Diabetes Mellitus and Obesity as Prognostic Factors in Arthroscopic Repair of Chronic Rotator Cuff Tears
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Subjects
2.3. Inclusion Criteria
- -
- Patients with chronic rotator cuff tear, diagnosed by ultrasound or MRI.
- -
- Follow-up time of at least 5 years.
- -
- Intervention performed by expert surgeons in this technique (all of them with similar learning curves: all patients included in the study have been treated by surgeons with more than 10 years of experience in arthroscopic shoulder surgery techniques, all of them having completed more than 200 cases of this type).
2.4. Exclusion Criteria
- -
- Absence of follow-up.
- -
- Non-acceptance of verbal consent via telephone call to take part in the study.
- -
- Subacromial impingement diagnosed by ultrasound or MRI (patients with osseous or ligamentous radiologic factors that could be responsible for the rotator cuff tear, such as: Bigliani Type III acromia, persistent os acromiale, acromial enthesophytes secondary to acromioclavicular osteoarthritis, coracoacromial ligaments with >1 bundle).
- -
- Diagnosis of depression or other psychiatric disorders.
2.5. Research Variables
- -
- Date of birth.
- -
- Age (years).
- -
- Sex (male or female).
- -
- Obesity (yes/no). Patients with a body mass index greater than 30 were included in the obese group.
- -
- Diabetes (yes/no). Patients with type II diabetes mellitus at the time of the operation were included in the group of diabetic patients (two separated test of HbA1c > 6.5%).
- -
- Smoking (yes/no).
- -
- Dominance (right/left).
- -
- Side operated on (right/left).
- -
- Date of surgery.
- -
- Age at the time of surgery (years).
- -
- Complications (yes/no): specifying which (postoperative organ pathology, infection, wound dehiscence, etc.)
- -
- Reintervention (yes/no): specifying cause and date of reintervention.
- -
- Residual pain (yes/no).
- -
- Pain improvement or worsening after surgery.
- -
- Subjective functionality after surgery (improvement, same, or worsening).
- -
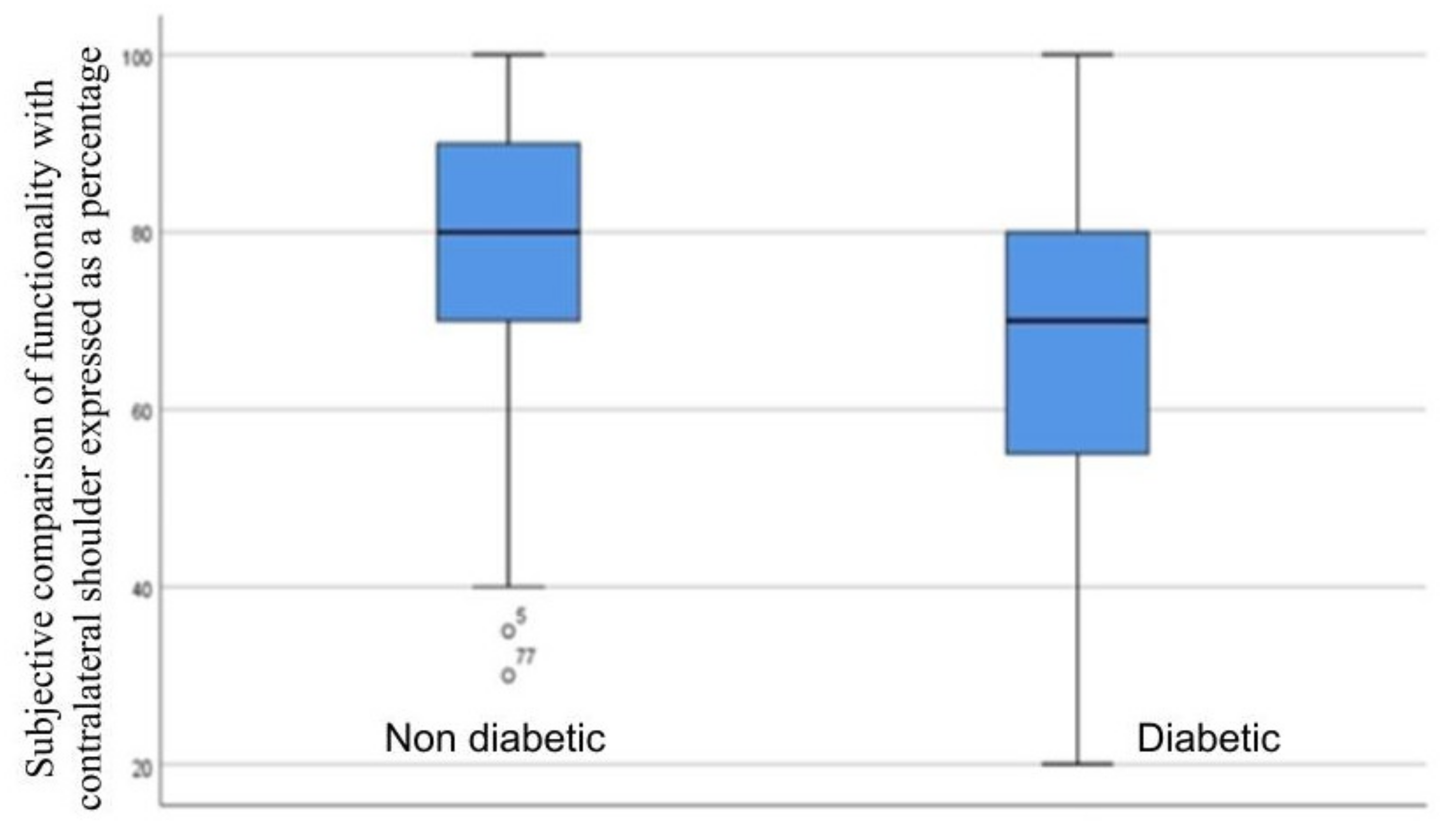
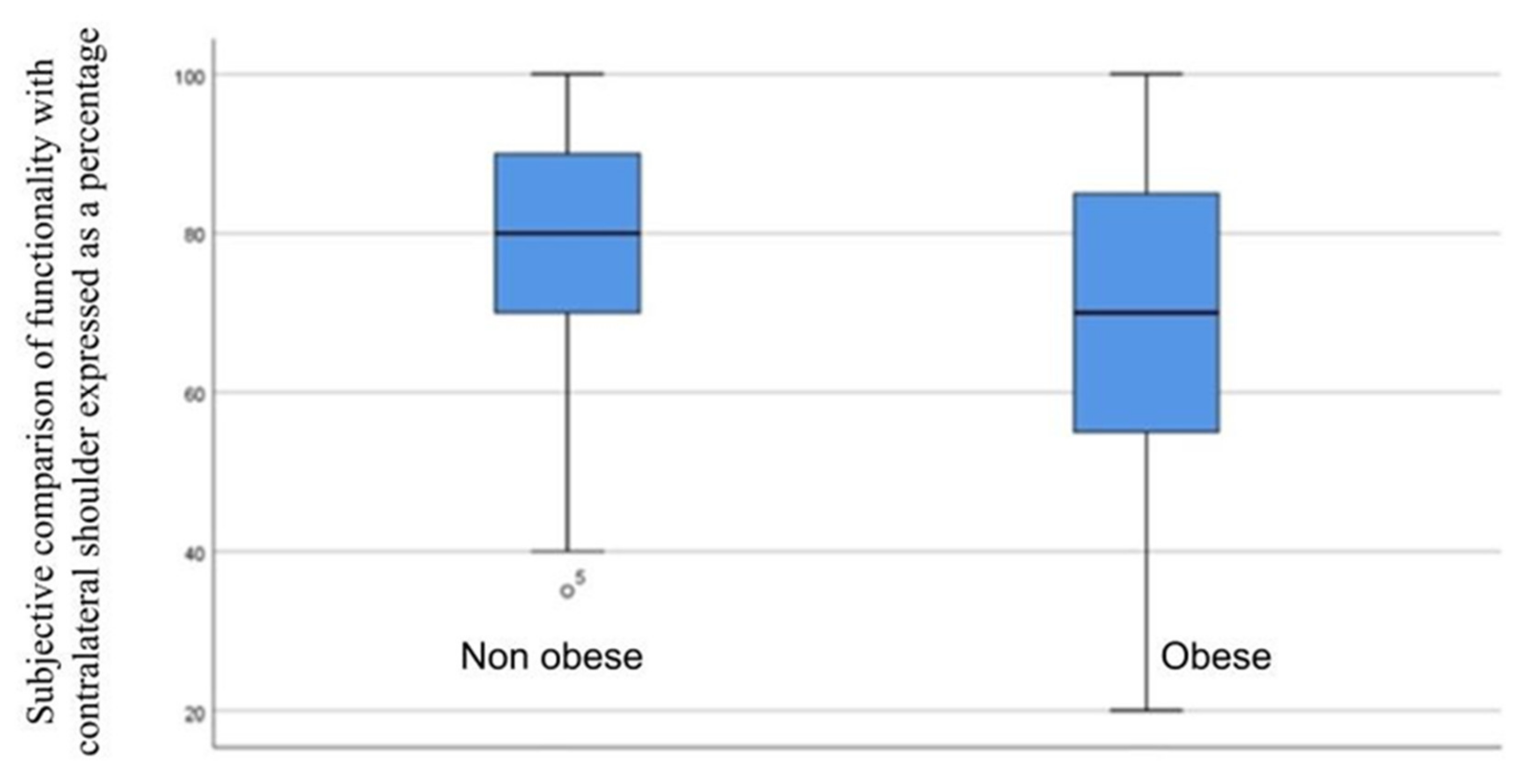
- Subjective comparison of functionality with contralateral shoulder expressed as a percentage. A total of 100% corresponded to complete functionality, without restrictions and without differences with respect to the healthy shoulder; and 0% corresponded to an extremely limited functionality with respect to the healthy shoulder, not being able to incorporate it into the basic activities of daily living (BADL).
- -
- Satisfaction level expressed by the answer to the following question: Would you have the surgery again? (yes/no) A situation was considered in which it would be necessary to operate again, and it was asked if you would be willing, based on your previous experience, to be operated on again or not.
2.6. Data Collection
2.7. Statistical Analysis of Data
3. Results
3.1. Impact of Diabetes
3.2. Impact of Obesity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fermont, A.J.M.; Wolterbeek, N.; Wessel, R.N.; Baeyens, J.-P.; de Bie, R.A. Prognostic Factors for Successful Recovery after Arthroscopic Rotator Cuff Repair: A Systematic Literature Review. J. Orthop. Sports Phys. Ther. 2014, 44, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Van der Zwaal, P.; Pekelharing, J.F.; Thomassen, B.J.W.; Swen, J.-W.A.; van Arkel, E.R.A. Diagnosis and treatment of rotator cuff tears. Ned. Tijdschr. Geneeskd. 2011, 155, A3163. [Google Scholar] [PubMed]
- Penas García, C.; González González, Y.; Alonso Calvete, A.; Da Cuña Carrera, I.; Penas García, C.; González González, Y.; Alonso Calvete, A.; Da Cuña Carrera, I. Factores de Riesgo Para La Rotura Del Manguito Rotador. Rev. Asoc. Esp. Espec. En Med. Trab. 2021, 30, 104–117. [Google Scholar]
- Mall, N.A.; Kim, H.M.; Keener, J.D.; Steger-May, K.; Teefey, S.A.; Middleton, W.D.; Stobbs, G.; Yamaguchi, K. Symptomatic Progression of Asymptomatic Rotator Cuff Tears: A Prospective Study of Clinical and Sonographic Variables. J. Bone Joint Surg. Am. 2010, 92, 2623–2633. [Google Scholar] [CrossRef] [PubMed]
- Boissonnault, W.G.; Badke, M.B.; Wooden, M.J.; Ekedahl, S.; Fly, K. Patient Outcome Following Rehabilitation for Rotator Cuff Repair Surgery: The Impact of Selected Medical Comorbidities. J. Orthop. Sports Phys. Ther. 2007, 37, 312–319. [Google Scholar] [CrossRef]
- Morse, K.; Davis, A.D.; Afra, R.; Kaye, E.K.; Schepsis, A.; Voloshin, I. Arthroscopic versus Mini-Open Rotator Cuff Repair: A Comprehensive Review and Meta-Analysis. Am. J. Sports Med. 2008, 36, 1824–1828. [Google Scholar] [CrossRef]
- MacDonald, P.; McRae, S.; Leiter, J.; Mascarenhas, R.; Lapner, P. Arthroscopic Rotator Cuff Repair with and without Acromioplasty in the Treatment of Full-Thickness Rotator Cuff Tears: A Multicenter, Randomized Controlled Trial. J. Bone Joint Surg. Am. 2011, 93, 1953–1960. [Google Scholar] [CrossRef]
- Strauss, E.J.; Salata, M.J.; Kercher, J.; Barker, J.U.; McGill, K.; Bach, B.R.; Romeo, A.A.; Verma, N.N. The Arthroscopic Management of Partial-Thickness Rotator Cuff Tears: A Systematic Review of the Literature. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2011, 27, 568–580. [Google Scholar] [CrossRef]
- McFarland, E.G.; O’Neill, O.R.; Hsu, C.Y. Complications of Shoulder Arthroscopy. J. South. Orthop. Assoc. 1997, 6, 190–196. [Google Scholar]
- Paxton, E.S.; Backus, J.; Keener, J.; Brophy, R.H. Shoulder Arthroscopy: Basic Principles of Positioning, Anesthesia, and Portal Anatomy. J. Am. Acad. Orthop. Surg. 2013, 21, 332–342. [Google Scholar] [CrossRef]
- Chung, S.W.; Oh, J.H.; Gong, H.S.; Kim, J.Y.; Kim, S.H. Factors Affecting Rotator Cuff Healing after Arthroscopic Repair: Osteoporosis as One of the Independent Risk Factors. Am. J. Sports Med. 2011, 39, 2099–2107. [Google Scholar] [CrossRef]
- Silva, C.M.M.; Mourão, N.M.; da Rocha, L.N.; Landim, J.I.V.D.; Rocha, H.A.L.; Lacerda, M.A.A.; Rocha, F.A.C.; Leite, J.A.D. Surgical Outcome Following Rotator Cuff Tear Repair in a Low-Income Population. Impact of Obesity and Smoking. BMC Musculoskelet. Disord. 2021, 22, 714. [Google Scholar] [CrossRef]
- Hong, C.-K.; Chang, C.-J.; Kuan, F.-C.; Hsu, K.-L.; Chen, Y.; Chiang, C.-H.; Su, W.-R. Patients with Diabetes Mellitus Have a Higher Risk of Tendon Retear After Arthroscopic Rotator Cuff Repair: A Meta-Analysis. Orthop. J. Sports Med. 2020, 8, 2325967120961406. [Google Scholar] [CrossRef]
- Lu, P.-P.; Chen, M.-H.; Dai, G.-C.; Li, Y.-J.; Shi, L.; Rui, Y.-F. Understanding Cellular and Molecular Mechanisms of Pathogenesis of Diabetic Tendinopathy. World J. Stem Cells 2020, 12, 1255–1275. [Google Scholar] [CrossRef]
- Prevalencia de Diabetes. Available online: https://www3.gobiernodecanarias.org/sanidad/scs/contenidoGenerico.jsp?idDocument=559b6b85-4488-11e8-9d80-a9ef3954dfeb&idCarpeta=6bcc897d-ab21-11dd-970d-d73a0633ac17 (accessed on 19 October 2022).
- Ranger, T.A.; Wong, A.M.Y.; Cook, J.L.; Gaida, J.E. Is There an Association between Tendinopathy and Diabetes Mellitus? A Systematic Review with Meta-Analysis. Br. J. Sports Med. 2016, 50, 982–989. [Google Scholar] [CrossRef]
- Warrender, W.J.; Brown, O.L.; Abboud, J.A. Outcomes of Arthroscopic Rotator Cuff Repairs in Obese Patients. J. Shoulder Elbow Surg. 2011, 20, 961–967. [Google Scholar] [CrossRef]
- Rothman, R.H.; Parke, W.W. The Vascular Anatomy of the Rotator Cuff. Clin. Orthop. 1965, 41, 176–186. [Google Scholar]
- Siervogel, R.M.; Wisemandle, W.; Maynard, L.M.; Guo, S.S.; Chumlea, W.C.; Towne, B. Lifetime Overweight Status in Relation to Serial Changes in Body Composition and Risk Factors for Cardiovascular Disease: The Fels Longitudinal Study. Obes. Res. 2000, 8, 422–430. [Google Scholar] [CrossRef]
- Kelsey, J.L.; White, A.A.; Pastides, H.; Bisbee, G.E. The Impact of Musculoskeletal Disorders on the Population of the United States. J. Bone Joint Surg. Am. 1979, 61, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Hubert, H.B.; Feinleib, M.; McNamara, P.M.; Castelli, W.P. Obesity as an Independent Risk Factor for Cardiovascular Disease: A 26-Year Follow-up of Participants in the Framingham Heart Study. Circulation 1983, 67, 968–977. [Google Scholar] [CrossRef]
- Abboud, J.A.; Kim, J.S. The Effect of Hypercholesterolemia on Rotator Cuff Disease. Clin. Orthop. 2010, 468, 1493–1497. [Google Scholar] [CrossRef] [PubMed]
- Ateschrang, A.; Eggensperger, F.; Ahrend, M.D.; Schröter, S.; Stöckle, U.; Kraus, T.M. Obesity Causes Poorer Clinical Results and Higher Re-Tear Rates in Rotator Cuff Repair. Arch. Orthop. Trauma Surg. 2018, 138, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Rui, Y.F.; Li, G.; Wang, C. Alterations of Tendons in Diabetes Mellitus: What Are the Current Findings? Int. Orthop. 2015, 39, 1465–1473. [Google Scholar] [CrossRef]
- Egemen, O.; Ozkaya, O.; Ozturk, M.B.; Sen, E.; Akan, M.; Sakiz, D.; Aygit, C. The Biomechanical and Histological Effects of Diabetes on Tendon Healing: Experimental Study in Rats. J. Hand Microsurg. 2012, 4, 60–64. [Google Scholar] [CrossRef]
- Borton, Z.; Shivji, F.; Simeen, S.; Williams, R.; Tambe, A.; Espag, M.; Cresswell, T.; Clark, D. Diabetic Patients Are Almost Twice as Likely to Experience Complications from Arthroscopic Rotator Cuff Repair. Shoulder Elb. 2020, 12, 109–113. [Google Scholar] [CrossRef]
| Age Range | N | % |
|---|---|---|
| 20–28 | 1 | 1.25 |
| 28–36 | 1 | 1.25 |
| 36–44 | 5 | 6.25 |
| 44–52 | 12 | 15 |
| 52–60 | 22 | 27.5 |
| 60–68 | 27 | 33.75 |
| 68–76 | 9 | 11.25 |
| 76–84 | 3 | 3.75 |
| Total | 80 |
| Sex | Dominant Hand | Side Operated |
|---|---|---|
| Male: N = 29; 36.25% | Right: N = 78; 97.50% | Right: N = 57; 71.25% |
| Female: N = 51; 36.25% | Left: N = 2; 2.50% | Left: N = 23; 28.75% |
| Patients | Residual Pain | Reoperation | |||||
|---|---|---|---|---|---|---|---|
| N | % 1 | N | % 2 | N | % 2 | ||
| Diabetes Mellitus | Yes | 24 | 30 | 13 | 54.16 | 0 | 0 |
| No | 56 | 70 | 27 | 48.21 | 7 | 12.5 | |
| Total | 80 | 40 | 7 | ||||
| Obesity | Yes | 47 | 58.8 | 28 | 59.57 | 4 | 8.51 |
| No | 33 | 41.2 | 12 | 26.26 | 3 | 9.09 | |
| Total | 80 | 40 | 7 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Álvarez de la Cruz, J.; Méndez Ojeda, M.M.; Álvarez Benito, N.; Herrera Rodríguez, A.; Pais Brito, J.L.; Márquez Marfil, F.J. Diabetes Mellitus and Obesity as Prognostic Factors in Arthroscopic Repair of Chronic Rotator Cuff Tears. J. Clin. Med. 2023, 12, 627. https://doi.org/10.3390/jcm12020627
Álvarez de la Cruz J, Méndez Ojeda MM, Álvarez Benito N, Herrera Rodríguez A, Pais Brito JL, Márquez Marfil FJ. Diabetes Mellitus and Obesity as Prognostic Factors in Arthroscopic Repair of Chronic Rotator Cuff Tears. Journal of Clinical Medicine. 2023; 12(2):627. https://doi.org/10.3390/jcm12020627
Chicago/Turabian StyleÁlvarez de la Cruz, Javier, Marye Mercé Méndez Ojeda, Nuria Álvarez Benito, Alejandro Herrera Rodríguez, Jose Luis Pais Brito, and Francisco Jesús Márquez Marfil. 2023. "Diabetes Mellitus and Obesity as Prognostic Factors in Arthroscopic Repair of Chronic Rotator Cuff Tears" Journal of Clinical Medicine 12, no. 2: 627. https://doi.org/10.3390/jcm12020627
APA StyleÁlvarez de la Cruz, J., Méndez Ojeda, M. M., Álvarez Benito, N., Herrera Rodríguez, A., Pais Brito, J. L., & Márquez Marfil, F. J. (2023). Diabetes Mellitus and Obesity as Prognostic Factors in Arthroscopic Repair of Chronic Rotator Cuff Tears. Journal of Clinical Medicine, 12(2), 627. https://doi.org/10.3390/jcm12020627







