Autoantibodies and Clinical Correlations in Polish Systemic Sclerosis Patients: A Cross-Sectional Study
Abstract
1. Introduction
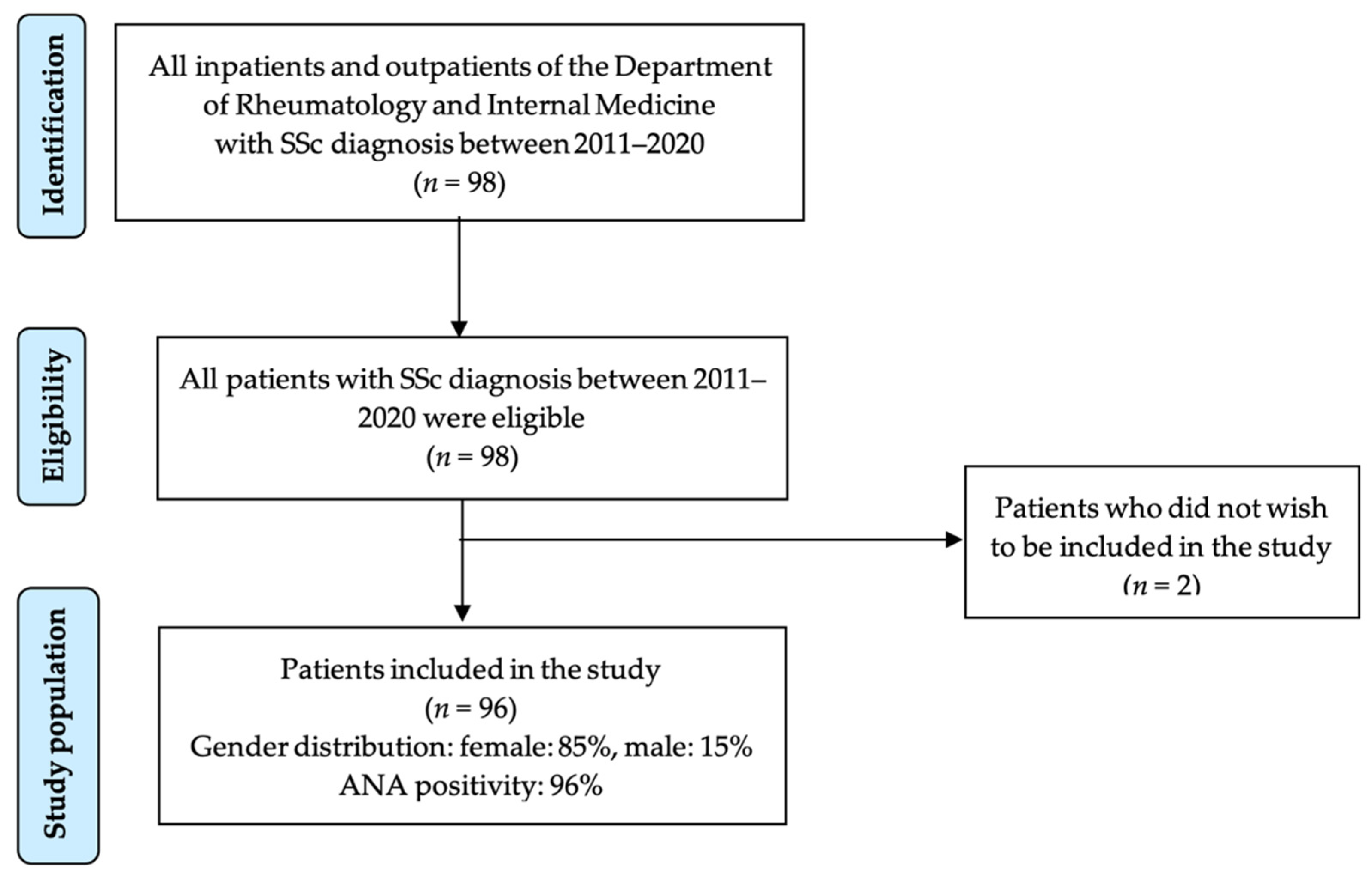
2. Materials and Methods
3. Results
3.1. Population Characteristics
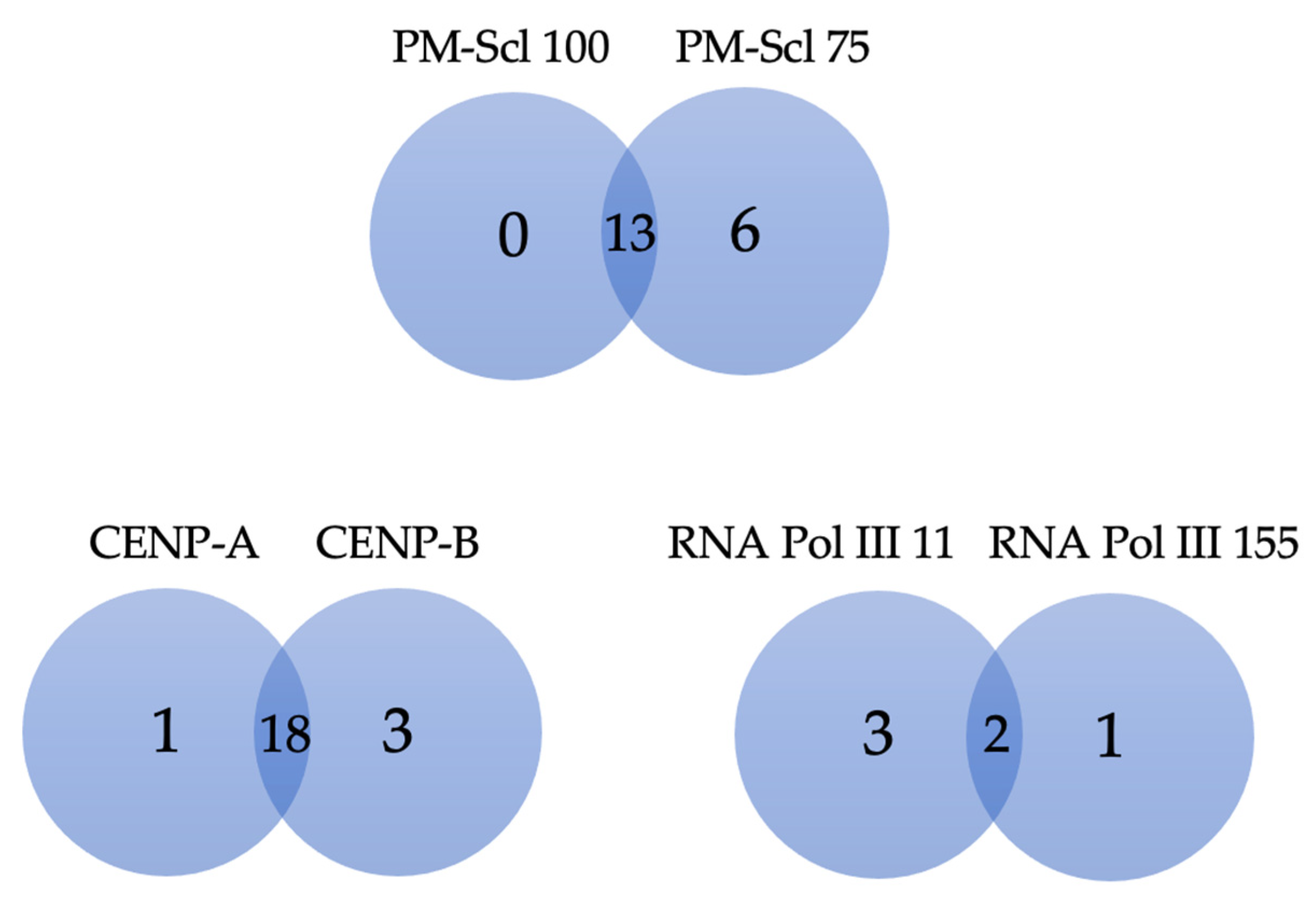
3.2. SSc Specific Autoantibodies and Clinical Associations in the Studied Population
3.3. Sensitivity of Systemic Sclerosis Profile vs. ANA Profile
3.4. SSc-Patients Negative for ATA, ACA, and RNAP3 (Triple-Negative)
4. Discussion
4.1. Anti-Topoisomerase I (Anti-Scl-70) Antibodies (ATA)
4.2. Anti-Centromere Antibodies (ACA)
4.3. Anti-RNA Polymerase III Antibodies (RNAP3)
4.4. Anti-Th/To Antibodies
4.5. Anti-Fibrillarin Antibodies (Anti-U3RNP, AFA)
4.6. Anti-PM-Scl Antibodies
4.7. Anti-Ku Antibodies
4.8. Anti-NOR90 (Anti-hUBF) Antibodies
4.9. Anti-PDGFR Antibodies
4.10. Anti-Ro-52 Antibodies
4.11. Clinical Usefulness of Systemic Sclerosis Profile (SSP)
4.12. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gabrielli, A.; Avvedimento, E.V.; Krieg, T. Scleroderma. N. Engl. J. Med. 2009, 360, 1989–2003. [Google Scholar] [CrossRef] [PubMed]
- LeRoy, E.C.; Black, C.; Fleischmajer, R.; Jablonska, S.; Krieg, T.; Medsger, T.A., Jr.; Rowell, N.; Wollheim, F. Scleroderma (systemic sclerosis): Classification, subsets and pathogenesis. J. Rheumatol. 1988, 15, 202–205. [Google Scholar] [PubMed]
- Masi, A.T. Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1980, 23, 581–590. [Google Scholar] [CrossRef] [PubMed]
- LeRoy, E.C.; Medsger, T.A., Jr. Criteria for the classification of early systemic sclerosis. J. Rheumatol. 2001, 28, 1573–1576. [Google Scholar]
- Spencer-Green, G.; Alter, D.; Welch, H.G. Test performance in systemic sclerosis: Anti-centromere and anti-Scl-70 antibodies. Am. J. Med. 1997, 103, 242–248. [Google Scholar] [CrossRef]
- Villalta, D.; Morozzi, G.; Tampoia, M.; Alpini, C.; Brusca, I.; Salgarolo, V.; Papisch, W.; Bizzaro, N. Antibodies to fibrillarin, PM-Scl and RNA polymerase III detected by ELISA assays in patients with systemic sclerosis. Clin. Chim. Acta 2010, 411, 710–713. [Google Scholar] [CrossRef]
- Bonroy, C.; Van Praet, J.; Smith, V.; Van Steendam, K.; Mimori, T.; Deschepper, E.; Deforce, D.; Devreese, K.; De Keyser, F. Optimization and diagnostic performance of a single multiparameter lineblot in the serological workup of systemic sclerosis. J. Immunol. Methods 2012, 379, 53–60. [Google Scholar] [CrossRef]
- Villalta, D.; Imbastaro, T.; Di Giovanni, S.; Lauriti, C.; Gabini, M.; Turi, M.C.; Bizzaro, N. Diagnostic accuracy and predictive value of extended autoantibody profile in systemic sclerosis. Autoimmun. Rev. 2012, 12, 114–120. [Google Scholar] [CrossRef]
- Puszczewicz, M. Antinuclear antibodies—What to do with them? Reumatologia 2013, 51, 172–178. [Google Scholar] [CrossRef]
- Peterson, L.K.; Jaskowski, T.D.; Mayes, M.D.; Tebo, A.E. Detection of anti-U3-RNP/fibrillarin IgG antibodies by line immunoblot assay has comparable clinical significance to immunoprecipitation testing in systemic sclerosis. Immunol. Res. 2016, 64, 483–488. [Google Scholar] [CrossRef]
- Wielosz, E.; Dryglewska, M.; Majdan, M. Serological profile of patients with systemic sclerosis. Adv. Hyg. Exp. Med. 2014, 68, 987–991. [Google Scholar] [CrossRef] [PubMed]
- Van den Hoogen, F.; Khanna, D.; Fransen, J.; Johnson, S.R.; Baron, M.; Tyndall, A.; Matucci-Cerinic, M.; Naden, R.P.; Medsger, T.A., Jr.; Carreira, P.E.; et al. 2013 classification criteria for systemic sclerosis: An American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum. 2013, 65, 2737–2747. [Google Scholar] [CrossRef] [PubMed]
- Walker, U.A.; Tyndall, A.; Czirjak, L.; Denton, C.; Farge-Bancel, D.; Kowal-Bielecka, O.; Muller-Ladner, U.; Bocelli-Tyndall, C.; Matucci-Cerinic, M. Clinical risk assessment of organ manifestations in systemic sclerosis: A report from the EULAR Scleroderma Trials And Research group database. Ann. Rheum. Dis. 2007, 66, 754–763. [Google Scholar] [CrossRef] [PubMed]
- Graf, S.W.; Hakendorf, P.; Lester, S.; Patterson, K.; Walker, J.G.; Smith, M.D.; Ahern, M.J.; Roberts-Thomson, P.J. South Australian Scleroderma Register: Autoantibodies as predictive biomarkers of phenotype and outcome. Int. J. Rheum. Dis. 2012, 15, 102–109. [Google Scholar] [CrossRef]
- Mehra, S.; Walker, J.; Patterson, K.; Fritzler, M.J. Autoantibodies in systemic sclerosis. Autoimmun. Rev. 2013, 12, 340–354. [Google Scholar] [CrossRef] [PubMed]
- Mierau, R.; Moinzadeh, P.; Riemekasten, G.; Melchers, I.; Meurer, M.; Reichenberger, F.; Buslau, M.; Worm, M.; Blank, N.; Hein, R.; et al. Frequency of disease-associated and other nuclear autoantibodies in patients of the German Network for Systemic Scleroderma: Correlation with characteristic clinical features. Arthritis Res. Ther. 2011, 13, R172. [Google Scholar] [CrossRef]
- Rodriguez-Reyna, T.S.; Hinojosa-Azaola, A.; Martinez-Reyes, C.; Nunez-Alvarez, C.A.; Torrico-Lavayen, R.; Garcia-Hernandez, J.L.; Cabiedes-Contreras, J. Distinctive autoantibody profile in Mexican Mestizo systemic sclerosis patients. Autoimmunity 2011, 44, 576–584. [Google Scholar] [CrossRef]
- Hanke, K.; Dahnrich, C.; Bruckner, C.S.; Huscher, D.; Becker, M.; Jansen, A.; Meyer, W.; Egerer, K.; Hiepe, F.; Burmester, G.R.; et al. Diagnostic value of anti-topoisomerase I antibodies in a large monocentric cohort. Arthritis Res. Ther. 2009, 11, R28. [Google Scholar] [CrossRef]
- Mendes, C.; Viana, V.S.T.; Pasoto, S.G.; Leon, E.P.; Bonfa, E.; Sampaio-Barros, P.D. Clinical and laboratory features of African-Brazilian patients with systemic sclerosis. Clin. Rheumatol. 2020, 39, 9–17. [Google Scholar] [CrossRef]
- Liaskos, C.; Marou, E.; Simopoulou, T.; Barmakoudi, M.; Efthymiou, G.; Scheper, T.; Meyer, W.; Bogdanos, D.P.; Sakkas, L.I. Disease-related autoantibody profile in patients with systemic sclerosis. Autoimmunity 2017, 50, 414–421. [Google Scholar] [CrossRef]
- Markusse, I.M.; Meijs, J.; de Boer, B.; Bakker, J.A.; Schippers, H.P.C.; Schouffoer, A.A.; Ajmone Marsan, N.; Kroft, L.J.M.; Ninaber, M.K.; Huizinga, T.W.J.; et al. Predicting cardiopulmonary involvement in patients with systemic sclerosis: Complementary value of nailfold videocapillaroscopy patterns and disease-specific autoantibodies. Rheumatology 2017, 56, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Tahiat, A.; Allam, I.; Abdessemed, A.; Mellal, Y.; Nebbab, R.; Ladjouze-Rezig, A.; Djidjik, R. Autoantibody profile in a cohort of Algerian patients with systemic sclerosis. Ann. Biol. Clin. 2020, 78, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, M.; Mertens, B.J.A.; Bakker, J.A.; Ninaber, M.K.; Ajmone Marsan, N.; van der Helm-van Mil, A.H.M.; Scherer, H.U.; Huizinga, T.W.J.; de Vries-Bouwstra, J.K. To what extent do autoantibodies help to identify high-risk patients in systemic sclerosis? Clin. Exp. Rheumatol. 2018, 36 (Suppl. S113), 109–117. [Google Scholar] [PubMed]
- Czompoly, T.; Simon, D.; Czirjak, L.; Nemeth, P. Anti-topoisomerase I autoantibodies in systemic sclerosis. Autoimmun. Rev. 2009, 8, 692–696. [Google Scholar] [CrossRef]
- Weiner, E.S.; Earnshaw, W.C.; Senecal, J.L.; Bordwell, B.; Johnson, P.; Rothfield, N.F. Clinical associations of anticentromere antibodies and antibodies to topoisomerase I. A study of 355 patients. Arthritis Rheum. 1988, 31, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Priora, M.; Manetta, T.; Scarati, M.; Parisi, S.; Lagana, A.; Peroni, C.L.; Bruzzone, M.; Borrelli, R.; Rende, M.; Mengozzi, G.; et al. Serological and clinical profile of systemic sclerosis: Analysis in a cohort of patients from a single center in Northern Italy. G. Ital. Derm. Venereol. 2018, 153, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Solomon, J.J.; Olson, A.L.; Fischer, A.; Bull, T.; Brown, K.K.; Raghu, G. Scleroderma lung disease. Eur. Respir. Rev. Off. J. Eur. Respir. Soc. 2013, 22, 6–19. [Google Scholar] [CrossRef]
- Wells, A.U. High-resolution computed tomography and scleroderma lung disease. Rheumatol. 2008, 47 (Suppl. S5), v59–v61. [Google Scholar] [CrossRef]
- Mahler, M.; You, D.; Baron, M.; Taillefer, S.S.; Hudson, M.; Fritzler, M.J. Anti-centromere antibodies in a large cohort of systemic sclerosis patients: Comparison between immunofluorescence, CENP-A and CENP-B ELISA. Clin. Chim. Acta 2011, 412, 1937–1943. [Google Scholar] [CrossRef]
- Russo, K.; Hoch, S.; Dima, C.; Varga, J.; Teodorescu, M. Circulating anticentromere CENP-A and CENP-B antibodies in patients with diffuse and limited systemic sclerosis, systemic lupus erythematosus, and rheumatoid arthritis. J. Rheumatol. 2000, 27, 142–148. [Google Scholar]
- Miyawaki, S.; Asanuma, H.; Nishiyama, S.; Yoshinaga, Y. Clinical and serological heterogeneity in patients with anticentromere antibodies. J. Rheumatol. 2005, 32, 1488–1494. [Google Scholar] [PubMed]
- Hudson, M.; Mahler, M.; Pope, J.; You, D.; Tatibouet, S.; Steele, R.; Baron, M.; Fritzler, M. Clinical correlates of CENP-A and CENP-B antibodies in a large cohort of patients with systemic sclerosis. J. Rheumatol. 2012, 39, 787–794. [Google Scholar] [CrossRef] [PubMed]
- Bunn, C.C.; Denton, C.P.; Shi-Wen, X.; Knight, C.; Black, C.M. Anti-RNA polymerases and other autoantibody specificities in systemic sclerosis. Br. J. Rheumatol. 1998, 37, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Meyer, O.; De Chaisemartin, L.; Nicaise-Roland, P.; Cabane, J.; Tubach, F.; Dieude, P.; Hayem, G.; Palazzo, E.; Chollet-Martin, S.; Kahan, A.; et al. Anti-RNA polymerase III antibody prevalence and associated clinical manifestations in a large series of French patients with systemic sclerosis: A cross-sectional study. J. Rheumatol. 2010, 37, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Nikpour, M.; Hissaria, P.; Byron, J.; Sahhar, J.; Micallef, M.; Paspaliaris, W.; Roddy, J.; Nash, P.; Sturgess, A.; Proudman, S.; et al. Prevalence, correlates and clinical usefulness of antibodies to RNA polymerase III in systemic sclerosis: A cross-sectional analysis of data from an Australian cohort. Arthritis Res. Ther. 2011, 13, R211. [Google Scholar] [CrossRef]
- Satoh, T.; Ishikawa, O.; Ihn, H.; Endo, H.; Kawaguchi, Y.; Sasaki, T.; Goto, D.; Takahashi, K.; Takahashi, H.; Misaki, Y.; et al. Clinical usefulness of anti-RNA polymerase III antibody measurement by enzyme-linked immunosorbent assay. Rheumatology 2009, 48, 1570–1574. [Google Scholar] [CrossRef]
- Gargiulo, M.L.A.; Perez, N.; Khoury, M.; Buhl, M.; Suarez, L.; Sarano, J.; Montoya, F.; Bazzalo, I.; Navarro, S.; Pendon, G.; et al. Anti-RNA Polymerase III Antibodies in Systemic Sclerosis: Multicentric Study from Argentina. Reum. Clin. 2021, 18, 368–373. [Google Scholar] [CrossRef]
- Hesselstrand, R.; Scheja, A.; Wuttge, D.M. Scleroderma renal crisis in a Swedish systemic sclerosis cohort: Survival, renal outcome, and RNA polymerase III antibodies as a risk factor. Scand. J. Rheumatol. 2012, 41, 39–43. [Google Scholar] [CrossRef]
- Nihtyanova, S.I.; Denton, C.P. Autoantibodies as predictive tools in systemic sclerosis. Nat. Rev. Rheumatol. 2010, 6, 112–116. [Google Scholar] [CrossRef]
- Ceribelli, A.; Cavazzana, I.; Franceschini, F.; Airo, P.; Tincani, A.; Cattaneo, R.; Pauley, B.A.; Chan, E.K.; Satoh, M. Anti-Th/To are common antinucleolar autoantibodies in Italian patients with scleroderma. J. Rheumatol. 2010, 37, 2071–2075. [Google Scholar] [CrossRef]
- Hamaguchi, Y.; Hasegawa, M.; Fujimoto, M.; Matsushita, T.; Komura, K.; Kaji, K.; Kondo, M.; Nishijima, C.; Hayakawa, I.; Ogawa, F.; et al. The clinical relevance of serum antinuclear antibodies in Japanese patients with systemic sclerosis. Br. J. Dermatol. 2008, 158, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Mitri, G.M.; Lucas, M.; Fertig, N.; Steen, V.D.; Medsger, T.A., Jr. A comparison between anti-Th/To- and anticentromere antibody-positive systemic sclerosis patients with limited cutaneous involvement. Arthritis Rheum. 2003, 48, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Gliddon, A.E.; Dore, C.J.; Dunphy, J.; Betteridge, Z.; McHugh, N.J.; Maddison, P.J.; Group, Q.T.S. Antinuclear antibodies and clinical associations in a british cohort with limited cutaneous systemic sclerosis. J. Rheumatol. 2011, 38, 702–705. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, S.; Sawada, J.; Saito, T.; Katayama, T.; Fujishiro, D.; Nishino, I.; Hasebe, N. [A case of anti-Th/To antibody-positive systemic sclerosis with muscle symptoms and interstitial pneumonia]. Rinsho Shinkeigaku 2021, 61, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Tormey, V.J.; Bunn, C.C.; Denton, C.P.; Black, C.M. Anti-fibrillarin antibodies in systemic sclerosis. Rheumatology 2001, 40, 1157–1162. [Google Scholar] [CrossRef]
- Tall, F.; Dechomet, M.; Riviere, S.; Cottin, V.; Ballot, E.; Tiev, K.P.; Montin, R.; Morin, C.; Chantran, Y.; Grange, C.; et al. The Clinical Relevance of Antifibrillarin (anti-U3-RNP) Autoantibodies in Systemic Sclerosis. Scand. J. Immunol. 2017, 85, 73–79. [Google Scholar] [CrossRef]
- Aggarwal, R.; Lucas, M.; Fertig, N.; Oddis, C.V.; Medsger, T.A., Jr. Anti-U3 RNP autoantibodies in systemic sclerosis. Arthritis Rheum. 2009, 60, 1112–1118. [Google Scholar] [CrossRef]
- Sharif, R.; Fritzler, M.J.; Mayes, M.D.; Gonzalez, E.B.; McNearney, T.A.; Draeger, H.; Baron, M.; Furst, D.E.; Khanna, D.K.; del Junco, D.J.; et al. Anti-fibrillarin antibody in African American patients with systemic sclerosis: Immunogenetics, clinical features, and survival analysis. J. Rheumatol. 2011, 38, 1622–1630. [Google Scholar] [CrossRef]
- Hanke, K.; Bruckner, C.S.; Dahnrich, C.; Huscher, D.; Komorowski, L.; Meyer, W.; Janssen, A.; Backhaus, M.; Becker, M.; Kill, A.; et al. Antibodies against PM/Scl-75 and PM/Scl-100 are independent markers for different subsets of systemic sclerosis patients. Arthritis Res. Ther. 2009, 11, R22. [Google Scholar] [CrossRef]
- Cozzani, E.; Muracchioli, A.; Murdaca, G.; Beccalli, M.; Caprioli, S.; Zentilin, P.; Ameri, P.; Grosso, M.; Russo, R.; Carmisciano, L.; et al. Correlation Between Skin and Affected Organs in 52 Sclerodermic Patients Followed in a Diseases Management Team: Development of a Risk Prediction Model of Organ-Specific Complications. Front. Immunol. 2021, 12, 588753. [Google Scholar] [CrossRef]
- Wielosz, E.; Dryglewska, M.; Majdan, M. The prevalence and significance of anti-PM/Scl antibodies in systemic sclerosis. Ann. Agric. Env. Med. 2021, 28, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Wodkowski, M.; Hudson, M.; Proudman, S.; Walker, J.; Stevens, W.; Nikpour, M.; Assassi, S.; Mayes, M.D.; Tatibouet, S.; Wang, M.; et al. Clinical correlates of monospecific anti-PM75 and anti-PM100 antibodies in a tri-nation cohort of 1574 systemic sclerosis subjects. Autoimmunity 2015, 48, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Lakota, K.; Thallinger, G.G.; Sodin-Semrl, S.; Rozman, B.; Ambrozic, A.; Tomsic, M.; Praprotnik, S.; Cucnik, S.; Mrak-Poljsak, K.; Ceribelli, A.; et al. International cohort study of 73 anti-Ku-positive patients: Association of p70/p80 anti-Ku antibodies with joint/bone features and differentiation of disease populations by using principal-components analysis. Arthritis Res. Ther. 2012, 14, R2. [Google Scholar] [CrossRef] [PubMed]
- Belizna, C.; Henrion, D.; Beucher, A.; Lavigne, C.; Ghaali, A.; Levesque, H. Anti-Ku antibodies: Clinical, genetic and diagnostic insights. Autoimmun. Rev. 2010, 9, 691–694. [Google Scholar] [CrossRef]
- Rozman, B.; Cucnik, S.; Sodin-Semrl, S.; Czirjak, L.; Varju, C.; Distler, O.; Huscher, D.; Aringer, M.; Steiner, G.; Matucci-Cerinic, M.; et al. Prevalence and clinical associations of anti-Ku antibodies in patients with systemic sclerosis: A European EUSTAR-initiated multi-centre case-control study. Ann. Rheum. Dis. 2008, 67, 1282–1286. [Google Scholar] [CrossRef]
- Casal-Dominguez, M.; Pinal-Fernandez, I.; Derfoul, A.; Graf, R.; Michelle, H.; Albayda, J.; Tiniakou, E.; Adler, B.; Danoff, S.K.; Lloyd, T.E.; et al. The phenotype of myositis patients with anti-Ku autoantibodies. Semin. Arthritis Rheum. 2021, 51, 728–734. [Google Scholar] [CrossRef]
- Valero, C.; Baldivieso, J.P.; Llorente, I.; Vicente-Rabaneda, E.F.; Esparcia Pinedo, L.; Garcia de Vicuna, R.; Alfranca, M.A.; Castañeda, S. AB0427 Anti-nor90 autoantibodies: Favorable or unfavorable prognosis? Ann. Rheum. Dis. 2021, 80, 1241–1242. [Google Scholar] [CrossRef]
- Liaskos, C.; Marou, E.; Simopoulou, T.; Gkoutzourelas, A.; Barmakoudi, M.; Efthymiou, G.; Scheper, T.; Meyer, W.; Katsiari, C.G.; Bogdanos, D.P.; et al. Multiparametric autoantibody profiling of patients with systemic sclerosis in Greece. Mediterr. J. Rheumatol. 2018, 29, 120–126. [Google Scholar] [CrossRef]
- Yamashita, Y.; Yamano, Y.; Muro, Y.; Ogawa-Momohara, M.; Takeichi, T.; Kondoh, Y.; Akiyama, M. Clinical significance of anti-NOR90 antibodies in systemic sclerosis and idiopathic interstitial pneumonia. Rheumatology 2022, 61, 1709–1716. [Google Scholar] [CrossRef]
- Hamaguchi, Y. Autoantibody profiles in systemic sclerosis: Predictive value for clinical evaluation and prognosis. J. Dermatol. 2010, 37, 42–53. [Google Scholar] [CrossRef]
- Dagher, J.H.; Scheer, U.; Voit, R.; Grummt, I.; Lonzetti, L.; Raymond, Y.; Senecal, J.L. Autoantibodies to NOR 90/hUBF: Longterm clinical and serological followup in a patient with limited systemic sclerosis suggests an antigen driven immune response. J. Rheumatol. 2002, 29, 1543–1547. [Google Scholar] [PubMed]
- Hudson, M.; Pope, J.; Mahler, M.; Tatibouet, S.; Steele, R.; Baron, M.; Canadian Scleroderma Research Group (CSRG); Fritzler, M.J. Clinical significance of antibodies to Ro52/TRIM21 in systemic sclerosis. Arthritis Res. Ther. 2012, 14, R50. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.C.; Burlingame, R.W.; Bunn, C.C. Prevalence of antibodies to Ro-52 in a serologically defined population of patients with systemic sclerosis. J. Autoimmune Dis. 2009, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Kruzer, K.; Goncalves Marangoni, R.; Heckler, I.; Elhage, A.; Varga, J.; Hinchcliff, M.; Carns, M.; Aren, K.; Wielgosz, A.; Nuzzo, M.; et al. Clinical and Autoantibody Associations in Antinuclear Antibody-Positive Systemic Sclerosis Lacking Prototypic Autoantibodies. J. Clin. Rheumatol. Pract. Rep. Rheum. Musculoskelet. Dis. 2023, 29, 47–51. [Google Scholar] [CrossRef] [PubMed]

| Variable | Mean (or %) | SD |
|---|---|---|
| Gender, female, % | 85% | |
| Limited cutaneous systemic sclerosis | 56% | |
| Diffuse cutaneous systemic sclerosis | 33% | |
| Polymyositis-scleroderma overlap syndrome | 7% | |
| Systemic sclerosis sine scleroderma | 1% | |
| Age, years | 53.7 | 13.8 |
| Disease duration since Raynaud, years | 11.3 | 8.9 |
| Disease duration since diagnosis, years 1 | 6.2 | 7.9 |
| ESR, mm/h | 18.8 | 15.8 |
| CRP, mg/L | 4.4 | 9.3 |
| Serum creatinine, umol/L | 86.3 | 25.8 |
| eGFR CKD EPI, mL/min/1.73 m2 | 91.9 | 13.6 |
| mRSS score 2 | 12.4 | 8.2 |
| Raynaud’s present, % | 97% | |
| Lung fibrosis (HRCT), % | 69% | |
| Joint contractures, % | 63% | |
| Esophageal symptoms (dysphagia, reflux), % | 60% | |
| Dyspnea (≥NYHA 2), % | 58% | |
| Digital ulcers, % | 52% | |
| Joint synovitis, % | 44% | |
| Muscle weakness, % | 42% | |
| Arterial hypertension, % | 40% | |
| Palpitations, % | 38% | |
| Intestinal symptoms (diarrhea, bloating, constipation), % | 26% | |
| Gastric symptoms (early satiety, vomiting), % | 23% | |
| Muscle atrophy, % | 21% | |
| Proteinuria, % | 19% | |
| CK-elevation, % | 17% | |
| Restrictive defect (VC < 80%) (n = 64), % | 16% | |
| Systolic dysfunction (contractility), % | 15% | |
| Conduction blocks, % | 15% | |
| Diastolic dysfunction, % | 14% | |
| Pulmonary hypertension (echocardiography), % | 13% | |
| Gangrene, % | 9% | |
| Tendon friction rubs, % | 7% | |
| Renal crisis, % | 1% | |
| eGFR CKD EPI < 60 mL/min/1.73 m2 | 1% | |
| FVC (%predicted) (n = 49), % | 88.9 | 22.5 |
| TLC (%predicted) (n = 60), % | 96.9 | 24.7 |
| LVEF, % | 61.3 | 9.2 |
| Scl-70 | Centromere A | Centromere B | Ro-52 | |||||
|---|---|---|---|---|---|---|---|---|
| p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | |
| lcSSc | 0.019 | 0.4 (0.1–0.8) | 0.009 | 5.5 (1.5–20.4) | 0.002 | 6.5 (1.8–24) | 1.000 | 1 (0.4–2.3) |
| dcSSc | 0.000 | 6.4 (2.5–16.4) | 0.016 | 0.2 (0–0.8) | 0.008 | 0.2 (0–0.7) | 0.343 | 0.6 (0.2–1.6) |
| PM/SSc | 0.080 | 0.1 (0–2.1) | 0.342 | 0.3 (0–5.1) | 0.332 | 0.2 (0–4.5) | 0.055 | 5.7 (1–32.9) |
| Raynaud’s present | 0.530 | 3 (0.1–64.8) | 1.000 | 1.4 (0.1–30) | 0.410 | 0.3 (0–4.8) | 1.000 | 2.2 (0.1–47.4) |
| Digital ulcers | 0.648 | 1.3 (0.5–3.2) | 0.270 | 0.5 (0.2–1.5) | 0.040 | 0.3 (0.1–0.9) | 0.090 | 2.5 (0.9–7.3) |
| Gangrene | 0.723 | 1.4 (0.3–5.5) | 0.681 | 0.5 (0.1–4.1) | 0.677 | 0.4 (0–3.5) | 0.016 | 6.1 (1.4–26.8) |
| Joint synovitis | 0.361 | 1.7 (0.7–4.2) | 0.778 | 0.8 (0.3–2.4) | 1.000 | 0.9 (0.3–2.6) | 0.096 | 2.4 (0.9–6.4) |
| Joint contractures | 0.287 | 2.1 (0.7–6.5) | 0.060 | 0.3 (0.1–1) | 0.014 | 0.2 (0.1–0.7) | 0.080 | 4.4 (0.9–20.8) |
| Tendon friction rubs | 0.419 | 2.4 (0.5–11.2) | 0.338 | 0.2 (0–4.4) | 0.340 | 0.2 (0–3.8) | 1.000 | 1 (0.2–5.5) |
| CK-elevation | 0.389 | 0.5 (0.2–1.8) | 0.034 | 0.1 (0–1.7) | 0.019 | 0.1 (0–1.5) | 0.344 | 1.9 (0.6–6.2) |
| Muscle weakness | 0.040 | 0.4 (0.1–0.9) | 1.000 | 1 (0.3–3.2) | 0.598 | 0.7 (0.2–2) | 1.000 | 1.1 (0.4–2.9) |
| Muscle atrophy | 0.055 | 0.3 (0.1–1) | 0.506 | 0.4 (0.1–2.1) | 0.217 | 0.3 (0.1–1.6) | 0.395 | 1.6 (0.6–4.9) |
| Esophageal symptoms (dysphagia, reflux) | 0.815 | 1.2 (0.5–3) | 0.277 | 2 (0.6–6.9) | 0.299 | 1.9 (0.6–5.9) | 0.629 | 1.4 (0.5–3.6) |
| Stomach symptoms (early satiety, vomiting) | 0.443 | 0.6 (0.2–1.7) | 0.350 | 1.9 (0.6–5.9) | 0.253 | 1.9 (0.6–5.6) | 0.592 | 0.7 (0.2–2.1) |
| Intestinal symptoms (diarrhea, bloating, constipation) | 0.324 | 0.6 (0.2–1.6) | 0.545 | 1.5 (0.5–4.8) | 1.000 | 1.1 (0.3–3.2) | 1.000 | 0.9 (0.3–2.6) |
| Arterial Hypertension | 0.652 | 0.8 (0.3–1.8) | 0.055 | 3.1 (1–9.4) | 0.121 | 2.5 (0.9–7) | 0.633 | 1.4 (0.5–3.5) |
| Dyspnea (≥NYHA 2) | 1.000 | 1 (0.4–2.5) | 0.392 | 0.6 (0.2–1.8) | 0.422 | 0.6 (0.2–1.8) | 1.000 | 1 (0.4–2.6) |
| Palpitations | 0.635 | 1.3 (0.5–3.4) | 1.000 | 1.1 (0.4–3.6) | 1.000 | 1 (0.3–2.9) | 0.305 | 1.8 (0.6–5) |
| Conduction blocks | 0.372 | 1.8 (0.6–5.7) | 1.000 | 0.7 (0.1–3.3) | 1.000 | 1 (0.2–4) | 1.000 | 1 (0.3–3.6) |
| Diastolic dysfunction | 0.546 | 1.5 (0.5–4.9) | 0.446 | 0.3 (0–2.6) | 0.281 | 0.3 (0–2.2) | 1.000 | 1.1 (0.3–4.1) |
| LVEF < 55% | 0.476 | 1.7 (0.4–7.3) | 0.338 | 0.2 (0–4.2) | 0.678 | 0.5 (0.1–4.2) | 0.098 | 4.5 (1–20.6) |
| Systolic dysfunction (contractility) | 0.376 | 1.8 (0.6–5.6) | 0.728 | 0.7 (0.1–3.3) | 1.000 | 1 (0.2–4) | 0.518 | 1.6 (0.5–5.3) |
| Pulmonary hypertension (ECHO) | 1.000 | 1.2 (0.3–4) | 0.216 | 2.7 (0.7–10.6) | 0.282 | 2 (0.5–7.7) | 0.299 | 2.1 (0.6–7.5) |
| Pulmonary hypertension (RHC) | 0.143 | 0.1 (0–2.1) | 1.000 | 1.5 (0.1–40.6) | 1.000 | 1.5 (0.1–40.6) | 0.143 | 16.3 (0.5–555.7) |
| Restrictive defect (VC < 80%) | 0.074 | 0.3 (0.1–1.1) | 0.667 | 0.4 (0–3.7) | 1.000 | 0.9 (0.2–4.9) | 0.740 | 0.6 (0.1–2.5) |
| Lung fibrosis (HRCT) | 0.171 | 0.5 (0.2–1.4) | 0.714 | 0.8 (0.2–3.3) | 0.481 | 0.6 (0.2–2.3) | 0.765 | 1.4 (0.4–5) |
| DLCO < 60% | 0.105 | 0.4 (0.1–1.2) | 0.418 | 3.7 (0.4–32.3) | 0.481 | 2.1 (0.4–10.7) | 0.036 | 5.3 (1.1–26.1) |
| Proteinuria | 0.176 | 0.4 (0.1–1.3) | 1.000 | 0.8 (0.2–3.1) | 0.342 | 0.4 (0.1–1.9) | 0.150 | 2.3 (0.8–6.7) |
| eGFR CKD EPI < 60 mL/min/1.73 m2 | 1.000 | 1.6 (0–84.9) | 1.000 | 3.9 (0.1–201.4) | 1.000 | 3.4 (0.1–177.4) | 1.000 | 2.5 (0–126.8) |
| Renal crisis | 1.000 | 0.6 (0–14) | 1.000 | 1.4 (0.1–35.4) | 1.000 | 1.1 (0–28.8) | 1.000 | 0.8 (0–20.2) |
| RNA Pol III 11 kDa | RNA Pol III 155 kDa | Fibrillarin | NOR90 | |||||
|---|---|---|---|---|---|---|---|---|
| p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | |
| lcSSc | 1.000 | 1.2 (0.2–7.5) | 0.581 | 0.4 (0–4.4) | 0.695 | 0.6 (0.1–2.7) | 0.502 | 4.1 (0.2–88) |
| dcSSc | 0.657 | 0.5 (0–4.3) | 0.271 | 4 (0.3–45.9) | 0.689 | 1.5 (0.3–7) | 0.544 | 0.4 (0–7.9) |
| PM/SSc | 0.289 | 4.2 (0.4–44.4) | 1.000 | 1.9 (0.1–40) | 1.000 | 0.8 (0–16.1) | 1.000 | 2.6 (0.1–60.7) |
| Raynaud’s present | 1.000 | 0.3 (0–6.4) | 1.000 | 0.2 (0–5.1) | 1.000 | 0.5 (0–10.5) | 1.000 | 0.1 (0–3.9) |
| Digital ulcers | 1.000 | 1.4 (0.1–15.7) | 0.562 | 0.3 (0–3.7) | 0.643 | 2.8 (0.3–26.7) | 1.000 | 0.7 (0–11) |
| Gangrene | 1.000 | 0.7 (0–13.4) | 1.000 | 1.1 (0.1–23.1) | 0.557 | 1.5 (0.2–13.7) | 1.000 | 1.6 (0.1–35.2) |
| Joint synovitis | 0.348 | 0.3 (0–2.9) | 0.108 | 0.1 (0–2.5) | 0.203 | 5.1 (0.6–46) | 0.495 | 4.9 (0.2–104.8) |
| Joint contractures | 0.571 | 2.5 (0.1–49.5) | 0.571 | 2.5 (0.1–49.5) | 0.326 | 4 (0.2–75.4) | 0.435 | 0.3 (0–5.3) |
| Tendon friction rubs | 1.000 | 1 (0–18.9) | 1.000 | 1.5 (0.1–32.6) | 0.091 | 6.2 (1–40.6) | 1.000 | 2.2 (0.1–49.6) |
| CK-elevation | 0.552 | 1.6 (0.2–16.2) | 1.000 | 0.6 (0–12.5) | 1.000 | 0.8 (0.1–6.7) | 1.000 | 1.5 (0.1–37.9) |
| Muscle weakness | 1.000 | 1.2 (0.2–8.9) | 0.591 | 2.4 (0.2–28.1) | 0.174 | 5.2 (0.6–48.5) | 0.207 | 6.2 (0.3–133.9) |
| Muscle atrophy | 1.000 | 1.1 (0.1–11.5) | 0.547 | 1.7 (0.1–20.1) | 0.009 | 16.8 (1.7–161.4) | 1.000 | 0.6 (0–13.9) |
| Esophageal symptoms (dysphagia, reflux) | 0.608 | 0.5 (0.1–3.9) | 1.000 | 1.1 (0.1–12.4) | 0.660 | 2.8 (0.3–25.5) | 1.000 | 0.5 (0–8.7) |
| Stomach symptoms (early satiety, vomiting) | 0.568 | 0.3 (0–5.9) | 0.568 | 0.4 (0–8) | 0.167 | 3.3 (0.6–17.5) | 0.444 | 3 (0.2–50.9) |
| Intestinal symptoms (diarrhea, bloating, constipation) | 1.000 | 1 (0.1–12.1) | 0.547 | 0.3 (0–5.6) | 0.657 | 1.4 (0.2–9.1) | 0.547 | 2.1 (0.1–35.4) |
| Arterial Hypertension | 0.028 | 14 (0.7–268.5) | 0.070 | 10.6 (0.5–210.9) | 0.691 | 1.4 (0.3–7.5) | 0.508 | 0.3 (0–5.7) |
| Dyspnea (≥NYHA 2) | 0.294 | 5.1 (0.3–97.2) | 0.548 | 3.9 (0.2–77.3) | 1.000 | 0.8 (0.1–4.9) | 1.000 | 0.5 (0–8.4) |
| Palpitations | 1.000 | 1.1 (0.1–8.4) | 0.242 | 0.1 (0–2.9) | 0.020 | 14.1 (0.8–265.5) | 0.221 | 5.9 (0.3–126.5) |
| Conduction blocks | 1.000 | 0.7 (0–13.6) | 1.000 | 0.9 (0–20.7) | 0.006 | 13.6 (2.2–84.2) | 1.000 | 0.9 (0–20.7) |
| Diastolic dysfunction | 1.000 | 0.7 (0–14.9) | 1.000 | 1 (0–22.7) | 1.000 | 1.1 (0.1–10.3) | 1.000 | 1 (0–22.7) |
| LVEF < 55% | 1.000 | 1.1 (0.1–23.9) | 1.000 | 1.6 (0.1–36.5) | 1.000 | 0.7 (0–13.8) | 1.000 | 1.6 (0.1–36.5) |
| Systolic dysfunction (contractility) | 0.430 | 2.6 (0.2–30.6) | 0.311 | 5.2 (0.3–89.1) | 1.000 | 1 (0.1–9.1) | 1.000 | 0.9 (0–20.4) |
| Pulmonary hypertension (ECHO) | 1.000 | 0.8 (0–16.1) | 1.000 | 1.1 (0.1–24.6) | 0.552 | 1.5 (0.2–14.9) | 1.000 | 1.1 (0.1–24.6) |
| Pulmonary hypertension (RHC) | 1.000 | 1.3 (0–82.5) | 1.000 | 1.3 (0–82.5) | 0.429 | 5.4 (0.2–188.8) | 1.000 | 1.3 (0–82.5) |
| Restrictive defect (VC < 80%) | 0.422 | 3.4 (0.2–57.2) | 1.000 | 1 (0–26.4) | 0.564 | 0.3 (0–6.3) | 1.000 | 0.6 (0–13.2) |
| Lung fibrosis (HRCT) | 1.000 | 1.8 (0.1–37.6) | 1.000 | 1.3 (0.1–28.4) | 0.135 | 0.3 (0.1–1.4) | 1.000 | 1.3 (0.1–28.4) |
| DLCO < 60 | 1.000 | 0.9 (0.1–10.9) | 0.538 | 0.5 (0–7.6) | 1.000 | 1.4 (0.1–14.6) | 0.538 | 0.5 (0–7.6) |
| Proteinuria | 1.000 | 1 (0.1–9.7) | 1.000 | 0.5 (0–11) | 0.026 | 6.7 (1.3–33.1) | 0.358 | 4.2 (0.3–71.2) |
| eGFR CKD EPI < 60 mL/min/1.73 m2 | 1.000 | 16.1 (0.3–890.5) | 1.000 | 25.9 (0.4–1503.3) | 1.000 | 11.5 (0.2–623.7) | 1.000 | 36.6 (0.6–2245) |
| Renal crisis | 0.045 | 73.3 (2.5–2140.5) | 0.034 | 103.8 (3.3–3233.3) | 1.000 | 4.2 (0.2–114.6) | 1.000 | 11.5 (0.4–359.3) |
| Th/To | PM-Scl100 | PM-Scl75 | Ku | PDGFR | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | |
| lcSSc | 0.695 | 0.6 (0.1–2.7) | 0.554 | 0.7 (0.2–2.1) | 0.209 | 0.5 (0.2–1.4) | 0.441 | 0.3 (0–6.5) | 0.082 | 0.1 (0–2.1) |
| dcSSc | 1.000 | 0.7 (0.1–4.1) | 0.004 | 0.1 (0–1) | 0.278 | 0.4 (0.1–1.5) | 1.000 | 0.6 (0–15.7) | 0.038 | 14.6 (0.7–291.8) |
| PM/SSc | 0.063 | 8.2 (1.2–56.1) | 0.000 | 188.1 (9.6–3673.8) | 0.000 | 90.6 (4.9–1687.7) | 0.065 | 47.7 (1.7–1313.1) | 1.000 | 1.9 (0.1–40) |
| Raynaud’s present | 1.000 | 0.5 (0–10.5) | 1.000 | 0.9 (0–19.4) | 1.000 | 1.4 (0.1–30) | 1.000 | 0.1 (0–2.7) | 1.000 | 0.2 (0–5.1) |
| Digital ulcers | 0.393 | 3.6 (0.4–32.6) | 0.753 | 0.8 (0.2–2.9) | 0.414 | 1.7 (0.5–5.4) | 0.402 | 0.2 (0–5.5) | 0.270 | 5 (0.3–100.9) |
| Gangrene | 1.000 | 0.6 (0–11) | 0.590 | 0.3 (0–6.3) | 0.672 | 1.3 (0.2–6.9) | 1.000 | 8.1 (0.2–429.9) | 0.288 | 4.6 (0.4–56.8) |
| Joint synovitis | 0.012 | 16.6 (0.9–301.7) | 0.068 | 3.8 (1–15.1) | 0.186 | 2.3 (0.8–6.7) | 0.482 | 0.3 (0–7.6) | 1.000 | 1.9 (0.2–21.8) |
| Joint contractures | 1.000 | 1.7 (0.2–15.5) | 1.000 | 0.9 (0.2–3.8) | 0.750 | 1.6 (0.4–6.4) | 1.000 | 1 (0–25.9) | 0.571 | 2.5 (0.1–49.5) |
| Tendon friction rubs | 0.444 | 2.1 (0.2–20.8) | 0.587 | 0.4 (0–6.6) | 0.633 | 1.6 (0.3–8.8) | 1.000 | 3.7 (0.1–98.1) | 0.005 | 75.9 (3.2–1783.2) |
| CK-elevation | 0.104 | 4.1 (0.8–20.5) | 0.000 | 28.3 (6.2–129.5) | 0.000 | 38.4 (9–164.1) | 0.179 | 14.4 (0.6–371) | 0.450 | 2.4 (0.2–28.3) |
| Muscle weakness | 0.044 | 8.3 (0.9–71.9) | 0.005 | 8.4 (1.7–41) | 0.017 | 4 (1.3–12.6) | 0.458 | 3.6 (0.1–92) | 1.000 | 0.6 (0.1–6.7) |
| Muscle atrophy | 0.193 | 2.8 (0.6–13.9) | 0.070 | 3.5 (1–12) | 0.010 | 5 (1.6–15.5) | 1.000 | 1.1 (0–27.7) | 0.547 | 1.7 (0.1–20.1) |
| Esophageal symptoms (dysphagia, reflux) | 0.047 | 0.2 (0–1) | 0.358 | 0.6 (0.2–1.8) | 0.792 | 0.9 (0.3–2.5) | 1.000 | 1.6 (0.1–41.7) | 0.549 | 4 (0.2–79.9) |
| Stomach symptoms (early satiety, vomiting) | 0.673 | 0.5 (0.1–4.1) | 0.281 | 0.2 (0–1.9) | 0.768 | 1.2 (0.4–3.8) | 1.000 | 1 (0–24.3) | 1.000 | 1.5 (0.1–17.4) |
| Intestinal symptoms (diarrhea, bloating, constipation) | 0.657 | 1.4 (0.2–9.1) | 1.000 | 1 (0.2–4.6) | 0.364 | 1.7 (0.5–5.7) | 1.000 | 0.7 (0–17.1) | 1.000 | 1 (0.1–12.1) |
| Arterial Hypertension | 0.124 | 3.9 (0.7–21.2) | 0.346 | 0.5 (0.1–1.9) | 0.284 | 0.5 (0.2–1.6) | 1.000 | 0.5 (0–11.4) | 1.000 | 0.7 (0.1–7.9) |
| Dyspnea (≥NYHA 2) | 1.000 | 1 (0.2–6) | 0.499 | 0.6 (0.2–2.1) | 1.000 | 0.9 (0.3–2.9) | 0.341 | 0.2 (0–4.3) | 0.548 | 3.9 (0.2–77.3) |
| Palpitations | 1.000 | 1.1 (0.2–5.9) | 0.740 | 0.7 (0.2–2.7) | 0.774 | 1.3 (0.4–4.2) | 1.000 | 0.4 (0–9.1) | 0.601 | 2.3 (0.2–26.4) |
| Conduction blocks | 1.000 | 0.8 (0.1–7.4) | 0.197 | 0.2 (0–3.2) | 0.725 | 0.6 (0.1–3) | 1.000 | 1.6 (0.1–41.2) | 1.000 | 0.7 (0–13.6) |
| Diastolic dysfunction | 1.000 | 0.9 (0.1–8.2) | 1.000 | 0.5 (0.1–4.4) | 1.000 | 0.7 (0.1–3.4) | 1.000 | 1.7 (0.1–45) | 1.000 | 0.7 (0–14.9) |
| LVEF < 55% | 0.546 | 1.5 (0.2–14.5) | 1.000 | 0.9 (0.1–7.7) | 1.000 | 1.2 (0.2–6.7) | 1.000 | 2.7 (0.1–72.4) | 0.196 | 9.9 (0.6–175.4) |
| Systolic dysfunction (contractility) | 0.336 | 2.1 (0.4–12.3) | 0.681 | 0.5 (0.1–3.9) | 1.000 | 1.1 (0.3–4.4) | 1.000 | 1.6 (0.1–40.6) | 0.430 | 2.6 (0.2–30.6) |
| Pulmonary hypertension (ECHO) | 1.000 | 1 (0.1–9) | 1.000 | 0.6 (0.1–4.8) | 0.704 | 1.4 (0.3–5.7) | 1.000 | 1.9 (0.1–48.8) | 1.000 | 0.8 (0–16.1) |
| Pulmonary hypertension (RHC) | 1.000 | 0.3 (0–11.3) | 1.000 | 0.3 (0–11.3) | 1.000 | 1.5 (0.1–40.6) | 1.000 | 1.3 (0–82.5) | 1.000 | 1.3 (0–82.5) |
| Restrictive defect (VC < 80%) | 0.622 | 1.7 (0.3–10.3) | 1.000 | 1.1 (0.3–4.7) | 1.000 | 1 (0.3–3.6) | 1.000 | 1 (0–26.4) | 1.000 | 1 (0–26.4) |
| Lung fibrosis (HRCT) | 1.000 | 1.5 (0.2–13.7) | 0.062 | 8.3 (0.5–147.8) | 0.017 | 13.5 (0.8–237.1) | 1.000 | 0.8 (0–19.7) | 0.098 | 0.1 (0–1.3) |
| DLCO < 60 | 0.649 | 0.7 (0.1–4.4) | 1.000 | 0.9 (0.2–3.5) | 0.757 | 1.5 (0.4–5.6) | 1.000 | 1.4 (0.1–37.1) | 1.000 | 1.4 (0.1–37.1) |
| Proteinuria | 0.026 | 6.7 (1.3–33.1) | 0.714 | 1.3 (0.3–5.2) | 0.516 | 1.6 (0.5–5.4) | 1.000 | 1.3 (0.1–33.4) | 1.000 | 0.5 (0–11) |
| eGFR CKD EPI < 60 mL/min/1.73 m2 | 1.000 | 11.5 (0.2–623.7) | 0.138 | 19.6 (0.8–507.3) | 0.202 | 12.2 (0.5–312.9) | 1.000 | 61.7 (0.9–4275.8) | 1.000 | 25.9 (0.4–1503.3) |
| Renal crisis | 1.000 | 3.6 (0.1–96.9) | 1.000 | 2 (0.1–52.9) | 1.000 | 1.3 (0–32.5) | 1.000 | 19.4 (0.5–700.7) | 1.000 | 8.1 (0.3–237.8) |
| ANAP+ | ANAP− | ||
|---|---|---|---|
| SSP + n, % | 65 | 12 | 77 |
| 68% | 12% | 80% | |
| SSP − n, % | 0 | 19 | 19 |
| 0% | 20% | 20% | |
| 65 | 31 | 96 | |
| 68% | 32% | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Żebryk, P.; Przymuszała, P.; Nowak, J.K.; Piorunek, T.; Mularek-Kubzdela, T.; Puszczewicz, M. Autoantibodies and Clinical Correlations in Polish Systemic Sclerosis Patients: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 657. https://doi.org/10.3390/jcm12020657
Żebryk P, Przymuszała P, Nowak JK, Piorunek T, Mularek-Kubzdela T, Puszczewicz M. Autoantibodies and Clinical Correlations in Polish Systemic Sclerosis Patients: A Cross-Sectional Study. Journal of Clinical Medicine. 2023; 12(2):657. https://doi.org/10.3390/jcm12020657
Chicago/Turabian StyleŻebryk, Paweł, Piotr Przymuszała, Jan Krzysztof Nowak, Tomasz Piorunek, Tatiana Mularek-Kubzdela, and Mariusz Puszczewicz. 2023. "Autoantibodies and Clinical Correlations in Polish Systemic Sclerosis Patients: A Cross-Sectional Study" Journal of Clinical Medicine 12, no. 2: 657. https://doi.org/10.3390/jcm12020657
APA StyleŻebryk, P., Przymuszała, P., Nowak, J. K., Piorunek, T., Mularek-Kubzdela, T., & Puszczewicz, M. (2023). Autoantibodies and Clinical Correlations in Polish Systemic Sclerosis Patients: A Cross-Sectional Study. Journal of Clinical Medicine, 12(2), 657. https://doi.org/10.3390/jcm12020657








