Congenital, Acquired, and Trauma-Related Risk Factors for Thoracic Outlet Syndrome—Review of the Literature
Abstract
1. Introduction
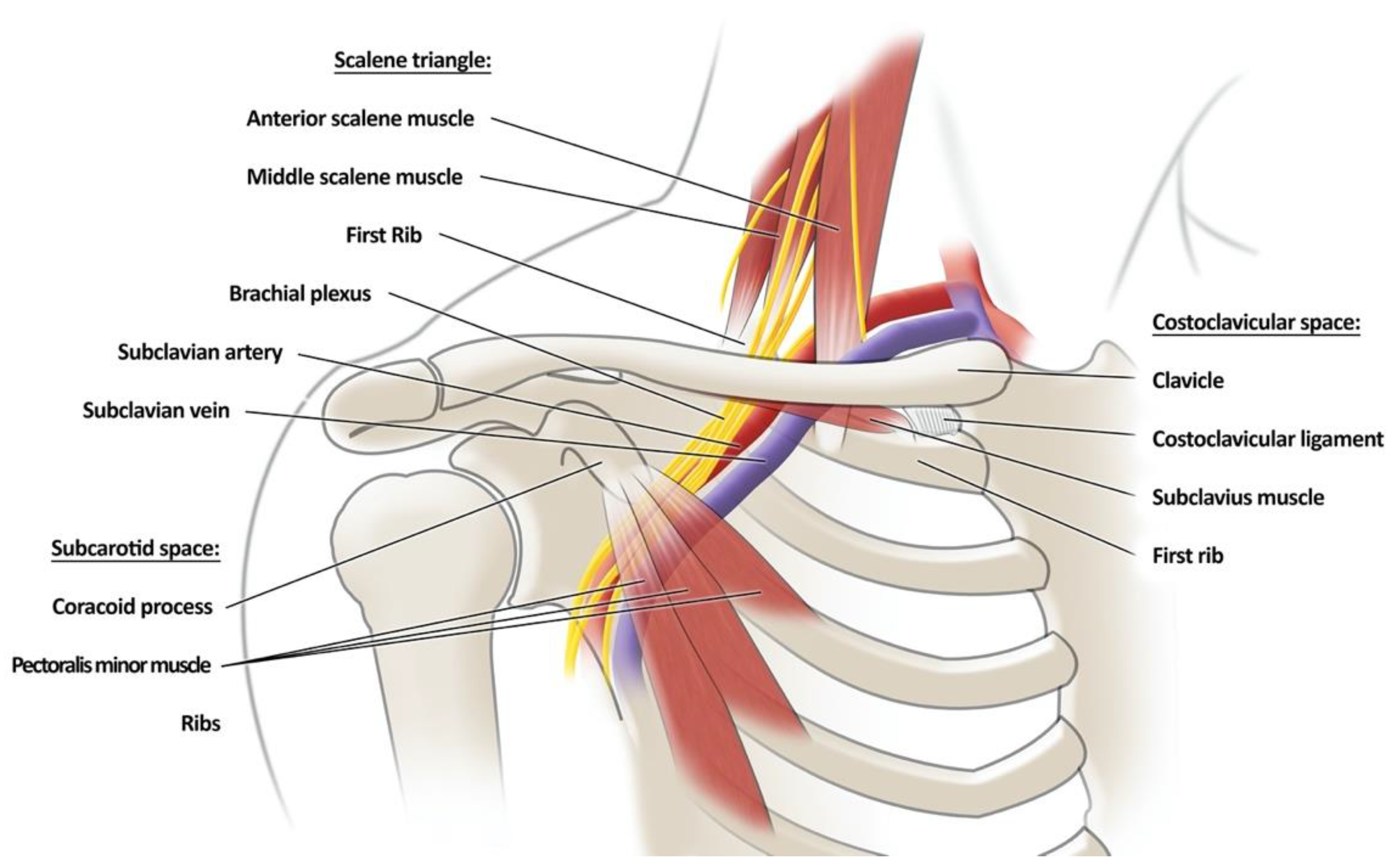
2. Anatomy of the Thoracic Outlet—Figure 1
3. Congenital Risk Factor
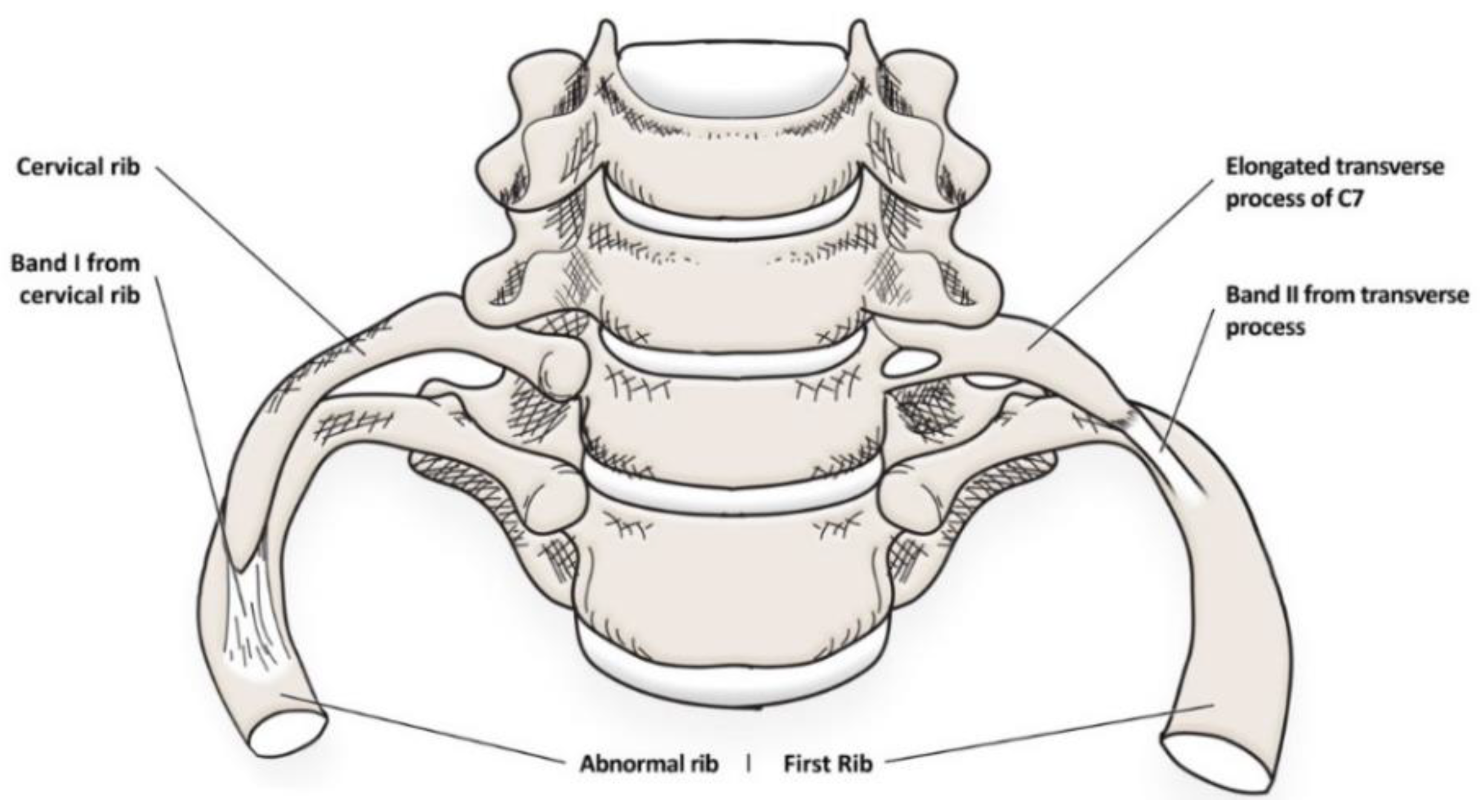
3.1. Bone Abnormalities
3.1.1. Cervical Ribs (CR)
3.1.2. Elongated Transverse Process of C7
3.1.3. First Rib Variation
3.1.4. Congenital Pseudoarthrosis of the Clavicle
3.2. Muscle Variation Associated with Thoracic Outlet Syndrome
3.2.1. Anterior Scalene Muscle
3.2.2. Middle Scalene Muscle
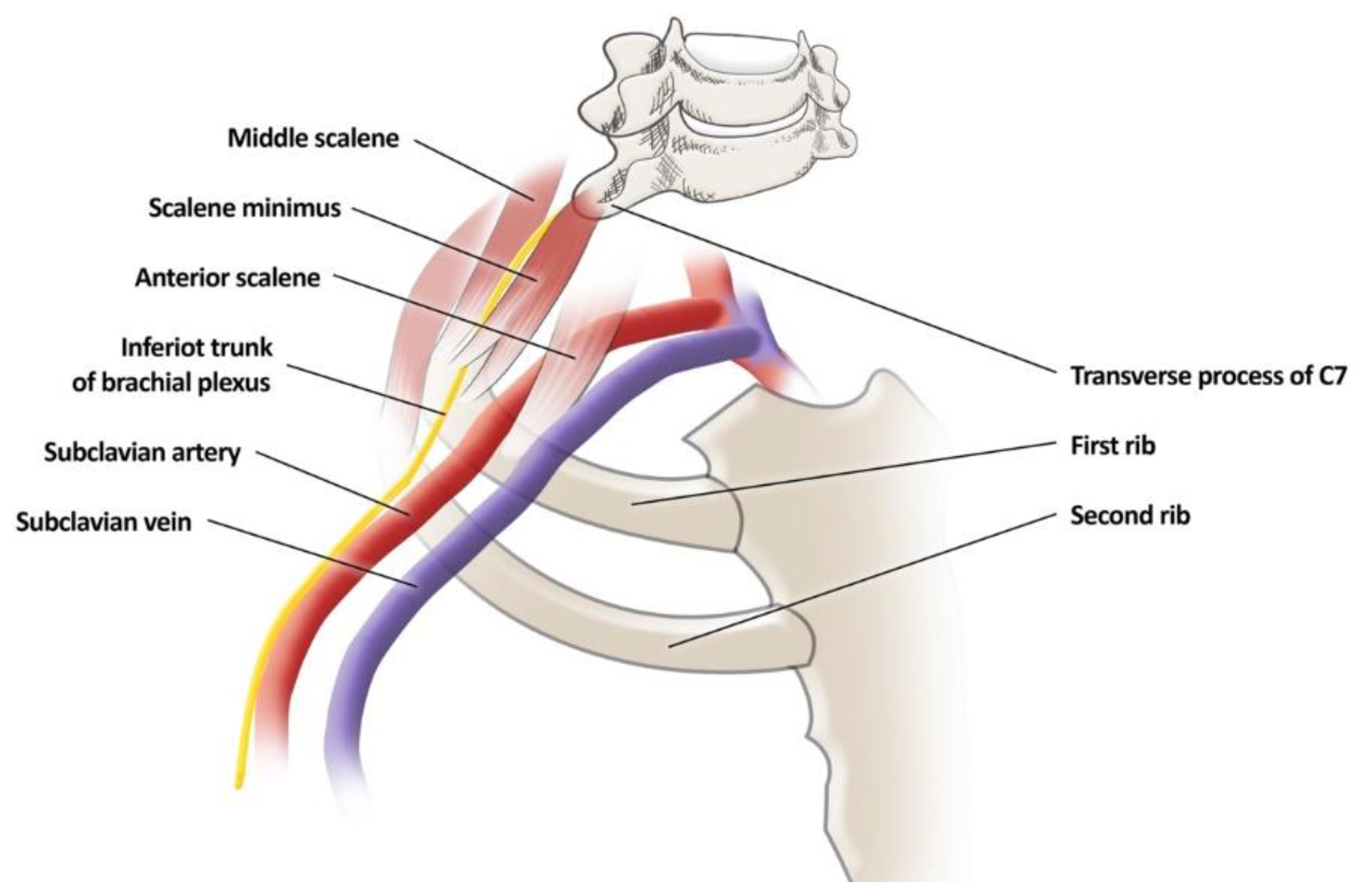
3.2.3. Scalenus Minimus Muscle
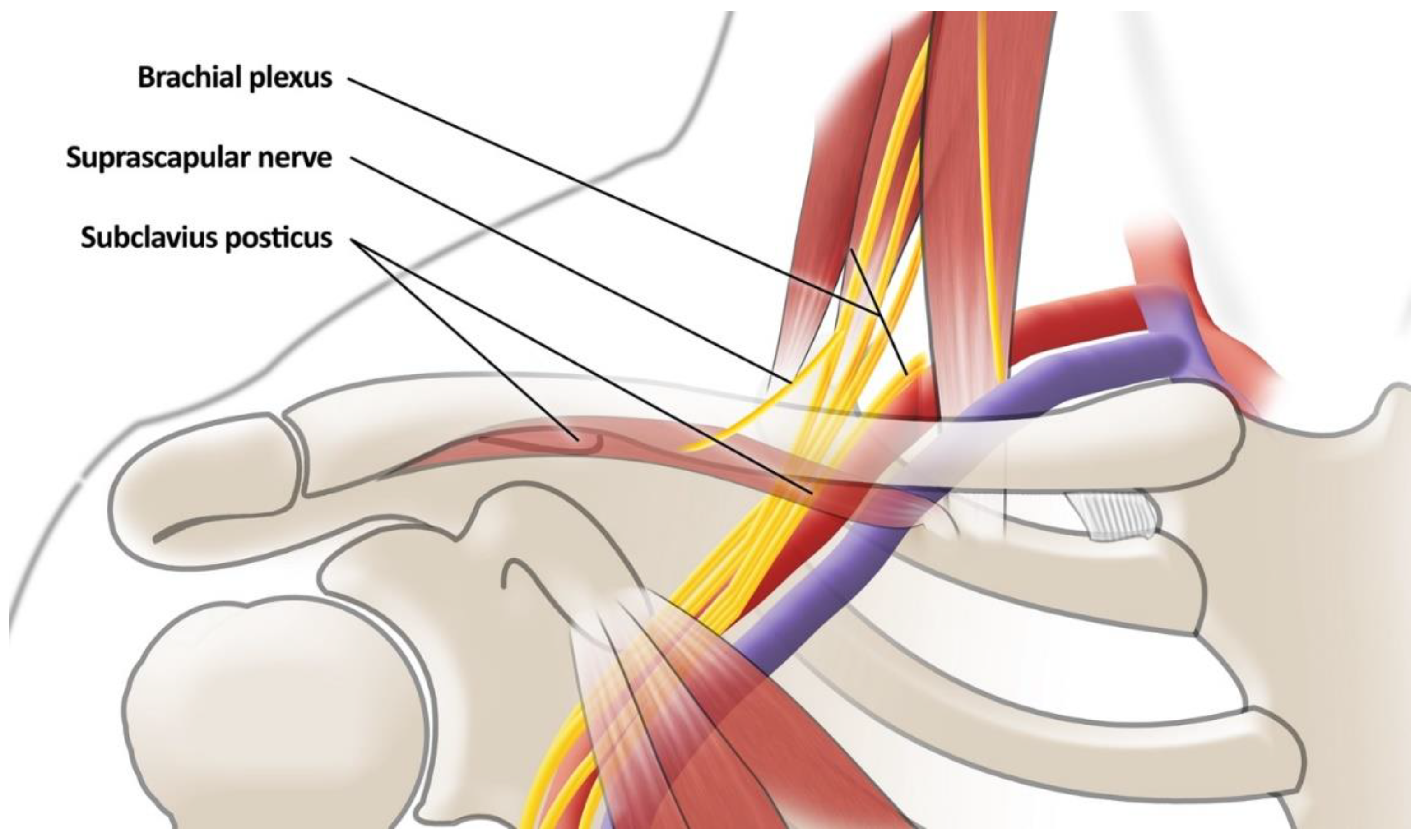
3.2.4. Subclavius Posticous Muscle (SPM)—Figure 4
3.2.5. Ectopic Insertion of the Pectoralis Minor (PM)
3.3. Brachial Plexus Variation Associated with TOS
- Single-piercing type—the superior trunk of BP passing through AS;
- Multiple-piercing type—superior and middle trunk of BP separately piercing AS;
- C5 piercing type;
- C5 anterior type—C5 and C6 coursed in front of the AS.
3.4. Inborn Ligaments and Bands
3.5. Superior Pleural Sinus
4. Acquired Risk Factors
4.1. Changes in Muscle Structures Lead to TOS
4.1.1. Hypertrophy of the Anterior Scalenus Muscle
4.1.2. Hypertrophy of the Subclavius Muscle
4.2. Sports Associated with the Risk of TOS Development: Repetitive Overhead Movements
4.3. Lower Position of the Shoulder Girdle
4.4. Hypermobility of the Shoulder Joint
4.5. Occupations Associated with a Risk of TOS
4.6. Thrombophilia
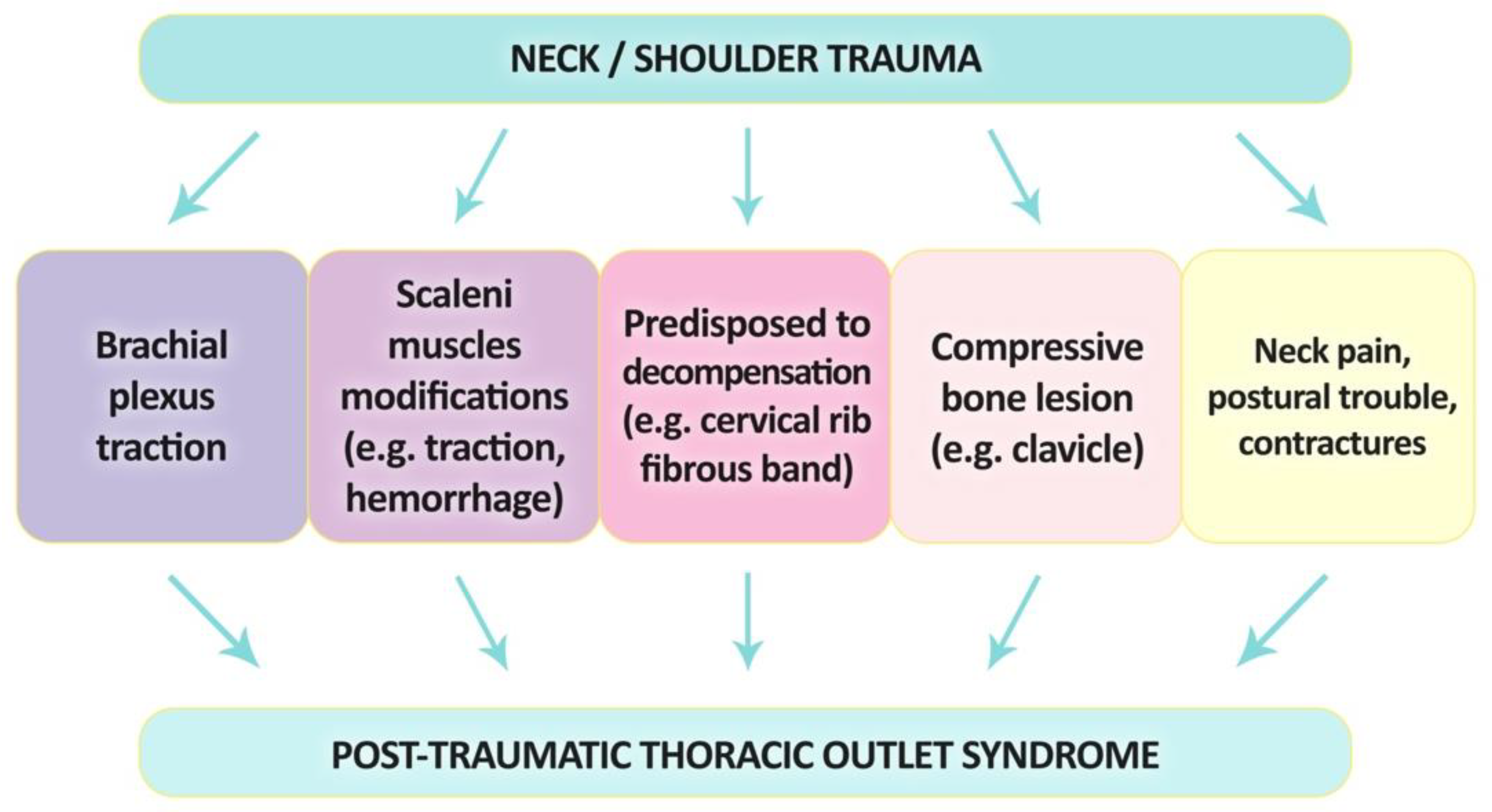
5. Trauma-Related Thoracic Outlet Syndrome (TR-TOS)
5.1. Pathophysiology—Trauma of the Shoulder or Neck
5.2. Incidence of TR-TOS
5.3. TOS Secondary to Inflammations
6. Risk Factors and Treatment
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Stewman, C.; Vitanzo, P.C.; Harwood, M.I. Neurologic Thoracic Outlet Syndrome: Summarizing a Complex History and Evolution. Curr. Sports Med. Rep. 2014, 13, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Bordoni, B.; Varacallo, M. Anatomy, Head and Neck, Scalenus Muscle; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Laulan, J.; Fouquet, B.; Rodaix, C.; Jauffret, P.; Roquelaure, Y.; Descatha, A. Thoracic Outlet Syndrome: Definition, Aetiological Factors, Diagnosis, Management and Occupational Impact. J. Occup. Rehabil. 2011, 21, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Freischlag, J.; Orion, K. Understanding Thoracic Outlet Syndrome. Scientifica 2014, 2014, 248163. [Google Scholar] [CrossRef]
- Masocatto, N.O.; Da-Matta, T.; Prozzo, T.G.; Couto, W.J.; Porfirio, G. Thoracic Outlet Syndrome: A Narrative Review. Rev. Col. Bras. Cir. 2019, 46, e20192243. [Google Scholar] [CrossRef] [PubMed]
- Janák, D.; Novotný, K.; Roček, M.; Rohn, V. Thoracic Outlet Syndrome: A Significant Family Genetic Phenotypic Presentation. Prague Med. Rep. 2016, 117, 117–123. [Google Scholar] [CrossRef]
- Goeteyn, J.; Pesser, N.; van Nuenen, B.; van Sambeek, M.; Teijink, J. Familial Predisposition of Thoracic Outlet Syndrome: Does a Familial Syndrome Exist? Report of Cases and Review of Literature. Acta Chir. Belg. 2021, 121, 211–214. [Google Scholar] [CrossRef]
- Hooper, T.L.; Denton, J.; McGalliard, M.K.; Brismée, J.M.; Sizer, P.S. Thoracic Outlet Syndrome: A Controversial Clinical Condition. Part 1: Anatomy, and Clinical Examination/Diagnosis. J. Man. Manip. Ther. 2010, 18, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Illig, K.A.; Rodriguez-Zoppi, E.; Bland, T.; Muftah, M.; Jospitre, E. The Incidence of Thoracic Outlet Syndrome. Ann. Vasc. Surg. 2021, 70, 263–272. [Google Scholar] [CrossRef]
- Otoshi, K.; Kikuchi, S.; Kato, K.; Sato, R.; Igari, T.; Kaga, T.; Shishido, H.; Konno, S.; Koga, R.; Furushima, K.; et al. The Prevalence and Characteristics of Thoracic Outlet Syndrome in High School Baseball Players. Health 2017, 9, 1223–1234. [Google Scholar] [CrossRef]
- Maru, S.; Dosluoglu, H.; Dryjski, M.; Cherr, G.; Curl, G.R.; Harris, L.M. Thoracic Outlet Syndrome in Children and Young Adults. Eur. J. Vasc. Endovasc. Surg. 2009, 38, 560–564. [Google Scholar] [CrossRef]
- Balderman, J.; Abuirqeba, A.A.; Eichaker, L.; Pate, C.; Earley, J.A.; Bottros, M.M.; Jayarajan, S.N.; Thompson, R.W. Physical Therapy Management, Surgical Treatment, and Patient-Reported Outcomes Measures in a Prospective Observational Cohort of Patients with Neurogenic Thoracic Outlet Syndrome. J. Vasc. Surg. 2019, 70, 832–841. [Google Scholar] [CrossRef]
- Sanders, R.J.; Hammond, S.L.; Rao, N.M. Diagnosis of Thoracic Outlet Syndrome. J. Vasc. Surg. 2007, 46, 601–604. [Google Scholar] [CrossRef]
- Henry, B.M.; Vikse, J.; Sanna, B.; Taterra, D.; Gomulska, M.; Pękala, P.A.; Tubbs, R.S.; Tomaszewski, K.A. Cervical Rib Prevalence and Its Association with Thoracic Outlet Syndrome: A Meta-Analysis of 141 Studies with Surgical Considerations. World Neurosurg. 2018, 110, e965–e978. [Google Scholar] [CrossRef] [PubMed]
- Connolly, M.R.; Auchincloss, H.G. Anatomy and Embryology of the Thoracic Outlet. Thorac. Surg. Clin. 2021, 31, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kitsis, C.K.; Marino, A.J.; Krikler, S.J.; Birch, R. Late Complications Following Clavicular Fractures and Their Operative Management. Injury 2003, 34, 69–74. [Google Scholar] [CrossRef]
- Sanders, R.J. Anatomy of the Thoracic Outlet and Related Structures. In Thoracic Outlet Syndrome; Springer: London, UK, 2013; pp. 17–24. [Google Scholar] [CrossRef]
- Paraskevas, G.; Natsis, K.; Ioannidis, O.; Papaziogas, B.; Kitsoulis, P.; Spanidou, S. Accessory Muscles in the Lower Part of the Anterior Compartment of the Arm That May Entrap Neurovascular Elements. Clin. Anat. 2008, 21, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Weber, A.E.; Criado, E. Relevance of Bone Anomalies in Patients with Thoracic Outlet Syndrome. Ann. Vasc. Surg. 2014, 28, 924–932. [Google Scholar] [CrossRef]
- Aignatoaei, A.M.; Moldoveanu, C.E.; Caruntu, I.D.; Giusca, S.E.; Vicoleanu, S.P.; Nedelcu, A.H. Incidental Imaging Findings of Congenital Rib Abnormalities—A Case Series and Review of Developmental Concepts. Folia Morphol. 2018, 77, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.R.; Prabhakar, A.; Viswanath, O.; Urits, I.; Green, J.B.; Kendrick, J.B.; Brunk, A.J.; Eng, M.R.; Orhurhu, V.; Cornett, E.M.; et al. Thoracic Outlet Syndrome: A Comprehensive Review of Pathophysiology, Diagnosis, and Treatment. Pain. Ther. 2019, 8, 5–18. [Google Scholar] [CrossRef]
- Sanders, R.J.; Hammond, S.L. Management of Cervical Ribs and Anomalous First Ribs Causing Neurogenic Thoracic Outlet Syndrome. J. Vasc. Surg. 2002, 36, 51–56. [Google Scholar] [CrossRef]
- Gruber, W. Ueber Die Halsrippen des Menschen Vergleichend-Anatomischen Remerkungen. Scientia 1869, 2, 7–27. [Google Scholar]
- Paton, G.J.; Billings, B.K. Cervical Rib Synostosis to the First Rib: A Rare Anatomic Variation. World Neurosurg. 2020, 138, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Walden, M.J.; Adin, M.E.; Visagan, R.; Viertel, V.G.; Intrapiromkul, J.; Maluf, F.; Patel, N.V.; Alluwaimi, F.; Lin, D.; Yousem, D.M. Cervical Ribs: Identification on MRI and Clinical Relevance. Clin. Imaging 2013, 37, 938–941. [Google Scholar] [CrossRef]
- Hardy, A.; Pougès, C.; Wavreille, G.; Behal, H.; Demondion, X.; Lefebvre, G. Thoracic Outlet Syndrome: Diagnostic Accuracy of MRI. Orthop. Traumatol. Surg. Res. 2019, 105, 1563–1569. [Google Scholar] [CrossRef] [PubMed]
- White, R.; Hollier, L. Vascular Surgery: Basic Science and Clinical Correlations; John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Todd, T.W. The Relations of the Thoracic Operculum Considered in Reference to the Anatomy of Cervical Ribs of Surgical Importance. J. Anat. Physiol. 1911, 45, 293–304. [Google Scholar] [PubMed]
- Sanders, R.J.; Hammond, S.L.; Rao, N.M. Thoracic Outlet Syndrome: A Review. Neurologist 2008, 14, 365–373. [Google Scholar] [CrossRef]
- Chang, C.S.; Chwei-Chin Chuang, D.; Chin, S.C.; Chang, C.J. An Investigation of the Relationship between Thoracic Outlet Syndrome and the Dimensions of the First Rib and Clavicle. J. Plast. Reconstr. Aesthetic Surg. 2011, 64, 1000–1006. [Google Scholar] [CrossRef] [PubMed]
- Gharagozloo, F.; Meyer, M.; Tempesta, B.; Strother, E.; Margolis, M.; Neville, R. Proposed Pathogenesis of Paget-Schroetter Disease: Impingement of the Subclavian Vein by a Congenitally Malformed Bony Tubercle on the First Rib. J. Clin. Pathol. 2012, 65, 262–266. [Google Scholar] [CrossRef]
- Gharagozloo, F.; Meyer, M.; Tempesta, B.J.; Margolis, M.; Strother, E.T.; Tummala, S. Robotic En Bloc First-Rib Resection for Paget-Schroetter Disease, a Form of Thoracic Outlet Syndrome: Technique and Initial Results. Innovations 2012, 7, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Gharagozloo, F.; Meyer, M.; Tempesta, B.; Gruessner, S. Robotic Transthoracic First-Rib Resection for Paget-Schroetter Syndrome. Eur. J. Cardiothorac. Surg. 2019, 55, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Gharagozloo, F.; Atiquzzaman, N.; Meyer, M.; Tempesta, B.; Werden, S. Robotic First Rib Resection for Thoracic Outlet Syndrome. J. Thorac. Dis. 2021, 13, 6141–6154. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, K.A.; Leino, E.; Lepäntalo, M.; Paukku, P. Recurrent Thoracic Outlet Syndrome after First Rib Resection. Arch. Phys. Med. Rehabil. 1991, 72, 208–210. [Google Scholar] [PubMed]
- Gelabert, H.A.; Jabori, S.; Barleben, A.; Kiang, S.; O’Connell, J.; Jimenez, J.C.; DeRubertis, B.; Rigberg, D. Regrown First Rib in Patients with Recurrent Thoracic Outlet Syndrome. Ann. Vasc. Surg. 2014, 28, 933–938. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, M.J.P.S.S.; dos Reis Braga, S.; Akkari, M.; Prado, J.C.L.; Santili, C. Congenital Pseudarthrosis of the Clavicle. Rev. Bras. Ortop. 2012, 47, 21. [Google Scholar] [CrossRef] [PubMed]
- Lozano, P.; Díaz, M.; Riera, R.; Gomez, F.T. Venous Thoracic Outlet Syndrome Secondary to Congenital Pseudoarthrosis of the Clavicle. Presentation in the Fourth Decade of Life. Eur. J. Vasc. Endovasc. Surg. 2003, 25, 592–593. [Google Scholar] [CrossRef] [PubMed]
- Hahn, K.; Shah, R.; Shalev, Y.; Schmidt, D.H.; Bajwa, T. Congenital Clavicular Pseudoarthrosis Associated with Vascular Thoracic Outlet Syndrome: Case Presentation and Review of the Literature. Cathet Cardiovasc. Diagn. 1995, 35, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Khu, K.; Midha, R. Clavicle Pseudarthrosis: A Rare Cause of Thoracic Outlet Syndrome. Can. J. Neurol. Sci. 2010, 37, 863–865. [Google Scholar] [CrossRef]
- Bargar, W.L.; Marcus, R.E.; Ittleman, F.P. Late Thoracic Outlet Syndrome Secondary to Pseudarthrosis of the Clavicle. J. Trauma 1984, 24, 857–859. [Google Scholar] [CrossRef] [PubMed]
- Watson, H.I.; Hopper, G.P.; Kovacs, P. Congenital Pseudarthrosis of the Clavicle Causing Thoracic Outlet Syndrome. BMJ Case Rep. 2013, 2013, bcr2013010437. [Google Scholar] [CrossRef] [PubMed]
- Heyn, J.; Ozimek, A.; Sadeghi-Azandaryani, M.; Bürklein, D.; Steckmeier, B. Thoracic Outlet Syndrome Caused by a Pseudoaneurysm after Pseudarthrosis of the Clavicle. Eur. J. Trauma. Emerg. Surg. 2008, 34, 511–514. [Google Scholar] [CrossRef]
- Makhoul, R.G.; Machleder, H.I. Developmental Anomalies at the Thoracic Outlet: An Analysis of 200 Consecutive Cases. J. Vasc. Surg. 1992, 16, 534–545. [Google Scholar] [CrossRef] [PubMed]
- Collins, R.M.; Bhana, J.; Patricios, J.S.; Du Plessis, A.; Veller, M.; Schultz, D.; Janse Van Rensburg, D.C. Thoracic Outlet Syndrome in a Patient with Absent Scalenus Anterior Muscle. Clin. J. Sport. Med. 2014, 24, 268–270. [Google Scholar] [CrossRef]
- Valera-Calero, J.A.; Gómez-Sánchez, S.; Fernández-de-las-Peñas, C.; Plaza-Manzano, G.; Sánchez-Jorge, S.; Navarro-Santana, M.J. A Procedure for Measuring Anterior Scalene Morphology and Quality with Ultrasound Imaging: An Intra- and Inter-Rater Reliability Study. Ultrasound Med. Biol. 2023, 49, 1817–1823. [Google Scholar] [CrossRef] [PubMed]
- McNamara, K.P.; Greene, K.A.; Tooze, J.A.; Dang, J.; Khattab, K.; Lenchik, L.; Weaver, A.A. Neck Muscle Changes Following Long-Duration Spaceflight. Front. Physiol. 2019, 10, 1115. [Google Scholar] [CrossRef] [PubMed]
- Weaver, M.L.; Hicks, C.W.; Fritz, J.; Black, J.H.; Lum, Y.W. Local Anesthetic Block of the Anterior Scalene Muscle Increases Muscle Height in Patients with Neurogenic Thoracic Outlet Syndrome. Ann. Vasc. Surg. 2019, 59, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Greene, K.A.; Tooze, J.A.; Lenchik, L.; Weaver, A.A. Change in Lumbar Muscle Size and Composition on MRI with Long-Duration Spaceflight. Ann. Biomed. Eng. 2022, 50, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Thomas, G.I.; Jones, T.W.; Stavney, L.S.; Manhas, D.R. The Middle Scalene Muscle and Its Contribution to the Thoracic Outlet Syndrome. Am. J. Surg. 1983, 145, 589–592. [Google Scholar] [CrossRef]
- Paraskevas, G.; Ioannidis, O.; Papaziogas, B.; Natsis, K.; Spanidou, S.; Kitsoulis, P. An Accessory Middle Scalene Muscle Causing Thoracic Outlet Syndrome. Folia Morphol. 2007, 66, 194–197. [Google Scholar]
- Natsis, K.; Totlis, T.; Didagelos, M.; Tsakotos, G.; Vlassis, K.; Skandalakis, P. Scalenus Minimus Muscle: Overestimated or Not? An Anatomical Study. Am. Surg. 2013, 79, 372–374. [Google Scholar] [CrossRef]
- Machleder, H.I.; Moll, F.; Verity, M.A. The Anterior Scalene Muscle in Thoracic Outlet Compression Syndrome: Histochemical and Morphometric Studies. Arch. Surg. 1986, 121, 1141–1144. [Google Scholar] [CrossRef] [PubMed]
- Stott, C.F. A Note on the Scalenus Minimus Muscle. J. Anat. 1928, 62, 359–361. [Google Scholar] [PubMed]
- Savgaonkar, M.G.; Chimmalgi, M.; Kulkarni, U.K. Anatomy of Inter-Scalene Triangle and Its Role in Thoracic Outlet Compression Syndrome. J. Anat. Soc. India 2006, 55, 52–55. [Google Scholar]
- Sanli, E.C.; Aktekin, M.; Kurtoglu, Z. A Case of Large Scalenus Minimus Muscle. Neurosciences 2007, 12, 336–337. [Google Scholar]
- Ulusoy, O.L.; Alis, D.; Oz, A.; Barlas, S.B.; Sokmen, B.K.; Sever, S.; Mutlu, A.; Colakoglu, B. The Prevalence and Characteristics of the Subclavius Posticus Muscle in the Adult Population on MRI. Surg. Radiol. Anat. 2018, 40, 1141–1145. [Google Scholar] [CrossRef] [PubMed]
- Akita, K.; Ibukuro, K.; Yamaguchi, K.; Heima, S.; Sato, T. The Subclavius Posticus Muscle: A Factor in Arterial, Venous or Brachial Plexus Compression? Surg. Radiol. Anat. 2000, 22, 111–115. [Google Scholar] [CrossRef]
- Cogar, A.C.; Johnsen, P.H.; Potter, H.G.; Wolfe, S.W. Subclavius Posticus: An Anomalous Muscle in Association with Suprascapular Nerve Compression in an Athlete. Hand 2015, 10, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Sam, Y.; Park, S.; Kim, C.S. Absence of the Subclavius Muscle with Contralateral Subclavius Posticus Muscle: First Imaging Report. Clin. Imaging 2018, 49, 54–57. [Google Scholar] [CrossRef]
- Asghar, A.; Narayan, R.K.; Satyam, A.; Naaz, S. Prevalence of Anomalous or Ectopic Insertion of Pectoralis Minor: A Systematic Review and Meta-Analysis of 4146 Shoulders. Surg. Radiol. Anat. 2021, 43, 631–643. [Google Scholar] [CrossRef]
- Le Double, A.F. Traité des Variations du Système Musculaire de l’ Homme; Schleicher Frères: Paris, France, 1897. [Google Scholar]
- Homsi, C.; Rodrigues, M.B.; Silva, J.J.; Stump, X.; Morvan, G. Aspect Échographique Des Anomalies d’insertion Du Muscle Pectoralis Minor (Petit Pectoral) [Anomalous Insertion of the Pectoralis Minor Muscle: Ultrasound Findings]. J. Radiol. 2003, 84, 1007–1011. (In French) [Google Scholar] [PubMed]
- Dumontier, C.; Sautet, A.; Gagey, O.; Apoil, A. Rotator Interval Lesions and Their Relation to Coracoid Impingement Syndrome. J. Shoulder Elb. Surg. 1999, 8, 130–135. [Google Scholar] [CrossRef]
- Lee, S.J.; Ha, D.H.; Lee, S.M. Unusual Variation of the Rotator Interval: Insertional Abnormality of the Pectoralis Minor Tendon and Absence of the Coracohumeral Ligament. Skelet. Radiol. 2010, 39, 1205–1209. [Google Scholar] [CrossRef]
- Lee, C.B.; Choi, S.J.; Ahn, J.H.; Ryu, D.S.; Park, M.S.; Jung, S.M.; Shin, D.R. Ectopic Insertion of the Pectoralis Minor Tendon: Inter-Reader Agreement and Findings in the Rotator Interval on MRI. Korean J. Radiol. 2014, 15, 764–770. [Google Scholar] [CrossRef] [PubMed]
- Leonhard, V.; Smith, R.; Caldwell, G.; Smith, H.F. Anatomical Variations in the Brachial Plexus Roots: Implications for Diagnosis of Neurogenic Thoracic Outlet Syndrome. Ann. Anat. 2016, 206, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Leonhard, V.; Caldwell, G.; Goh, M.; Reeder, S.; Smith, H.F. Ultrasonographic Diagnosis of Thoracic Outlet Syndrome Secondary to Brachial Plexus Piercing Variation. Diagnostics 2017, 7, 40. [Google Scholar] [CrossRef]
- Roos, D.B. Congenital Anomalies Associated with Thoracic Outlet Syndrome. Anatomy, Symptoms, Diagnosis, and Treatment. Am. J. Surg. 1976, 132, 771–778. [Google Scholar] [CrossRef]
- Tokat, A.O.; Atınkaya, C.; Fırat, A.; Apaydın, N.; Tekdemir, İ.; Güngör, A. Cadaver analysis of thoracic outlet anomalies. Turk. J. Thorac. Cardiovasc. Surg. 2011, 19, 72–76. [Google Scholar]
- Chavhan, G.B.; Batmanabane, V.; Muthusami, P.; Towbin, A.J.; Borschel, G.H. MRI of Thoracic Outlet Syndrome in Children. Pediatr. Radiol. 2017, 47, 1222–1234. [Google Scholar] [CrossRef] [PubMed]
- Baltopoulos, P.; Tsintzos, C.; Prionas, G.; Tsironi, M. Exercise-Induced Scalenus Syndrome. Am. J. Sports Med. 2008, 36, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Bortolani, E.; Miani, S.; D’Armini, A.; Gallo, E.; Morbidelli, A. Role of Anterior Scalene Muscle Hypertrophy in Thoracic Outlet Syndrome. Minerva Chir. 1989, 44, 1305–1309. [Google Scholar]
- Qaja, E.; Honari, S.; Rhee, R. Arterial Thoracic Outlet Syndrome Secondary to Hypertrophy of the Anterior Scalene Muscle. J. Surg. Case Rep. 2017, 2017, rjx158. [Google Scholar] [CrossRef][Green Version]
- Farina, R.; Foti, P.V.; Iannace, F.A.; Conti, A.; Ferlito, A.; Conti, A.; Pennisi, M.; Santonocito, S.; Basile, A. Thoracic Outlet Syndrome: A Rare Case with Bilateral Cervical Ribs and Bilateral Anterior Scalene Hypertrophy. J. Ultrasound 2021, 24, 331–336. [Google Scholar] [CrossRef]
- Telford, E.D.; Mottershead, S. Pressure at the Cervico-Brachial Junction; an Operative and Anatomical Study. J. Bone Jt. Surg. Br. 1948, 30B, 249–265. [Google Scholar] [CrossRef]
- Aziz, S.; Straehley, C.J.; Whelan, T.J. Effort-Related Axillosubclavian Vein Thrombosis. A New Theory of Pathogenesis and a Plea for Direct Surgical Intervention. Am. J. Surg. 1986, 152, 57–61. [Google Scholar] [CrossRef]
- Kunkel, J.M.; Machleder, H.I. Treatment of Paget-Schroetter Syndrome. A Staged, Multidisciplinary Approach. Arch. Surg. 1989, 124, 1153–1158. [Google Scholar] [CrossRef] [PubMed]
- Hackenberg Booksellers ABAA. Medico-Surgical Tributes to Harold Brunn; a Series of Essays on Various Aspects of Surgery and Medicine Written by His Pupils and Friends; University of California Press: Berkeley, CA, USA, 1942; Available online: https://www.abebooks.com/Medico-surgical-Tributes-Harold-Brunn-Series-Essays/49473238/bd (accessed on 13 December 2022).
- Yin, J.; Qi, Z.; Chen, Y.; Chen, Y. A Case Report of Membranous Occlusion of the Subclavian Vein: A Rare Cause of McCleery Syndrome. Ann. Transl. Med. 2021, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Wiley, A.P.; Freischlag, J.A. Delay in Diagnosis for Two Patients with McCleery Syndrome. Vasc. Endovasc. Surg. 2023, 57, 501–503. [Google Scholar] [CrossRef]
- Garraud, T.; Pomares, G.; Daley, P.; Menu, P.; Dauty, M.; Fouasson-Chailloux, A. Thoracic Outlet Syndrome in Sport: A Systematic Review. Front. Physiol. 2022, 13, 1189. [Google Scholar] [CrossRef]
- Chandra, V.; Little, C.; Lee, J.T. Thoracic Outlet Syndrome in High-Performance Athletes. J. Vasc. Surg. 2014, 60, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Beteck, B.; Shutze, W.; Richardson, B.; Shutze, R.; Tran, K.; Dao, A.; Ogola, G.O.; Pearl, G. Comparison of Athletes and Nonathletes Undergoing Thoracic Outlet Decompression for Neurogenic Thoracic Outlet Syndrome. Ann. Vasc. Surg. 2019, 54, 269–275. [Google Scholar] [CrossRef]
- Sancho-González, I.; Bonilla-Hernández, M.V.; Ibañez-Muñoz, D.; Vicente-Campos, D.; Chicharro, J.L. Upper Extremity Deep Vein Thrombosis in a Triathlete: Again Intense Endurance Exercise as a Thrombogenic Risk. Am. J. Emerg. Med. 2017, 35, 808.e1–808.e3. [Google Scholar] [CrossRef]
- Lutter, C.; Monasterio, E.; Schöffl, V. Rock Climbing-Related Subclavian Vein Thrombosis. Case Rep. 2015, 2015, bcr2015212021. [Google Scholar] [CrossRef] [PubMed]
- Leung, Y.F.; Chung, O.M.; Ip, P.S.; Wong, A.; Wai, Y.L. An Unusual Case of Thoracic Outlet Syndrome Associated with Long Distance Running. Br. J. Sports Med. 1999, 33, 279–281. [Google Scholar] [CrossRef] [PubMed]
- Ijaopo, R.; Oguntolu, V.; Da Costa, D.; Garnham, A.; Hobbs, S. A Case of Paget-Schroetter Syndrome (PSS) in a Young Judo Tutor: A Case Report. J. Med. Case Rep. 2016, 10, 63. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Smith, T.M.; Sawyer, S.F.; Sizer, P.S.; Brismée, J.M. The Double Crush Syndrome: A Common Occurrence in Cyclists with Ulnar Nerve Neuropathy—A Case-Control Study. Clin. J. Sport. Med. 2008, 18, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Zakaria, A.; Gill, J.; Nishi, L.M.; Nadwodny, J.; Pujalte, G.G.A. Soccer Player with Unusual Right Shoulder and Arm Pain and Swelling. J. Prim. Health Care 2020, 12, 181–183. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.J.; Lee, H.J.; Gong, H.S.; Rhee, S.H.; Park, S.J.; Baek, G.H. The Radiologic Relationship of the Shoulder Girdle to the Thorax as an Aid in Diagnosing Neurogenic Thoracic Outlet Syndrome. J. Hand Surg. 2012, 37, 1187–1193. [Google Scholar] [CrossRef]
- Hudson, N.; Starr, M.R.; Esdaile, J.M.; Fitzcharles, M.A. Diagnostic Associations with Hypermobility in Rheumatology Patients. Br. J. Rheumatol. 1995, 34, 1157–1161. [Google Scholar] [CrossRef]
- Levine, N.A.; Rigby, B.R. Thoracic Outlet Syndrome: Biomechanical and Exercise Considerations. Healthcare 2018, 6, 68. [Google Scholar] [CrossRef]
- Atasoy, E. Thoracic Outlet Compression Syndrome. Orthop. Clin. N. Am. 1996, 27, 265–303. [Google Scholar] [CrossRef]
- Cheng, S.W.K.; Stoney, R.J. Supraclavicular Reoperation for Neurogenic Thoracic Outlet Syndrome. J. Vasc. Surg. 1994, 19, 565–572. [Google Scholar] [CrossRef]
- Sanders, R.J.; Haug, C.E.; Pearce, W.H. Recurrent Thoracic Outlet Syndrome. J. Vasc. Surg. 1990, 12, 390–400. [Google Scholar] [CrossRef] [PubMed]
- Demaree, C.J.; Wang, K.; Lin, P.H. Thoracic Outlet Syndrome Affecting High-Performance Musicians Playing Bowed String Instruments. Vascular 2017, 25, 329–332. [Google Scholar] [CrossRef]
- Franklin, G.M. Work-Related Neurogenic Thoracic Outlet Syndrome: Diagnosis and Treatment. Phys. Med. Rehabil. Clin. N. Am. 2015, 26, 551–561. [Google Scholar] [CrossRef]
- Pascarelli, E.F.; Hsu, Y.P. Understanding Work-Related Upper Extremity Disorders: Clinical Findings in 485 Computer Users, Musicians, and Others. J. Occup. Rehabil. 2001, 11, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Sällström, J.; Schmidt, H. Cervicobrachial Disorders in Certain Occupations, with Special Reference to Compression in the Thoracic Outlet. Am. J. Ind. Med. 1984, 6, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, M.; Wegman, D.H. Prevalence Rates and Odds Ratios of Shoulder-Neck Diseases in Different Occupational Groups. Br. J. Ind. Med. 1987, 44, 602. [Google Scholar] [CrossRef]
- Trenor, C.C.; Fisher, J.G.; Khan, F.A.; Sparks, E.A.; Duzan, J.; Harney, K.; Dillon, B.; Menard, M.; Modi, B.P. Paget-Schroetter Syndrome in 21 Children: Outcomes after Multidisciplinary Care. J. Pediatr. 2015, 166, 1493–1497. [Google Scholar] [CrossRef]
- Dintaman, J.; Watson, C.; Fox, C.J.; Hoover, N.; Roberts, S.; Gillespie, D.L. Case of Adolescent with Paget-Schroetter Syndrome and Underlying Thrombophilia Due to an Elevated Lipoprotein (A). Pediatr. Blood Cancer 2007, 49, 1036–1038. [Google Scholar] [CrossRef]
- Conard, J.; Horellou, M.H.; Van Dreden, P.; Lecompte, T.; Samama, M. Thrombosis and Pregnancy in Congenital Deficiencies in AT III, Protein C or Protein S: Study of 78 Women. Thromb. Haemost. 1990, 63, 319–320. [Google Scholar] [CrossRef]
- Sayinalp, N.; Özcebe, O.I.; Kirazli, Ş.; Doǧan, R.; Dündar, S.V.; Gürgey, A. Paget-Schroetter Syndrome Associated with FV:Q506 and Prothrombin 20210A—A Case Report. Angiology 1999, 50, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Adekoya, O. A Case of Upper Limb Venous Thrombosis in Paget-Schroetter Syndrome. Cureus 2021, 13, e13187. [Google Scholar] [CrossRef] [PubMed]
- Tchaikovski, S.N.; Rosing, J. Mechanisms of Estrogen-Induced Venous Thromboembolism. Thromb. Res. 2010, 126, 5–11. [Google Scholar] [CrossRef]
- Curry, P.; Fitchett, D.; Stubbs, W. The Pill and the Thoracic Outlet and Bilateral Carpal Tunnel Syndromes. J. Natl. Med. Assoc. 1981, 73, 995. [Google Scholar]
- Cramer, A.C.M.; McLean, A.W.; Ahari, J. Upper Extremity Deep Venous Thrombosis and Pulmonary Embolus after Ovarian Hyperstimulation. Case Rep. 2016, 2016, bcr2016216719. [Google Scholar] [CrossRef]
- Alderman, D.B.; Kwass, W. Vascular Complications of Cervical Rib. Conn. Med. 1978, 42, 156–158. [Google Scholar] [PubMed]
- Kommareddy, A.; Zaroukian, M.H.; Hassouna, H.I. Upper Extremity Deep Venous Thrombosis. Semin. Thromb. Hemost. 2002, 28, 89–99. [Google Scholar] [CrossRef]
- Stricker, S.J.; Sowers, D.K.; Sowers, J.R.; Sirridge, M.S. “Effort Thrombosis” of the Subclavian Vein Associated with Oral Contraceptives. Ann. Emerg. Med. 1981, 10, 596–599. [Google Scholar] [CrossRef] [PubMed]
- Valanejad, S.M.; Davis, K.A. Direct Oral Anticoagulants in Select Patients with Hypercoagulable Disorders. Ann. Pharmacother. 2021, 55, 891–901. [Google Scholar] [CrossRef] [PubMed]
- Ellison, D.W.; Wood, V.E. Trauma-Related Thoracic Outlet Syndrome. J. Hand Surg. Br. 1994, 19, 424–426. [Google Scholar] [CrossRef]
- Schwartzman, R.J. Brachial Plexus Traction Injuries. Hand Clin. 1991, 7, 547–556. Available online: https://pubmed.ncbi.nlm.nih.gov/1658012/ (accessed on 28 December 2022). [CrossRef] [PubMed]
- Ide, M.; Ide, J.; Yamaga, M.; Takagi, K. Symptoms and Signs of Irritation of the Brachial Plexus in Whiplash Injuries. J. Bone Jt. Surg. Br. 2001, 83, 226–229. [Google Scholar] [CrossRef]
- Sanders, R.J.; Jackson, C.G.R.; Banchero, N.; Pearce, W.H. Scalene Muscle Abnormalities in Traumatic Thoracic Outlet Syndrome. Am. J. Surg. 1990, 159, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Kai, Y.; Oyama, M.; Kurose, S.; Inadome, T.; Oketani, Y.; Masuda, Y. Neurogenic Thoracic Outlet Syndrome in Whiplash Injury. J. Spinal Disord. 2001, 14, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Crotti, F.M.; Carai, A.; Carai, M.; Sgaramella, E.; Sias, W. Post-Traumatic Thoracic Outlet Syndrome (TOS). Acta Neurochir. Suppl. 2005, 92, 13–15. [Google Scholar] [CrossRef]
- Alexandre, A.; Corò, L.; Azuelos, A.; Pellone, M. Thoracic Outlet Syndrome Due to Hyperextension-Hyperflexion Cervical Injury. Acta Neurochir. Suppl. 2005, 92, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Mailis, A.; Papagapiou, M.; Vanderlinden, R.G.; Campbell, V.; Taylor, A. Thoracic Outlet Syndrome after Motor Vehicle Accidents in a Canadian Pain Clinic Population. Clin. J. Pain. 1995, 11, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Dubuisson, A.; Lamotte, C.; Foidart-Dessalle, M.; Nguyen Khac, M.; Racaru, T.; Scholtes, F.; Kaschten, B.; Lénelle, J.; Martin, D. Post-Traumatic Thoracic Outlet Syndrome. Acta Neurochir. 2012, 154, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Mulder, S.; Greenwood, F.A.; Brooks, C.E. Posttraumatic Thoracic Outlet Syndrome. J. Trauma Inj. Infect. Crit. Care 1973, 13, 706–715. [Google Scholar] [CrossRef] [PubMed]
- Casbas, L.; Chauffour, X.; Cau, J.; Bossavy, J.P.; Midy, D.; Baste, J.C.; Barret, A. Post-Traumatic Thoracic Outlet Syndromes. Ann. Vasc. Surg. 2005, 19, 25–28. [Google Scholar] [CrossRef]
- Woods, W.W.; Diego, S. Thoracic Outlet Syndrome. West. J. Med. 1978, 128, 9. [Google Scholar] [PubMed]
- Weinberg, H.; Nathan, H.; Magora, F.; Robin, G.C.; Aviad, I. Arthritis of the First Costovertebral Joint as a Cause of Thoracic Outlet Syndrome. Clin. Orthop. Relat. Res. 1972, 86, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, J.H.; Nguyen, E.T.; Boachie-Adjei, K.; Gribbin, C.; Lee, S.K.; Daluiski, A.; Wolfe, S.W. The Electrodiagnostic Natural History of Parsonage-Turner Syndrome. Muscle Nerve 2017, 56, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Seror, P. Neuralgic Amyotrophy. An Update. Jt. Bone Spine 2017, 84, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.Z.; Likes, K.; Davis, K.; Demos, J.; Freischlag, J.A. The Significance of Cervical Ribs in Thoracic Outlet Syndrome. J. Vasc. Surg. 2013, 57, 771–775. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.H.; Zager, E.L.; McGillicuddy, J.E.; Benzel, E.C.; Adelson, P.D.; Kline, D.G. Thoracic Outlet Syndrome. Neurosurgery 2004, 55, 897–903. [Google Scholar] [CrossRef]
- Kuhn, J.E.; Lebus, V.G.F.; Bible, J.E. Thoracic Outlet Syndrome. J. Am. Acad. Orthop. Surg. 2015, 23, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Burt, B.M. Thoracic Outlet Syndrome for Thoracic Surgeons. J. Thorac. Cardiovasc. Surg. 2018, 156, 1318–1323.e1. [Google Scholar] [CrossRef] [PubMed]
- Goeteyn, J.; Pesser, N.; Houterman, S.; van Sambeek, M.R.H.M.; van Nuenen, B.F.L.; Teijink, J.A.W. Surgery Versus Continued Conservative Treatment for Neurogenic Thoracic Outlet Syndrome: The First Randomised Clinical Trial (STOPNTOS Trial). Eur. J. Vasc. Endovasc. Surg. 2022, 64, 119–127. [Google Scholar] [CrossRef]
- Lindgren, K.A. Conservative Treatment of Thoracic Outlet Syndrome: A 2-Year Follow-Up. Arch. Phys. Med. Rehabil. 1997, 78, 373–378. [Google Scholar] [CrossRef]
- Warrick, A.; Davis, B. Neurogenic Thoracic Outlet Syndrome in Athletes—Nonsurgical Treatment Options. Curr. Sports Med. Rep. 2021, 20, 319–326. [Google Scholar] [CrossRef] [PubMed]
| Space | Borders | Contents |
|---|---|---|
| Scalene triangle | Anterior: Scalenus anterior Posterior: Scalenus middle Inferior: 1st rib | Brachial plexus (trunks) Subclavian artery |
| Costoclavicular space | Anterior: Clavicle (or subclavicular muscle) Posterolateral: Upper board of the scapula Posteromedial: 1st rib | Brachial plexus (division) Subclavian vessels |
| Subcoracoid space | Anterior: Pectoralis minor muscle Superior: Coracoid process of the scapula Posterior: 2nd–4th ribs | Brachial plexus (cords) Axillary vessels |
| Type | CR Type Description |
|---|---|
| I | CR extends to the transverse process of the 7th cervical vertebrae |
| II | CR extends beyond TPs with no connection to FR |
| III | CR extends beyond TP with partial fusion to FR by fibrous bands or cartilage |
| IV | CR is fully fused to FR |
| Type | Type Description (in Relation to Coracoid Process) |
|---|---|
| I | Only the tendon of PM crosses above CP |
| II | Tendon of PM crosses above CP, and much of the muscle mass runs under CP |
| III | The whole PM runs above CP |
| Type 1 A band from the anterior apex of an incomplete CR to the middle of the upper surface (posterior to scalene tubercle) of the FR. Type 2 A strip originated at elongated C7 that attached to the FR in the same place as a type 1 Type 3 A band that had origin near the neck of FR and insertion behind the scalene tubercle Type 4 A band lies along the anterior edge of SM, which has an origin on the transverse process and is inserted into the FR with SM Type 5 The scalene minimus muscle (SMM)—described in more detail later in this paper Type 6 SMM inserts into Sibson’s fascia (not to the FR) above the cupola of the pleura Type 7 A fibrous strand running in front of AS, down to FR, and inserts to the sternum or costochondral junction (CJ). Due to the close relation to the subclavian vein (right behind it), it may cause her obstruction. Type 8 A strip arising from MS passes below the subclavian vessels (vein and artery) to insert into CJ Type 9 The network filling the inner, posterior arch of the FR, consisting of muscles and their fascias Type 10 AS-derived muscle fibers attaching to the brachial bundle (perinerium) Type 11 Muscle fibers that form bands that connect the AS and AM and run between the cords of BP Type 12 An anomalous AS (inferior part) runs posterior to the C5 and C6 roots Type 13 n band consisting of fused scalene muscles Type 14 Fibrous bands run vertically, behind the AS, and anteriorly to the roots of BP |
| Congenital Risk Factors | Acquired Risk Factors | Trauma-Related Risk Factors |
|---|---|---|
| Cervical rib [22] Pseudoarthrosis of the clavicle [38] First rib variation (increased width, congenital malformation) [30] Ectopic insertion of pectoralis minor [62] Morphological variations of scalene muscles (AS, MS, SMM) [45,50] Subclavius posticous muscle presence [58] Brachial plexus variation (piercing AS and/or MS) [67] Superior pleural sinus presence [26] Congenital ligaments and bands [69] Elongated transverse process of C7 [27] | Hypertrophy of the AS, MS, and subclavius muscle [1,72,76] Repetitive overhead shoulder movements [82] Sports associated with risk of TOS (baseball, swimming, water polo, judo, climbing) [82,83] Lower position of the shoulder girdle [91] Hypermobility of the shoulder joint [92] Occupations with overhead movements or sedentary work patterns (e.g., computer users or musicians) [98,99,100] | Whiplash injury car/motorcycle accident [115] Arthritis of the first costovertebral joint and hydrocortisone injection into the costovertebral joint [126] Neuritis of the brachial plexus [127] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maślanka, K.; Zielinska, N.; Karauda, P.; Balcerzak, A.; Georgiev, G.; Borowski, A.; Drobniewski, M.; Olewnik, Ł. Congenital, Acquired, and Trauma-Related Risk Factors for Thoracic Outlet Syndrome—Review of the Literature. J. Clin. Med. 2023, 12, 6811. https://doi.org/10.3390/jcm12216811
Maślanka K, Zielinska N, Karauda P, Balcerzak A, Georgiev G, Borowski A, Drobniewski M, Olewnik Ł. Congenital, Acquired, and Trauma-Related Risk Factors for Thoracic Outlet Syndrome—Review of the Literature. Journal of Clinical Medicine. 2023; 12(21):6811. https://doi.org/10.3390/jcm12216811
Chicago/Turabian StyleMaślanka, Krystian, Nicol Zielinska, Piotr Karauda, Adrian Balcerzak, Georgi Georgiev, Andrzej Borowski, Marek Drobniewski, and Łukasz Olewnik. 2023. "Congenital, Acquired, and Trauma-Related Risk Factors for Thoracic Outlet Syndrome—Review of the Literature" Journal of Clinical Medicine 12, no. 21: 6811. https://doi.org/10.3390/jcm12216811
APA StyleMaślanka, K., Zielinska, N., Karauda, P., Balcerzak, A., Georgiev, G., Borowski, A., Drobniewski, M., & Olewnik, Ł. (2023). Congenital, Acquired, and Trauma-Related Risk Factors for Thoracic Outlet Syndrome—Review of the Literature. Journal of Clinical Medicine, 12(21), 6811. https://doi.org/10.3390/jcm12216811





