Rat Calvaria Model Mimicking the Intraoral Lesion of Medication-Related Osteonecrosis in the Jaw: A Preliminary Test
Abstract
:1. Introduction
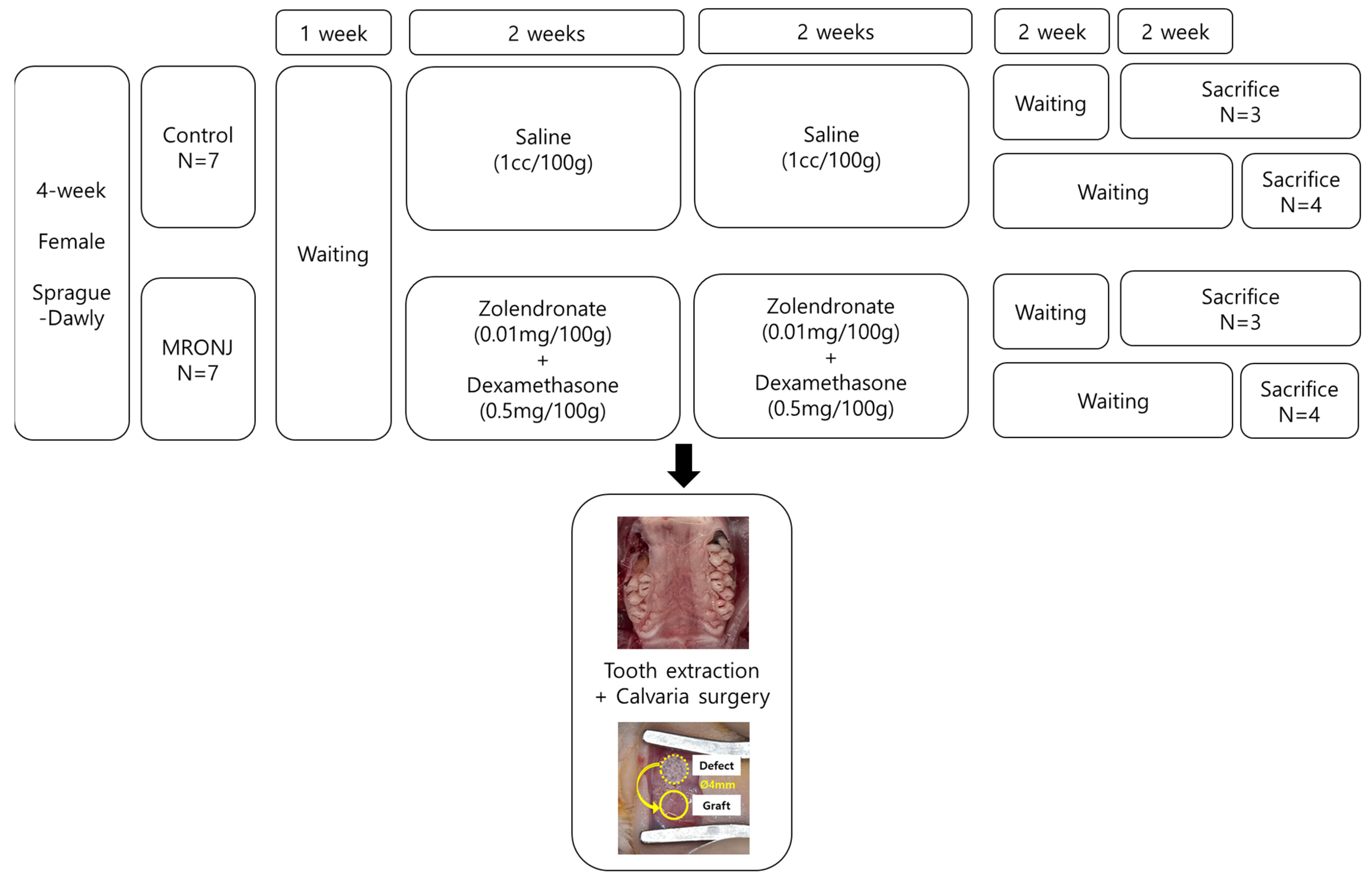
2. Materials and Methods
2.1. Experimental Protocol
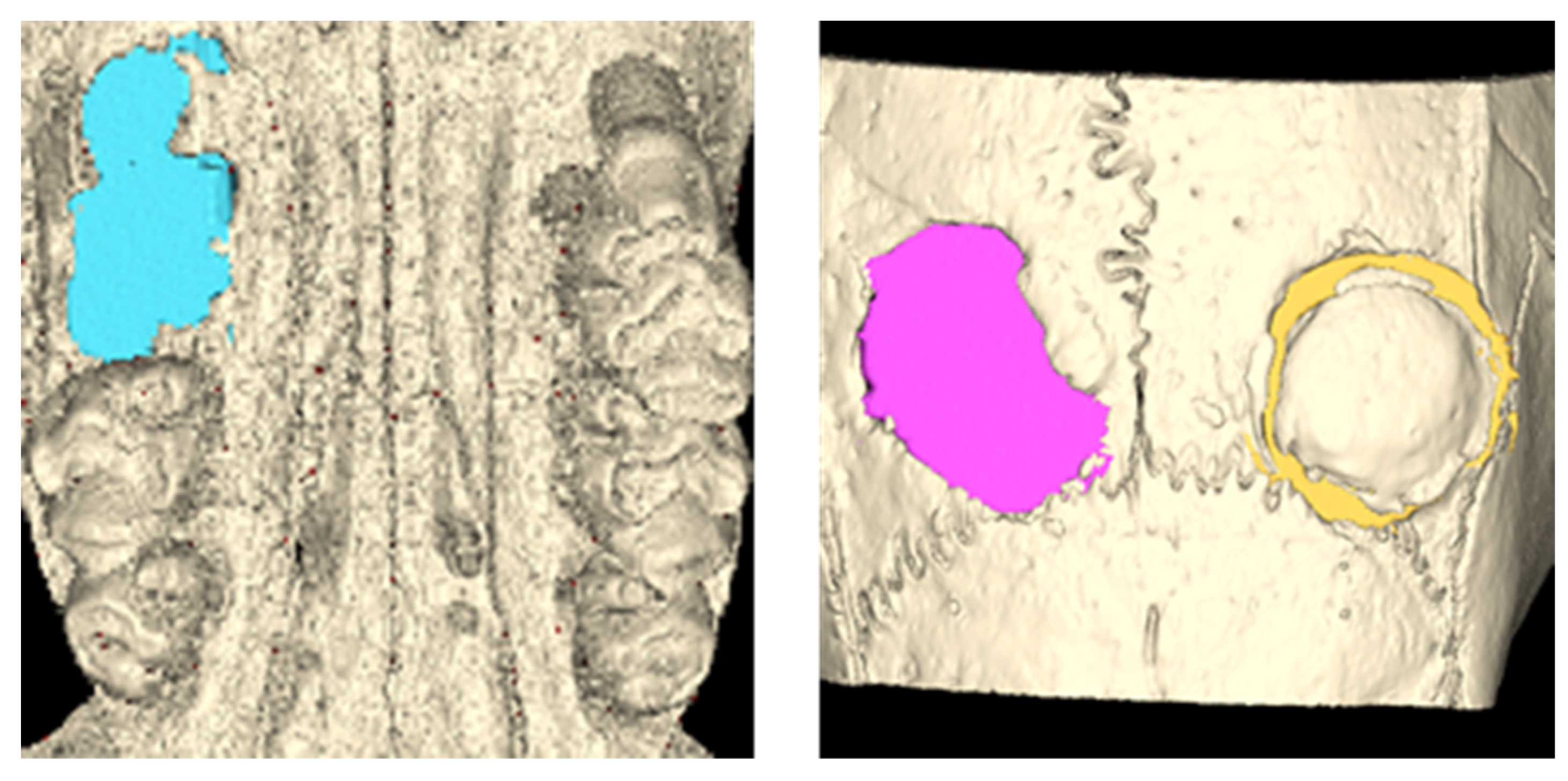
2.2. Evaluation Methods
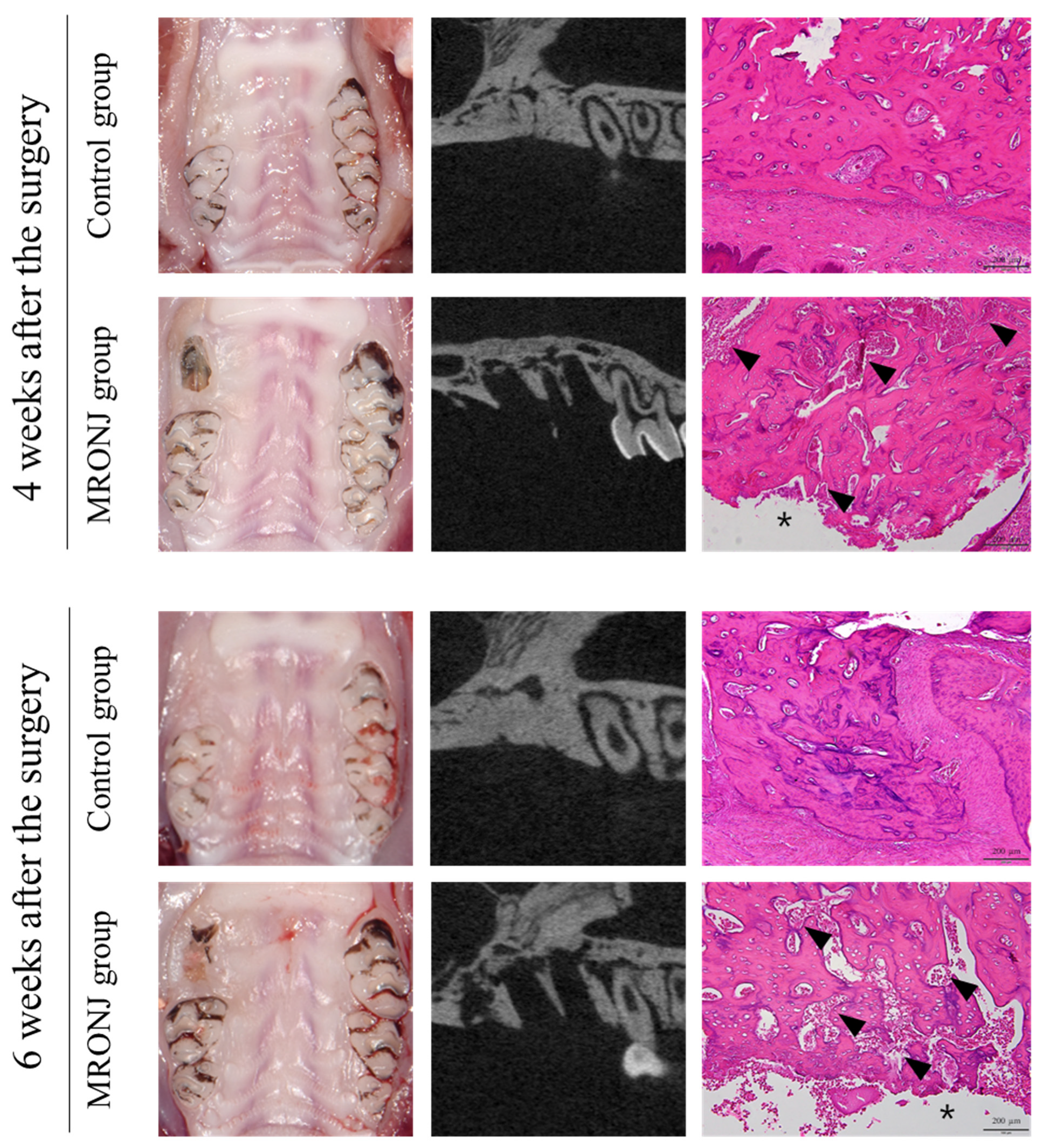
3. Results
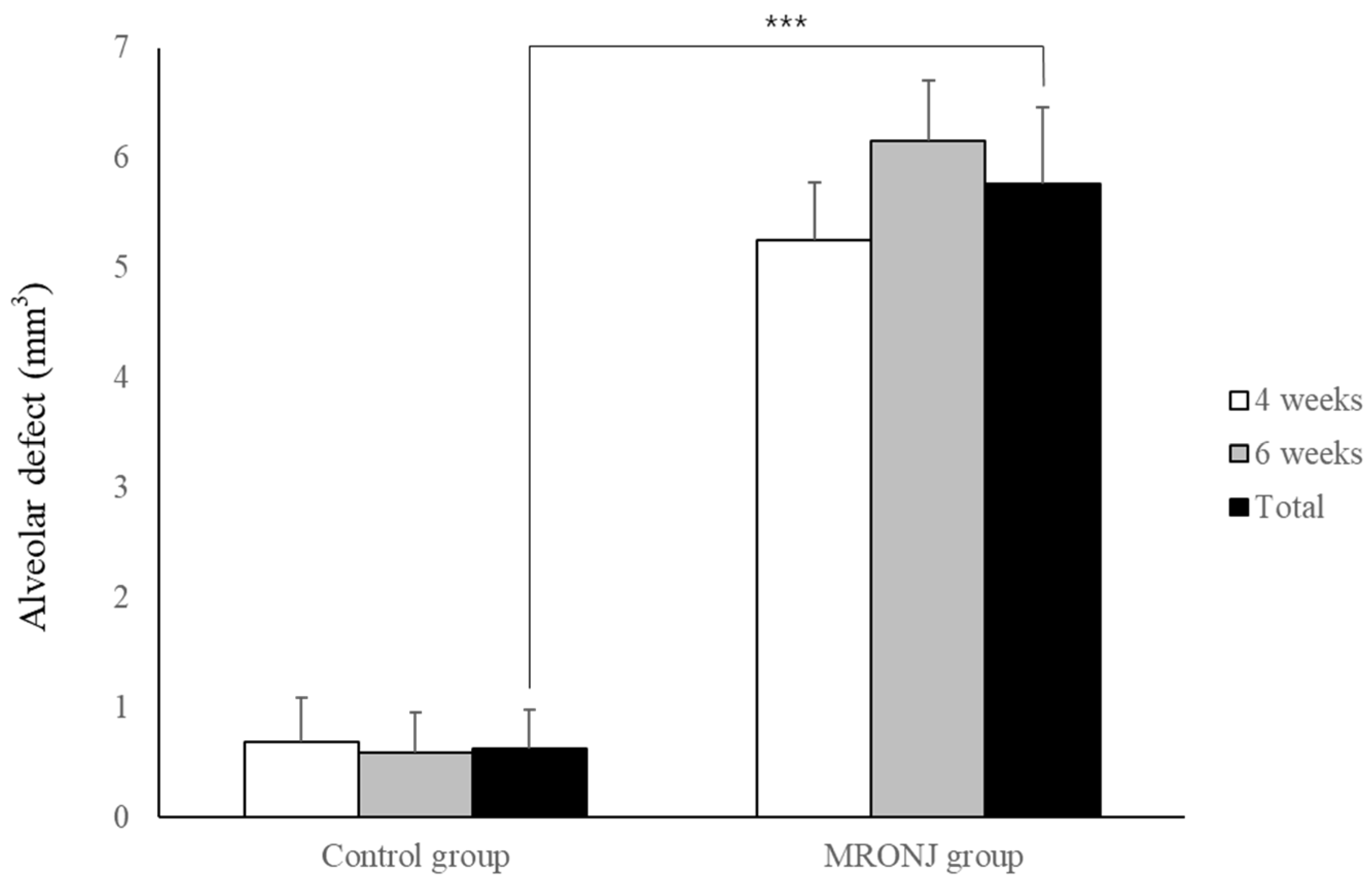
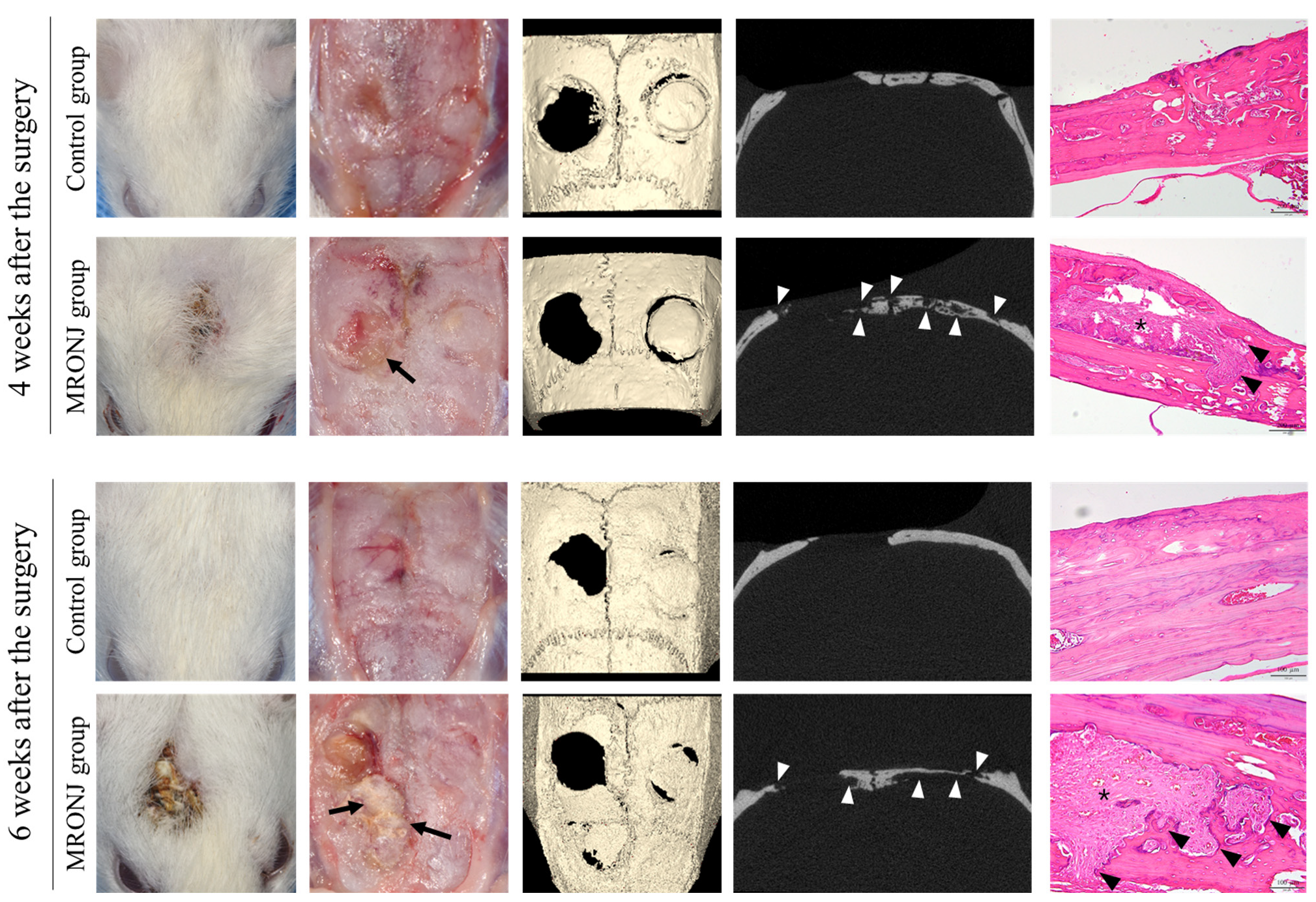
3.1. Alveolar Defect
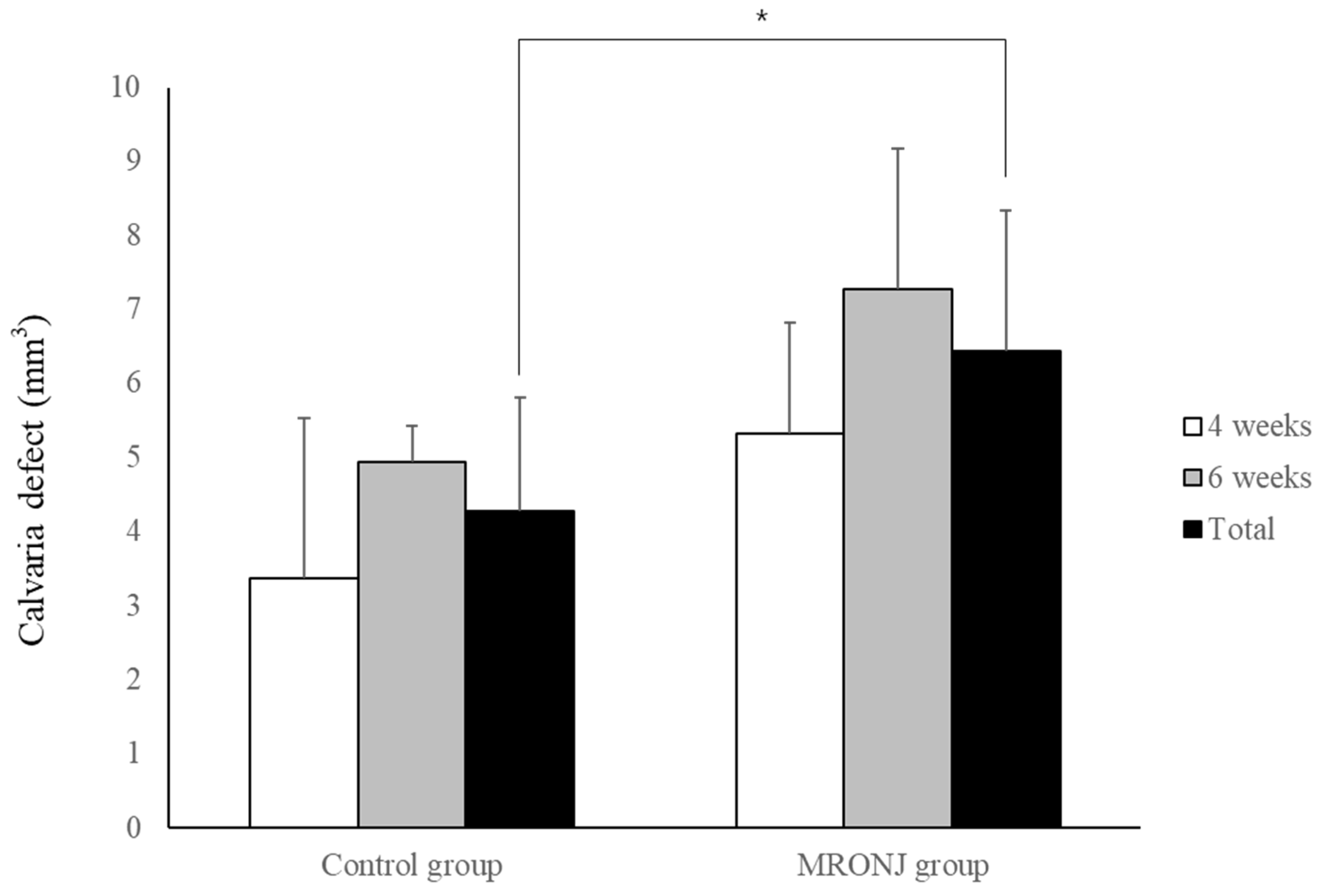
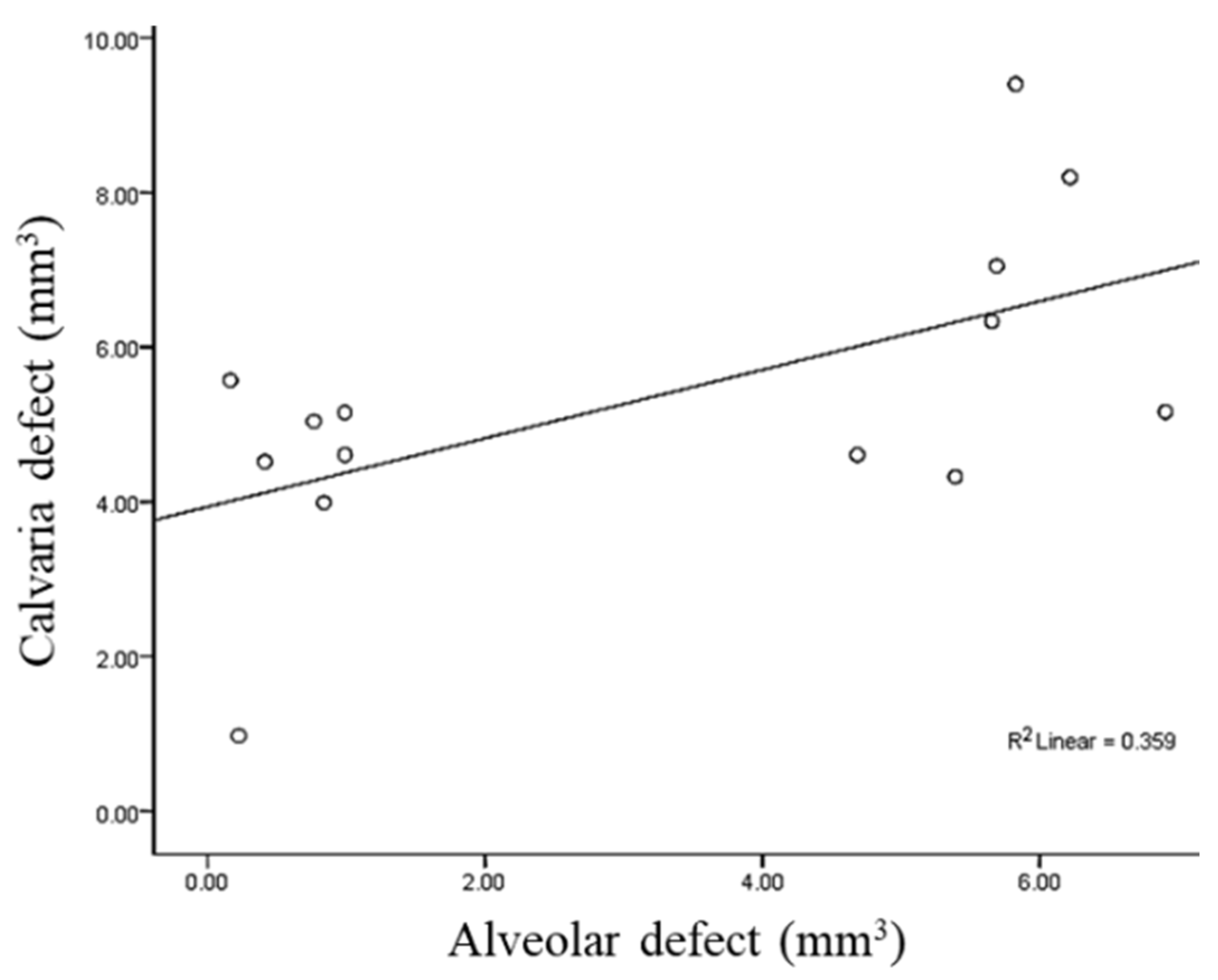
3.2. Calvaria Defect
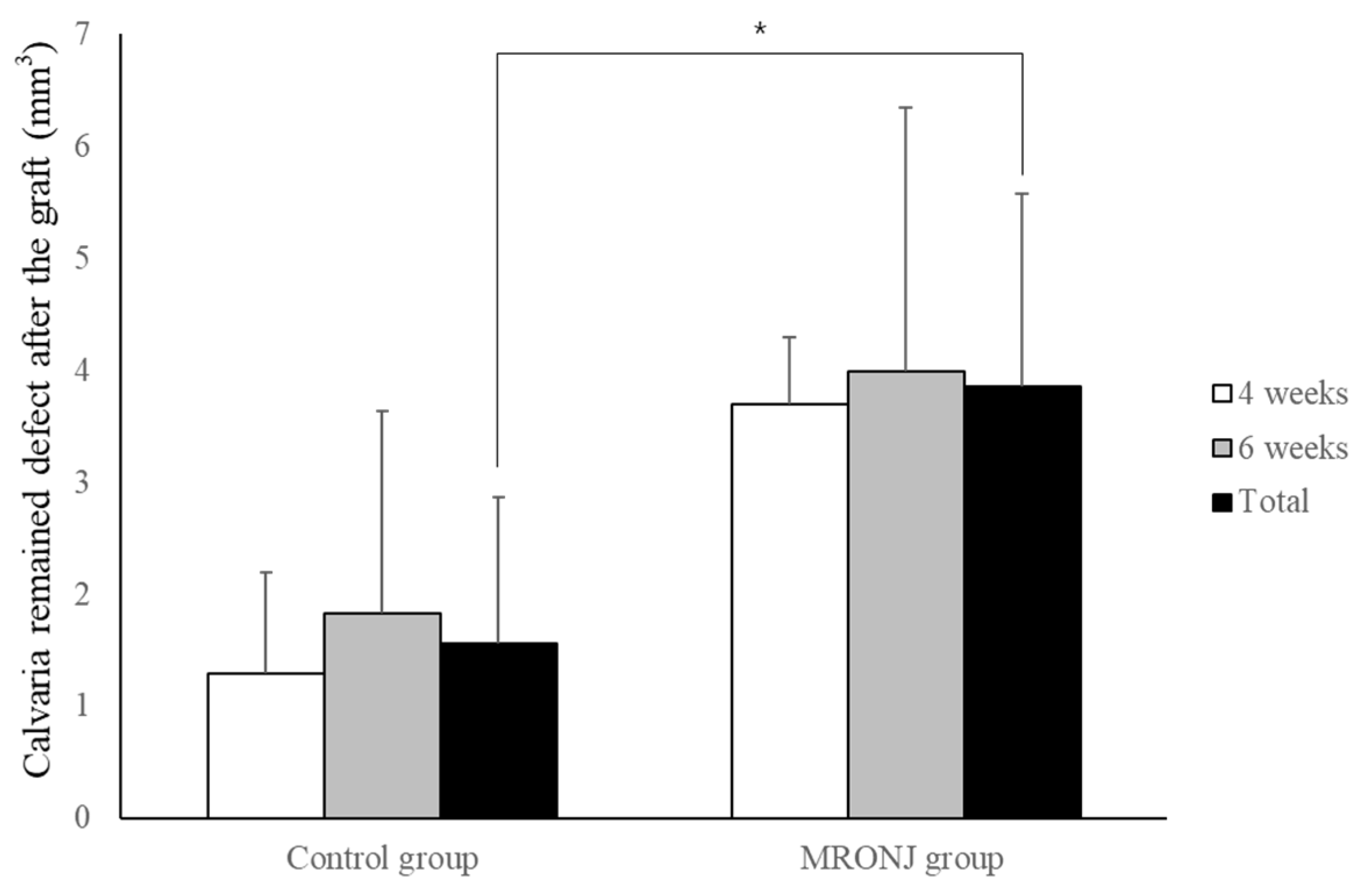
3.3. Autogenous Bone Grafts in Calvaria Defect
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim, Y.H.; Lee, H.K.; Song, S.I.; Lee, J.K. Drug holiday as a prognostic factor of medication-related osteonecrosis of the jaw. J. Korean Assoc. Oral Maxillofac. Surg. 2014, 40, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Haworth, A.E.; Webb, J. Skeletal complications of bisphosphonate use: What the radiologist should know. Br. J. Radiol. 2012, 85, 1333–1342. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, S.L.; Dodson, T.B.; Fantasia, J.; Goodday, R.; Aghaloo, T.; Mehrotra, B.; O’Ryan, F. American association of oral and maxillofacial surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2014, 72, 1938–1956. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.E. Pamidronate (aredia) and zoledronate (zometa) induced avascular necrosis of the jaws: A growing epidemic. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2003, 61, 1115–1117. [Google Scholar] [CrossRef]
- Mavrokokki, T.; Cheng, A.; Stein, B.; Goss, A. Nature and frequency of bisphosphonate-associated osteonecrosis of the jaws in australia. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007, 65, 415–423. [Google Scholar] [CrossRef]
- Khosla, S.; Burr, D.; Cauley, J.; Dempster, D.W.; Ebeling, P.R.; Felsenberg, D.; Gagel, R.F.; Gilsanz, V.; Guise, T.; Koka, S.; et al. Bisphosphonate-associated osteonecrosis of the jaw: Report of a task force of the american society for bone and mineral research. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2007, 22, 1479–1491. [Google Scholar] [CrossRef]
- Lee, J.K.; Kim, K.W.; Choi, J.Y.; Moon, S.Y.; Kim, S.G.; Kim, C.H.; Kim, H.M.; Kwon, Y.D.; Kim, Y.D.; Lee, D.K.; et al. Bisphosphonates-related osteonecrosis of the jaw in korea: A preliminary report. J. Korean Assoc. Oral Maxillofac. Surg. 2013, 39, 9–13. [Google Scholar] [CrossRef]
- Pérez-Sayáns, M.; Vidal-Real, C.; Suárez-Peñaranda, J.M.; García-García, A. Osteonecrosis of the jaws. Prevalence, risk factors and role of microbiota and inflammation in a population of spain. Osteonecrosis 2017, 45, 46–78. [Google Scholar]
- Bilezikian, J.P. Osteonecrosis of the jaw—Do bisphosphonates pose a risk? N. Engl. J. Med. 2006, 355, 2278–2281. [Google Scholar] [CrossRef]
- Wat, W.Z.M. Current controversies on the pathogenesis of medication-related osteonecrosis of the jaw. Dent. J. 2016, 4, 38. [Google Scholar] [CrossRef]
- On, S.W.; Cho, S.W.; Byun, S.H.; Yang, B.E. Various therapeutic methods for the treatment of medication-related osteonecrosis of the jaw (mronj) and their limitations: A narrative review on new molecular and cellular therapeutic approaches. Antioxidants 2021, 10, 680. [Google Scholar] [CrossRef] [PubMed]
- Yan, R.; Jiang, R.; Hu, L.; Deng, Y.; Wen, J.; Jiang, X. Establishment and assessment of rodent models of medication-related osteonecrosis of the jaw (mronj). Int. J. Oral Sci. 2022, 14, 41. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Alshaikh, A.; Kim, T.; Kim, S.; Dang, M.; Mehrazarin, S.; Shin, K.H.; Kang, M.; Park, N.H.; Kim, R.H. Preexisting periapical inflammatory condition exacerbates tooth extraction-induced bisphosphonate-related osteonecrosis of the jaw lesions in mice. J. Endod. 2016, 42, 1641–1646. [Google Scholar] [CrossRef]
- Kim, J.-W.; Tatad, J.C.I.; Landayan, M.E.A.; Kim, S.-J.; Kim, M.-R. Animal model for medication-related osteonecrosis of the jaw with precedent metabolic bone disease. Bone 2015, 81, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Niibe, K.; Ouchi, T.; Iwasaki, R.; Nakagawa, T.; Horie, N. Osteonecrosis of the jaw in patients with dental prostheses being treated with bisphosphonates or denosumab. J. Prosthodont. Res. 2015, 59, 3–5. [Google Scholar] [CrossRef]
- Xia, C.W.; Pan, J.R.; Fan, L.; Xiao, Q.; Pu, Y.; Wang, Y.X. The feasibility of locating the affected bone of bronj with indocyanine green. Oral Dis. 2020, 26, 1086–1089. [Google Scholar] [CrossRef]
- Ning, H.; Wu, X.; Wu, Q.; Yu, W.; Wang, H.; Zheng, S.; Chen, Y.; Li, Y.; Su, J. Microfiber-reinforced composite hydrogels loaded with rat adipose-derived stem cells and bmp-2 for the treatment of medication-related osteonecrosis of the jaw in a rat model. ACS Biomater. Sci. Eng. 2019, 5, 2430–2443. [Google Scholar] [CrossRef]
- Yadegari, A.; Aminzadeh, A.; Seyyedkhamesi, S.; Aminian, M. The effect of melatonin on prevention of bisphosphonate-related osteonecrosis of the jaw: An animal study in rats. J. Korean Assoc. Oral Maxillofac. Surg. 2020, 46, 266–274. [Google Scholar] [CrossRef]
- Choi, J.-Y.; Kim, H.-J.; Lee, Y.-C.; Cho, B.-O.; Seong, H.-S.; Cho, M.; Kim, S.-G. Inhibition of bone healing by pamidronate in calvarial bony defects. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 321–328. [Google Scholar] [CrossRef]
- Prueter, J.; Dildeep, A. Bisphosphonate related osteonecrosis of calvarial bone. Am. J. Otolaryngol. 2016, 37, 470–472. [Google Scholar] [CrossRef]
- McCadden, L.; Leonard, C.G.; Primrose, W.J. Bisphosphonate-induced osteonecrosis of the ear canal: Our experience and a review of the literature. J. Laryngol. Otol. 2018, 132, 372–374. [Google Scholar] [CrossRef]
- True, H.D.; Ricks, R.G.; Smith, J.A. Denosumab and bisphosphonate associated bilateral osteonecrosis of the external auditory canal. BMJ Case Rep. 2021, 14, e241203. [Google Scholar] [CrossRef]
- Wang, J.; Huang, Z.; Wang, F.; Yu, X.; Li, D. Materialise’s interactive medical image control system (mimics) is feasible for volumetric measurement of urinary calculus. Urolithiasis 2020, 48, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Lee, Y.J.; Jeong, S.H.; Kwon, T.G. Density of the alveolar and basal bones of the maxilla and the mandible. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Yavuz, M.S.; Buyukkurt, M.C.; Tozoglu, S.; Dagsuyu, I.M.; Kantarci, M. Evaluation of volumetry and density of mandibular symphysis bone grafts by three-dimensional computed tomography. Dent. Traumatol. 2009, 25, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Ku, J.K.; Han, M.; Yongvikul, A.; Huh, J.K.; Kim, J.Y. Volumetric analysis of spontaneous bone healing after jaw cyst enucleation. Sci. Rep. 2022, 12, 14953. [Google Scholar] [CrossRef] [PubMed]
- Gomes, P.S.; Fernandes, M.H. Rodent models in bone-related research: The relevance of calvarial defects in the assessment of bone regeneration strategies. Lab. Anim. 2011, 45, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Vajgel, A.; Mardas, N.; Farias, B.C.; Petrie, A.; Cimões, R.; Donos, N. A systematic review on the critical size defect model. Clin. Oral Implant. Res. 2014, 25, 879–893. [Google Scholar] [CrossRef]
- Donos, N.; Akcali, A.; Padhye, N.; Sculean, A.; Calciolari, E. Bone regeneration in implant dentistry: Which are the factors affecting the clinical outcome? Periodontology 2000 2023, 00, 1–30. [Google Scholar] [CrossRef]
- Bosch, C.; Melsen, B.; Vargervik, K. Importance of the critical-size bone defect in testing bone-regenerating materials. J. Craniofacial Surg. 1998, 9, 310–316. [Google Scholar] [CrossRef]
- Mikai, A.; Ono, M.; Tosa, I.; Nguyen, H.T.T.; Hara, E.S.; Nosho, S.; Kimura-Ono, A.; Nawachi, K.; Takarada, T.; Kuboki, T.; et al. Bmp-2/β-tcp local delivery for bone regeneration in mronj-like mouse model. Int. J. Mol. Sci. 2020, 21, 7028. [Google Scholar] [CrossRef] [PubMed]
- Listik, E.; Giro, G.; Negrisoli, S.; Rodrigues, I.V.; Duarte, P.M.; Nahás-Scocate, A.C.R. Bisphosphonate therapy and orthodontics: Implications for postmenopausal women. J. Clin. Orthod. 2022, 56, 175–182. [Google Scholar] [PubMed]
- Jung, J.; Yoo, H.Y.; Kim, G.T.; Lee, J.W.; Lee, Y.A.; Kim, D.Y.; Kwon, Y.D. Short-term teriparatide and recombinant human bone morphogenetic protein-2 for regenerative approach to medication-related osteonecrosis of the jaw: A preliminary study. J. Bone Min. Res. 2017, 32, 2445–2452. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Jang, H.W.; Kim, J.I.; Cha, I.H. Effects of pre-extraction intermittent pth administration on extraction socket healing in bisphosphonate administered ovariectomized rats. Sci. Rep. 2021, 11, 54. [Google Scholar] [CrossRef]
- Khoury, F.; Hidajat, H. Extensive autogenous bone augmentation and implantation in patients under bisphosphonate treatment: A 15-case series. Int. J. Periodontics Restor. Dent. 2016, 36, 9–18. [Google Scholar] [CrossRef]
- Ku, J.K.; Lee, K.G.; Ghim, M.S.; Kim, Y.K.; Park, S.H.; Park, Y.; Cho, Y.S.; Lee, B.K. Onlay-graft of 3D printed kagome-structure pcl scaffold incorporated with rhbmp-2 based on hyaluronic acid hydrogel. Biomed. Mater. 2021, 16, 055004. [Google Scholar] [CrossRef]
- Araújo, C.R.G.; Astarita, C.; D’Aquino, R.; Pelegrine, A.A. Evaluation of bone regeneration in rat calvaria using bone autologous micrografts and xenografts: Histological and histomorphometric analysis. Materials 2020, 13, 4284. [Google Scholar] [CrossRef]
- de Almeida, A.L.; Medeiros, I.L.; Cunha, M.J.; Sbrana, M.C.; de Oliveira, P.G.; Esper, L.A. The effect of low-level laser on bone healing in critical size defects treated with or without autogenous bone graft: An experimental study in rat calvaria. Clin. Oral Implant. Res. 2014, 25, 1131–1136. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.; Ku, J.-K. Rat Calvaria Model Mimicking the Intraoral Lesion of Medication-Related Osteonecrosis in the Jaw: A Preliminary Test. J. Clin. Med. 2023, 12, 6731. https://doi.org/10.3390/jcm12216731
Kim Y, Ku J-K. Rat Calvaria Model Mimicking the Intraoral Lesion of Medication-Related Osteonecrosis in the Jaw: A Preliminary Test. Journal of Clinical Medicine. 2023; 12(21):6731. https://doi.org/10.3390/jcm12216731
Chicago/Turabian StyleKim, Yesel, and Jeong-Kui Ku. 2023. "Rat Calvaria Model Mimicking the Intraoral Lesion of Medication-Related Osteonecrosis in the Jaw: A Preliminary Test" Journal of Clinical Medicine 12, no. 21: 6731. https://doi.org/10.3390/jcm12216731
APA StyleKim, Y., & Ku, J.-K. (2023). Rat Calvaria Model Mimicking the Intraoral Lesion of Medication-Related Osteonecrosis in the Jaw: A Preliminary Test. Journal of Clinical Medicine, 12(21), 6731. https://doi.org/10.3390/jcm12216731





