Comparison of Early versus Traditional Rehabilitation Protocol after Rotator Cuff Repair: An Umbrella-Review
Abstract
:1. Introduction
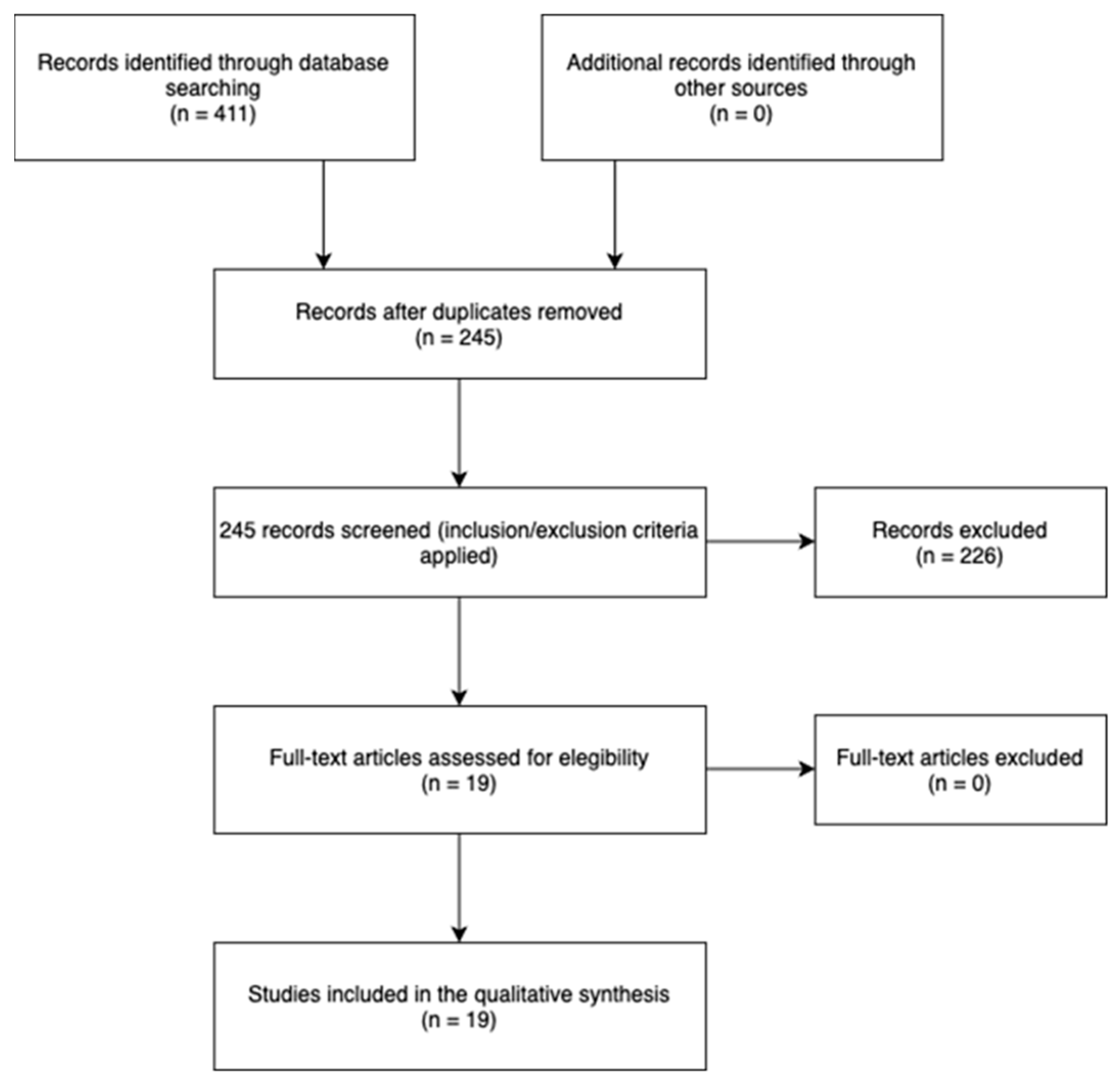
2. Materials and Methods
2.1. Eligibility Criteria
- Population: patients with rotator cuff tear undergoing surgical repair, over 18 years old;
- Intervention: early rehabilitation protocol;
- Comparison: standard/delayed rehabilitation protocol;
- Primary outcome: pain;
- Secondary outcome: function (range of motion, strength) and risk of retear.
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
2.1.3. Information Sources and Search Strategy
2.1.4. Selection Strategy
2.1.5. Methodological Quality
3. Results
4. Discussion
4.1. Pain
4.2. Functional Recovery
4.3. Risk of Retear
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Littlewood, C.; May, S.; Walters, S. Epidemiology of Rotator Cuff Tendinopathy: A Systematic Review. Shoulder Elb. 2013, 5, 256–265. [Google Scholar] [CrossRef]
- Consigliere, P.; Haddo, O.; Levy, O.; Sforza, G. Subacromial impingement syndrome: Management challenges. Orthop. Res. Rev. 2018, 10, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Keener, J.D.; Patterson, B.M.; Orvets, N.; Chamberlain, A.M. Degenerative rotator cuff tears: Refining surgical indications based on natural history data. J. Am. Acad. Orthop. Surg. 2019, 27, 156–165. [Google Scholar] [CrossRef]
- Yazdani, A.N.; Rai, V.; Agrawal, D.K. Rotator Cuff Health, Pathology, and Repair in the Perspective of Hyperlipidemia. J. Orthop. Sport. Med. 2022, 4, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Razmjou, H.; Lincoln, S.; Axelrod, T.; Holtby, R. Factors Contributing to Failure of Rotator Cuff Surgery in Persons with Work-Related Injuries. Physiother. Can. 2008, 60, 125. [Google Scholar] [CrossRef]
- Oh, J.H.; Park, M.S.; Rhee, S.M. Treatment Strategy for Irreparable Rotator Cuff Tears. Clin. Orthop. Surg. 2018, 10, 119–134. [Google Scholar] [CrossRef]
- Tempelhof, S.; Rupp, S.; Seil, R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J. Shoulder Elb. Surg. 1999, 8, 296–299. [Google Scholar] [CrossRef]
- Minagawa, H.; Yamamoto, N.; Abe, H.; Fukuda, M.; Seki, N.; Kikuchi, K.; Kijima, H.; Itoi, E. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J. Orthop. 2013, 10, 8–12. [Google Scholar] [CrossRef]
- Littlewood, C.; Bateman, M.; Butler-Walley, S.; Bathers, S.; Bromley, K.; Lewis, M.; Funk, L.; Denton, J.; Moffatt, M.; Winstanley, R.; et al. Rehabilitation following rotator cuff repair: A multi-centre pilot & feasibility randomised controlled trial (RaCeR). Clin. Rehabil. 2021, 35, 829–839. [Google Scholar] [CrossRef]
- Gartsman, G.M. Arthroscopic management of rotator cuff disease. J. Am. Acad. Orthop. Surg. 1998, 6, 259–266. [Google Scholar] [CrossRef]
- Ensor, K.L.; Kwon, Y.W.; Dibeneditto, M.R.; Zuckerman, J.D.; Rokito, A.S. The rising incidence of rotator cuff repairs. J. Shoulder Elb. Surg. 2013, 22, 1628–1632. [Google Scholar] [CrossRef]
- Mazuquin, B.; Moffatt, M.; Gill, P.; Selfe, J.; Rees, J.; Drew, S.; Littlewood, C. Effectiveness of early versus delayed rehabilitation following rotator cuff repair: Systematic review and meta-analyses. PLoS ONE 2021, 16, e0252137. [Google Scholar] [CrossRef]
- Jain, N.B.; Higgins, L.D.; Losina, E.; Collins, J.; Blazar, P.E.; Katz, J.N. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet. Disord. 2014, 15, 4. [Google Scholar] [CrossRef]
- Littlewood, C.; Mazuquin, B.; Moffatt, M.; Bateman, M. Rehabilitation following rotator cuff repair: A survey of current practice. Musculoskelet. Care 2021, 19, 165–171. [Google Scholar] [CrossRef]
- Cho, C.-H.; Song, K.-S.; Jung, G.H.; Lee, Y.K.; Shin, H.K. Early postoperative outcomes between arthroscopic and mini-open repair for rotator cuff tears. Orthopedics 2012, 35, 1347–1352. [Google Scholar] [CrossRef]
- Nazari, G.; MacDermid, J.C.; Bryant, D.; Dewan, N.; Athwal, G.S. Effects of arthroscopic vs. mini-open rotator cuff repair on function, pain & range of motion. A systematic review and meta-analysis. PLoS ONE 2019, 14, e0222953. [Google Scholar] [CrossRef]
- Cole, B.J.; McCarty, L.P.; Kang, R.W.; Alford, W.; Lewis, P.B.; Hayden, J.K. Arthroscopic rotator cuff repair: Prospective functional outcome and repair integrity at minimum 2-year follow-up. J. Shoulder Elb. Surg. 2007, 16, 579–585. [Google Scholar] [CrossRef]
- DeFranco, M.J.; Bershadsky, B.; Ciccone, J.; Yum, J.K.; Iannotti, J.P. Functional outcome of arthroscopic rotator cuff repairs: A correlation of anatomic and clinical results. J. Shoulder Elb. Surg. 2007, 16, 759–765. [Google Scholar] [CrossRef]
- Iannotti, J.P.; Deutsch, A.; Green, A.; Rudicel, S.; Christensen, J.; Marraffino, S.; Rodeo, S. Time to failure after rotator cuff repair: A prospective imaging study. J. Bone Jt. Surg. Am. 2013, 95, 965–971. [Google Scholar] [CrossRef]
- Zhao, J.; Luo, M.; Pan, J.; Liang, G.; Feng, W.; Zeng, L.; Yang, W.; Liu, J. Risk factors affecting rotator cuff retear after arthroscopic repair: A meta-analysis and systematic review. J. Shoulder Elb. Surg. 2021, 30, 2660–2670. [Google Scholar] [CrossRef]
- Cuff, D.J.; Pupello, D.R. Prospective randomized study of arthroscopic rotator cuff repair using an early versus delayed postoperative physical therapy protocol. J. Shoulder Elb. Surg. 2012, 21, 1450–1455. [Google Scholar] [CrossRef]
- Düzgün, I.; Baltacı, G.; Atay, O.A. Comparison of slow and accelerated rehabilitation protocol after arthroscopic rotator cuff repair: Pain and functional activity. Acta Orthop. Traumatol. Turc. 2011, 45, 23–33. [Google Scholar] [CrossRef]
- Arndt, J.; Clavert, P.; Mielcarek, P.; Bouchaib, J.; Meyer, N.; Kempf, J.F. French Society for Shoulder & Elbow (SOFEC). Immediate passive motion versus immobilization after endoscopic supraspinatus tendon repair: A prospective randomized study. Orthop. Traumatol. Surg. Res. 2012, 98, S131–S138. [Google Scholar] [CrossRef]
- Peltzm, C.D.; Sarver, J.J.; Dourte, L.M.; Würgler-Hauri, C.C.; Williams, G.R.; Soslowsky, L.J. Exercise following a short immobilization period is detrimental to tendon properties and joint mechanics in a rat rotator cuff injury model. J. Orthop. Res. 2010, 28, 841–845. [Google Scholar] [CrossRef]
- Huberty, D.P.; Schoolfield, J.D.; Brady, P.C.; Vadala, A.P.; Arrigoni, P.; Burkhart, S.S. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy 2009, 25, 880–890. [Google Scholar] [CrossRef]
- Papalia, R.; Franceschi, F.; Vasta, S.; Gallo, A.; Maffulli, N.; Denaro, V. Shoulder stiffness and rotator cuff repair. Br. Med. Bull. 2012, 104, 163–174. [Google Scholar] [CrossRef]
- Chen, L.; Peng, K.; Zhang, D.; Peng, J.; Xing, F.; Xiang, Z. Rehabilitation protocol after arthroscopic rotator cuff repair: Early versus delayed motion. Int. J. Clin. Exp. Med. 2015, 8, 8329–8338. [Google Scholar]
- Namdari, S.; Green, A. Range of motion limitation after rotator cuff repair. J. Shoulder Elb. Surg. 2010, 19, 290–296. [Google Scholar] [CrossRef]
- Pollock, M.; Fernandes, R.M.; Pieper, D.; Tricco, A.C.; Gates, M.; Gates, A.; Hartling, L. Preferred Reporting Items for Overviews of Reviews (PRIOR): A protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst. Rev. 2019, 8, 335. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, 4008. [Google Scholar] [CrossRef]
- Bandara, U.; An, V.V.G.; Imani, S.; Nandapalan, H.; Sivakumar, B.S. Rehabilitation protocols following rotator cuff repair: A meta-analysis of current evidence. ANZ J. Surg. 2021, 91, 2773–2779. [Google Scholar] [CrossRef]
- Houck, D.A.; Kraeutler, M.J.; Schuette, H.B.; McCarty, E.C.; Bravman, J.T. Early Versus Delayed Motion after Rotator Cuff Repair: A Systematic Review of Overlapping Meta-analyses. Am. J. Sport. Med. 2017, 45, 2911–2915. [Google Scholar] [CrossRef]
- Li, S.; Sun, H.; Luo, X.; Wang, K.; Wu, G.; Zhou, J.; Wang, P.; Sun, X. The clinical effect of rehabilitation following arthroscopic rotator cuff repair: A meta-analysis of early versus delayed passive motion. Medicine 2018, 97, e9625. [Google Scholar] [CrossRef] [PubMed]
- Littlewood, C.; Bateman, M.; Clark, D.; Selfe, J.; Watkinson, D.; Walton, M.; Funk, L. Rehabilitation following rotator cuff repair: A systematic review. Shoulder Elb. 2015, 7, 115–124. [Google Scholar] [CrossRef]
- Longo, U.G.; Risi Ambrogioni, L.; Berton, A.; Candela, V.; Migliorini, F.; Carnevale, A.; Schena, E.; Nazarian, A.; DeAngelis, J.; Denaro, V. Conservative versus accelerated rehabilitation after rotator cuff repair: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2021, 22, 637. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Carnevale, A.; Piergentili, I.; Berton, A.; Candela, V.; Schena, E.; Denaro, V. Retear rates after rotator cuff surgery: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2021, 22, 749. [Google Scholar] [CrossRef] [PubMed]
- Matlak, S.; Andrews, A.; Looney, A.; Tepper, K.B. Postoperative Rehabilitation of Rotator Cuff Repair: A Systematic Review. Sports Med. Arthrosc. Rev. 2021, 29, 119–129. [Google Scholar] [CrossRef]
- Saltzman, B.M.; Zuke, W.A.; Go, B.; Mascarenhas, R.; Verma, N.N.; Cole, B.J.; Romeo, A.A.; Forsythe, B. Does early motion lead to a higher failure rate or better outcomes after arthroscopic rotator cuff repair? A systematic review of overlapping meta-analyses. J. Shoulder Elb. Surg. 2017, 26, 1681–1691. [Google Scholar] [CrossRef]
- Silveira, A.; Luk, J.; Tan, M.; Kang, S.H.; Sheps, D.M.; Bouliane, M.; Beaupre, L. Move It or Lose It? The Effect of Early Active Movement on Clinical Outcomes Following Rotator Cuff Repair: A Systematic Review with Meta-analysis. J. Orthop. Sport. Phys. Ther. 2021, 51, 331–344. [Google Scholar] [CrossRef]
- Thomson, S.; Jukes, C.; Lewis, J.S. Rehabilitation following surgical repair of the rotator cuff: A systematic review. Physiotherapy 2016, 102, 20–28. [Google Scholar] [CrossRef]
- Gallagher, B.P.; Bishop, M.E.; Tjoumakaris, F.P.; Freedman, K.B. Early versus delayed rehabilitation following arthroscopic rotator cuff repair: A systematic review. Phys. Sport. 2015, 43, 178–187. [Google Scholar] [CrossRef]
- Chang, K.V.; Hung, C.Y.; Han, D.S.; Chen, W.S.; Wang, T.G.; Chien, K.L. Early versus delayed passive range of motion exercise for arthroscopic rotator cuff repair: A meta-analysis of randomized controlled trials. Am. J. Sport. Med. 2015, 43, 1265–1273. [Google Scholar] [CrossRef]
- Chan, K.; MacDermid, J.C.; Hoppe, D.J.; Ayeni, O.R.; Bhandari, M.; Foote, C.J.; Athwal, G.S. Delayed versus early motion after arthroscopic rotator cuff repair: A meta-analysis. J. Shoulder Elb. Surg. 2014, 23, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.; Tang, Z.H.; Hu, J.Z.; Zou, G.Y.; Xiao, R.C.; Yan, D.X. Does immobilization after arthroscopic rotator cuff repair increase tendon healing? A systematic review and meta-analysis. Arch. Orthop. Trauma Surg. 2014, 134, 1279–1285. [Google Scholar] [CrossRef]
- Huang, T.S.; Wang, S.F.; Lin, J.-J. Comparison of Aggressive and Traditional Postoperative Rehabilitation Protocol after Rotator Cuff Repair: A Meta-analysis. J. Nov. Physiother. 2013, 3, 170. [Google Scholar] [CrossRef]
- Riboh, J.C.; Garrigues, G.E. Early passive motion versus immobilization after arthroscopic rotator cuff repair. Arthrosc.-J. Arthrosc. Relat. Surg. 2014, 30, 997–1005. [Google Scholar] [CrossRef]
- Kluczynski, M.A.; Nayyar, S.; Marzo, J.M.; Bisson, L.J. Early Versus Delayed Passive Range of Motion after Rotator Cuff Repair: A Systematic Review and Meta-analysis. Am. J. Sport. Med. 2015, 43, 2057–2063. [Google Scholar] [CrossRef] [PubMed]
- Kluczynski, M.A.; Isenburg, M.M.; Marzo, J.M.; Bisson, L.J. Does Early versus Delayed Active Range of Motion Affect Rotator Cuff Healing after Surgical Repair? Am. J. Sport. Med. 2016, 44, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Brian, M.G.; Jonathan, D.H.; Stephanie, A.B.; Albert, L.; Bryson, P.L. Comparison of Functional Outcomes after Arthroscopic Rotator Cuff Repair between Patients with Traumatic and Atraumatic Tears. Orthop. J. Sport. Med. 2022, 10, 23259671221126551. [Google Scholar] [CrossRef]
- Paul, S.; Yadav, A.K.; Goyal, T. Comparison of tear characteristics, outcome parameters and healing in traumatic and non-traumatic rotator cuff tear: A prospective cohort study. Musculoskelet. Surg. 2022, 106, 433–440. [Google Scholar] [CrossRef] [PubMed]
| Week | Early Protocol | Delayed Protocol |
|---|---|---|
| 0–3 |
|
|
| 4–6 |
|
|
| 6–10 |
|
|
| 10–12 |
|
|
| Authors | q1 | q2 | q3 | q4 | q5 | q6 | q7 | q8 | q9 | q10 | q11 | q12 | q13 | q14 | q15 | q16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bandara et al. [32] (2021) | yes | partial yes | yes | partial yes | yes | yes | no | partial yes | no | no | yes | no | no | yes | no | no |
| Houck et al. [33] (2017) | no | partial yes | yes | partial yes | yes | yes | no | partial yes | no | no | yes | no | yes | yes | no | yes |
| Li et al. [34] (2017) | yes | partial yes | yes | partial yes | yes | yes | Partial Yes | yes | yes | no | yes | yes | yes | yes | yes | yes |
| Littlewood et al. [35] (2014) | yes | partial yes | yes | partial yes | no | no | no | yes | no | yes | no-meta | no-meta | no | no | no-meta | no |
| Longo et al. [36] (2021) | yes | partial yes | yes | partial yes | yes | yes | no | yes | yes | yes | yes | yes | yes | yes | yes | yes |
| Longo et al. [37] (2021) | yes | partial yes | yes | partial yes | yes | yes | no | yes | yes | no | yes | yes | yes | yes | yes | yes |
| Matlak et al. [38] (2021) | no | partial yes | yes | partial yes | yes | yes | no | yes | no | no | no-meta | no-meta | yes | no | no-meta | yes |
| Mazuquin et al. [12] (2021) | yes | partial yes | yes | partial yes | yes | yes | yes | yes | yes | no | yes | yes | yes | yes | yes | yes |
| Saltzman et al. [39] (2017) | no | partial yes | yes | partial yes | yes | yes | no | no | no | yes | no-meta | no-meta | no | yes | no-meta | no |
| Silveira et al. [40] (2021) | yes | partial yes | yes | partial yes | yes | yes | partial yes | yes | yes | yes | yes | yes | yes | yes | yes | no |
| Thomson et al. [41] (2015) | yes | partial yes | yes | yes | yes | yes | partial yes | partial yes | no | no | no-meta | no-meta | no | no | no-meta | yes |
| Gallagher et al. [42] (2015) | yes | yes | yes | yes | no | no | no | yes | yes | no | no meta | no meta | yes | yes | no meta | yes |
| Chang et al. [43] (2014) | yes | yes | yes | yes | yes | yes | partial yes | yes | yes | no | yes | yes | yes | yes | yes | yes |
| Chan et al. [44] (2014) | yes | yes | yes | yes | yes | yes | yes | yes | partial yes | no | yes | yes | no | yes | yes | no |
| Shen et al. [45] (2014) | yes | yes | yes | yes | yes | yes | no | partial yes | yes | no | yes | yes | no | yes | yes | no |
| Huang et al. [46] (2013) | yes | partial yes | yes | yes | yes | no | no | yes | no | no | no | yes | no | yes | no | no |
| Riboh et al. [47] (2014) | yes | yes | yes | yes | yes | yes | no | yes | yes | no | no | yes | yes | yes | yes | yes |
| Kluczynski et al. [48] (2014) | yes | yes | yes | yes | no | no | no | partial yes | no | no | yes | no | no | yes | no | yes |
| Kluczynski et al. [49] (2015) | yes | yes | yes | yes | yes | yes | no | yes | no | no | no | no | no | yes | no | yes |
| Article Type | Population | Evaluation Time | Results | Outcomes and Scales | Conclusions | Limitations | |
|---|---|---|---|---|---|---|---|
| Bandara et al. [32] | Systematic review (6 RCT) | 531 patients Diagnosis: All participants received rotator cuff repair Average age and DS: non specified. M = non specified F = non specified | T0 = first postoperative day T1 = 6 month after rotator cuff repair T2 = 12 month after rotator cuff repair | =ROM EP > Constant-Murley Score (no increased risk of recurrence) | Joints balance = ROM. Function = Constant-Murley Shoulder Score. Structure = Recurrence rate | (1) EP = TP—ROM. (2) EP > risk of recurrence but > functional recovery (3) EP = TP—safe and reproducible results in the short and long term. | 1 Variable design of each individual study. 2 High heterogeneity revealed in pooled analyses. 3 Variability in the description of each rehabilitation protocol and timing 4 Possibility of bias in a number of the included studies |
| Houck et al. [33] | Systematic review (7 RCT) | 5896 patients Diagnosis: All participants received rotator cuff repair Average age: 46–59 years DS: non specified M = non specified F = non specified | T0 = first postoperative day T1 = 6 month after rotator cuff repair T2 = 12 month after rotator cuff repair T3 = 24 month after rotator cuff repair | EP > ROM EP > risk of recurrence TP > Cure rate TP > ASES score EP > small injuries TP > large injuries | joints balance = ROM. Function = ASES score. Structure = Recurrence rate | (1) EP > ROM but >risk of recurrence | 1 lack of reporting follow-up results, age, sex, tear size, and the rotator cuff muscles involved. 2 surgical techniques inconsistently reported in the included studies. 3 risks of bias in the ROM reported due to a lack of blinding. |
| Li et al. [34] (2017) | Systematic review (8 RCT) | 671 patients Diagnosis: All participants received rotator cuff repair Average age: 58.1 ± 3.9 DS M = non specified F = non specified | T0 = first postoperative day T1 = 3 month after rotator cuff repair T2 = 6 month after rotator cuff repair T3 = 12–24 month after rotator cuff repair | EP > ROM =cure rate, ASES at T2, SST, Constant-Murley score TP > ASES at T3 | joints balance = ROM. Function = Constant-Murley Shoulder Score, ASES, SST. Structure = Recurrence rate | (1) EP > ROM but < shoulder functionality (2) EP < cure rate for large injuries | 1 number of trials relatively small 2 no high quality of evidence in all outcomes 3 outcome assessors were not blinded to rehabilitation protocol. 4 the standard deviation is not provided in some included studies. |
| Littlewood et al. [35] (2014) | Systematic review (12 RCT) | 819 patients Diagnosis: All participants received rotator cuff repair Average age: 58.1 DS: non specified M = 430 F = 389 | T0 = first postoperative day T1 = 3 month after rotator cuff repair T2 = 6 month after rotator cuff repair T3 = 12 month after rotator cuff repair | =pain, risk of recurrence and disability | Function = pain, disability Structure = Recurrence rate | (1) EP = TP | 1 small mean number of included participants per trial 2 only one reviewer identified relevant studies, extracted data, and synthesized the findings. |
| Longo et al. [36] (2021) | Systematic review (16 RCT) | 1424 patients Diagnosis: All participants received rotator cuff repair Average age: 56.1 ± 8.7 DS PP56.6 ± 9 DS PT M = 776 F = 648 | T0 = first postoperative day T1 = 3 month after rotator cuff repair T2 = 6 month after rotator cuff repair T3 = 12 month after rotator cuff repair T4 = 24 month after rotator cuff repair | EP > ROM external rotation at T1. EP > ROM T2. =ROM at T4. =risk of recurrence and Constant-Murley score | joints balance = ROM. Function = Constant-Murley Shoulder Score. Structure = Recurrence rate | (1) = recurrence rate between the 2 groups (2) EP > external rotation at 3- and 6-months follow-up, but = at 24 | 1 lack of information on the RC tear characteristics 2 muscle atrophy and fatty infiltration were not specified in most of the included articles. 3 Different early protocols in terms of exercise and timing |
| Longo et al. [37] (2021) | Systematic review (31 RCT) | 5109 patients Diagnosis: All participants received rotator cuff repair Average age: 58.2 years ± 3.7 DS M = 2396. F = 2231 | T0 = first postoperative day T1 = 3 month after rotator cuff repair T2 = 6 month after rotator cuff repair T3 = 12 month after rotator cuff repairT4 = 24 month after rotator cuff repair | =immobilization period =passive ROM EP active ROM > risk of recurrence TP complete active ROM > risk of recurrence =strengthening exercises | Structure = Recurrence rate | (1) = recurrence rate for immobilization, passive ROM, and force exercises. (2) EP active ROM > recurrence rate (3) TP full active ROM > recurrence rate | 1 insufficient number of studies reporting the preoperative tear size. 2 no conclusions regarding clinical outcomes were made. |
| Matlak et al. [38] (2021) | Systematic review (22 RCT) | 1782 patients | T0 = first postoperative day | EP > ROM; | joints balance = ROM; | (1) EP = reduced risk of stiffness, improves ROM and function faster | 1 Lack of high quality studies about subscapularis rehabilitation |
| Diagnosis: All participants received rotator cuff repair | T1 = 6 weeks after rotator cuff repair | EP > Function | Structure = Recurrence rate, rigidity | (2) TP = Reduced risk of recurrence. | |||
| Average age: 45–64.8 years | T2 = 3 month after rotator cuff repair | EP < Rigidity | Structure = strength | (3) CPM can accelerate ROM gain but does not improve long-term results. | 2 Literature gaps about optimal dosage of frequency and intensity of exercise, ideal time to begin loading. | ||
| DS: non specified | T3 = 6 month after rotator cuff repair | TP < risk of recurrence | (4) Early isometric loading may be beneficial for increasing strength and tendon shaping but requires further research | ||||
| M = non specified | EP > strength | ||||||
| F = non specified | |||||||
| Mazuquin et al. [12] (2021) | Systematic review (20 RCT) | 1841 patients | T0 = first postoperative day | =VAS; | joints balance = ROM; | (1) EP > ROM and same tendon integrity | 1 The majority of the RCTs were considered of high or unclear overall risk of bias, had small sample sizes and their definition of early and delayed rehabilitation were not consistent |
| Diagnosis: All participants received rotator cuff repair | T1 = 6 weeks after rotator cuff repair | =ASES, Constant-Murley, SST, WORC; | Function = ASES, Constant-Murley Shoulder Score, SST, WORC; SANE; | 2 subgroup analyses were not possible due to the lack of data reported by tear size | |||
| Average age: 54–65.4 years | T2 = 3 month after rotator cuff repair | EP > SANE Score; | Structure = strength, tendon integrity | ||||
| DS: non specified | T3 = 6 month after rotator cuff repair | =Strength, tendon integrity | |||||
| M = non specified | T4 = 1 year after rotator cuff repair | EP > ROM short term | |||||
| F = non specified | T5 = 2 years after rotator cuff repair | TP > rigidity long term | |||||
| Saltzman et al. [39] (2017) | Systematic review (9 RCT) | 265 −2251 patients | T0 = first postoperative day | =tendon healing, risk of recurrence, functional outcomes, and strength | joints balance = ROM; | (1) EP > ROM | Difficulty in controlling for heterogeneity, small sample sizes and narrow study populations, lack of blinding in individual studies |
| Diagnosis: All participants received rotator cuff repair | T1 = 6 month after rotator cuff repair | EP > ROM; | Function = ASES, Constant-Murley, SST, WORC; | (2) = Functional results and recurrence rate | |||
| Average age: 57.7–60.38 years | T2 = 12 month after rotator cuff repair | EP > risk of recurrence for large injuries | Structure = Recurrence rate and recovery rate | (3) EP > Recurrence rate for large injuries | |||
| DS: non specified | |||||||
| M = non specified | |||||||
| F = non specified | |||||||
| Silveira et al. [40] (2021) | Systematic review (8 RCT) | 756 patients | T0 = first postoperative day | =pain, strength, and integrity | joints balance = ROM; | (1) EP > freedom of movement of the shoulder but worse quality of life; | Different tear size and surgical techniques |
| Diagnosis: All participants received rotator cuff repair | T1 = 6 weeks after rotator cuff repair | TP > WORC Index at T1, | Function = WORC Index, Constant-Murley score; | (2) Differences between groups do not appear to be clinically important | |||
| Average age: 50.43–57.68 years | T2 = 3 month after rotator cuff repair | =in other follow-up times | Structure = strength, tendon integrity | ||||
| DS: non specified | T3 = 6 month after rotator cuff repair | =Constant-Murley score; | |||||
| M = 442; | T4 = 1 year after rotator cuff repair | EP > ROM at T1, = in other follow-up times | |||||
| F = 344. | T5 = 2 years after rotator cuff repair | ||||||
| Thomson et al. [41] (2015) | Systematic review (11 RCT) | 706 patients | T0 = first postoperative day | EP > ROM | joints balance = ROM | (1) EP = TP | 1 Data extracted by only one reviewer 2 Language and publication bias |
| Diagnosis: All participants received rotator cuff repair | T1 = 6 month after rotator cuff repair | TP > large injuries | |||||
| Average age: 58.1 years | T2 = 12 month after rotator cuff repair | ||||||
| DS: non specified | |||||||
| M = non specified | |||||||
| F = non specified | |||||||
| Gallagher et al. [42] (2015) | Systematic review (6 RCT) | 80 patients | T0 = first postoperative day | =risk of recurrence, PAIN | Function: Constant shoulder score, ASES, SST, UCLA, and DASH score | EP better ROM in short term, but =in long term | 1 lack of uniform, prospective trials comparing similar rehabilitation protocols 2 All studies suffered from an intrinsic inability to properly blind individuals and several suffered from inadequate randomization or insufficient incomplete outcome reporting |
| Diagnosis: All participants received rotator cuff repair | T1 = 3 month after rotator cuff repair | EP > ROM at T2, = ROM at T3 | |||||
| Average age: 54.5–63.2 | T2 = 6 month after rotator cuff repair | =stiffness, =healing | |||||
| DS: non specified | T3 = 12 month after rotator cuff repair | =ASES, SST, DASH | |||||
| M = non specified | EP > UCLA at T1, but = at T2 and T3 | ||||||
| F = non specified | |||||||
| Chang et al. [43] (2014) | Systematic review (6 RCT) | 482 patients | T0 = closest day to surgery | =external rotation range | Function = UCLA and Constant | Early ROM exercises improve postoperative stiffness but improper tendon healing in large-sized tears | 1 Small numbers of included trials |
| Diagnosis: All participants received rotator cuff repair | T1 = 6 month after rotator cuff repair | EP > shoulder forward flexion range at T1 and T2 | 2 heterogeneities among the included articles regarding the severity of the rotator cuff tears, surgical techniques, and functional outcome assessment scales | ||||
| Average age: 54.5–63.5 | T2 = 12 month after rotator cuff repair | EP > recurrency | Structure = recurrence rate | 3 not all the included trials reported | |||
| DS: non specified | EP = reduce stiffness | reoperation rate | |||||
| M = 233 | |||||||
| F = 249 | |||||||
| Chan et al. [44] (2014) | Systematic review (4 RCT) | 370 patients | T0 = closest day to surgery | =ASES (4 RCT), CMS (2 RCT), SST, WORC | Function = ASES, Constant, SST, WORC, DASH | No statistically significant differences in functional outcomes scores, relative risks of recurrent rotator cuff tears | 1 Unavailable data for several studies included in the review. |
| Diagnosis: All participants received rotator cuff repair | T1 = latest time point in all trials | =recurrence | Structure = recurrence rate | 2 None of the outcomes were judged to be of high quality by the author | |||
| Average age: 65 | =ROM | Joint balance = ROM | 3 Lack of blinding | ||||
| DS: non specified | |||||||
| M = 203 | |||||||
| F = 167 | |||||||
| Shen et al. [45] (2014) | Systematic review (3 RCT) | 265 patients | T0 = day one postoperatory | EP > Constant (1 RTC) at 12 months | Function = ASES, Constant, SST | No significant differences in tendon healing. EP > external rotation at six moths but no at 1 year | 1 small number of rcTs included |
| Diagnosis: All participants received rotator cuff repair | T1 = 6 months | =ASES, SST e VAS | Pain = VAS | EP Fastest ROM recovery | 2 some clinical heterogeneity among trials | ||
| Average age: 55.3–63.5 | T2 = 12 months | =tendon healing | |||||
| DS: non specified | =ROM | ||||||
| Huang et al. [46] (2013) | Systematic review (6 RCT) | 448 patients | T0 = day one postoperatory | EP > ROM | Function: DASH, Constant, ASES, SST | EP > ROM but greater risk of un-healing or re-tearing | 1 few article with variable outcome measures and time points of follow-up |
| Diagnosis: All participants received rotator cuff repair | T1 = 6 months | EP > function | Pain = VAS | 2 data of some studies did not fit normal distributions and could not be calculated | |||
| Average age: 55–63 | T2 = 12 months | TP > healing | Structure = healing | ||||
| DS: non specified | EP > risk of retear | 3 all articles were only of fair quality | |||||
| EP > VAS at week 5 and 16, but EP = TP | |||||||
| at T1 and T2 | |||||||
| Riboh et al. [47] (2014) | Systematic review (5 RCT) | 451 patients | T0 = day one postoperatory | Function = Constant, SST, ASES, UCLA | EP > shoulder forward flexion at 3/6/12 months, external rotation only at 3 months | 1 methodologic limitations and moderate risk of bias of 3 of the 5 randomized studies included | |
| Diagnosis: All participants received rotator cuff repair | T1 = 3 months | =recurrence | Pain = VAS | =recurrency | 2 all of the studies suffered from performance bias because neither surgeons nor patients could be blinded to the treatment-group assignment. | ||
| Average age: 54.8–63.2 | T2 = 6 months | EP > ROM | Structure = healing | 3 All 5 studies provide only Level II data | |||
| DS: non specified | T3 = 12 months | ||||||
| Kluczynski et al. [48] 2014 | Meta Analysis (28 RCT) | 1729 patients | T0 = day one postoperatory | EP > risk of retear >5 cm | Structure = recurrence rate, healing | EP greater risk of retear for >5 cm tears, TP greater risk of <3 cm tears | 1 RC healing as only outcome examined |
| Diagnosis: All participants received rotator cuff repair | T1 = latest time point in all trials | TP > risk of retear <3 cm | 2 Most studies included in this review provided evidence levels of 2 to 4 | ||||
| 3 Focused only on passive ROM | |||||||
| Average age: non specified | |||||||
| DS: non specified | |||||||
| Kluczynski et al. [49] 2015 | Meta Analysis (37 RCT) | 2251 patients | T0 = day one postoperatory | EP > risk of retear | Structure = recurrence rate, healing | EP greater risk of retear for >5 cm tears ad <3 cm tears | 1 RC healing as only outcome examined |
| Diagnosis: All participants received rotator cuff repair | T1 = latest time point in all trials, at least 1 year | 2 focused only on the active ROM component of rehabilitation | |||||
| 3 unable to control for the heterogeneity of these studies | |||||||
| Average age: non specified | 4 small sample size of the early active ROM group | ||||||
| DS: non specified |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paolucci, T.; Agostini, F.; Conti, M.; Cazzolla, S.; Mussomeli, E.; Santilli, G.; Poso, F.; Bernetti, A.; Paoloni, M.; Mangone, M. Comparison of Early versus Traditional Rehabilitation Protocol after Rotator Cuff Repair: An Umbrella-Review. J. Clin. Med. 2023, 12, 6743. https://doi.org/10.3390/jcm12216743
Paolucci T, Agostini F, Conti M, Cazzolla S, Mussomeli E, Santilli G, Poso F, Bernetti A, Paoloni M, Mangone M. Comparison of Early versus Traditional Rehabilitation Protocol after Rotator Cuff Repair: An Umbrella-Review. Journal of Clinical Medicine. 2023; 12(21):6743. https://doi.org/10.3390/jcm12216743
Chicago/Turabian StylePaolucci, Teresa, Francesco Agostini, Marco Conti, Sara Cazzolla, Elena Mussomeli, Gabriele Santilli, Federica Poso, Andrea Bernetti, Marco Paoloni, and Massimiliano Mangone. 2023. "Comparison of Early versus Traditional Rehabilitation Protocol after Rotator Cuff Repair: An Umbrella-Review" Journal of Clinical Medicine 12, no. 21: 6743. https://doi.org/10.3390/jcm12216743
APA StylePaolucci, T., Agostini, F., Conti, M., Cazzolla, S., Mussomeli, E., Santilli, G., Poso, F., Bernetti, A., Paoloni, M., & Mangone, M. (2023). Comparison of Early versus Traditional Rehabilitation Protocol after Rotator Cuff Repair: An Umbrella-Review. Journal of Clinical Medicine, 12(21), 6743. https://doi.org/10.3390/jcm12216743










