, 1811–1817. [Google Scholar] [CrossRef] [PubMed]
- Dimitrijevic, M.R. Motor control in chronic spinal cord injury patients. Scand. J. Rehabil. Med. Suppl. 1994, 30, 53–62. [Google Scholar]
- McKay, W.B.; Lim, H.K.; Priebe, M.M.; Stokic, D.S.; Sherwood, A.M. Clinical neurophysiological assessment of residual motor control in post-spinal cord injury paralysis. Neurorehabil. Neural Repair 2004, 18, 144–153. [Google Scholar] [CrossRef]
- Sherwood, A.M.; Dimitrijevic, M.R.; McKay, W.B. Evidence of subclinical brain influence in clinically complete spinal cord injury: Discomplete SCI. J. Neurol. Sci. 1992, 110, 90–98. [Google Scholar] [CrossRef]
- Tolle, H.; Rapacz, A.; Weintraub, B.; Shogren, C.; Harkema, S.J.; Gibson, J.L. Establishing the NeuroRecovery Network Community Fitness and Wellness facilities: Multi-site fitness facilities provide activity-based interventions and assessments for evidence-based functional gains in neurologic disorders. Disabil. Rehabil. 2018, 40, 3086–3093. [Google Scholar] [CrossRef]
- Kaiser, A.; Chan, K.; Pakosh, M.; Musselman, K.E. Characteristics of activity-based therapy interventions for people living with spinal cord injury or disease across the continuum of care: A scoping review protocol. BMJ Open 2020, 10, e040014. [Google Scholar] [CrossRef]
- Sadowsky, C.L.; McDonald, J.W. Activity-based restorative therapies: Concepts and applications in spinal cord injury-related neurorehabilitation. Dev. Disabil. Res. Rev. 2009, 15, 112–116. [Google Scholar] [CrossRef]
- Behrman, A.L.; Bowden, M.G.; Nair, P.M. Neuroplasticity after spinal cord injury and training: An emerging paradigm shift in rehabilitation and walking recovery. Phys. Ther. 2006, 86, 1406–1425. [Google Scholar] [CrossRef] [PubMed]
- Sherwood, A.M.; McKay, W.B.; Dimitrijevic, M.R. Motor control after spinal cord injury: Assessment using surface EMG. Muscle Nerve 1996, 19, 966–979. [Google Scholar] [CrossRef]
- Zytnicki, D.; Lafleur, J.; Horcholle-Bossavit, G.; Lamy, F.; Jami, L. Reduction of Ib autogenetic inhibition in motoneurons during contractionsof an ankle extensor muscle in the cat. J. Neurophysiol. 1990, 64, 1380–1389. [Google Scholar] [CrossRef]
- Wernig, A.; Müller, S.; Nanassy, A.; Cagol, E. Laufband therapy based on “rules of spinal locomotion” is effective in spinal cord injured persons. Eur. J. Neurosci. 1995, 7, 823–829. [Google Scholar] [CrossRef]
- Harkema, S.J.; Wernig, A.; Müeller, S.; Requejo, P.S.; Douglas, S.; Dobkin, B.H.; Edgerton, V.R. Human lumbar spinal cord generates appropriate motor output associated with weight supporting stepping. J. Neurol. Rehabil. 1995, 9, 125–126. [Google Scholar]
- Dietz, V.; Colombo, G.; Jensen, L.; Baumgartner, L. Locomotor capacity of spinal cord in paraplegic patients. Ann. Neurol. 1995, 37, 574–582. [Google Scholar] [CrossRef]
- Barbeau, H.; Nadeau, S.; Garneau, C. Physical determinants, emerging concepts, and training approaches in gait of individuals with spinal cord injury. J. Neurotrauma 2006, 23, 571–585. [Google Scholar] [CrossRef] [PubMed]
- Behrman, A.L.; Harkema, S.J. Physical rehabilitation as an agent for recovery after spinal cord injury. Phys. Med. Rehabil. Clin. N. Am. 2007, 18, 183–202. [Google Scholar] [CrossRef]
- Dietz, V.; Colombo, G. Recovery from spinal cord injury—Underlying mechanisms and efficacy of rehabilitation. Acta Neurochir. Suppl. 2004, 89, 95–100. [Google Scholar]
- De Leon, R.D.; Hodgson, J.A.; Roy, R.R.; Edgerton, V.R. Full weight-bearing hindlimb standing following stand training in the adult spinal cat. J. Neurophysiol. 1998, 80, 83–91. [Google Scholar] [CrossRef]
- de Leon, R.D.; Hodgson, J.A.; Roy, R.R.; Edgerton, V.R. Locomotor capacity attributable to step training versus spontaneous recovery after spinalization in adult cats. J. Neurophysiol. 1998, 79, 1329–1340. [Google Scholar] [CrossRef]
- Cha, J.; Heng, C.; Reinkensmeyer, D.J.; Roy, R.R.; Edgerton, V.R.; de Leon, R.D. Locomotor ability in spinal rats is dependent on the amount of activity imposed on the hindlimbs during treadmill training. J. Neurotrauma 2007, 24, 1000–1012. [Google Scholar] [CrossRef] [PubMed]
- Basso, D.M. Neuroanatomical substrates of functional recovery after experimental spinal cord injury: Implications of basic science research for human spinal cord injury. Phys. Ther. 2000, 80, 808–817. [Google Scholar] [CrossRef]
- Dietz, V.; Muller, R.; Colombo, G. Locomotor activity in spinal man: Significance of afferent input from joint and load receptors. Brain 2002, 125, 2626–2634. [Google Scholar] [CrossRef] [PubMed]
- Rossignol, S.; Dubuc, R.; Gossard, J.P. Dynamic sensorimotor interactions in locomotion. Physiol. Rev. 2006, 86, 89–154. [Google Scholar] [CrossRef]
- Harkema, S.J.; Hurley, S.L.; Patel, U.K.; Requejo, P.S.; Dobkin, B.H.; Edgerton, V.R. Human lumbosacral spinal cord interprets loading during stepping. J. Neurophysiol. 1997, 77, 797–811. [Google Scholar] [CrossRef] [PubMed]
- Timoszyk, W.K.; Nessler, J.A.; Acosta, C.; Roy, R.R.; Edgerton, V.R.; Reinkensmeyer, D.J.; de Leon, R. Hindlimb loading determines stepping quantity and quality following spinal cord transection. Brain Res. 2005, 1050, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Donkers, M.J.; An, K.N.; Chao, E.Y.; Morrey, B.F. Hand position affects elbow joint load during push-up exercise. J. Biomech. 1993, 26, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Rejc, E.; Angeli, C.A.; Bryant, N.; Harkema, S.J. Effects of Stand and Step Training with Epidural Stimulation on Motor Function for Standing in Chronic Complete Paraplegics. J. Neurotrauma 2017, 34, 1787–1802. [Google Scholar] [CrossRef]
- Angeli, C.A.; Edgerton, V.R.; Gerasimenko, Y.P.; Harkema, S.J. Altering spinal cord excitability enables voluntary movements after chronic complete paralysis in humans. Brain 2014, 137, 1394–1409. [Google Scholar] [CrossRef]
- Gill, M.L.; Grahn, P.J.; Calvert, J.S.; Linde, M.B.; Lavrov, I.A.; Strommen, J.A.; Beck, L.A.; Sayenko, D.G.; Van Straaten, M.G.; Drubach, D.I.; et al. Neuromodulation of lumbosacral spinal networks enables independent stepping after complete paraplegia. Nat. Med. 2018, 24, 1677–1682. [Google Scholar] [CrossRef]
- Angeli, C.A.; Boakye, M.; Morton, R.A.; Vogt, J.; Benton, K.; Chen, Y.; Ferreira, C.K.; Harkema, S.J. Recovery of Over-Ground Walking after Chronic Motor Complete Spinal Cord Injury. N. Engl. J. Med. 2018, 379, 1244–1250. [Google Scholar] [CrossRef] [PubMed]
- Darrow, D.; Balser, D.; Netoff, T.I.; Krassioukov, A.; Phillips, A.; Parr, A.; Samadani, U. Epidural Spinal Cord Stimulation Facilitates Immediate Restoration of Dormant Motor and Autonomic Supraspinal Pathways after Chronic Neurologically Complete Spinal Cord Injury. J. Neurotrauma 2019, 36, 2325–2336. [Google Scholar] [CrossRef] [PubMed]
- Peña Pino, I.; Hoover, C.; Venkatesh, S.; Ahmadi, A.; Sturtevant, D.; Patrick, N.; Freeman, D.; Parr, A.; Samadani, U.; Balser, D.; et al. Long-Term Spinal Cord Stimulation after Chronic Complete Spinal Cord Injury Enables Volitional Movement in the Absence of Stimulation. Front. Syst. Neurosci. 2020, 14, 35. [Google Scholar] [CrossRef]
- Mansour, N.M.; Pena Pino, I.; Freeman, D.; Carrabre, K.; Venkatesh, S.; Darrow, D.; Samadani, U.; Parr, A.M. Advances in Epidural Spinal Cord Stimulation to Restore Function after Spinal Cord Injury: History and Systematic Review. J. Neurotrauma 2022, 39, 1015–1029. [Google Scholar] [CrossRef] [PubMed]
- Garnier-Villarreal, M.; Pinto, D.; Mummidisetty, C.K.; Jayaraman, A.; Tefertiller, C.; Charlifue, S.; Taylor, H.B.; Chang, S.H.; McCombs, N.; Furbish, C.L.; et al. Predicting Duration of Outpatient Physical Therapy Episodes for Individuals with Spinal Cord Injury Based on Locomotor Training Strategy. Arch. Phys. Med. Rehabil. 2022, 103, 665–675. [Google Scholar] [CrossRef]
- Dionne, A.; Mac-Thiong, J.M.; Alsofyani, M.A.; Richard-Denis, A. Are early-onset spasms predictive of poor neurological recovery after traumatic spinal cord injury? J. Spinal Cord. Med. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Sangari, S.; Chen, B.; Grover, F.; Salsabili, H.; Sheth, M.; Gohil, K.; Hobbs, S.; Olson, A.; Eisner-Janowicz, I.; Anschel, A.; et al. Spasticity Predicts Motor Recovery for Patients with Subacute Motor Complete Spinal Cord Injury. Ann. Neurol. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Crane, D.A.; Hoffman, J.M.; Reyes, M.R. Benefits of an exercise wellness program after spinal cord injury. J. Spinal Cord. Med. 2017, 40, 154–158. [Google Scholar] [CrossRef]
- Heinemann, A.W.; Jayaraman, A.; Mummidisetty, C.K.; Spraggins, J.; Pinto, D.; Charlifue, S.; Tefertiller, C.; Taylor, H.B.; Chang, S.H.; Stampas, A.; et al. Experience of Robotic Exoskeleton Use at Four Spinal Cord Injury Model Systems Centers. J. Neurol. Phys. Ther. 2018, 42, 256–267. [Google Scholar] [CrossRef]
- Cragg, J.J.; Noonan, V.K.; Dvorak, M.; Krassioukov, A.; Mancini, G.B.; Borisoff, J.F. Spinal cord injury and type 2 diabetes: Results from a population health survey. Neurology 2013, 81, 1864–1868. [Google Scholar] [CrossRef]
- Cragg, J.J.; Noonan, V.K.; Krassioukov, A.; Borisoff, J. Cardiovascular disease and spinal cord injury: Results from a national population health survey. Neurology 2013, 81, 723–728. [Google Scholar] [CrossRef]
- Gorgey, A.S.; Dolbow, D.R.; Dolbow, J.D.; Khalil, R.K.; Castillo, C.; Gater, D.R. Effects of spinal cord injury on body composition and metabolic profile—Part I. J. Spinal Cord. Med. 2014, 37, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Sherwood, A.; McKay, W. Assessment of spasticity and upper motor neuron dysfunction. Wiley Encycl. Biomed. Eng. 2006, 5, 3306–3315. [Google Scholar]

| Task | Orientation | Position | Variations |
|---|---|---|---|
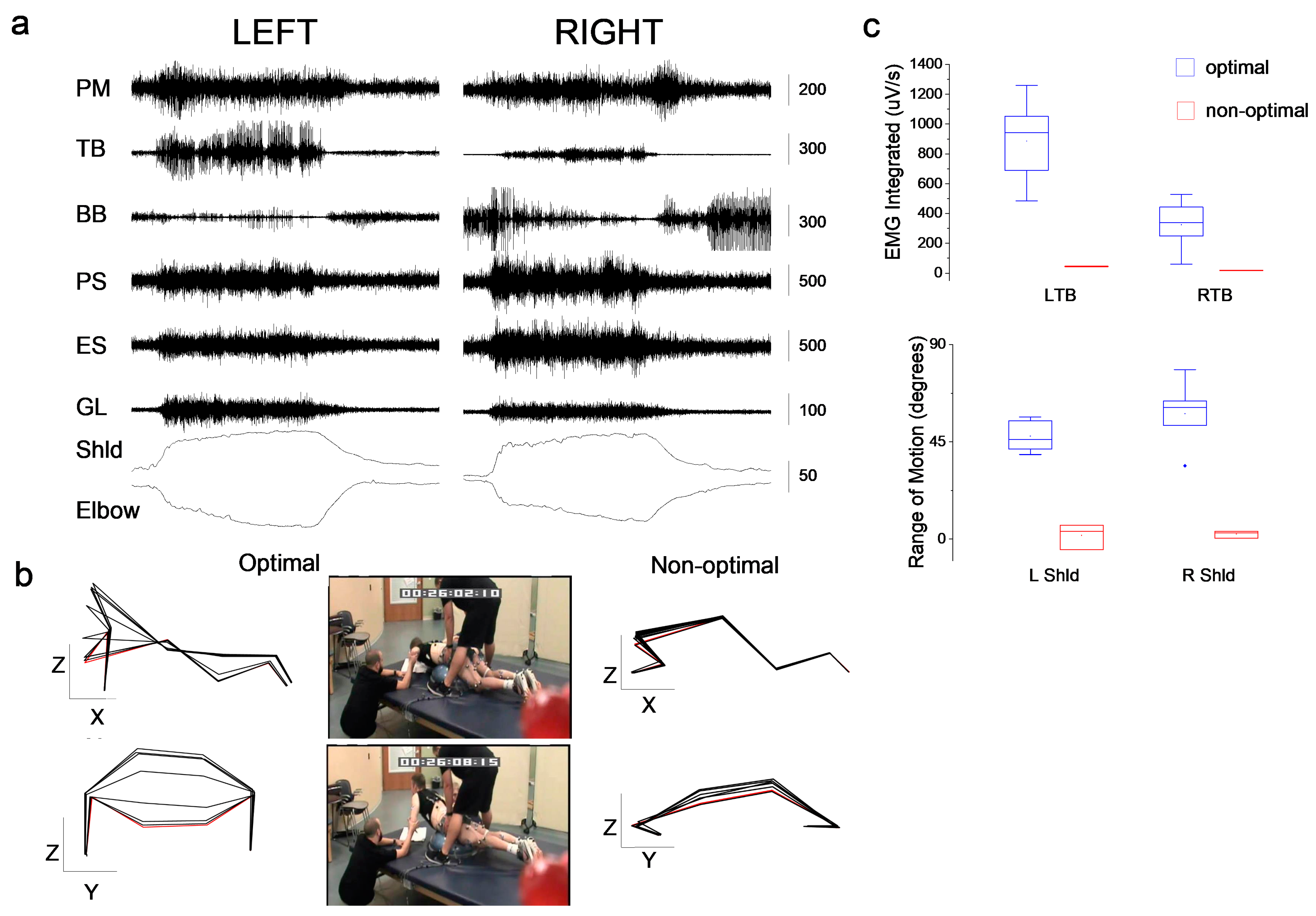
| Push-ups | Prone | Bosu ball under hips; hands facing forward; shoulder width apart |
|
| Shoulder flexion | Supine | Arms to side of trunk; legs extended | |
| Hip bridges | Supine | Arms to side of trunk; knees bent |
|
| Trunk extension | Sitting | Trunk forward |
|
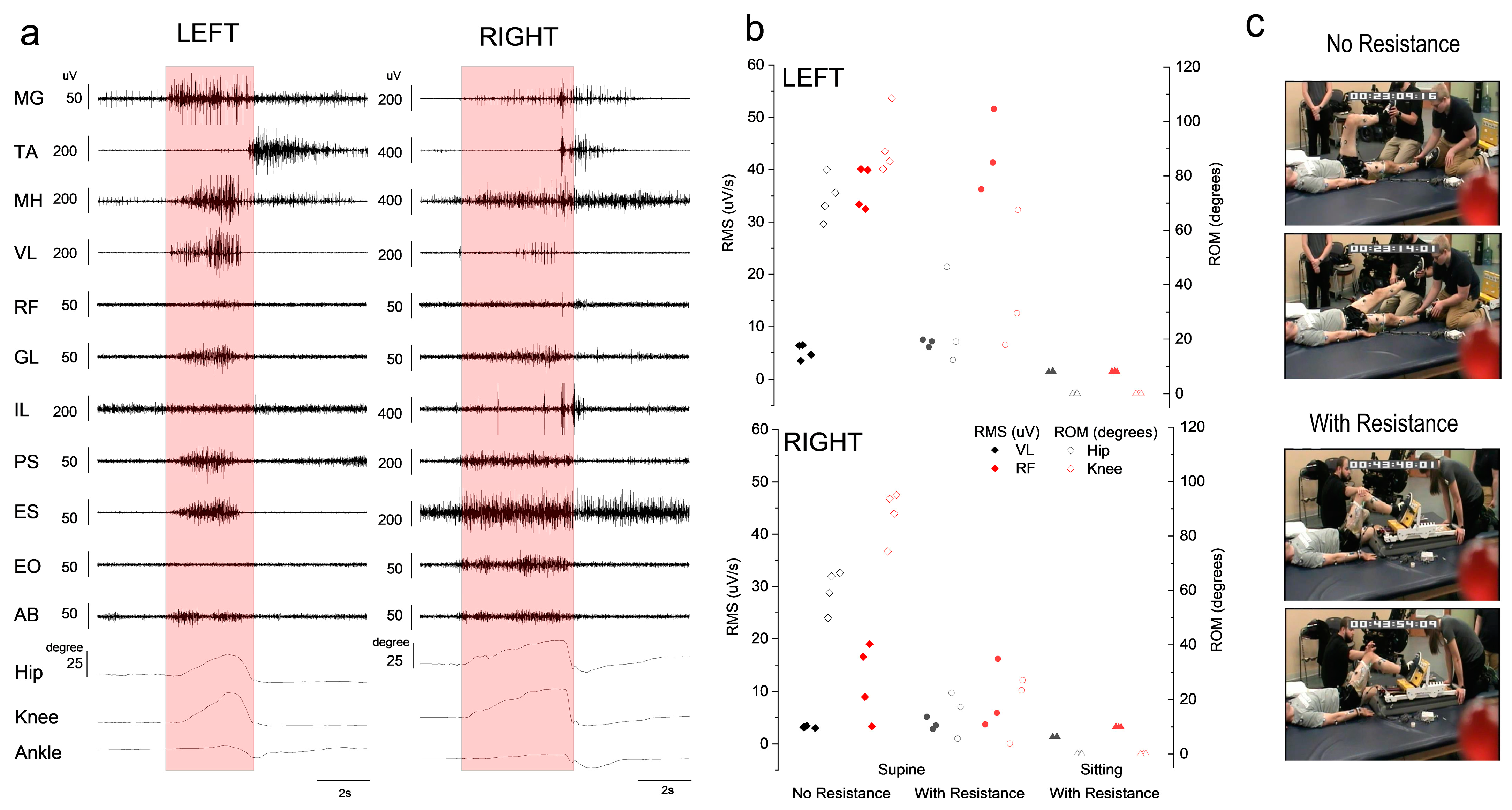
| Hip/knee extension | Supine | Arms to side of trunk; hip and knee bent; pressure on plantar surface of foot |
|
| Sitting | Sitting at edge of mat/chair |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angeli, C.; Wagers, S.; Harkema, S.; Rejc, E. Sensory Information Modulates Voluntary Movement in an Individual with a Clinically Motor- and Sensory-Complete Spinal Cord Injury: A Case Report. J. Clin. Med. 2023, 12, 6875. https://doi.org/10.3390/jcm12216875
Angeli C, Wagers S, Harkema S, Rejc E. Sensory Information Modulates Voluntary Movement in an Individual with a Clinically Motor- and Sensory-Complete Spinal Cord Injury: A Case Report. Journal of Clinical Medicine. 2023; 12(21):6875. https://doi.org/10.3390/jcm12216875
Chicago/Turabian StyleAngeli, Claudia, Sarah Wagers, Susan Harkema, and Enrico Rejc. 2023. "Sensory Information Modulates Voluntary Movement in an Individual with a Clinically Motor- and Sensory-Complete Spinal Cord Injury: A Case Report" Journal of Clinical Medicine 12, no. 21: 6875. https://doi.org/10.3390/jcm12216875
APA StyleAngeli, C., Wagers, S., Harkema, S., & Rejc, E. (2023). Sensory Information Modulates Voluntary Movement in an Individual with a Clinically Motor- and Sensory-Complete Spinal Cord Injury: A Case Report. Journal of Clinical Medicine, 12(21), 6875. https://doi.org/10.3390/jcm12216875







