A Systematic Review of Varying Definitions and the Clinical Significance of Fredet’s Fascia in the Era of Complete Mesocolic Excision
Abstract
:1. Introduction
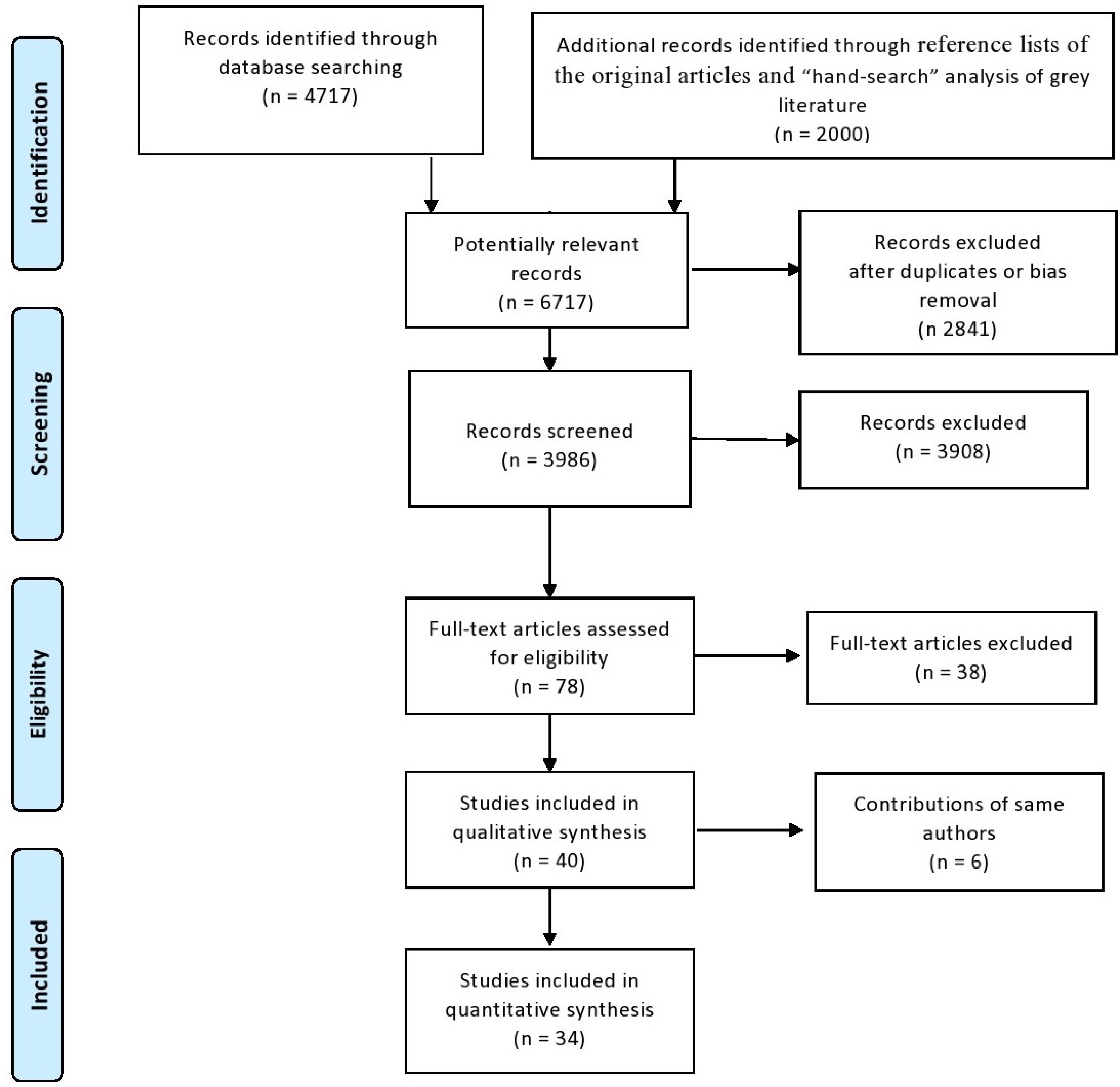
2. Materials and Methods
- “Fredet” on PubMed, WOS, and SCOPUS
- “Fredet’s” and “area” or fascia”, and pancreatectomy” on PubMed, WOS, SCOPUS, Google, and Google Scholar
- “Fredet’s” and “area” or fascia”, and “gastrectomy” on PubMed, WOS, SCOPUS, Google, and Google Scholar
- “Fredet’s” and “area” or fascia”, and “colectomy” on PubMed, WOS, SCOPUS, Google, and Google Scholar
- “Preduodenopancreatic” and “fascia” on PubMed, WOS, SCOPUS, Google, and Google Scholar
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Hohenberger, W.; Weber, K.; Matzel, K.; Papadopoulos, T.; Merkel, S. Standardized surgery for colonic cancer: Complete mesocolic excision and central ligation—Technical notes and outcome. Color. Dis. 2009, 11, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Bertelsen, C.A.; Neuenschwander, A.U.; Jansen, J.E.; Wilhelmsen, M.; Kirkegaard-Klitbo, A.; Tenma, J.R.; Bols, B.; Ingeholm, P.; Rasmussen, L.A.; Jepsen, L.V.; et al. Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: A retrospective, population-based study. Lancet Oncol. 2015, 16, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.F.K.; Kim, S.H. Laparoscopic complete mesocolic excision: West meets East. World J. Gastroenterol. 2014, 20, 14301–14307. [Google Scholar] [CrossRef] [PubMed]
- Treves, F. Lectures on the Anatomy of the Intestinal Canal and Peritoneum in Man. Br. Med. J. 1885, 1, 415–419. [Google Scholar] [CrossRef]
- Culligan, K.; Coffey, J.C.; Kiran, R.P.; Kalady, M.; Lavery, I.C.; Remzi, F.H. The mesocolon: A prospective observational study. Color. Dis. 2012, 14, 421–428. [Google Scholar] [CrossRef]
- Toldt, C. Bau und Wachstumsveraenderungen der Gekroese des menschlichen Darmkanales. Denkschr. Math. Naturwissensch. 1879, 41, 1–56. [Google Scholar]
- Liang, J.-T.; Huang, J.; Chen, T.-C.; Hung, J.-S. The Toldt fascia: A historic review and surgical implications in complete mesocolic excision for colon cancer. Asian J. Surg. 2019, 42, 1–5. [Google Scholar] [CrossRef]
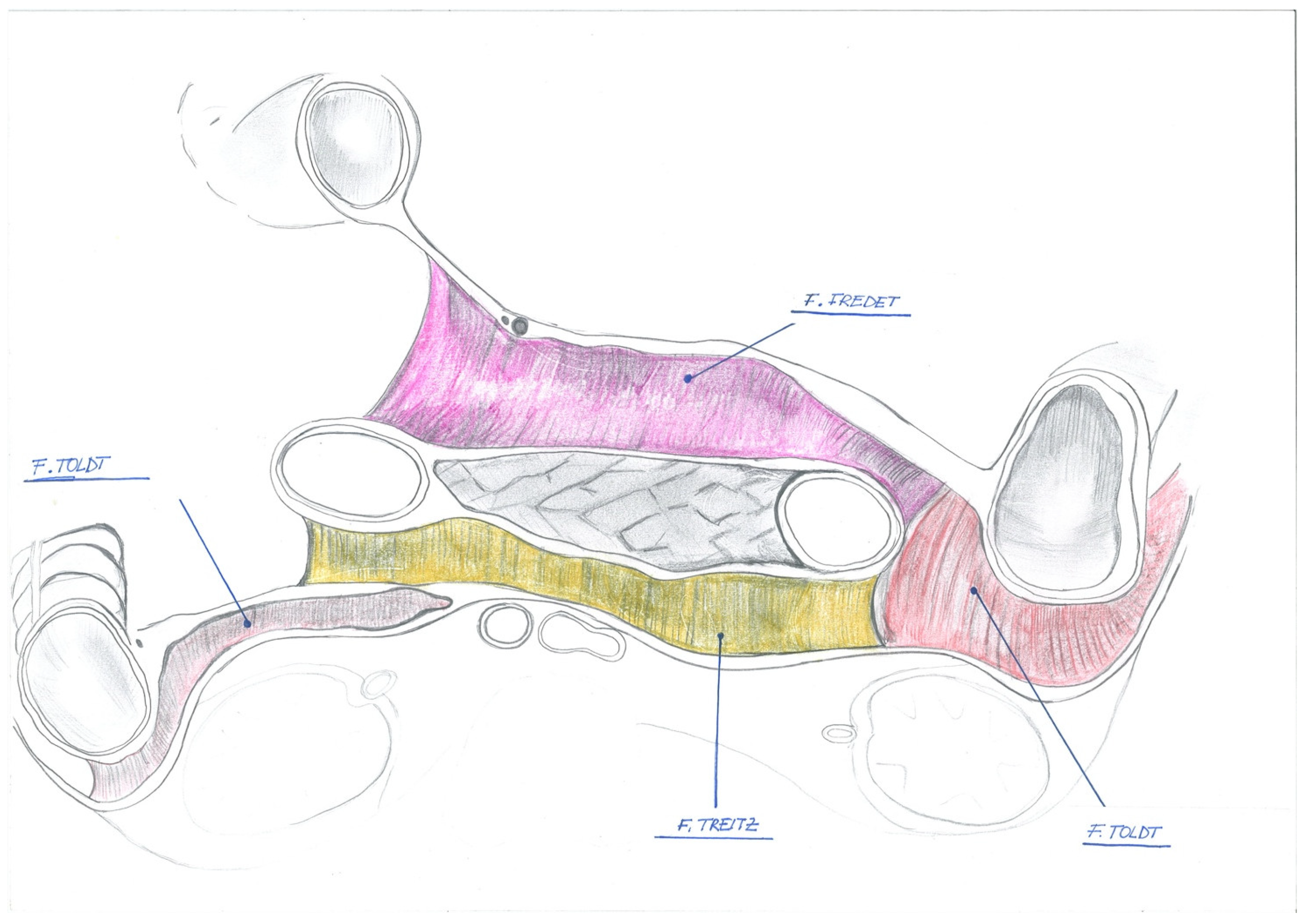
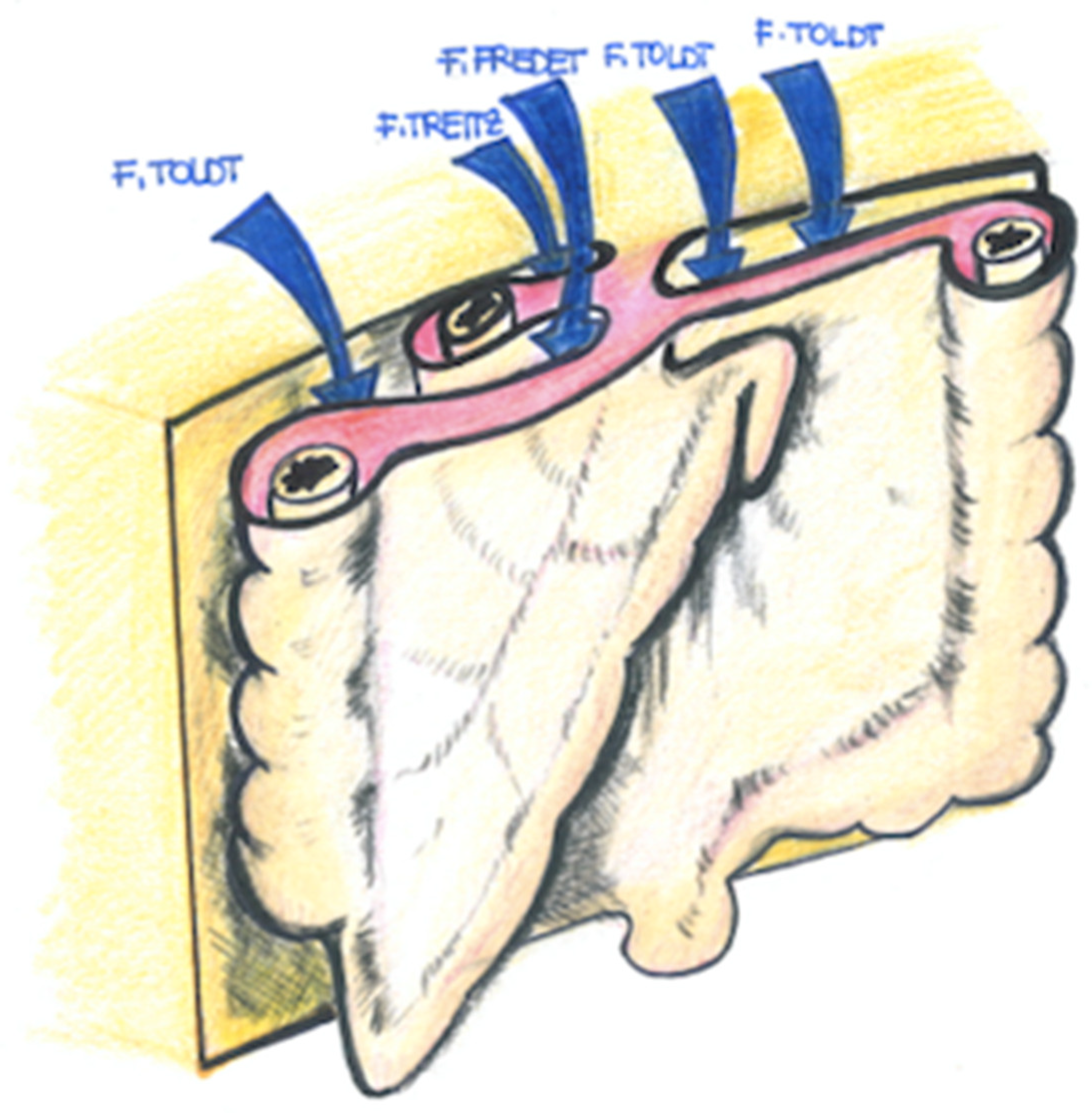
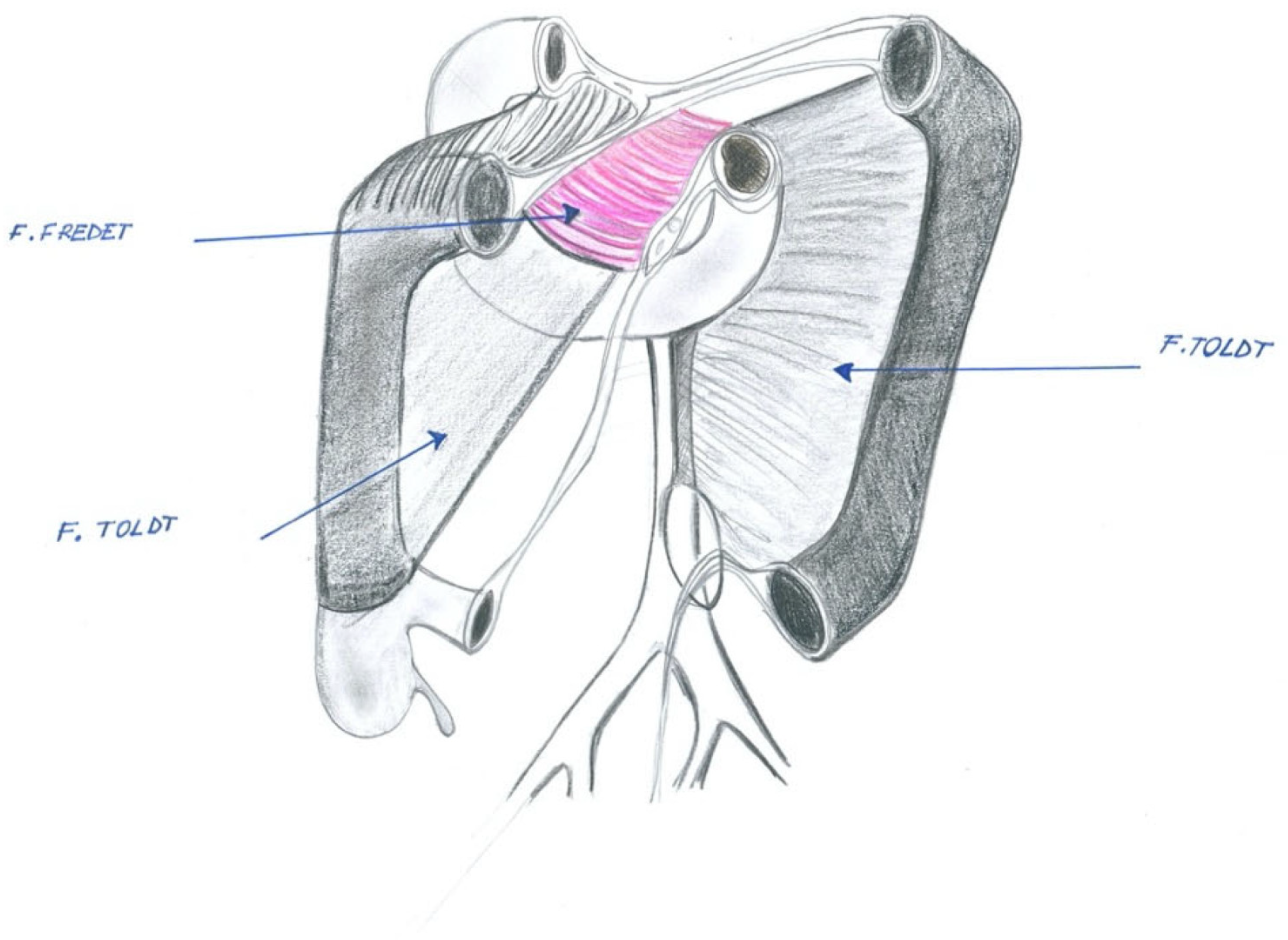
- Garcia-Granero, A.; Pellino, G.; Frasson, M.; Fletcher-Sanfeliu, D.; Bonilla, F.; Sánchez-Guillén, L.; Dolz, A.D.; Romaguera, V.P.; Ortí, L.S.; Martinez-Soriano, F.; et al. The fusion fascia of Fredet: An important embryological landmark for complete mesocolic excision and D3-lymphadenectomy in right colon cancer. Surg. Endosc. 2019, 33, 3842–3850. [Google Scholar] [CrossRef]
- Strey, C.W.; Wullstein, C.; Adamina, M.; Agha, A.; Aselmann, H.; Becker, T.; Grützmann, R.; Kneist, W.; Maak, M.; Mann, B.; et al. Faculty Opinions recommendation of Laparoscopic right hemicolectomy with CME: Standardization using the “critical view” concept. Surg. Endosc. 2018, 32, 5021–5030. [Google Scholar] [CrossRef]
- Esch, J.S.A.; Iosivan, S.-I.; Steinfurth, F.; Mahdi, A.; Förster, C.; Wilkens, L.; Nasser, A.; Sarikaya, H.; Benhidjeb, T.; Krüger, M. A standardized suprapubic bottom-to-up approach in robotic right colectomy: Technical and oncological advances for complete mesocolic excision (CME). BMC Surg. 2019, 19, 72. [Google Scholar] [CrossRef]
- Spinoglio, G.; Bianchi, P.P.; Marano, A.; Priora, F.; Lenti, L.M.; Ravazzoni, F.; Petz, W.; Borin, S.; Ribero, D.; Formisano, G.; et al. Robotic Versus Laparoscopic Right Colectomy with Complete Mesocolic Excision for the Treatment of Colon Cancer: Perioperative Outcomes and 5-Year Survival in a Consecutive Series of 202 Patients. Ann. Surg. Oncol. 2018, 25, 3580–3586. [Google Scholar] [CrossRef] [PubMed]
- Primo Romanguera, V.; Garcia-Granero, A.; Pellino, G. Fascia de coalescencia de Fredet: Nuevo “landmark” embriológico en la escisión completa del mesocolon en cáncer de colon derecho. Cirugía Española 2019, 97, 41. [Google Scholar]
- Siani, L.M.; Lucchi, A.; Berti, P.; Garulli, G. Laparoscopic complete mesocolic excision with central vascular ligation in 600 right total mesocolectomies: Safety, prognostic factors and oncologic outcome. Am. J. Surg. 2017, 214, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Siani, L.M.; Garulli, G. The importance of the mesofascial interface in complete mesocolic excision. Surgeon 2017, 15, 240–249. [Google Scholar] [CrossRef]
- Spinoglio, G.; Marano, A.; Bianchi, P.P.; Priora, F.; Lenti, L.M.; Ravazzoni, F.; Formisano, G. Robotic Right Colectomy with Modified Complete Mesocolic Excision: Long-Term Oncologic Outcomes. Ann. Surg. Oncol. 2016, 23, 684–691. [Google Scholar] [CrossRef]
- Formisano, G.; Misitano, P.; Giuliani, G.; Calamati, G.; Salvischiani, L.; Bianchi, P.P. Laparoscopic versus robotic right colectomy: Technique and outcomes. Updat. Surg. 2016, 68, 63–69. [Google Scholar] [CrossRef]
- Cutini, G.; Falsetti, F.; Caracino, V.; Coletta, P. Total and subtotal D2 laparoscopic gastrectomy. In Total, Subtotal and Proximal Gastrectomy in Cancer; Siquini, W., Ed.; Springer: Milano, Italy, 2016; pp. 157–186. [Google Scholar]
- Siani, L.M.; Garulli, G. Laparoscopic complete mesocolic excision with central vascular ligation in right colon cancer: A comprehensive review. World J. Gastrointest. Surg. 2016, 8, 106–114. [Google Scholar] [CrossRef]
- Aseni, P.; Mariani, A.; De Carlis, R.; Buscemi, V.E.; Concone, G. Detailed abdominal organ inspection and early surgical steps for abdominal organ procurement. In Multiorgan Procurement for Transplantation; Aseni, P., Grande, A., De Carlis, L., Eds.; Springer: Cham, Switzerland, 2016; pp. 109–122. [Google Scholar]
- Siani, L.M.; Pulica, C. Laparoscopic Complete Mesocolic Excision with Central Vascular Ligation in right colon cancer: Long-term oncologic outcome between mesocolic and non-mesocolic planes of surgery. Scand. J. Surg. 2015, 104, 219–226. [Google Scholar] [CrossRef]
- Galindo, F. (Ed.) Resecciones Pancreaticas. In Enciclopedica Cirurgia Digestiva; Sociedad Argentina de Cirugía Digestiva; Buenos Aires, Buenos Aires, 2015; pp. 1–40. Available online: https://sacd.org.ar/wp-content/uploads/2020/05/IV-487-ESECCIONES-PANCREATICAS.pdf (accessed on 12 May 2023).
- Leroy, J.; Melani, A.; Marescaux, J. Laparoscopic Sigmoidectomy for Benign Diverticular Disease. 2014. Available online: http://www.websurg.com/doi-vd01en3910.htm (accessed on 12 May 2023).
- Trastulli, S.; Desiderio, J.; Farinacci, F.; Ricci, F.; Listorti, C.; Cirocchi, R.; Boselli, C.; Noya, G.; Parisi, A. Robotic right colectomy for cancer with intracorporeal anastomosis: Short-term outcomes from a single institution. Int. J. Color. Dis. 2013, 28, 807–814. [Google Scholar] [CrossRef]
- Yoo, J.S.; Pryor, A.D. Surgical techniques: Distal pancreasectomy. In Contemporary Surgical Management of Liver, Biliary Tract and Pancreatic Disease; Blazer, D.G., III, Kuo, P.C., Pappas, T., Clary, B.M., Eds.; World Scientific: Singapore, 2019; pp. 607–620. [Google Scholar]
- Topgul, K.; Yururker, S.S.; Koca, B.; Kesicioglu, T. Spleen-preserving laparoscopic distal pancreatectomy: Two cases and review of the technique. Ulus Cerrahi Derg. 2013, 29, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-X.; Huang, C.-M.; Zheng, C.-H.; Li, P.; Xie, J.-W.; Wang, J.-B.; Lu, J. Laparoscopy-assisted gastrectomy with D2 lymph node dissection for advanced gastric cancer without serosa invasion: A matched cohort study from South China. World J. Surg. Oncol. 2013, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Ruotolo, F. Surgical significance of Fredet’s area. G. Chir. 2012, 33, 205–208. [Google Scholar] [PubMed]
- Vasiliadis, K.; Papavasiliou, X.; Delivorias, I.; Paralikodi, D.; Makridis, X. Gastrocolic trunk of Henle. Surg. Chron. 2012, 17, 127–132. [Google Scholar]
- Vasiliadis, K.; Papavassiliou, X.; Delivorias, I.I.; Makridis, C. Surgical approaches to superior mesenteric artery, and periampullary cancer resectability. Surg. Chron. 2012, 19, 10–20. [Google Scholar]
- Roscio, F.; Bertoglio, C.; De Luca, A.; Frattini, P.; Scandroglio, I. Totally laparoscopic versus laparoscopic assisted right colectomy for cancer. Int. J. Surg. 2012, 10, 290–295. [Google Scholar] [CrossRef]
- D’Annibale, A.; Pernazza, G.; Pende, V.; Monsellato, I. Minimally Invasive Robot–Assisted Colorectal Resections. In Colorectal Cancer—From Prevention to Patient Care; Ettarh, R., Ed.; InTech: Rijeka, Croatia, 2012; pp. 521–538. [Google Scholar]
- Pugliese, R. Total and subtotal miniinvasive gastrectomy. In Surgery in the Multimodal Management of Gastric Cancer; De Manzoni, G., Roviello, F., Siquini, W., Eds.; Springer: Cham, Switzerland, 2012; pp. 251–264. [Google Scholar]
- Shuang, J.; Qi, S.; Zheng, J.; Zhao, Q.; Li, J.; Kang, Z.; Hua, J.; Du, J. A case–control study of laparoscopy-assisted and open distal gastrectomy for advanced gastric cancer. J. Gastrointest. Surg. 2011, 15, 57–62. [Google Scholar] [CrossRef]
- Milivoje, V.; Dragan, K.; Nebojsa, M.; Vesna, V. Fredet’s Fascia. Anatomy 2010, 4, 53–91. [Google Scholar]
- Benzoni, C.; Benini, B.; Pirozzi, C. Intestinal derotation in emergency surgery. Eur. J. Trauma Emerg. Surg. 2010, 36, 495–498. [Google Scholar] [CrossRef]
- D’annibale, A.; Pernazza, G.; Morpurgo, E.; Monsellato, I.; Pende, V.; Lucandri, G.; Termini, B.; Orsini, C.; Sovernigo, G. Robotic right colon resection: Evaluation of first 50 consecutive cases for malignant disease. Ann. Surg. Oncol. 2010, 17, 2856–2862. [Google Scholar] [CrossRef]
- Ocampo, C.; Zandalazini, H. Anatomia quirurgica del pancreas. Cirurgia Digestiva 2009, IV-468, 1–6. [Google Scholar]
- Casadei, R.; Ricci, C.; Antonacci, N.; Minni, F. Indications and Technique of Central Pancreatectomy. In Surgical Treatment of Pancreatic Diseases; Siquini, W., Ed.; Springer: Cham, Switzerland, 2008; pp. 329–336. [Google Scholar] [CrossRef]
- Huscher, C.; Marescaux, J. Laparoscopic Right Colectomy in an Obese Patient with a Dysplastic Adenoma; E Publication WebSurg.com. 2009. Available online: http://websurg.com/doi/vd01en2498 (accessed on 12 May 2023).
- Valle, M.; Federici, O.; Tarantino, E.; Corona, F.; Garofalo, A. Laparoscopic intestinal derotation: Original technique. Surg. Laparosc. Endosc. Percutan. Tech. 2009, 19, e80–e84. [Google Scholar] [CrossRef] [PubMed]
- Hüscher, C.G.S.; Ponzano, C.; Di Paola, M. Laparoscopic management of pancreatic neoplasms. In Diseases of the Pancreas: Current Surgical Therapy; Beger, H.G., Matsuno, S., Cameron, J.L., Eds.; Springer: Berlin, Germany, 2008; pp. 653–658. [Google Scholar]
- Pugliese, R.; Boniardi, M.; de Carli, S.; Sansonna, F.; Costanzi, A.; Maggioni, D.; Ferrari, G.C.; Di Lernia, S.; Loli, P.; Grossrubatscher, E.; et al. Laparoscopic bilateral simultaneous adrenalectomy: Results of 11 operations. J. Laparoendosc. Adv. Surg. Tech. A 2008, 18, 588–592. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, R.; Maggioni, D.; Sansonna, F.; Scandroglio, I.; Ferrari, G.C.; Di Lernia, S.; Costanzi, A.; Pauna, J.; de Martini, P. Total and subtotal laparoscopic gastrectomy for adenocarcinoma. Surg. Endosc. 2007, 21, 21–27. [Google Scholar] [CrossRef]
- Talamini, M.A. (Ed.) Laparoscopic pancreatic resection. In Advanced Therapy in Minimally Invasive Surgery; BC Decker: Hamilton, ON, Canada, 2006; pp. 206–210. [Google Scholar]
- Maldovanu, R. Duodenopancreatectomia cefalică. Jurnalul de Chirurgie 2005, 1, 307–325. [Google Scholar]
- Natale, F.; Maffei, F.; Natale, C. Surgery of carcinoma of the transverse colon. G. Chir. 2005, 26, 177–186. [Google Scholar]
- Ruotolo, F.; Sgarzini, G.; Ipri, M.; Mereu, A.; Hüscher, C.G.S. Surgical anatomy. In Trasverse Colon; Hüscher, C.G.S., Ed.; Surgical Video Production: Padova, Italia, 2002; pp. 11–47. [Google Scholar]
- Siani, L.M. Laparoscopic Right Colectomy with CME and CLV (Total Right Mesocolectomy). In Advanced Laparoscopy. Available online: http://www.smgebooks.com/advanced-laparoscopy/chapters/ALAP-16-06.pdf (accessed on 15 July 2020).
- Wedel, T.; Heimke, M.; Fletcher, J.; Miskovic, D.; Benz, S.; Stelzner, S.; Heinze, T. The retrocolic fascial system revisited for right hemicolectomy with complete mesocolic excision based on anatomical terminology: Do we need the eponyms Toldt, Gerota, Fredet and Treitz? Color. Dis. 2022, 25, 764–774. [Google Scholar] [CrossRef]
- Peltrini, R.; Di Nuzzo, M.M.; Caricato, C.; Bracale, U.; Corcione, F. The “complete common mesentery” and the agenesis of Toldt’s and Fredet’s fasciae. Surg. Radiol. Anat. 2021, 43, 1437–1439. [Google Scholar] [CrossRef]
- Tebala, G.D.; Di Saverio, S.; Gallo, G.; Cirocchi, R.; Milani, M.S.; Bond-Smith, G. Importance of the Duodenal Window and Fredet’s Fascia in Laparoscopic Right Hemicolectomy: Technical Note. Surg. Technol. Int. 2021, 39, 173–175. [Google Scholar] [CrossRef]
- Matsuda, T.; Yamashita, K.; Hasegawa, H.; Utsumi, M.; Kakeji, Y. Current status and trend of laparoscopic right hemicolectomy for colon cancer. Ann. Gastroenterol. Surg. 2020, 4, 521–527. [Google Scholar] [CrossRef]
- Lin, L.; Yuan, S.-B.; Guo, H. Does cranial-medial mixed dominant approach have a unique advantage for laparoscopic right hemicolectomy with complete mesocolic excision? World J. Gastrointest. Surg. 2022, 14, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Testut, L.; Latarjet, A. Trattato di Anatomia Umana; Edra: Palm Beach Garden, FL, USA, 2017; p. 5740. ISBN 9788821445378. [Google Scholar]
- Federative Committee on Anatomical Terminology—FCAT. Terminologia Anatomica—International Anatomical Terminology; Thieme: Stuttgart, Germany, 1998. [Google Scholar]
| Author, Year of Publication | Observational Study | Chapter of Book | Narrative Review | Case Report | Technical Note |
|---|---|---|---|---|---|
| Lin 2022 [54] | X | ||||
| Wedel 2022 [50] | X | ||||
| Tebala 2021 [52] | X | ||||
| Peltrini 2021 [51] | X | ||||
| Matsuda 2020 [53] | X | ||||
| Garcia-Granero 2019 [9] | X | ||||
| Primo Romaguera 2019 [13] | X | ||||
| Spinoglio 2018 [12] | X | ||||
| Siani 2017 [14] | X | ||||
| Siani 2017 [15] | X | ||||
| Spinoglio 2016 [16] | X | ||||
| Formisano 2016 [17] | X | ||||
| Cutini 2016 [18] | X | ||||
| Siani 2016 [19] | X | ||||
| Aseni 2016 [20] | X | ||||
| Siani 2015 [21] | X | ||||
| Galindo 2015 [22] | X | ||||
| Leroy 2014 [23] | X | ||||
| Trastulli 2013 [24] | X | ||||
| Yoo 2019 [25] | X | ||||
| Topgül 2013 [26] | X | ||||
| Lin 2013 [27] | X | ||||
| Ruotolo 2012 [28] | X | ||||
| Vasiliadis 2012 [29] | X | ||||
| Roscio 2012 [31] | X | ||||
| D’Annibale 2012 [32] | X | ||||
| Pugliese 2012 [33] | X | ||||
| Vasiliadis 2012 [30] | X | ||||
| Shuang 2011 [34] | X | ||||
| Milivoje 2010 [35] | X | ||||
| Benzoni 2010 [36] | X | ||||
| D’Annibale 2010 [37] | X | ||||
| Ocampo 2009 [38] | X | ||||
| Casadei 2009 [39] | X | ||||
| Huscher 2009 [40] | X | ||||
| Valle 2009 [41] | X | ||||
| Huscher 2008 [42] | X | ||||
| Pugliese 2008 [43] | X | ||||
| Pugliese 2007 [44] | X | ||||
| Talamini 2006 [45] | X | ||||
| Madovanu 2005 [46] | X | ||||
| Natale 2005 [47] | X | ||||
| Ruotolo 2002 [48] | X | ||||
| Siani [49] | X | ||||
| Total | 17 | 12 | 10 | 3 | 3 |
| Author, Year of Publication | Fredet’s Fascia | Fredet Pre-Duodenal Pancreatic Fascia | Fredet’s Area | Pre-Duodenal Pancreatic Sub-Mesocolic Fredet Fascia | Fredet’s Right Transverse Mesocolon Fascia | Duodeno-Pancreatic Sub-Mesocolic Fascia |
|---|---|---|---|---|---|---|
| Lin 2022 [54] | X | |||||
| Wedel 2022 [50] | X | X | X | |||
| Tebala 2021 [52] | X | |||||
| Peltrini 2021 [51] | X | |||||
| Matsuda 2020 [53] | X | |||||
| Garcia-Granero 2019 [9] | X | |||||
| Primo Romaguera 2019 [13] | X | |||||
| Spinoglio 2018 [12] | X | |||||
| Siani 2017 [14] | X | |||||
| Siani 2017 [15] | X | |||||
| Spinoglio 2016 [16] | X | |||||
| Formisano 2016 [17] | X | |||||
| Cutini 2016 [18] | ||||||
| Siani 2016 [19] | X | |||||
| Aseni 2016 [20] | X | X | ||||
| Siani 2015 [21] | X | |||||
| Galindo 2015 [22] | X | |||||
| Leroy 2014 [23] | X | |||||
| Trastulli 2013 [24] | X | |||||
| Yoo 2019 [25] | X | |||||
| Topgül 2013 [26] | X | |||||
| Lin 2013 [27] | X | |||||
| Ruotolo 2012 [28] | X | X | X | |||
| Vasiliadis 2012 [29] | X | |||||
| Roscio 2012 [31] | X | |||||
| D’Annibale 2012 [32] | X | |||||
| Pugliese 2012 [33] | X |
| Definition Reported of Fredet’s Fascia | Below the Root of the Mesocolon, the Fusion of the Inferior Lining of the Right Transverse Mesocolon to the Ventral Surface of the Pancreas (Pre-Duodenal Pancreatic Peritoneum) | Below the Root of the Mesocolon, the Fusion of the Inferior Lining of the Transverse Mesocolon (Right and Left) to the Ventral Surface of the Pancreas (Body and Tail) |
| Author, year of publication | Lin 2022 [54] Wedel 2022 [50] Tebala 2021 [52] Peltrini 2021 [51] Matsuda 2020 [53] Garcia-Granero 2019 [9] Primo Romaguera 2019 [13] Ruotolo 2012 [28] Ocampo 2009 [37] Huscher 2008 [42] Natale 2005 [47] Ruotolo 2002 [48] | Leroy 2014 [23] Yoo 2019 [25] Topgül 2013 [26] |
| Author, Year of Publication | Indication of Surgical Procedures | Fredet’s Area or Fascia |
|---|---|---|
| Lin 2022 [54] | Right colectomy | “The surgeon first dissected the fusion fascia in the innermost area adjacent to the gastric antrum, entered the dorsal side of the fusion fascia of Fredet, and then gently expanded the surgical plane between the fusion fascia of Fredet and the visceral duodenal-pancreatic peritoneum in a medial-to-lateral direction” |
| Wedel 2022 [50] | Right colectomy | “The mesocolic fascia was attached to the parietal peritoneal fascia (‘fascia of Toldt’) along the parieto–mesocolic interface, and further cranially to the pre-duodenopancreatic fascia along the mesocolic–duodenopancreatic interface (‘space of Fredet’)” |
| Tebala 2021 [52] | Right colectomy | “After the Duodenal Window is opened, Fredet’s and Toldt’s fasciae are dissected, usually in a bloodless fashion, and can be extended up to the lateral Toldt’s line, to the hepatic flexure and to the gastroepiploic vessels, thus allowing complete preparation of the right mesocolon”. |
| Garcia-Granero 2019 [9] | Right colectomy | “Fusion fascia of Fredet: adhesion plane between visceral peritoneum of the mesocolon of ascending colon and hepatic colonic flexure and the visceral peritoneum of duodenum and pancreas” |
| Primo Romaguera 2019 [13] | Duodenopancreatectomy | “La fascia de Fredet, coalescencia entre el mesocolon ascendente y el peritoneo visceral duodeno-pancreático” |
| Cutini 2016 [18] | Gastrectomy | “During this maneuver the assistant’s grasper pulls up the great curvature of the antropyloric region while the surgeon, dissecting Fredet’s area, exposes the superior mesenteric vein” |
| Aseni 2016 [20] | Transplantation | “The correct line of dissection continues among Gerota’s fascia, Toldt’s fascia, and the preduodenopancreatic fascia or Fredet’s area” |
| Lin 2013 [27] | Gastrectomy | “The dissection moved to the hepatic flexure and the pylorus. The right gastroepiploicvein was divided between titanium clips flush with theHenle’s trunk and ended up in the Fredet area, wheregroup 14v was removed” |
| Ruotolo 2012 [28] | Surgical anatomy | “Below the root of the mesocolon, the fusion of the primary preduodenopancreatic peritoneum (anterior mesoduodenum) with the lower leaflet of the right transverse mesocolon generates the submesocolicpreduodenopancreatic fascia or Fredet’s area” |
| Pugliese 2012, 2007 [33,44] | Right colectomy | “The right gastroepiploic artery is sectioned at its origin from the gastroduodenal artery, just above the pancreatic head. This allows clearance of station 6 and of Fredet’s area, where lymph node station 14v is removed” |
| Shuang 2011 [34] | Right colectomy | “The right gastroepiploic vein was divided between titanium clips flush with the Henle’s trunk and ended up in the Fredet area, where group 14v was removed”. |
| Surgical Step | Surgical Relevance of Fredet’s Fascia | Author |
|---|---|---|
| Robotic/Laparoscopic Right Colectomy | ||
| “A complete mesocolic excision is performed by dissecting along the plane between the intact dorsal mesocolon of the hepatic flexure and the Fredet preduodenopancreatic fascia” | “The dissection is sharp in this area This plane is bloodless (completely avascular)” | Lin 2022 [54] Wedel 2022 [50] Tebala 2021 [52] Garcia-Granero 2019 [9] Primo Romaguera 2019 [13] Spinoglio 2018, 2016 [12,16] Formisano 2016 [17] Siani (2015–2017) [14,19,21] Huscher 2009 [40] |
| Duodenopancreatectomy | ||
| “Dissection along the plane of the area of Fredet allows the exposure of the anterior aspect of the head of pancreas dorsal to the mesentery root, the second portion of duodenum below the papilla of Vater and the third and fourth portions of duodenum This maneuver is also one of the main steps of the Cattel-Braash maneuver” | “Dissection of the fascia of Fredet is certainly more challenging if compared with dissection along the right side of Toldt and the fascia of Trietz” | Galindo 2015 [22] Talamini 2006 [45] |
| “Fredet’s fascia is left intact during the dissection” | “Enbloc”resection of the pancreatic head covered anteriorly by Fredet’s fascia and posteriorly by Treitz’s fascia | Huscher 2009 [40] |
| Laparoscopic gastrectomy | ||
| “The gastrocolic ligament is divided along the border of the transverse colon and the dissection moved to the hepatic flexure and the pylorus at area of Fredet” | “The dissection of Fredet’s area exposes the superior mesenteric vein. The dissection proceeds in order to identify the right colic vein, the gastroepiploic vein, and Henle’s trunk. In this manner the nodes of 14v station are removed, and the right gastroepiploic vein is clipped and sectioned” | Cutini 2016 [18] Shuang 2011 [34] |
| Author, Year of Publication | Vascular Landmarks | Type of Surgery |
|---|---|---|
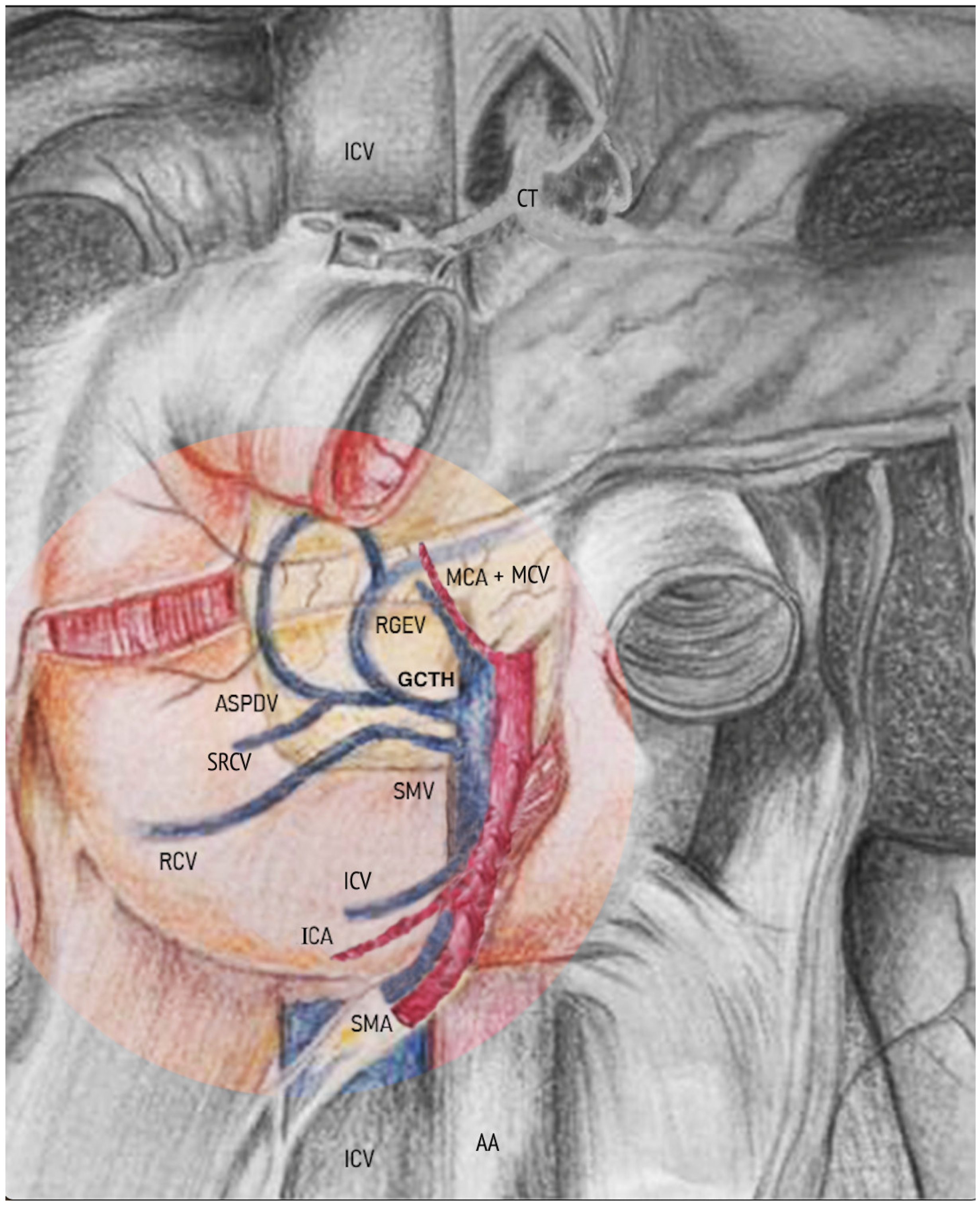
| Lin 2022 [54] | “Using the projection of the superior right colic vein (SRCV) on the fusion fascia of Fredet as a landmark, the surgical plane was expanded medially to expose the gastrocolic trunk of Henle (GCTH), and the nonvascularized mesocolic area was expanded on the left side of the root of the middle colonic vessels, completing the dissection of the surgical area of the GCTH [14,15] (SAGCTH), defined as the area of the superior mesenteric vein (SMV) located at the head of the pancreas and including the venous confluence of the right gastroepiploic vein (RGEV), anterosuperior pancreaticduodenal vein (ASPV), and SRCV” | Laparoscopic right colectomy |
| Tebala 2021 [52] | “Fredet’s fascia is an important landmark during anatomical mesocolic dissection of the right and proximal transverse colon and its preparation is one of the most challenging steps of this manoeuvre, mostly due to the risk of bleeding from the small tributaries to the superior mesenteric vein, including Henle’s trunk” | Laparoscopic right colectomy |
| Matsuda 2020 [53] | “Fusion fascia of Fredet as an essential embryological landmark during LRH, which corresponds to the plane between the ascending mesocolon and the visceral duodenal-pancreatic peritoneum” | Laparoscopic right colectomy |
| Garcia-Granero 2019 [9] | “We found that the medial limit of the fascia of Fredet is represented by the SMV and GCTH. In fact, the dissection of the fascia of Fredet allowed us to enter this area safer, with better exposure, and it offered a correct mesocolic plane, thus reducing the risk of injuries and bleeding from the SMV. The optimal knowledge of this anatomical landmark is crucial to avoid injuries to the SMV, which can lead to life-threatening complications” | Laparoscopic right colectomy |
| Primo Romaguera 2019 [13] | “The anatomical knowledge of Fredet’s fascia is necessary to achieve D3-lymphadenectomy in right colon cancer and can reduce the risk of postoperative complications” | Laparoscopic right colectomy |
| Cutini 2016 [18] | “The same manner the surgeon completes coloepiploic detachment moving the dissection toward the pylorus and achieving the lymphadenectomy of station 4a. During this maneuver the assistant’s grasper pulls up the great curvature of the antropyloric region while the surgeon, dissecting Fredet’s area, exposes the superior mesenteric vein. The dissection proceeds in order to identify the right colic vein, the gastroepiploic vein, and Henle’s trunk. In this manner the nodes of 14v station are removed, and the right gastroepiploic vein is clipped and sectioned” | Laparoscopic gastrectomy |
| Lin 2013 [27] | “The right gastroepiploic vein was divided between titanium clips flush with the Henle’s trunk and ended up in the Fredet area, where group 14v was removed” | Laparoscopic gastrectomy |
| Pugliese 2012, 2007 [33,44] Shuang 2011 [34] | “The right gastroepiploic artery is sectioned at its origin from the gastroduodenal artery, just above the pancreatic head. This allows clearance of station 6 and of Fredet’s area, where lymph node station 14v is removed” | Laparoscopic gastrectomy |
| Huscher 2008 [42] | “The only opening in Fredet’s fascia is right before the superior mesenteric vein (SMV), at the level where the Henle (grastro omental) trunk merges into the vein” | Duodenopancreatectomy |
| Moldovanu 2005 [46] | “The head of the pancreas has relations with the gastroduodenal arteries, the superior pancreaticoduodenal artery, the right gastroepiploic, the superior right colic and with the Fredet fascia” | Duodenopancreatectomy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brachini, G.; Cirillo, B.; Matteucci, M.; Cirocchi, R.; Tebala, G.D.; Cavaliere, D.; Giacobbi, L.; Papa, V.; Solaini, L.; Avenia, S.; et al. A Systematic Review of Varying Definitions and the Clinical Significance of Fredet’s Fascia in the Era of Complete Mesocolic Excision. J. Clin. Med. 2023, 12, 6233. https://doi.org/10.3390/jcm12196233
Brachini G, Cirillo B, Matteucci M, Cirocchi R, Tebala GD, Cavaliere D, Giacobbi L, Papa V, Solaini L, Avenia S, et al. A Systematic Review of Varying Definitions and the Clinical Significance of Fredet’s Fascia in the Era of Complete Mesocolic Excision. Journal of Clinical Medicine. 2023; 12(19):6233. https://doi.org/10.3390/jcm12196233
Chicago/Turabian StyleBrachini, Gioia, Bruno Cirillo, Matteo Matteucci, Roberto Cirocchi, Giovanni Domenico Tebala, Davide Cavaliere, Lorenza Giacobbi, Veronica Papa, Leonardo Solaini, Stefano Avenia, and et al. 2023. "A Systematic Review of Varying Definitions and the Clinical Significance of Fredet’s Fascia in the Era of Complete Mesocolic Excision" Journal of Clinical Medicine 12, no. 19: 6233. https://doi.org/10.3390/jcm12196233
APA StyleBrachini, G., Cirillo, B., Matteucci, M., Cirocchi, R., Tebala, G. D., Cavaliere, D., Giacobbi, L., Papa, V., Solaini, L., Avenia, S., D’Andrea, V., Davies, J., Fedeli, P., & De Santis, E. (2023). A Systematic Review of Varying Definitions and the Clinical Significance of Fredet’s Fascia in the Era of Complete Mesocolic Excision. Journal of Clinical Medicine, 12(19), 6233. https://doi.org/10.3390/jcm12196233









