Assessing the Accuracy of Spinal Instrumentation Using Augmented Reality (AR): A Systematic Review of the Literature and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Literature Search
2.2. Study Selection
2.3. Data Extraction
2.4. Evidence Assessment
2.5. Statistical Analysis
3. Results
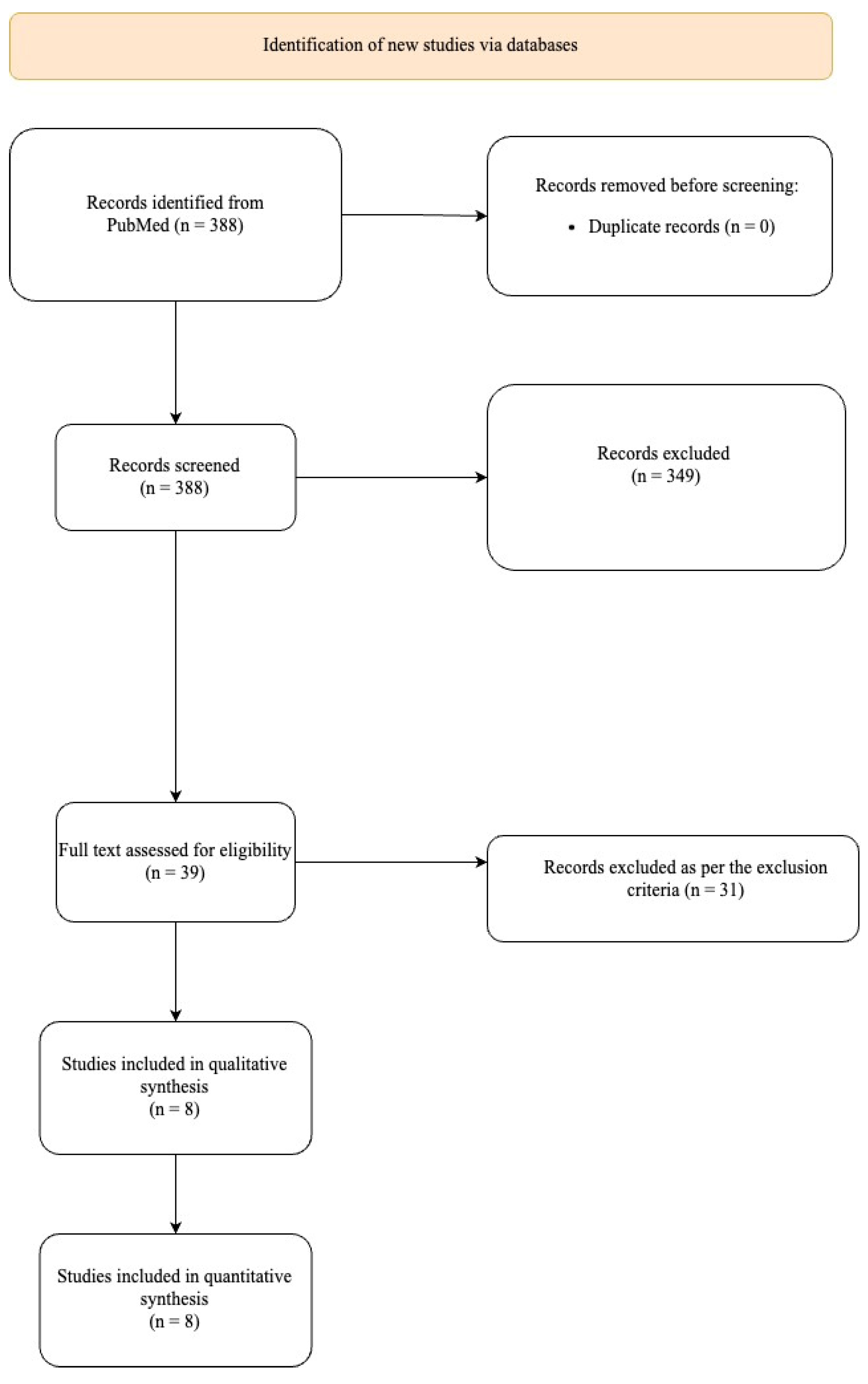
3.1. Study Selection
3.2. Patient Characteristics
3.3. Accuracy
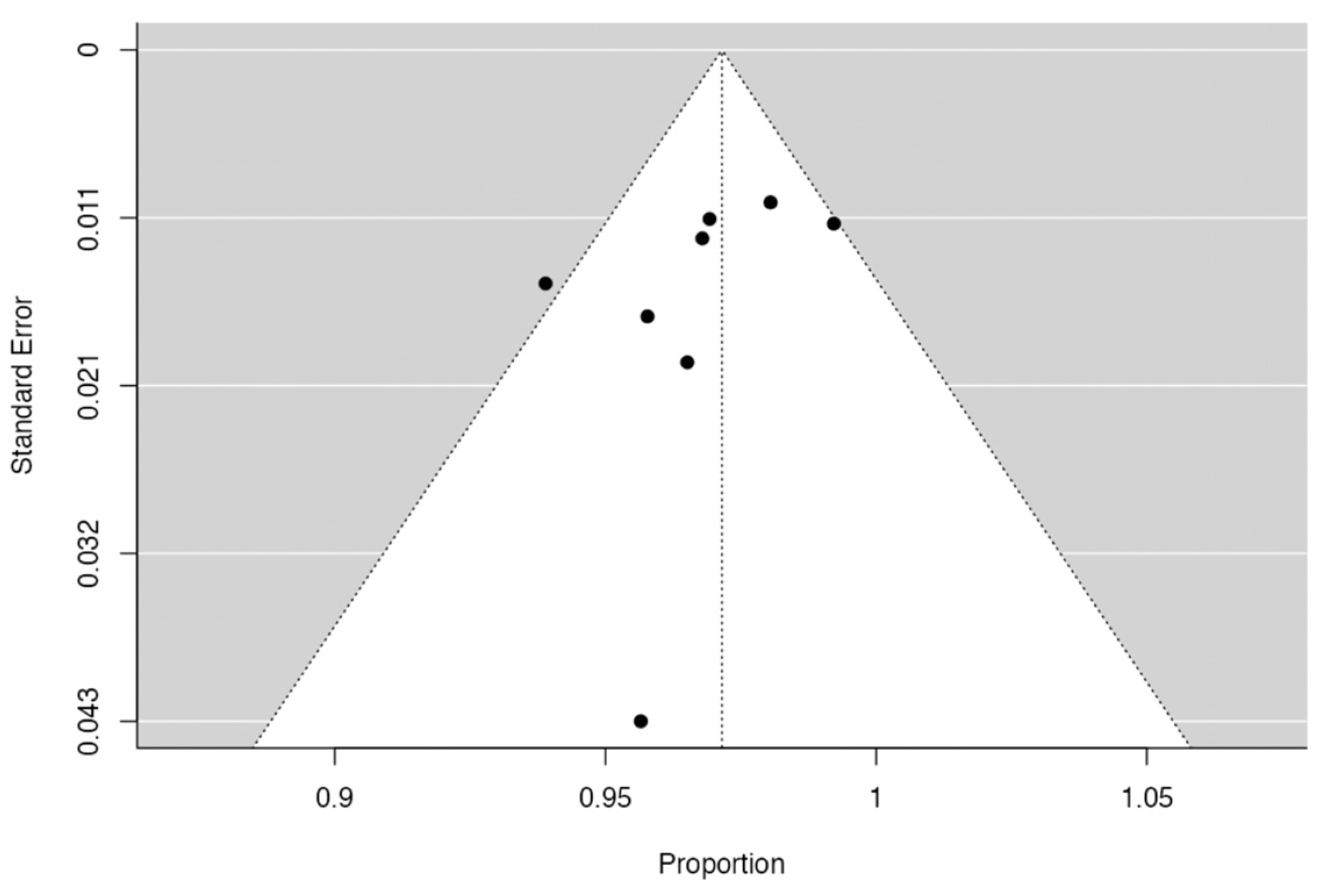
3.4. Publication Bias Assessment
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Perna, F.; Borghi, R.; Pilla, F.; Stefanini, N.; Mazzotti, A.; Chehrassan, M. Pedicle screw insertion techniques: An update and review of the literature. Musculoskelet. Surg. 2016, 100, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Berryman, D.R. Augmented Reality: A Review. Med. Ref. Serv. Q. 2012, 31, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Tagaytayan, R.; Kelemen, A.; Sik-Lanyi, C. Augmented reality in neurosurgery. Arch. Med. Sci. 2018, 14, 572–578. [Google Scholar] [CrossRef]
- Pandya, A.; Siadat, M.R.; Auner, G. Design, implementation and accuracy of a prototype for medical augmented reality. Comput. Aided Surg. 2005, 10, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Molina, C.A.; Dibble, C.F.; Lo, S.-F.L.; Witham, T.; Sciubba, D.M. Augmented reality–mediated stereotactic navigation for execution of en bloc lumbar spondylectomy osteotomies. J. Neurosurg. Spine 2021, 34, 700–705. [Google Scholar] [CrossRef]
- Yahanda, A.T.; Moore, E.; Ray, W.Z.; Pennicooke, B.; Jennings, J.W.; Molina, C.A. First in-human report of the clinical accuracy of thoracolumbar percutaneous pedicle screw placement using augmented reality guidance. Neurosurg. Focus 2021, 51, E10. [Google Scholar] [CrossRef]
- Gu, Y.; Yao, Q.; Xu, Y.; Zhang, H.; Wei, P.; Wang, L. A Clinical Application Study of Mixed Reality Technology Assisted Lumbar Pedicle Screws Implantation. Med. Sci. Monit. 2020, 26, e924982-1. [Google Scholar] [CrossRef]
- Elmi-Terander, A.; Burström, G.; Nachabé, R.; Fagerlund, M.; Ståhl, F.; Charalampidis, A.; Edström, E.; Gerdhem, P. Augmented reality navigation with intraoperative 3D imaging vs fluoroscopy-assisted free-hand surgery for spine fixation surgery: A matched-control study comparing accuracy. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef]
- Liu, H.; Chen, W.; Wang, Z.; Lin, J.; Meng, B.; Yang, H. Comparison of the accuracy between robot-assisted and conventional freehand pedicle screw placement: A systematic review and meta-analysis. Int. J. Comput. Assist. Radiol. Surg. 2016, 11, 2273–2281. [Google Scholar] [CrossRef]
- Burström, G.; Cewe, P.; Charalampidis, A.; Nachabe, R.; Söderman, M.; Gerdhem, P.; Elmi-Terander, A.; Edström, E. Intraoperative cone beam computed tomography is as reliable as conventional computed tomography for identification of pedicle screw breach in thoracolumbar spine surgery. Eur. Radiol. 2020, 31, 2349–2356. [Google Scholar] [CrossRef]
- Bhatt, F.R.; Orosz, L.D.; Tewari, A.; Boyd, D.; Roy, R.; Good, C.R.; Schuler, T.C.; Haines, C.M.; Jazini, E. Augmented Reality-Assisted Spine Surgery: An Early Experience Demonstrating Safety and Accuracy with 218 Screws. Glob. Spine J. 2022, 13, 2047–2052. [Google Scholar] [CrossRef] [PubMed]
- Harel, R.; Anekstein, Y.; Raichel, M.; Molina, C.A.; Ruiz-Cardozo, M.A.; Orrú, E.; Khan, M.; Mirovsky, Y.; Smorgick, Y. The XVS System During Open Spinal Fixation Procedures in Patients Requiring Pedicle Screw Placement in the Lumbosacral Spine. World Neurosurg. 2022, 164, e1226–e1232. [Google Scholar] [CrossRef]
- Judy, B.F.; Liu, A.; Jin, Y.; Ronkon, C.; Khan, M.; Cottrill, E.; Ehresman, J.; Pennington, Z.; Bydon, A.; Lo, S.-F.L.; et al. In-Human Report of S2 Alar-Iliac Screw Placement Using Augmented Reality Assistance. Oper. Neurosurg. 2023, 24, 68–73. [Google Scholar] [CrossRef]
- Gertzbein, S.D.; Robbins, S.E. Accuracy of Pedicular Screw Placement In Vivo. Spine 1990, 15, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Mason, A.; Paulsen, R.; Babuska, J.M.; Rajpal, S.; Burneikiene, S.; Nelson, E.L.; Villavicencio, A.T. The accuracy of pedicle screw placement using intraoperative image guidance systems. J. Neurosurg. Spine 2014, 20, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Krishan, S.; Haendlmayer, K.; Mohsen, A. Functional outcome of computer-assisted spinal pedicle screw placement: A systematic review and meta-analysis of 23 studies including 5992 pedicle screws. Eur. Spine J. 2010, 19, 370–375. [Google Scholar] [CrossRef]
- Alomari, S.; Lubelski, D.; Lehner, K.; Tang, A.; Wolinsky, J.-P.; Theodore, N.; Sciubba, D.M.; Lo, S.-F.M.L.; Belzberg, A.; Weingart, J.; et al. Safety and Accuracy of Freehand Pedicle Screw Placement and the Role of Intraoperative O-Arm: A Single-Institution Experience. Spine 2023, 48, 180–188. [Google Scholar] [CrossRef]
- Vörös, V.; Li, R.; Davoodi, A.; Wybaillie, G.; Poorten, E.V.; Niu, K. An Augmented Reality-Based Interaction Scheme for Robotic Pedicle Screw Placement. J. Imaging 2022, 8, 273. [Google Scholar] [CrossRef]
- Elmi-Terander, A.; Skulason, H.; Söderman, M.; Racadio, J.; Homan, R.; Babic, D.; van der Vaart, N.; Nachabe, R. Surgical Navigation Technology Based on Augmented Reality and Integrated 3D Intraoperative Imaging: A Spine Cadaveric Feasibility and Accuracy Study. Spine 2016, 41, E1303–E1311. [Google Scholar] [CrossRef]
- Peh, S.; Chatterjea, A.; Pfarr, J.; Schäfer, J.P.; Weuster, M.; Klüter, T.; Seekamp, A.; Lippross, S. Accuracy of augmented reality surgical navigation for minimally invasive pedicle screw insertion in the thoracic and lumbar spine with a new tracking device. Spine J. 2020, 20, 629–637. [Google Scholar] [CrossRef]
- Butler, A.J.; Colman, M.W.; Lynch, J.; Phillips, F.M. Augmented reality in minimally invasive spine surgery: Early efficiency and complications of percutaneous pedicle screw instrumentation. Spine J. 2023, 23, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, I.H.; Hardenbrook, M.A.; Wang, J.C.; Guyer, R.D. Assessment of Pedicle Screw Placement Accuracy, Procedure Time, and Radiation Exposure Using a Miniature Robotic Guidance System. J. Spinal Disord. Tech. 2012, 25, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Meyers, J.E.; Siasios, I.; Pollina, J. Next-Generation Robotic Spine Surgery: First Report on Feasibility, Safety, and Learning Curve. Oper. Neurosurg. 2019, 17, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Edström, E.; Burström, G.; Persson, O.; Charalampidis, A.; Nachabe, R.; Gerdhem, P.; Elmi-Terander, A. Does Augmented Reality Navigation Increase Pedicle Screw Density Compared to Free-Hand Technique in Deformity Surgery? Single Surgeon Case Series of 44 Patients. Spine 2020, 45, E1085–E1090. [Google Scholar] [CrossRef] [PubMed]
- Boyaci, M.G.; Fidan, U.; Yuran, A.F.; Yildizhan, S.; Kaya, F.; Kimsesiz, O.; Ozdil, M.; Cengiz, A.; Aslan, A. Augmented reality supported cervical transpedicular fixation on 3D-printed vertebrae model: An experimental education study. Turk. Neurosurg. 2020, 30, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Xun, H.; Abousy, M.; Long, C.; Sacks, J.M. No Microscope? No Problem: A Systematic Review of Microscope-Free Microsurgery Training Models. J. Reconstr. Microsurg. 2021, 38, 106–114. [Google Scholar] [CrossRef]
- Menger, R.P.; Savardekar, A.R.; Farokhi, F.; Sin, A. A Cost-Effectiveness Analysis of the Integration of Robotic Spine Technology in Spine Surgery. Neurospine 2018, 15, 216–224. [Google Scholar] [CrossRef]
- Rivkin, M.A.; Yocom, S.S. Thoracolumbar instrumentation with CT-guided navigation (O-arm) in 270 consecutive patients: Accuracy rates and lessons learned. Neurosurg. Focus 2014, 36, E7. [Google Scholar] [CrossRef]
- Zhang, Q.; Fan, M.-X.; Han, X.-G.; Liu, Y.-J.; He, D.; Liu, B.; Tian, W. Risk Factors of Unsatisfactory Robot-Assisted Pedicle Screw Placement: A Case-Control Study. Neurospine 2021, 18, 839–844. [Google Scholar] [CrossRef]
- Murata, K.; Fujibayashi, S.; Otsuki, B.; Shimizu, T.; Masamoto, K.; Matsuda, S. Accuracy of fluoroscopic guidance with the coaxial view of the pedicle for percutaneous insertion of lumbar pedicle screws and risk factors for pedicle breach. J. Neurosurg. Spine 2020, 1, 52–59. [Google Scholar] [CrossRef]

| Author, Year | Study | Technology | No. of Screws | No. of Patients | Gender | Mean Age (yrs) | Spinal Level | Pathology | Accuracy Assessment Tool | Accuracy (%) | Breach Grade |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gu et al., 2020 [7] | RCT | MR | 142 | 25 | 11 M 14 F | 44.32 | 142 L | Lumbar spondylolisthesis (n = 7) | NR | 95.77 | NR |
| Emi-Terander et al., 2020 [8] | Prospective | Allura ARSN | 262 | 20 | 9 M 11 F | 30 | 166 T, 96LS | Scoliosis (n = 13), kyphosis (n = 2), other (n = 5) | G | 93.9 | 63.4% Grade 0 30.5% Grade 1 6.1% Grade 2 |
| Liu et al., 2021 [9] | Retrospective | XVS | 205 | 28 | 11 M 17 F | 62.5 * | 67 T, 112 L, 26 S1 | 12 degenerative disease; 12 deformity correction; 3 tumor; and 1 trauma | GR scale | 98 | 94% Grade A 4% Grade B 1.5% Grade C 0.5% Grade D |
| Yahanda et al., 2021 [6] | Retrospective | XVS | 63 | 9 | 5 M 4 F | 71.9 | 32 T, 31 L | 4 tumors, 3 degenerative disease, 1 spinal deformity, and 1 infection | GR scale | 100 | 96.8% Grade A, 3.2% Grade B |
| Burström et al., 2021 [10] | Retrospective | Allura ARSN | 260 | 20 | 9 M 11 F | 30.5 | 166 T, 94 LS | 13 scoliosis, 2 kyphosis, 3 lumbar spondylolisthesis, 1 lumbar spinal stenosis, 1 lumbar degenerative disk disease | GR scale | 97 | NR |
| R Bhatt et al., 2022 [11] | Prospective | XVS | 218 | 32 | 13 M 19 F | 50.9 | TLSP | 6 deformity, 5 instability, 9 postlaminectomy syndrome, 2 pseudoarthrosis, 10 stenosis | GR scale | 97.1 | 91.8% Grade A, 5.3% Grade B |
| Harel et al., 2022 [12] | Prospective | XVS | 86 | 17 | 7 M 10 F | 60.23 | 40 L, 46 LS | 17 spondylosis | GR scale | 97.7 | 84.9% Grade A, 12.8% Grade B, 2.3% Grade C |
| Judy et al., 2023 [13] | Retrospective | XVS | 23 | 12 | 4 M 8 F | 63 * | S2 alar-iliac | 3 degenerative disease, 8 deformity, 1 tumor | G | 95.6 | 91.3% Grade 0, 4.3% Grade 1, 4.3% Grade 3 |
| Parameter | Frequency |
|---|---|
| Number of Screws | 1259 |
| Thoracic | 431 (34.2%) |
| Lumbar | 194 (15.4%) |
| Lumbosacral | 221 (17.6%) |
| S1 | 26 (2.1%) |
| S2 alar-iliac | 23 (1.8%) |
| No. of Patients | 163 |
| Males | 69 (42.3%) |
| Females | 94 (57.7%) |
| Conditions | |
| Deformity | 74 (45.4%) |
| Tumor | 8 (5%) |
| Degenerative disease | 35 (21.5%) |
| Spondylolisthesis | 10 (6.1%) |
| Trauma | 1 (0.6%) |
| Infection | 1 (0.6%) |
| Pseudoarthrosis | 2 (1.2%) |
| Postlaminectomy syndrome | 9 (5.5%) |
| Others | 5 (3.1%) |
| AR System | |
| XVision, head mounted | 595 screws |
| Allura ARSN | 462 screws |
| Mixed reality | 142 screws |
| Gertzbein Classification | Gertzbein and Robbins Grading | Interpretation |
|---|---|---|
| Grade 0 | Grade A | No cortical breach or screw within pedicle |
| Grade 1 | Grade B | 0–2 mm breach |
| Grade 2 | Grade C | 2–4 mm breach |
| Grade 3 | Grade D | 4–6 mm breach |
| Grade E | >6 mm breach |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pahwa, B.; Azad, T.D.; Liu, J.; Ran, K.; Liu, C.J.; Tracz, J.; Sattari, S.A.; Khalifeh, J.M.; Judy, B.F.; Bydon, A.; et al. Assessing the Accuracy of Spinal Instrumentation Using Augmented Reality (AR): A Systematic Review of the Literature and Meta-Analysis. J. Clin. Med. 2023, 12, 6741. https://doi.org/10.3390/jcm12216741
Pahwa B, Azad TD, Liu J, Ran K, Liu CJ, Tracz J, Sattari SA, Khalifeh JM, Judy BF, Bydon A, et al. Assessing the Accuracy of Spinal Instrumentation Using Augmented Reality (AR): A Systematic Review of the Literature and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(21):6741. https://doi.org/10.3390/jcm12216741
Chicago/Turabian StylePahwa, Bhavya, Tej D. Azad, Jiaqi Liu, Kathleen Ran, Connor J. Liu, Jovanna Tracz, Shahab Aldin Sattari, Jawad M. Khalifeh, Brendan F. Judy, Ali Bydon, and et al. 2023. "Assessing the Accuracy of Spinal Instrumentation Using Augmented Reality (AR): A Systematic Review of the Literature and Meta-Analysis" Journal of Clinical Medicine 12, no. 21: 6741. https://doi.org/10.3390/jcm12216741
APA StylePahwa, B., Azad, T. D., Liu, J., Ran, K., Liu, C. J., Tracz, J., Sattari, S. A., Khalifeh, J. M., Judy, B. F., Bydon, A., & Witham, T. F. (2023). Assessing the Accuracy of Spinal Instrumentation Using Augmented Reality (AR): A Systematic Review of the Literature and Meta-Analysis. Journal of Clinical Medicine, 12(21), 6741. https://doi.org/10.3390/jcm12216741






