Bleeding Complications in COVID-19 Critically Ill ARDS Patients Receiving VV-ECMO Therapy
Abstract
:1. Introduction
2. Materials and Methods
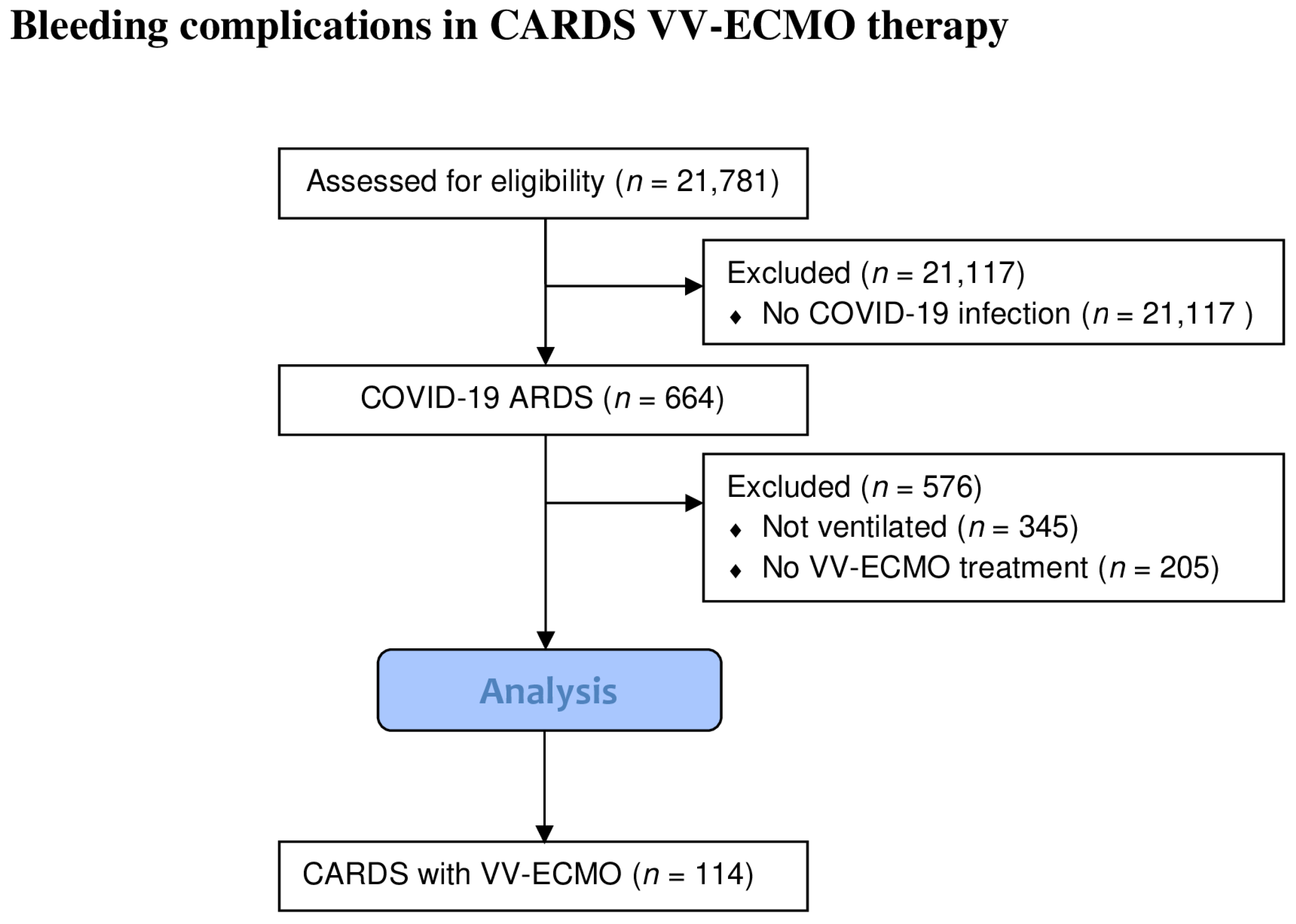
2.1. Patient Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Bleeding Events and Assignment
3.2. Transfusion Therapy
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hill, J.D.; O’Brien, T.G.; Murray, J.J.; Dontigny, L.; Bramson, M.; Osborn, J.; Gerbode, F. Prolonged extracorporeal oxygenation for acute post-traumatic respiratory failure (shock-lung syndrome) use of the Bramson membrane lung. N. Engl. J. Med. 1972, 286, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Mosier, J.M.; Kelsey, M.; Raz, Y.; Gunnerson, K.J.; Meyer, R.; Hypes, C.D.; Malo, J.; Whitmore, S.P.; Spaite, D.W. Extracorporeal membrane oxygenation (ECMO) for critically ill adults in the emergency department: History, current applications, and future directions. Crit. Care 2015, 19, 431. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; Kostousov, V.; Teruya, J. Bleeding and Thrombotic Complications in the Use of Extracorporeal Membrane Oxygenation. Semin. Thromb. Hemost. 2018, 44, 020–029. [Google Scholar] [CrossRef] [PubMed]
- Olson, S.R.; Murphree, C.R.; Zonies, D.; Meyer, A.D.; Mccarty, O.J.T.; Deloughery, T.G.; Shatzel, J.J. Thrombosis and Bleeding in Extracorporeal Membrane Oxygenation (ECMO) Without Anticoagulation: A Systematic Review. ASAIO J. 2021, 67, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Squiers, J.J.; Lima, B.; Dimaio, J.M. Contemporary extracorporeal membrane oxygenation therapy in adults: Fundamental principles and systematic review of the evidence. J. Thorac. Cardiovasc. Surg. 2016, 152, 20–32. [Google Scholar] [CrossRef]
- Ware, J.H. Investigating Therapies of Potentially Great Benefit: ECMO. Stat. Sci. 1989, 4, 298–306. [Google Scholar] [CrossRef]
- Friedrichson, B.; Mutlak, H.; Zacharowski, K.; Piekarski, F. Insight into ECMO, mortality and ARDS: A nationwide analysis of 45,647 ECMO runs. Crit. Care 2021, 25, 38. [Google Scholar] [CrossRef]
- Barbaro, R.P.; Maclaren, G.; Boonstra, P.S.; Iwashyna, T.J.; Slutsky, A.S.; Fan, E.; Bartlett, R.H.; Tonna, J.E.; Hyslop, R.; Fanning, J.J.; et al. Extracorporeal membrane oxygenation support in COVID-19: An international cohort study of the Extracorporeal Life Support Organization registry. Lancet 2020, 396, 1071–1078. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Mostert, C.; Hentschker, C.; Voshaar, T.; Malzahn, J.; Schillinger, G.; Klauber, J.; Janssens, U.; Marx, G.; Weber-Carstens, S.; et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: An observational study. Lancet Respir. Med. 2020, 8, 853–862. [Google Scholar] [CrossRef]
- Ramanathan, K.; Shekar, K.; Ling, R.R.; Barbaro, R.P.; Wong, S.N.; Tan, C.S.; Rochwerg, B.; Fernando, S.M.; Takeda, S.; Maclaren, G.; et al. Extracorporeal membrane oxygenation for COVID-19: A systematic review and meta-analysis. Crit. Care 2021, 25, 211. [Google Scholar] [CrossRef]
- Dreier, E.; Malfertheiner, M.V.; Dienemann, T.; Fisser, C.; Foltan, M.; Geismann, F.; Graf, B.; Lunz, D.; Maier, L.S.; Müller, T.; et al. ECMO in COVID-19—Prolonged therapy needed? A retrospective analysis of outcome and prognostic factors. Perfusion 2021, 36, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Xu, Y.; Liu, D.; Liu, X.; Zhou, L.; Huang, Y.; Li, Y.; Liu, X. Case report: Prolonged VV-ECMO (111 Days) support in a patient with severe COVID-19. Front. Med. 2021, 8, 681548. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, A.L.; Vachharajani, H.H.; Davidson, B.P.; Kruit, N.J.; Eslick, A.T. The Prolonged Use of VV ECMO Support in COVID-19: A Case Report. J. Crit. Care Med. 2020, 6, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Lorusso, R.; De Piero, M.E.; Mariani, S.; Di Mauro, M.; Folliguet, T.; Taccone, F.S.; Camporota, L.; Swol, J.; Wiedemann, D.; Belliato, M.; et al. In-hospital and 6-month outcomes in patients with COVID-19 supported with extracorporeal membrane oxygenation (EuroECMO-COVID): A multicentre, prospective observational study. Lancet Respir. Med. 2022, 11, 151–162. [Google Scholar] [CrossRef]
- Herrmann, J.; Lotz, C.; Karagiannidis, C.; Weber-Carstens, S.; Kluge, S.; Putensen, C.; Wehrfritz, A.; Schmidt, K.; Ellerkmann, R.K.; Oswald, D.; et al. Key characteristics impacting survival of COVID-19 extracorporeal membrane oxygenation. Crit. Care 2022, 26, 190. [Google Scholar] [CrossRef]
- Flinspach, A.N.; Raimann, F.J.; Bauer, F.; Zacharowski, K.; Ippolito, A.; Booke, H. Therapy and Outcome of Prolonged Veno-Venous ECMO Therapy of Critically Ill ARDS Patients. J. Clin. Med. 2023, 12, 2499. [Google Scholar] [CrossRef]
- Sauer, C.M.; Yuh, D.D.; Bonde, P. Extracorporeal Membrane Oxygenation Use Has Increased by 433% in Adults in the United States from 2006 to 2011. ASAIO J. 2015, 61, 31–36. [Google Scholar] [CrossRef]
- Flinspach, A.N.; Booke, H.; Zacharowski, K.; Balaban, Ü.; Herrmann, E.; Adam, E.H. High sedation needs of critically ill COVID-19 ARDS patients—A monocentric observational study. PLoS ONE 2021, 16, e0253778. [Google Scholar] [CrossRef]
- Zaim, S.; Chong, J.H.; Sankaranarayanan, V.; Harky, A. COVID-19 and Multiorgan Response. Curr. Probl. Cardiol. 2020, 45, 100618. [Google Scholar] [CrossRef]
- ATTACC Investigators; ACTIV-4a Investigators; REMAP-CAP Investigators; Lawler, P.R.; Goligher, E.C.; Berger, J.S.; Neal, M.D.; McVerry, B.J.; Nicolau, J.C.; Gong, M.N.; et al. Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 385, 790–802. [Google Scholar] [CrossRef]
- Sadeghipour, P.; Talasaz, A.H.; Rashidi, F.; Sharif-Kashani, B.; Beigmohammadi, M.T.; Farrokhpour, M.; Sezavar, S.H.; Payandemehr, P.; Dabbagh, A.; Moghadam, K.G.; et al. Effect of Intermediate-Dose vs Standard-Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality Among Patients With COVID-19 Admitted to the Intensive Care Unit. JAMA 2021, 325, 1620. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Flinspach, A.N.; Booke, H.; Zacharowski, K.; Balaban, Ü.; Herrmann, E.; Adam, E.H. Associated Factors of High Sedative Requirements within Patients with Moderate to Severe COVID-19 ARDS. J. Clin. Med. 2022, 11, 588. [Google Scholar] [CrossRef] [PubMed]
- Hoyler, M.M.; Flynn, B.; Iannacone, E.M.; Jones, M.-M.; Ivascu, N.S. Clinical Management of Venoarterial Extracorporeal Membrane Oxygenation. J. Cardiothorac. Vasc. Anesth. 2020, 34, 2776–2792. [Google Scholar] [CrossRef]
- Marini, J.J.; Gattinoni, L. Management of COVID-19 Respiratory Distress. JAMA 2020, 323, 2329–2330. [Google Scholar] [CrossRef]
- Kluge, S.; Janssens, U.; Welte, T.; Weber-Carstens, S.; Marx, G.; Karagiannidis, C. German recommendations for critically ill patients with COVID-19. Med. Klin. Intensivmed. und Notfallmedizin 2020, 115, 1–4. [Google Scholar] [CrossRef]
- Guérin, C.; Reignier, J.; Richard, J.-C.; Beuret, P.; Gacouin, A.; Boulain, T.; Mercier, E.; Badet, M.; Mercat, A.; Baudin, O. Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 2013, 368, 2159–2168. [Google Scholar] [CrossRef]
- Alhazzani, W.; Evans, L.; Alshamsi, F.; Moller, M.H.; Ostermann, M.; Prescott, H.C.; Arabi, Y.M.; Loeb, M.; Ng Gong, M.; Fan, E.; et al. Surviving Sepsis Campaign Guidelines on the Management of Adults with Coronavirus Disease 2019 (COVID-19) in the ICU: First Update. Crit. Care Med. 2021, 49, e219–e234. [Google Scholar] [CrossRef]
- Materne, L.A.; Hunsicker, O.; Menk, M.; Graw, J.A. Hemolysis in patients with Extracorporeal Membrane Oxygenation therapy for severe Acute Respiratory Distress Syndrome—A systematic review of the literature. Int. J. Med. Sci. 2021, 18, 1730–1738. [Google Scholar] [CrossRef]
- Schulman, S.; Kearon, C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J. Thromb. Haemost. 2005, 3, 692–694. [Google Scholar] [CrossRef]
- Tran, A.; Fernando, S.M.; Rochwerg, B.; Barbaro, R.P.; Hodgson, C.L.; Munshi, L.; Maclaren, G.; Ramanathan, K.; Hough, C.L.; Brochard, L.J.; et al. Prognostic factors associated with mortality among patients receiving venovenous extracorporeal membrane oxygenation for COVID-19: A systematic review and meta-analysis. Lancet Respir. Med. 2022, 11, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Girelli, D.; Marchi, G.; Busti, F.; Vianello, A. Iron metabolism in infections: Focus on COVID-19. Semin. Hematol. 2021, 58, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Bellmann-Weiler, R.; Lanser, L.; Barket, R.; Rangger, L.; Schapfl, A.; Schaber, M.; Fritsche, G.; Wöll, E.; Weiss, G. Prevalence and Predictive Value of Anemia and Dysregulated Iron Homeostasis in Patients with COVID-19 Infection. J. Clin. Med. 2020, 9, 2429. [Google Scholar] [CrossRef] [PubMed]
- Boissier, E.; Lakhal, K.; Senage, T.; Bizouarn, P.; Lepoivre, T.; Nicolet, J.; Roussel, J.-C.; Rozec, B.; Vourc’h, M.; Bigot-Corbel, E. Haemolysis index: Validation for haemolysis detection during extracorporeal membrane oxygenation. Br. J. Anaesth. 2020, 125, e218–e220. [Google Scholar] [CrossRef] [PubMed]
- George, T.J.; Sheasby, J.; Shih, E.; Lilly, J.C.; Harness-Brumley, C.L.; Taylor, J.E.; Curry, M.W.; Erwin, G.E.; Vaquera, K.A.; Myers, D.P.; et al. Blood Product Utilization in Patients With COVID-19 on ECMO. J. Surg. Res. 2022, 276, 24–30. [Google Scholar] [CrossRef]
- Dell’Era, V.; Dosdegani, R.; Valletti, P.A.; Garzaro, M. Epistaxis in hospitalized patients with COVID-19. J. Int. Med. Res. 2020, 48, 0300060520951040. [Google Scholar] [CrossRef]
- Bathula, S.S.R.; Patrick, T.; Srikantha, L. Epistaxis management on COVID-19–positive patients: Our early case experience and treatment. Clin. Case Rep. 2020, 8, 2195–2198. [Google Scholar] [CrossRef]
- Martucci, G.; Schmidt, M.; Agerstrand, C.; Tabatabai, A.; Tuzzolino, F.; Giani, M.; Ramanan, R.; Grasselli, G.; Schellongowski, P.; Riera, J.; et al. Transfusion practice in patients receiving VV ECMO (PROTECMO): A prospective, multicentre, observational study. Lancet Respir. Med. 2022, 11, 245–255. [Google Scholar] [CrossRef]
- Koeckerling, D.; Pan, D.; Mudalige, N.L.; Oyefeso, O.; Barker, J. Blood transfusion strategies and ECMO during the COVID-19 pandemic. Lancet Respir. Med. 2020, 8, e40. [Google Scholar] [CrossRef]
- Martucci, G.; Grasselli, G.; Tanaka, K.; Tuzzolino, F.; Panarello, G.; Schmidt, M.; Bellani, G.; Arcadipane, A. Hemoglobin trigger and approach to red blood cell transfusions during veno-venous extracorporeal membrane oxygenation: The international TRAIN-ECMO survey. Perfusion 2019, 34, 39–48. [Google Scholar] [CrossRef]
- Posluszny, J.; Rycus, P.T.; Bartlett, R.H.; Engoren, M.; Haft, J.W.; Lynch, W.R.; Park, P.K.; Raghavendran, K.; Napolitano, L.M. Outcome of Adult Respiratory Failure Patients Receiving Prolonged (≥14 Days) ECMO. Ann. Surg. 2016, 263, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Sakusic, A.; Rabinstein, A.A. Cognitive outcomes after critical illness. Curr. Opin. Crit. Care 2018, 24, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Gribensk, A.; Schneider, A.; Gallaher, J.R.; Reid, T.S.; Kindell, D.G.; Charles, A.G.; Raff, L.A. Posthospitalization outcomes after extracorporeal membrane oxygenation (ECMO) for COVID-19. Surgery 2022, 172, 466–469. [Google Scholar] [CrossRef] [PubMed]


| Major Bleeding * | Minor Bleeding | No Bleeding | All | |
|---|---|---|---|---|
| Per patient n = | 23 (20.2%) | 56 (49.1%) | 35 (30.7%) | 114 (100%) |
| Overall | 103 | 2283 | 0 | 2386 |
| sex (male,%) | 20 (87.0%) | 45 (80.4%) | 32 (89.5%) | 97 (85.1%) |
| age (years) | 52 (IQR: 38/66) | 55 (IQR: 40/70) | 52 (IQR: 36/68) | 54 (IQR: 46/62) |
| diabetes mellitus | 4 (17.4%) | 17 (30.4%) | 6 (17.1%) | 27 (23.7%) |
| cardiovascular disease | 0 (0.0%) | 6 (10.7%) | 3 (7.9%) | 9 (7.7%) |
| chronic renal failure | 0 (0.0%) | 3 (5.4%) | 2 (5.3%) | 5 (4.3%) |
| arterial hypertension | 8 (34.8%) | 21 (37.5%) | 14 (36.8%) | 43 (36.8%) |
| smoking | 3 (13.0%) | 7 (1.3%) | 3 (7.9%) | 13 (11.1%) |
| weight | 92.0 (IQR: 74/110) | 92.0 (IQR: 69/115) | 96.0 (IQR: 86/106) | 95.0 (IQR: 81/109) |
| BMI (kg/m2) | 31.0 (IQR: 27/35) | 29.8 (IQR: 21/38.6) | 31.0 (IQR: 22/40) | 30.5 (IQR: 23.4/37.6) |
| mortality | 20 (87.0%) | 33 (58.9%) | 22 (62.9%) | 75 (65.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flinspach, A.N.; Bobyk, D.; Zacharowski, K.; Neef, V.; Raimann, F.J. Bleeding Complications in COVID-19 Critically Ill ARDS Patients Receiving VV-ECMO Therapy. J. Clin. Med. 2023, 12, 6415. https://doi.org/10.3390/jcm12196415
Flinspach AN, Bobyk D, Zacharowski K, Neef V, Raimann FJ. Bleeding Complications in COVID-19 Critically Ill ARDS Patients Receiving VV-ECMO Therapy. Journal of Clinical Medicine. 2023; 12(19):6415. https://doi.org/10.3390/jcm12196415
Chicago/Turabian StyleFlinspach, Armin Niklas, Dorothée Bobyk, Kai Zacharowski, Vanessa Neef, and Florian Jürgen Raimann. 2023. "Bleeding Complications in COVID-19 Critically Ill ARDS Patients Receiving VV-ECMO Therapy" Journal of Clinical Medicine 12, no. 19: 6415. https://doi.org/10.3390/jcm12196415
APA StyleFlinspach, A. N., Bobyk, D., Zacharowski, K., Neef, V., & Raimann, F. J. (2023). Bleeding Complications in COVID-19 Critically Ill ARDS Patients Receiving VV-ECMO Therapy. Journal of Clinical Medicine, 12(19), 6415. https://doi.org/10.3390/jcm12196415






