Good Mid-Term Implant Survival of a Novel Single-Design Rotating-Hinge Total Knee Arthroplasty
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Definitions
2.4. Surgical Procedures and Implant Features
2.5. Statistical Analysis
3. Results
3.1. Revisions
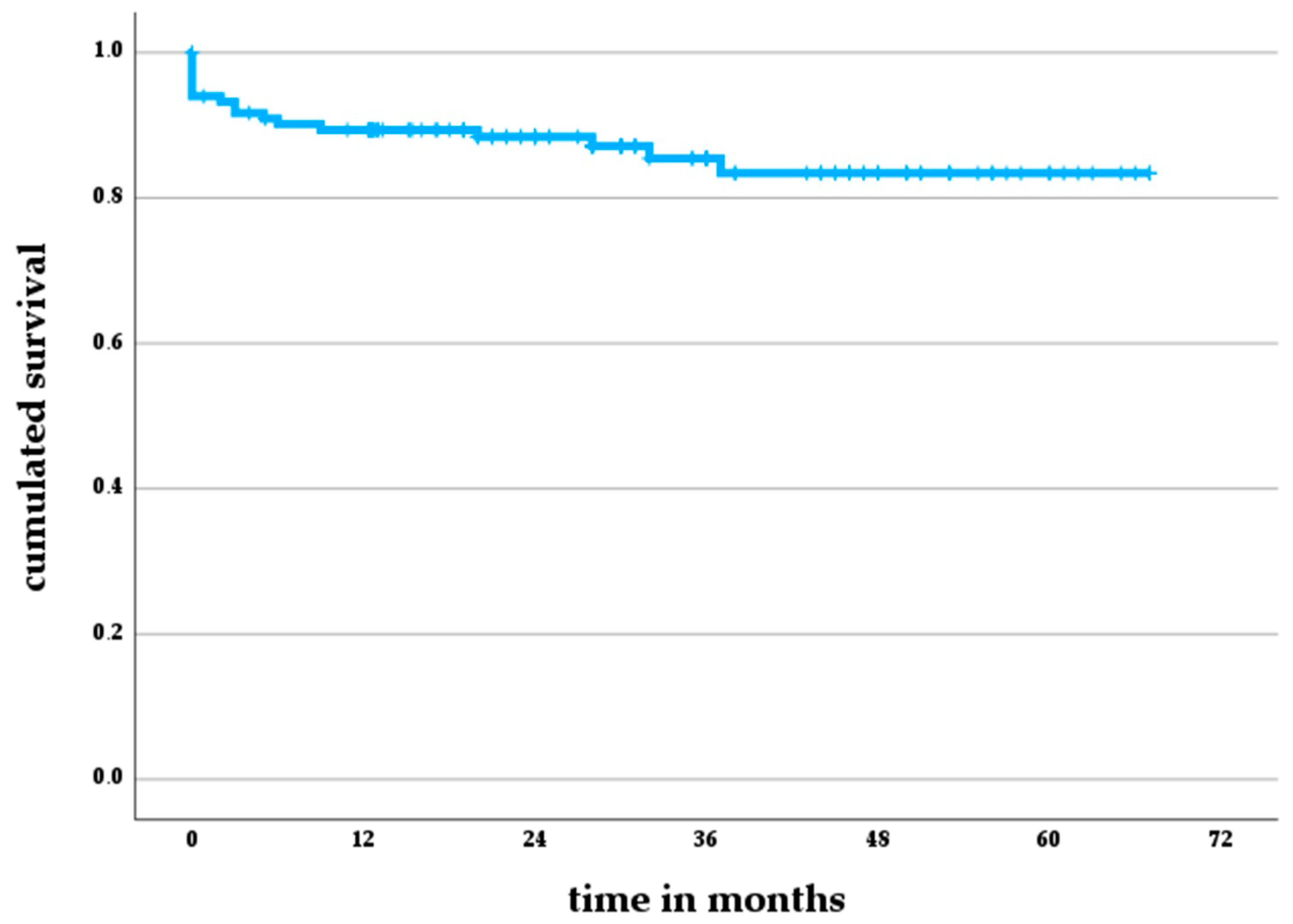
3.2. Revision-Free Survival
3.3. Results after Two-Stage Exchange for PJI
3.4. Risk Factors for Revision
3.5. Functional Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moldovan, F.; Moldovan, L.; Bataga, T. A Comprehensive Research on the Prevalence and Evolution Trend of Orthopedic Surgeries in Romania. Healthcare 2023, 11, 1866. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, T.; Kendoff, D.; Haasper, C. The role of hinges in primary total knee replacement. Bone Jt. J. 2014, 96-B, 93–95. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, J.; Zmistowski, B.; Berbari, E.F.; Bauer, T.W.; Springer, B.D.; Della Valle, C.J.; Garvin, K.L.; Mont, M.A.; Wongworawat, M.D.; Zalavras, C.G. New Definition for Periprosthetic Joint Infection: From the Workgroup of the Musculoskeletal Infection Society. Clin. Orthop. Relat. Res. 2011, 469, 2992–2994. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.H.; Gad, B.V.; Klika, A.K.; Styron, J.F.; Joyce, T.A.; Barsoum, W.K. Comparison of Mechanical and Nonmechanical Failure Rates Associated With Rotating Hinged Total Knee Arthroplasty in Nontumor Patients. J. Arthroplast. 2013, 28, 62–67.e1. [Google Scholar] [CrossRef]
- Pala, E.; Trovarelli, G.; Calabrò, T.; Angelini, A.; Abati, C.N.; Ruggieri, P. Survival of Modern Knee Tumor Megaprostheses: Failures, Functional Results, and a Comparative Statistical Analysis. Clin. Orthop. Relat. Res. 2015, 473, 891–899. [Google Scholar] [CrossRef]
- Chaudhry, H.; MacDonald, S.J.; Howard, J.L.; Lanting, B.A.; McCalden, R.W.; Naudie, D.D.; Vasarhelyi, E.M. Indications, Survivorship, and Clinical Outcomes of a Rotating Hinge Total Knee and Distal Femoral Arthroplasty System. J. Arthroplast. 2020, 35, 1323–1327. [Google Scholar] [CrossRef]
- E Inglis, A.; Walker, P.S. Revision of failed knee replacements using fixed-axis hinges. Bone Jt. Surg. Br. 1991, 73, 757–761. [Google Scholar] [CrossRef]
- Röhner, E.; Benad, K.; Zippelius, T.; Kloss, N.; Jacob, B.; Kirschberg, J.; Matziolis, G. Good clinical and radiological results of total knee arthroplasty using varus valgus constrained or rotating hinge implants in ligamentous laxity. Knee Surg. Sports Traumatol. Arthrosc. 2018, 27, 1665–1670. [Google Scholar] [CrossRef]
- Cottino, U.; Abdel, M.P.; Perry, K.I.; Mara, K.C.; Lewallen, D.G.; Hanssen, A.D. Long-Term Results After Total Knee Arthroplasty with Contemporary Rotating-Hinge Prostheses. J. Bone Jt. Surg. Am. 2017, 99, 324–330. [Google Scholar] [CrossRef]
- Farid, Y.R.; Thakral, R.; Finn, H.A. Intermediate-Term Results of 142 Single-Design, Rotating-Hinge Implants: Frequent Complications May Not Preclude Salvage of Severely Affected Knees. J. Arthroplast. 2015, 30, 2173–2180. [Google Scholar] [CrossRef]
- Pour, A.E.; Parvizi, J.; Slenker, N.; Purtill, J.J.; Sharkey, P.F. Rotating Hinged Total Knee Replacement. J. Bone Jt. Surg. Am. 2007, 89, 1735–1741. [Google Scholar] [CrossRef]
- Shen, C.; Lichstein, P.M.; Austin, M.S.; Sharkey, P.F.; Parvizi, J. Revision Knee Arthroplasty for Bone Loss: Choosing the Right Degree of Constraint. J. Arthroplast. 2014, 29, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Kahlenberg, C.A.; Baral, E.C.; Lieberman, L.W.; Huang, R.C.; Wright, T.M.; Padgett, D.E. Retrieval Analysis of Polyethylene Components in Rotating Hinge Knee Arthroplasty Implants. J. Arthroplast. 2021, 36, 2998–3003. [Google Scholar] [CrossRef] [PubMed]
- Hannon, C.P.; Stuart, M.B.; Abdel, M.P.; Pagnano, M.W.; Trousdale, R.T. Revision Total Knee Arthroplasty With a Rotating-Hinge Prosthesis Mated to a Well-Fixed Femoral Sleeve. J. Arthroplast. 2022, 37, S270–S275. [Google Scholar] [CrossRef]
- Panesar, K.; Al-Mouazzen, L.; Nessa, L.; Jonas, S.C.; Agarwal, S.; Morgan-Jones, R. Revision Total Knee Arthroplasty Using an Uncemented Metaphyseal Sleeve, Rotating Hinge Prosthesis: A Case Series of 99 Patients. J. Arthroplast. 2021, 36, 2121–2125. [Google Scholar] [CrossRef]
- Hossain, F.; Patel, S.; Haddad, F.S. Midterm Assessment of Causes and Results of Revision Total Knee Arthroplasty. Clin. Orthop. Relat. Res. 2010, 468, 1221–1228. [Google Scholar] [CrossRef]
- Ewald, F.C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin. Orthop. Relat. Res. 1989, 248, 9–12. [Google Scholar] [CrossRef]
- Tan, T.L.; Goswami, K.; Fillingham, Y.A.; Shohat, N.; Rondon, A.J.; Parvizi, J. Defining Treatment Success After 2-Stage Exchange Arthroplasty for Periprosthetic Joint Infection. J. Arthroplast. 2018, 33, 3541–3546. [Google Scholar] [CrossRef]
- Diaz-Ledezma, C.; Higuera, C.A.; Parvizi, J. Success After Treatment of Periprosthetic Joint Infection: A Delphi-based International Multidisciplinary Consensus. Clin. Orthop. Relat. Res. 2013, 471, 2374–2382. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Liu, E.X.; Kuhataparuks, P.; Liow, M.-H.L.; Pang, H.-N.; Tay, D.K.J.; Chia, S.-L.; Lo, N.-N.; Yeo, S.-J.; Chen, J.Y. Clinical Frailty Scale is a better predictor for adverse post-operative complications and functional outcomes than Modified Frailty Index and Charlson Comorbidity Index after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3186–3195. [Google Scholar] [CrossRef] [PubMed]
- Naal, F.; Impellizzeri, F.; Sieverding, M.; Loibl, M.; von Knoch, F.; Mannion, A.; Leunig, M.; Munzinger, U. The 12-item Oxford Knee Score: Cross-cultural adaptation into German and assessment of its psychometric properties in patients with osteoarthritis of the knee. Osteoarthr. Cartil. 2009, 17, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; MacDonald, D.; Simpson, A.H.R.W. The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1933–1939. [Google Scholar] [CrossRef] [PubMed]
- Abdelaziz, H.; Jaramillo, R.; Gehrke, T.; Ohlmeier, M.; Citak, M. Clinical Survivorship of Aseptic Revision Total Knee Arthroplasty Using Hinged Knees and Tantalum Cones at Minimum 10-Year Follow-Up. J. Arthroplast. 2019, 34, 3018–3022. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Osman, K.; Green, G.; Haddad, F.S. The epidemiology of failure in total knee arthroplasty: Avoiding your next revision. Bone Jt. J. 2016, 98-B, 105–112. [Google Scholar] [CrossRef]
- Wignadasan, W.; Chang, J.S.; Kayani, B.; Kontoghiorghe, C.; Haddad, F.S. Long-term results of revision total knee arthroplasty using a rotating hinge implant. Knee 2021, 28, 72–80. [Google Scholar] [CrossRef]
- Kowalczewski, J.; Marczak, D.; Synder, M.; Sibiński, M. Primary Rotating-Hinge Total Knee Arthroplasty: Good Outcomes at Mid-Term Follow-Up. J. Arthroplast. 2014, 29, 1202–1206. [Google Scholar] [CrossRef]
- Bozic, K.J.; Kurtz, S.M.; Lau, E.; Ong, K.; Chiu, V.; Vail, T.P.; Rubash, H.E.; Berry, D.J. The Epidemiology of Revision Total Knee Arthroplasty in the United States. Clin. Orthop. Relat. Res. 2010, 468, 45–51. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.C.; Son, M.-S.; Chang, E.T.; Zimmerli, W.; Parvizi, J. Are We Winning or Losing the Battle With Periprosthetic Joint Infection: Trends in Periprosthetic Joint Infection and Mortality Risk for the Medicare Population. J. Arthroplast. 2018, 33, 3238–3245. [Google Scholar] [CrossRef]
- Boelch, S.P.; Arnholdt, J.; Holzapfel, B.M.; Jakuscheit, A.; Rudert, M.; Hoberg, M. Revision knee arthroplasty with rotating hinge systems in patients with gross ligament instability. Int. Orthop. 2018, 42, 2825–2833. [Google Scholar] [CrossRef]
- Kearns, S.M.; Culp, B.M.; Bohl, D.D.; Sporer, S.M.; Della Valle, C.J.; Levine, B.R. Rotating Hinge Implants for Complex Primary and Revision Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 766–770. [Google Scholar] [CrossRef] [PubMed]
- Theil, C.; Stock, M.E.; Gosheger, G.; Moellenbeck, B.; Schwarze, J.; Schmidt-Braekling, T. Gastrocnemius Muscle Flaps for Soft Tissue Coverage in Periprosthetic Knee Joint Infection. J. Arthroplast. 2020, 35, 3730–3736. [Google Scholar] [CrossRef]
- Driesman, A.S.; Macaulay, W.; Schwarzkopf, R. Cemented versus Cementless Stems in Revision Total Knee Arthroplasty. J. Knee Surg. 2019, 32, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Fleischman, A.N.; Azboy, I.; Fuery, M.; Restrepo, C.; Shao, H.; Parvizi, J. Effect of Stem Size and Fixation Method on Mechanical Failure After Revision Total Knee Arthroplasty. J. Arthroplast. 2017, 32, S202–S208.e1. [Google Scholar] [CrossRef]
- Kang, S.G.; Park, C.H.; Song, S.J. Stem Fixation in Revision Total Knee Arthroplasty: Indications, Stem Dimensions, and Fixation Methods. Knee Surg. Relat. Res. 2018, 30, 187–192. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ettinger, M.; Savov, P.; Windhagen, H.; Bühren, V.; Hungerer, S. End-of-stem pain in hip and knee arthroplasty. Orthopade 2021, 50, 51–59. [Google Scholar] [CrossRef]
- Petursson, G.; Fenstad, A.M.; Havelin, L.I.; Gøthesen, Ø.; Lygre, S.H.L.; Röhrl, S.M.; Furnes, O. Better survival of hybrid total knee arthroplasty compared to cemented arthroplasty. Acta Orthop. 2015, 86, 714–720. [Google Scholar] [CrossRef]
- Wang, C.; Pfitzner, T.; von Roth, P.; Mayr, H.O.; Sostheim, M.; Hube, R. Fixation of stem in revision of total knee arthroplasty: Cemented versus cementless—A meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3200–3211. [Google Scholar] [CrossRef]
- Ohlmeier, M.; Alrustom, F.; Citak, M.; Salber, J.; Gehrke, T.; Frings, J. What Is the Mid-term Survivorship of Infected Rotating-hinge Implants Treated with One-stage-exchange? Clin. Orthop. Relat. Res. 2021, 479, 2714–2722. [Google Scholar] [CrossRef]
- Theil, C.; Schmidt-Braekling, T.; Gosheger, G.; Thuener, B.; Moellenbeck, B.; Roeder, J.; Andreou, D.; Schwarze, J.; Dieckmann, R. Acceptable mid- to long-term survival rates and functional outcomes following a single design rotating hinge total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1868–1875. [Google Scholar] [CrossRef]
- Theil, C.; Schneider, K.N.; Gosheger, G.; Schmidt-Braekling, T.; Ackmann, T.; Dieckmann, R.; Frommer, A.; Klingebiel, S.; Schwarze, J.; Moellenbeck, B. Revision TKA with a distal femoral replacement is at high risk of reinfection after two-stage exchange for periprosthetic knee joint infection. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Tan, T.L.; Li, W.T.; Goswami, K.; Parvizi, J. Reporting Outcomes of Treatment for Periprosthetic Joint Infection of the Knee and Hip Together With a Minimum 1-Year Follow-Up is Reliable. J. Arthroplast. 2020, 35, 1906–1911.e5. [Google Scholar] [CrossRef] [PubMed]
- Wyles, C.C.; Tibbo, M.E.; Yuan, B.J.; Trousdale, R.T.; Berry, D.J.; Abdel, M.P. Long-Term Results of Total Knee Arthroplasty with Contemporary Distal Femoral Replacement. J. Bone Jt. Surg. Am. 2020, 102, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Steinicke, A.C.; Schwarze, J.; Gosheger, G.; Moellenbeck, B.; Ackmann, T.; Theil, C. Repeat two-stage exchange arthroplasty for recurrent periprosthetic hip or knee infection: What are the chances for success? Arch. Orthop. Trauma Surg. 2023, 143, 1731–1740. [Google Scholar] [CrossRef] [PubMed]
- Fehring, K.A.; Abdel, M.P.; Ollivier, M.; Mabry, T.M.; Hanssen, A.D. Repeat Two-Stage Exchange Arthroplasty for Periprosthetic Knee Infection Is Dependent on Host Grade. J. Bone Jt. Surg. Am. 2017, 99, 19–24. [Google Scholar] [CrossRef] [PubMed]

| Variable | Median (25–75% Interquartile Range) |
|---|---|
| age | 72 (62–79) |
| BMI | 30 (25–33) |
| CCI | 4 (2–5) |
| ASA | 2 (2–3) |
| previous revisions | 2 (2–4) |
| Variable | Five Year Survival Probability (95% CI) | p-Value (Log-Rank) |
|---|---|---|
| male vs. female | 81% (95% CI 68–93%) vs. 86% (95% CI 78–96%) | 0.09 |
| smokers vs. non-smokers | 95% (95% CI 86–100%) vs. 83% (95% CI 73–93%) | 0.27 |
| diabetics vs. non-diabetics | 91% (95% CI 81–100%) vs. 83% (95% CI 70–94%) | 0.53 |
| Variable | Median (25–75 IQR) | p-Value |
|---|---|---|
| age | 74 (IQR 67–78) vs. 72 (IQR 62–80) | 0.63 |
| BMI | 31 (IQR 26–34) vs. 29 (IQR 25–33) | 0.45 |
| CCI | 4 (IQR 3–5) vs. 4 (IQR 2–5) | 0.69 |
| ASA | 2 (IQR 2–3) vs. 2 (IQR 2–3) | 0.52 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schlechter, M.; Theil, C.; Gosheger, G.; Moellenbeck, B.; Schwarze, J.; Puetzler, J.; Bockholt, S. Good Mid-Term Implant Survival of a Novel Single-Design Rotating-Hinge Total Knee Arthroplasty. J. Clin. Med. 2023, 12, 6113. https://doi.org/10.3390/jcm12196113
Schlechter M, Theil C, Gosheger G, Moellenbeck B, Schwarze J, Puetzler J, Bockholt S. Good Mid-Term Implant Survival of a Novel Single-Design Rotating-Hinge Total Knee Arthroplasty. Journal of Clinical Medicine. 2023; 12(19):6113. https://doi.org/10.3390/jcm12196113
Chicago/Turabian StyleSchlechter, Matthias, Christoph Theil, Georg Gosheger, Burkhard Moellenbeck, Jan Schwarze, Jan Puetzler, and Sebastian Bockholt. 2023. "Good Mid-Term Implant Survival of a Novel Single-Design Rotating-Hinge Total Knee Arthroplasty" Journal of Clinical Medicine 12, no. 19: 6113. https://doi.org/10.3390/jcm12196113
APA StyleSchlechter, M., Theil, C., Gosheger, G., Moellenbeck, B., Schwarze, J., Puetzler, J., & Bockholt, S. (2023). Good Mid-Term Implant Survival of a Novel Single-Design Rotating-Hinge Total Knee Arthroplasty. Journal of Clinical Medicine, 12(19), 6113. https://doi.org/10.3390/jcm12196113





