Abstract
Polypharmacy can result in drug–drug interactions, severe side-effects, drug–disease interactions, inappropriate medication use in the elderly, and escalating costs. This study aims to evaluate nursing home residents’ medication regimens using a rational drug use web assistant developed by researchers to mitigate unnecessary medication usage. This analytical, cross-sectional study included data from nursing home residents recently recorded in a training family health center. Sociodemographic information, medical conditions, and prescribed medications of all patients in the nursing home (n = 99) were documented. Medications were assessed using an artificial intelligence-aided rational drug use web assistant. Instances of inappropriate drug use and calculations of contraindicated drug costs were also recorded. The study revealed that 88.9% (n = 88) of patients experienced polypharmacy, with a mean value of 6.96 ± 2.94 drugs per patient. Potential risky drug–drug interactions were present in 89.9% (n = 89) of patients, contraindicated drug–drug interactions in 20.2% (n = 20), and potentially inappropriate drug use in 86.9% (n = 86). Plans to discontinue 83 medications were estimated to reduce total direct medication costs by 9.1% per month. After the assessment with the rational drug use web assistant, the number of drugs that patients needed to use and polypharmacy decreased significantly. This study concludes that the rational drug use web assistant application, which is more cost-effective than the traditional manual method, assisted by artificial intelligence, and integrated into healthcare services, may offer substantial benefits to family physicians and their geriatric patients.
1. Introduction
Individuals may have several diseases and have to use a lot of drugs for therapeutic purposes for these diseases. There may be drug–drug interactions when more than one drug is used. In this case, patients can be exposed to several side-effects instead of being treated. Regression in organ functions depending on pharmacokinetic and pharmacodynamic changes occurs due to aging, and for this reason, elderly patients are more exposed to the side-effects of drugs used for treatment [1]. Therefore, it is necessary to be sensitive in terms of drug side-effects in elderly patients, and drug side-effects should be taken into account for any new symptoms [2]. Inappropriate drug use has a great impact on the risk of drug side-effects and a decrease in cognitive functions [3]. In this manner, appropriate drug use is crucial, particularly in elderly patients [4].
The use of some drugs is inappropriate for patients above the age of 65. The term “polypharmacy” is generally known as the use of five or more drugs at the same time. However, as well as the number of drugs, inappropriate indications and the use of two or more unnecessary drugs together are also known as polypharmacy [5,6,7].
Polypharmacy may be caused by the patient or the healthcare system. Regarding patient-related conditions, the number of drugs used for chronic diseases increases, and therefore, polydrug use appears [8]. However, concomitant diseases in individuals independent of age also cause polydrug use and thereby the increase in related side-effects [1].
Conditions such as an insufficient number of family physicians who will coordinate drug treatment, extremely busy schedules of physicians, physicians’ lack of knowledge on side-effects of the drug, and drug–drug interactions can be among the factors regarding the healthcare system [8]. Moreover, “prescribing cascade”, which is defined as prescribing another drug to treat the side-effect of a drug, is also another important cause of polypharmacy [9,10].
Drug–drug interaction, side-effects of drugs, drug–disease interaction, inappropriate drug use in the elderly, and increase in treatment costs, hospitalization, and mortality are among the complications of polypharmacy [7]. As the number of drugs used increases, side-effects of drugs increase.
Family physicians provide primary healthcare services and several patients visit them to have their drugs prescribed. While prescribing the drugs of patients here, assessment of drugs, diseases, drug–drug interactions, drug appropriateness, and rational drug use become crucial. Moreover, family physicians approach patients in a holistic way and evaluate them with all their diseases and keep their patients from overmedicalization through quaternary prevention. In this regard, they have crucial responsibilities in regulating patients’ drugs.
Our study aimed to assess patients staying in a nursing home in terms of diseases, drugs used, drug–drug interactions of these drugs, and appropriate use of these drugs by age through a rational drug use web assistant [7] developed by researchers. Therefore, the drugs of these patients were checked, and inappropriate or unnecessary drugs were detected; cessation of these drugs after consulting related departments could be possible. Decreasing the rates of mortality, morbidity, hospitalization, and side-effects and the direct and indirect unnecessary costs of these were targeted by preventing patients from using unnecessary and unregulated drugs.
2. Materials and Methods
Our research is an observational and cross-sectional study. A web-assisted application for rational drug use [7] that was developed by the researchers and used in the healthcare center in which we provided primary healthcare services was utilized in our study. In addition, a data collection form structured particularly to the study established with parameters that were determined by the researchers was used.
The study population consisted of all patients staying in the nursing home who had recently been recorded at the Çayyolu Training Family Health Center of Ankara Bilkent City Hospital. All volunteer patients from the nursing home (n = 99), whose records were available in our healthcare center, were included in the study between 30 July and 30 August 2023.
2.1. Data Collection Tools
In our study, patients’ age, gender, occupation, educational status, marital status, diseases, drugs used were collected. Patients’ information and drugs used were obtained from the patients themselves or from those who constantly gave primary care to the patients and were scanned and controlled from the related e-Pulse database, the national health database. E-Pulse is a personal health record system integrated by the Turkish Ministry of Health into all healthcare institutions’ information systems. This innovative platform enables individuals to access a comprehensive range of medical information, including laboratory results, medical images, prescription and medication details, emergency information, diagnosis details, reports, and comprehensive health records, all of which pertain to their examinations. Accessible through both desktop and mobile platforms, e-Pulse empowers individuals to manage their healthcare effectively. Additionally, the platform allows users to securely share their medical records with healthcare professionals and family members, ensuring confidentiality within specified regulations [11]. Drug–drug interactions of these drugs and their appropriateness to the disease or age were assessed via a rational drug use web assistant [7] developed by the researchers. Reports of the web assistant were also evaluated by physicians in this study. Cancellation of PPI therapy in the prescription which was in the control of primary healthcare physicians was regulated by the physicians designing the study. However, regulation of psychiatric drugs such as quetiapine was performed by consulting the related department.
2.2. Rational Drug Use Web Assistant and Its Features
Before this study, an artificial intelligence-aided web application with rule-based algorithms was developed to simplify patient assessment based on age, medications, and chronic diseases in clinical practice [7]. This artificial intelligence system uses an extensive database to quickly retrieve interaction information and makes decisions based on predefined rules from pharmaceutical sources and the medical literature. It also offers access to the sources for decision justification.
In the database of the artificial intelligence-aided Fast&Rational rational drug use assistant (http://fastrational.com/ accessed on 30 July 2023), 6 guides (TIME-to-STOPP, AGS Beers 2019, US-FORTA, Stopp Criteria v2, EU (7) PIM, and PRISCUS 1.0 List) revealing the criteria of Potentially Inappropriate Medication (PIM) use in the elderly which are commonly used in today’s literature and health service presentation are used.
Before this web application, 430 active and frequently used oral drug agents (parenteral forms, suspended drugs, foreign drugs, and canceled drugs are not included) in Turkey and the 70 most common chronic diseases/medical conditions were identified. Three separate sheets were made with the Microsoft Excel 2021 program. Information on whether 430 drug agents are inappropriate in patients over the age of 65 was recorded in the first sheet, drug interactions were recorded in the second sheet, and drug–disease interaction tables were made in the last sheet. First, these 430 drug agents were screened with 6 PIM criteria. Additional dose information and duration of drug use in the criteria related to each drug agent were added as comments. Information about the source from which each output and comment was taken was also added. In the second stage, a table of interactions of these 430 drug agents was made and interaction information was scanned from drug prospectuses, pharmacology medical books, and related articles published in peer-reviewed journals. In the third stage, a drug–disease interaction table was made, and interaction information was searched from drug prospectuses, chronic disease guides, pharmacology medicine books, and articles published in peer-reviewed journals. According to these sources, interaction information was classified into 3 different categories as “risky (orange color)”, “contraindicated (red color)”, and “no warning was found”. Additional information about the interaction was added to the table along with the sources from which it was taken from as comments. Then, the algorithms of the tables which were prepared in Microsoft Excel 2021 (drug–age, drug–drug, drug–disease) were made by an expert artificial intelligence engineer using a rule-based artificial intelligence supported system. The web application interface was made with these algorithms. The web application’s interface design was developed with the Python version 3.10 programming language using the Streamlit Library.
Moreover, this web application is actively used in our clinic.
2.3. Cost Analysis
First of all, a cost-effectiveness analysis was performed between the manual approach, described as the traditional and gold standard method, in which the related guide, prospectus, and medical information based on current evidence were assessed and concluded by the physician, and our artificial intelligence-aided rational drug use web assistant including all related guides and prospectus information. Nursing home patients’ initial conditions managed by the traditional method before web assistant use were accepted as the basal level during the related polypharmacy process, and the state of “doing nothing”, in other words, no additional interference, used in cost-effectiveness analyses was defined as the alternative method [12] and considered in our study.
Potential polypharmacy costs were primarily collected by scanning the related literature [13,14,15], described and summarized (Figure 1) before the analysis of cost-effectiveness within the scope of this study.
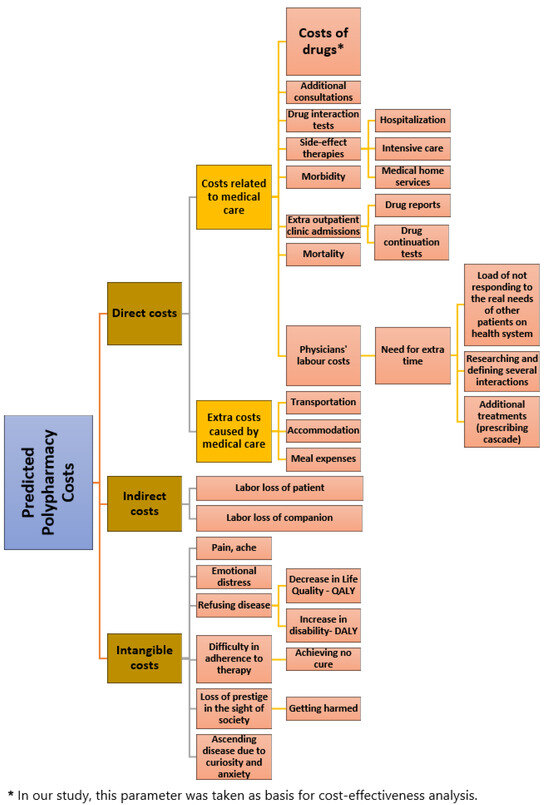
Figure 1.
Potential costs of polypharmacy.
Cost-effectiveness analysis was performed between the two methods (traditional method and web assistant method) in terms of the costs of drugs stated as the leading cause of costs related to medical care, regarding only direct costs among several potential cost items of polypharmacy. Therefore, all of the patients’ drugs obtained from the related patient files and their caregivers and confirmed in the e-Pulse national database were documented in Excel format. Prices of the related drugs were noted down and listed by specialists one by one according to the prices defined as the public price in Turkey and determined on a legal basis as cheaper than the retail price in the repayment cover. Because only the generic names of drugs were anonymized and given to the individuals who would note the related drug fees down and due to the abundance of drugs for patients, the drugs were conveyed regardless of their usage periods or doses. A drug was selected among those drugs whose generic names were given, and the average dose was based among all the doses of the drug selected as the most affordable one among all its equivalents in the market. It was considered that, for each drug, only one pack was used in a month and the total cost was obtained by calculating the minimum average costs. Thus, total costs were compared for the initial states of patients and the states as a result of drug regulation after web assistant use. Cost calculation was performed in currency, and effectiveness was measured with the frequency of exposure to polypharmacy, a quantitative medical outcome in our study, which is suitable for a general approach in these kinds of cost-effectiveness analyses.
2.4. Statistical Analysis
Statistical analysis of all data was performed with the SPSS 25.0 software program after combining it in a common database. For descriptive statistics, continuous variables were expressed in mean ± standard deviation and discrete data in numbers and percentile. Whether continuous variables were normally distributed or not and histogram graphs were evaluated with interpretations of Kolmogorov–Smirnov and Shapiro–Wilk tests. One sample t test was used to find out whether the mean value of a variable exhibited a difference according to a determined constant number. Correlation analysis was performed to determine the correlation between two or more variables and detect the power and direction of the correlation if available. The chi-square test was used for intergroup and intragroup comparisons of qualitative data. The McNemar test was used to analyze paired nominal data related to the polypharmacy status of nursing home patients before and after the assessment conducted through the web application. Confidence interval was determined as 95% for differences between groups, and p < 0.05 was accepted as the significant value.
3. Results
A total of 99 individuals staying in a nursing home were included in our study. The mean age of the patients was 79.81 ± 7.64 (min: 62, max: 99). Of the patients, 63.6% were female and 47.5% were widowed or divorced. Sociodemographic information of the patients is given in Table 1.

Table 1.
Sociodemographic information and disease status of patients.
In our study, 18.2% (n = 18) of the total number of patients were using fewer than 5 drugs, 69.7% (n = 69) were using 5–10 drugs, and 12.1% (n = 12) were using 11–14 drugs. Inappropriate drug use was detected in 81 individuals using five or more drugs and in 7 individuals using fewer than five drugs, which means 88.9% (n = 88) of the patients were exposed to polypharmacy.
The mean number of drugs used by the patients in our study was 6.96 ± 2.94. The highest number of drugs used was 14, and there was only one patient who had not been using any drugs. In addition, the number of patients’ diseases had been assessed and the mean number of diseases was calculated as 6.37 ± 2.97 (minimum: 0; maximum: 13).
In our study, drug–drug interaction and potentially inappropriate drug use above the age of 65 in our nursing home patients who had recently been recorded were determined with a rational drug use web assistant established by the researchers and used within the context of preventive healthcare services in our primary healthcare center.
3.1. Detailed Classification of Drug–Drug Interaction and Contraindicated Drugs
As a result of the assessment of drug–drug interaction with a rational drug use web assistant, potential risky drug–drug interaction was detected in 89.9% (n = 89) of the patients. Contraindicated drug–drug interaction was detected in 20.2% (n = 20) of the patients. When contraindicated drug interactions were assessed, an interaction with a minimum of two and a maximum of four active agents was detected. The number of patients who had contraindicated drug–drug interaction with two active agents was 14, and 71.4% (n = 10) of them had quetiapine drug interactions. Quetiapine drug interaction was monitored in one half and rasagiline drug interaction was monitored in the other half of the patients (n = 4) who had contraindicated drug–drug interaction with three active agents. In those who had contraindicated drug–drug interaction with four active agents (n = 2), quetiapine, rasagiline, and olanzapine drug interactions were observed.
3.2. Potentially Inappropriate Drug Use above the Age of 65
Potentially inappropriate drug use was detected in 86.9% (n = 86) of geriatric patients. Proton Pump Inhibitor (PPI) use was the most common with a rate of 64% (n = 55) among these patients. Potentially inappropriate drug use of quetiapine was reported in 31.4% (n = 27) of the patients.
According to the recommendations of the web assistant and the evaluation of our physicians, it was determined that a minimum of one and a maximum of three active agents must be removed from the drugs used in 58 (58.6%) patients. The related drugs were ceased in cooperation with the family physicians conducting the study and the physicians of the related departments they consulted. In this way, all contraindicated drug–drug interactions with the drugs planned to be taken out (p < 0.001) were removed, and potentially inappropriate drug use above the age of 65 was significantly decreased (p < 0.001) (Table 2). As a result, 12.2% (n = 83) of total active agents (n = 683) were able to be removed from the drug lists. On the other hand, the related web assistant recommended 13 patients to add PPI into their treatment plans. The recommendations were assessed by the physicians in this study and considered appropriate, and PPI was added to the treatment.

Table 2.
Number of patients’ drugs, total cost of drugs, number of drugs involved in inappropriate drug use above the age of 65, and number of drugs detected as red risk in web application per patient pre- and post-assessment via the “Artificial Intelligence-Supported Rational Drug Use Web Assistant”.
No significant difference was observed between the sociodemographic findings of patients (age, gender, marital status, educational status, and occupation) and the presence of drug–drug interactions and inappropriate drug use above the age of 65 (p > 0.05).
A significant difference was detected between the number of drugs used by patients before and after the assessment with the rational drug use web assistant and is given in Table 2.
The correlation of the number of diseases patients had and the number of drugs they used with the number of drugs before and after the assessment of the web application and costs of ceased drugs is given in Table 3.

Table 3.
Correlation between pre- and post-assessment medication use via the “Artificial intelligence-supported rational drug use web assistant”, patient disease count, and planned drug discontinuation costs.
3.3. Results of Cost-Effectiveness Analysis
The total medication cost of drugs used by the nursing home patients was calculated to be 115,232 Turkish Liras (TRY) (about USD 17,071 based on the real price and the currency, determined using legal regulations for the drugs) according to the total number of active agents (per pillbox and at the prevailing Social Security Institute public price). The direct cost of drugs planned to be ceased was calculated to be TRY 10,434 (USD 1545) in total (per pillbox and over public price), which accounts for 9.1% of all drugs used by all patients included in our study. On one hand, this extra cost stood for TRY 105 (USD 15) on average per patient. On the other hand, PPI addition was planned for 13 patients as a result of the web application’s suggestions, and the total cost was calculated to be TRY 825 (USD 122). The total cost obtained and the total cost as a result of the removal of the drugs that was predicted to decrease by the recommendation of the web assistant and physician’s decision were compared for the cost-effectiveness analysis. It was accordingly determined that drug costs decreased by a rate of 9.1% (p < 0.001) (Table 2), polypharmacy decreased by a rate of 19.2% in the total population, and the costs decreased by a rate of 21.6% in those with polypharmacy (p < 0.001) (Figure 2).
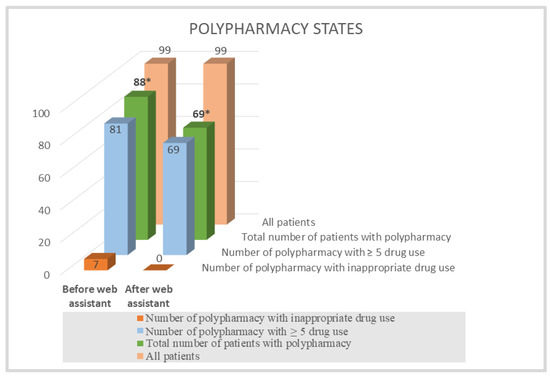
Figure 2.
Distributions of polypharmacy states before and after web assistant use in cost-effectiveness analysis. * A significant decrease was observed between polypharmacy states of nursing home patients before and after rational drug use web assistant use (p < 0.001).
4. Discussion
The increase in average lifespan and thereby the elderly population, the number of chronic diseases, and reasons such as natural disasters have recently increased the workload of a clinician and decreased the time to be spent on the patient [16]. This raises the importance and place of artificial intelligence and web assistant implementations in health in order to facilitate the jobs of clinicians [17]. Artificial intelligence implementations help the clinician in the processes of diagnosing diseases, predicting the prognoses of diseases, and deciding on the treatment [17]. These implementations are expected to help physicians in diagnosis, treatment, and follow-up processes rather than replace them [18,19]. There are some artificial intelligence implementations revealing drug–drug interactions [20,21,22]. There are also online websites facilitating physicians to prescribe elderly patients [23,24,25,26,27]. In our study, the drug use of nursing home patients recently recorded in a training family health center was assessed with a rational drug use web assistant we designed with the largest database in the literature. The presence of polypharmacy and risky drug–drug interactions were detected in a high majority of patients in our study with the help of this web application.
Most of the patients in our study had a drug use history with 5–10 drugs. In a study performed by Ozbek et al. to investigate adherence to treatment in 56 elderly patients staying in a nursing home, more than half of the patients were using five or more drugs [28]. According to a study performed by Wawruch et al. [29] on 600 patients at the age of 65 and above in Slovakia, the rate of polypharmacy was 60.3%. In a study performed by Onder et al. [30] on 4023 elderly patients staying in nursing homes in eight different European countries, the rate of polypharmacy was 74%. According to the findings in our study and the literature, it is obvious that polypharmacy is common among the elderly staying in nursing homes. When regulating a new treatment plan for these patients, it should be considered that elderly patients are in the vulnerable patient group and have several chronic diseases. It is also important to obtain information about the drugs they use. Regulating the treatment and nursing care plan [31] is of utmost importance for patients who face increased complexity due to polydrug use. In this regard, we can say that a rational drug use web application is an undeniable necessity. It is considered that not only will the patients be protected from several potential risks particularly caused by the side-effects of drugs but also the unnecessary use of the healthcare system will be prevented with this web application by easily controlling drugs and ensuring appropriate drug use.
The mean number of drugs used by the patients in our study was 6.96 ± 2.94. In a thesis study [32] assessing inappropriate drug use in 1263 elderly individuals, the mean number of drugs used by the patients was 6.10 ± 3.40. The mean number of drugs used by the patients was 5.4 ± 3.24 in a study performed on the elderly by Kitis et al. and 7 ± 3.60 in the study by Lee et al. [33,34]. Regarding the findings in our study and the literature, the mean number of drugs used by elderly patients indicates polypharmacy. Polypharmacy appears a crucial health problem in elderly patients. Controlling the drugs used by these patients and preventing unnecessary drug use are of great importance. Increasing the number of drugs used can increase the number of side-effects as well, and prescribing cascade may occur in geriatric patients. As this may cause significant health problems for elderly patients, the utilization of web applications for rational drug use seems important for the prevention of PIM.
When drug–drug interaction was evaluated with the rational drug use web assistant, potential risky drug–drug interaction was detected in the majority of patients and contraindicated drug–drug interaction was detected in about one-fifth of the patients. According to the assessments of contraindicated drug interactions in our study, drug interaction with a minimum of two and a maximum of four active agents was detected, and contraindicated drug–drug interactions with two active agents were mostly due to quetiapine. Quetiapine drug interaction was observed in one half and rasagiline drug interaction was observed in the other half of the patients who had contraindicated drug–drug interactions with three active agents. In those who had contraindicated drug–drug interaction with four active agents, quetiapine, rasagiline, and olanzapine drug interactions were observed. The most common disease in our nursing home population was hypertension followed by neuro-psychiatric disorders such as depression, dementia, and anxiety, which confirms that. In a study on elderly patients, it was revealed that the use of some drugs such as digoxin, beta blockers, diuretics, antidiabetics, anticoagulants, nonsteroidal analgesics, and psychiatric drugs increased particularly the side-effects and interactions [35]. In the literature, antidepressants and antipsychotics have been revealed to create high risks for drug interactions [36,37,38]. It has also been stated in the literature that antiepileptic and anticholinergic drugs, drugs suppressing the central nervous system, and acetylcholinesterase inhibitors create high risks for elderly patients in terms of drug interactions [39,40,41,42]. Findings in our study and the literature reveal that it is crucial to be careful, especially about the use of drugs affecting the central nervous system in elderly patients. The number of chronic diseases may be high in elderly patients, which may require the use of more than one drug. In this regard, it is especially crucial for family physicians who can approach their patients in a holistic way to follow up on their patients. It is possible to say that the web application we used in our study will provide great convenience for family physicians holistically approaching their patients in the assessment of drugs used.
When potentially inappropriate drug use above the age of 65 was assessed in our study, potentially inappropriate drug use was detected in most of the patients. PPI use was the most common among patients and quetiapine use was detected as potentially inappropriate drug use in about one-third of patients. In studies performed on the elderly in the literature, it is observed that PPIs are prescribed as off-label [43,44]. In a study performed by Çelikci on elderly patients in palliative care service, potentially inappropriate drugs among 564 used drugs were assessed according to the criteria of Beers and TIME-to-STOPP, and the most frequently used potentially inappropriate drug was found to be PPI in both criteria [45]. The web application we used in our study gave us the opportunity to assess potentially inappropriate drug use by age according to the criteria of TIME-to-STOPP, AGS Beers 2019, US-FORTA, Stopp/Start v2, EU(7)PIM, and Priscus 1.0 List. The most commonly used potentially inappropriate drug was PPI both in our study and in the literature [43,44,45,46]. While prescribing PPI to patients, other drugs used by the patients should also be evaluated, and it should be prescribed only if it has indications for patients. Inappropriate drug use is not only harmful to the health of patients but also increases the costs of health expenses, which appears a crucial problem. It is possible to say that starting web-assisted applications for rational drug use to prevent patients from inappropriate drug use in busy polyclinic conditions will be beneficial.
On the other hand, the desired results in the struggle against polypharmacy may not be generally achieved as the need for additional time to detect inappropriate drug use cannot be met due to patient density, and several drug interactions may not be considered due to the lack of knowledge or due to the fact that guide evaluation is performed or remembered in daily practice. As a result of the cost-effectiveness analysis, our web assistant, which we presented as the gold standard method in other studies by us and which was revealed as an alternative method with several detected advantages (2 times more inclusive and 60 times faster than the largest PIM criterion [7]) compared to the traditional manual methods, was revealed as a more cost-effective method compared with the alternative “doing nothing” used in cost-effectiveness analyses. Previous states of the related patient groups before they were registered in our training family health center support this detection. Likewise, although inappropriate drug use was presented by traditional methods in many health services, several inappropriate drug uses that could not be detected or interfered with were observed, as revealed in our study.
There was a positive correlation between the number of drugs involved in drug–drug interactions, the number of drugs involved in inappropriate drug use above the age of 65, total number of diseases, and the number of drugs used. In other words, as inappropriate drug use above the age of 65, the total number of diseases, and the number of drugs used increased, the number of drugs involved in drug–drug interactions increased in our study.
There was no significant correlation between the number of drugs detected as red risk in the web application and the total number of diseases; however, there was a positive significant correlation with the number of drugs used. Drugs detected as red risk represented those with contraindications. According to that result, it was not the number of diseases but the number of drugs used that increased the risk of use of drugs with contraindications in patients. In this regard, the importance of searching the interactions between the drugs used while regulating the treatments of patients comes out. It is obvious that the rational drug use web assistant we used easily met this need.
While there was no significant correlation between the drug costs planned to be ceased with the web application, the number of diseases, the number of drugs used, and the number of drugs involved in drug–drug interactions, there was a positive significant correlation with the number of drugs involved in inappropriate drug use above the age of 65. It is evident that inappropriate drug use above the age of 65 increases drug costs here, which comes out as an important issue. It can be seen that, when reflected in the total geriatric population in Turkey, this additional cost would make a huge amount. While such a high amount appears when only the direct costs of drugs are considered, it is an unforgettable fact that these numbers will increase more when we consider additional health problems caused by the potential side-effects of these drugs and hospital stays, even intensive care stays depending on these problems. In addition to all of these, the condition may become more nonignorable as it will cause loss of labor and inefficient use of limited resources. Therefore, a rational drug use web assistant is needed to decrease inappropriate drug use by rapidly detecting inappropriate drug use above the age of 65 even for the decrease of these costs only, and it has been well understood once again that the use of this web assistant by all healthcare systems is a necessity.
Limitations of the Study
Inappropriateness of some drug agents in advanced age depends on the dose and exposure time of the drug agent. For example, use of PPIs for more than 8 weeks is inappropriate according to the inappropriateness criteria of most drugs. In our study, statistical analysis was performed assuming that patients in our sample had been using their drugs for a long time, which is among the limitations of our study. Additionally, the number of nursing home patients in our study is not sufficient to ensure broad generalizations for the broader population. Nevertheless, our web-based assistant holds the potential to become a pivotal tool for optimizing patient treatments. Follow-ups of the related population must be performed in the long term in order to reveal the health outcomes more clearly; however, the health outcomes in our study could not be assessed with cost-effectiveness analyses such as QALY (Quality Adjusted Life Year) and DALY (Disability Adjusted Life Years), which is another limitation of our study. Instead of that, costs of the drugs and polypharmacy outcomes were used in cost-effectiveness analyses in our study.
5. Conclusions
When drug use of patients in nursing homes was assessed with a rational drug use web assistant in our study it was concluded that most of the patients had polypharmacy and potential drug–drug interaction. In addition, there was inappropriate drug use in most of the patients above the age of 65, and it was detected that this increased drug costs, which appears a crucial problem. A significant decline in terms of polypharmacy was observed with the regulation after the related recommendations of the web assistant and the physician’s decision. Therefore, about one-third of patients in whom polypharmacy was detected were kept from several potential side-effects and costs (direct, indirect, or intangible) of polypharmacy. It was concluded in our study that the discontinuation of drugs due to inappropriate drug use in a group including about 100 individuals could directly decrease drug costs by a rate of 10%. According to this, it was observed that the web assistant was more cost-effective than the traditional manual calculation method. Moreover, the total number of active agents used by all patients revealed that no contraindicated drug–drug interaction remained after the number of active agents was decreased by a rate of 12.15% (n: 83) following the web assistant and the physician’s decision.
In this specific context, the web application, supported by artificial intelligence and developed by researchers with the primary goal of promoting rational drug utilization, has been recognized for its ability to offer substantial convenience to physicians.
In addition, it has been well understood once again in this study that significant responsibilities fall upon family physicians who can deal with all health problems and medications of patients, approach them in a holistic way, provide care coordination, and base on quaternary prevention.
Moreover, it is considered that this study will raise awareness about the rational drug use web assistant to physicians, guide large masses by encouraging the use of this application in their clinics, and contribute to the proliferation of its national and international use for its ease of application.
Author Contributions
All authors made critical contributions to this study. T.Y. and Ş.C. designed the conceptualization and details of the study. T.Y., Ş.C. and Ş.H.A. provided the data. Ş.C., Ş.H.A. and T.E.Y. investigated the data and ensured accuracy and exclusions according to the study criteria. The analysis was carried out by T.Y., Ş.C. and T.E.Y., T.Y. and T.E.Y. interpreted the analysis and wrote the paper. T.Y., Ş.C., Ş.H.A. and T.E.Y. contributed to the critical evaluation, supervision, and revision of the manuscript. T.Y. and T.E.Y. developed the final version. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki. Ethics committee approval was obtained from the Clinical Research Ethics Committee of Ankara Bilkent City Hospital (protocol code E1-23-3721 and date of approval 21 June 2023), and research permission regarding performing the study in primary healthcare institutions was obtained from the Institutional Review Board of Ankara Provincial Health Directorate Presidency of Public Health Services (protocol code E-51381736-771-221267198 and date of permission 27 July 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study. The data are not publicly available due to ethical and legal considerations.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author. The data are not publicly available due to ethical and legal issues.
Acknowledgments
We extend our gratitude to Fatih Çağatay Akyön, a graduate of the Faculty of Informatics at Middle East Technical University, for his valuable contributions and technical support in the development of the Fast & Rational artificial intelligence-aided web assistant. We would also like to thank Yakup Kırtel and his team for their great help and attention in the calculations of drug costs.
Conflicts of Interest
The authors declare no conflict of interest.
References
- T.C. Sağlık Bakanlığı Temel Sağlık Hizmetleri Genel Müdürlüğü. Birinci Basamak Sağlık Hizmetlerinde Çalışan Hekimler için Yaşlı Sağlığı Tanı ve Tedavi Rehberi Ankara. 2010. Available online: https://hsgm.saglik.gov.tr/depo/birimler/kronik-hastaliklar-ve-yasli-sagligi-db/Dokumanlar/Kitaplar/Yasli_Sagligi_Tani_Tedavi_Rehberi.pdf (accessed on 16 August 2023).
- Rochon, P.A.; Schmader, K.E. Drug Prescribing For Older Adults. 2021. Available online: https://www.uptodate.com/contents/drug-prescribing-for-older-adults (accessed on 1 October 2023).
- Krüger, C.; Schäfer, I.; Bussche, H.V.D.; Bickel, H.; Dreischulte, T.; Fuchs, A.; König, H.H.; Maier, W.; Mergenthal, K.; Riedel-Heller, S.G.; et al. Comparison of FORTA, PRISCUS and EU(7)-PIM lists on identifying potentially inappropriate medication and its impact on cognitive function in multimorbid elderly German people in primary care: A multicentre observational study. BMJ Open 2021, 11, e050344. [Google Scholar] [CrossRef] [PubMed]
- Arslan, Ş.E.; Dağcıoğlu, B.F. Is there a significant clinical difference between 2015 and 2019 AGS beers criteria in terms of inappropriate drug use: A cross-sectional study. Ank. Med. J. 2020, 20, 1027–1040. [Google Scholar] [CrossRef]
- Halli-Tierney, A.D.; Scarbrough, C.; Carroll, D. Polypharmacy: Evaluating risks and deprescribing. Am. Fam. Physician 2019, 100, 32–38. [Google Scholar] [PubMed]
- Eyigör, S.; Kutsal, Y.G. Polypharmacy in the elderly: To prescribe, or not prescribe “that is the question”. Turk. J. Geriatr. 2012, 15, 445–454. [Google Scholar]
- Akyon, S.H.; Akyon, F.C.; Yılmaz, T.E. Artificial intelligence-supported web application design and development for reducing polypharmacy side effects and supporting rational drug use in geriatric patients. Front. Med. 2023, 10, 1029198. [Google Scholar] [CrossRef]
- Colley, C.A.; Lucas, L.M. Polypharmacy: The cure becomes the disease. J. Gen. Int. Med. 1993, 8, 278–283. [Google Scholar] [CrossRef]
- Gokula, M.; Holmes, H.M. Tools to reduce polypharmacy. Clin. Geriatr. Med. 2012, 28, 323–341. [Google Scholar] [CrossRef]
- Pesante-Pinto, J.L. Clinical pharmacology and the risks of polypharmacy in the geriatric patient. Phys. Med. Rehabilit. Clin. N. Am. 2017, 28, 739–746. [Google Scholar] [CrossRef]
- Turkish National Personal Health Record System: E-Pulse. Available online: https://wsa-global.org/winner/turkish-national-personal-health-record-system-e-pulse/ (accessed on 1 October 2023).
- Muennig, P.; Khan, K. Designing and Conducting Cost-Effectiveness Analyses in Medicine and Health Care, 1st ed.; Jossey-Bass: San Francisco, CA, USA, 2002; pp. 1–384. [Google Scholar]
- Balçık, P.Y.; Şahin, B. Sağlık hizmetlerinde maliyet etkililik analizi ve karar analizi. Hacet. Sağlık Idaresi Derg. 2013, 16, 121–134. [Google Scholar]
- Marshall, D.A.; Douglas, P.R.; Drummond, M.F.; Torrance, G.W.; Macleod, S.; Manti, O.; Cheruvu, L.; Corvari, R. Guidelines for conducting pharmaceutical budget impact analysis for submission to public drug plans in Canada. Pharmacoeconomics 2008, 26, 477–495. [Google Scholar] [CrossRef]
- Özgen, H.; Tatar, M. Sağlık sektöründe bir verimlilik değerlendirme tekniği olarak maliyet etkililik analizi ve Türkiye’de durum. Hacet. Sağlık İdaresi Derg. 2007, 10, 109–137. [Google Scholar]
- Akalın, B.; Veranyurt, Ü. Sağlık hizmetleri ve yönetiminde yapay zekâ. Acta Infologica 2021, 5, 231–240. [Google Scholar] [CrossRef]
- Çilhoroz, Y. Yapay zekâ: Sağlık hizmetlerinden uygulamalar. Ank. Hacı Bayram Veli Üniversitesi İktisadi Ve İdari Bilim. Fakültesi Derg. 2021, 23, 573–588. [Google Scholar]
- Cakir, S.S.; Otunctemur, A. Artificial intelligence in medicine. Eur. Arch. Med. Res. 2018, 34 (Suppl. S1), S1–S3. [Google Scholar] [CrossRef]
- Babalik, A.; Güler, İ. Boğaz enfeksiyonlarının teşhis ve tedavisinde uzman sistem kullanımı. J. Technol.-Online 2007, 6, 109–119. [Google Scholar]
- Farmantek. Farmantek Rational Drug Use Assistant. Available online: http://farmantek.herokuapp.com/ (accessed on 1 October 2023).
- Medscape, Drug Interaction Checker. Available online: https://reference.medscape.com/drug-interactionchecker (accessed on 1 October 2023).
- Vademecum Api. Available online: https://www.vademecumonline.com.tr/site/vademecum-api (accessed on 1 October 2023).
- Niehoff, K.M.; Rajeevan, N.; Charpentier, P.A.; Miller, P.L.; Goldstein, M.K.; Fried, T.R. Development of the Tool to Reduce Inappropriate Medications (TRIM): A clinical decision support system to ımprove medication prescribing for older adults. Pharmacotherapy 2016, 36, 694–701. [Google Scholar] [CrossRef]
- MedStopper. Available online: http://medstopper.com (accessed on 1 October 2023).
- Canadian Medication Appropriateness and Deprescribing Network. Available online: https://www.deprescribingnetwork.ca/ (accessed on 1 October 2023).
- Prescqipp, Community Interest Company. Available online: https://www.prescqipp.info/ (accessed on 1 October 2023).
- MedSafer, Working Towards Safer Prescribing. Available online: https://www.medsafer.org/ (accessed on 1 October 2023).
- Özbek, S.; Kaya, E.; Tekin, A.; Doğan, Ş. Yaşlılarda tedaviye uyum. Turk. J. Geriatr. 2006, 9, 177–181. [Google Scholar]
- Wawruch, M.; Zikavska, M.; Wsolova, L.; Kuzelova, M.; Tisonova, J.; Gajdosik, J.; Urbanek, K.; Kristova, V. Polypharmacy in elderly hospitalized patients in Slovakia. Pharm. World Sci. 2008, 30, 235–242. [Google Scholar] [CrossRef]
- Onder, G.; Liperoti, R.; Fialova, D.; Topinkova, E.; Tosato, M.; Danese, P.; Gallo, P.F.; Carpenter, L.; Finne-Soveri, H.; Gindin, J.; et al. Polypharmacy in nursing home in Europe: Results from the SHELTER study. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 698–704. [Google Scholar] [CrossRef]
- Hidayat, A.A.A.; Uliyah, M.; Haryanti, T. Mobile nursing care plan information system for nursing service in hospitals. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 13–19. [Google Scholar]
- Bay, İ. Elderly of İnappropriate Drug Use 2012 Beers Criteria and Stopper Version 2 Evaluation Criteria. Ph.D. Thesis, İstanbul University, İstanbul, Türkiye, 2015. [Google Scholar]
- Kitiş, Y.; Terzi, H. The beers criteria: A guide for the prevention of inappropriate drug utilization in the elderly individuals: Review. Turk. Klin. J. Nurs. 2016, 8, 162–175. [Google Scholar] [CrossRef]
- Lee, D.; Martini, N.; Moyes, S.; Hayman, K.; Zolezzi, M.; Kerse, N. Potentially inappropriate medication use: The Beers’ Criteria used among older adults with depressive symptoms. J. Prim. Health Care 2013, 5, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Eckardt, R.; Steinhagen-Thiessen, E.; Kämpfe, S.; Buchmann, N. Polypharmazie und Arzneimitteltherapiesicherheit im Alter. Z. Für Gerontol. Und Geriatr. 2014, 47, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Schellander, R.; Donnerer, J. Antidepressants: Clinically relevant drug interactions to be considered. Pharmacology 2010, 86, 203–215. [Google Scholar] [CrossRef]
- Vieweg, W.V.R.; Wood, M.A.; Fernandez, A.; Beatty-Brooks, M.; Hasnain, M.; Pandurangi, A.K. Proarrhythmic risk with antipsychotic and antidepressant drugs: Implications in the elderly. Drugs Aging 2009, 26, 997–1012. [Google Scholar] [CrossRef]
- Urichuk, L.; Prior, T.I.; Dursun, S.; Baker, G. Metabolism of atypical antipsychotics: Involvement of cytochrome p450 enzymes and relevance for drug–drug interactions. Curr. Drug Metab. 2008, 9, 410–418. [Google Scholar] [CrossRef]
- Mallet, L.; Spinewine, A.; Huang, A. The challenge of managing drug interactions in elderly people. Lancet 2007, 370, 185–191. [Google Scholar] [CrossRef]
- Hanlon, J.T.; Schmader, K.E. Drug–drug interactions in older adults: Which ones matter? Am. J. Geriatr. Pharmacother. 2005, 3, 61–63. [Google Scholar] [CrossRef]
- Campbell, N.; Boustani, M.; Limbil, T.; Ott, C.; Fox, C.; Maidment, I.; Schubert, C.C.; Munger, S.; Fick, D.; Miller, D.; et al. The cognitive impact of anticholinergics: A clinical review. Clin. Interv. Aging 2009, 4, 225–233. [Google Scholar]
- Taipale, H.T.; Hartikainen, S.; Bell, J.S. A comparison of four methods to quantify the cumulative effect of taking multiple drugs with sedative properties. Am. J. Geriatr. Pharmacother. 2010, 8, 460–471. [Google Scholar] [CrossRef]
- Clyne, B.; Smith, S.M.; Hughes, C.M.; Boland, F.; Bradley, M.C.; Cooper, J.A.; Fahey, T. Effectiveness of a multifaceted ıntervention for potentially ınappropriate prescribing in older patients in primary care: A cluster-randomized controlled trial (OPTI SCRIPT Study). Ann. Fam. Med. 2015, 13, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Demircan, C.; Hasanzade, U. Polypharmacy and potential inappropriate drug use in the elderly admitted to the general internal medicine outpatient clinic. Turk. J. Intern. Med. 2021, 3, 46–48. [Google Scholar] [CrossRef]
- Çelikçi, S. Palyatif bakım servisindeki yaşlı hastalarda polifarmasi ve uygunsuz ilaç kullanımının beers ve TIME-to-STOP kriterlerine göre değerlendirilmesi. Uludağ Üniversitesi Tıp Fakültesi Derg. 2021, 47, 405–409. [Google Scholar] [CrossRef]
- Alharbi, S.A.; Alfadl, A.A.; Almogbel, Y. Polypharmacy and inappropriate prescribing in elderly patients: A retrospective study at Buriadah Central Hospital, Saudi Arabia. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 3325–3333. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).