Intraocular Pressure Variations in Postural Changes: Comparison between Obese and Non-Obese Controls
Abstract
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kang, J.M.; Tanna, A.P. Glaucoma. Med. Clin. N. Am. 2021, 105, 493–510. [Google Scholar] [CrossRef] [PubMed]
- Ahn, M.W.; Lee, J.W.; Shin, J.H.; Lee, J.S. Relationship between intraocular pressure and parameters of obesity in ocular hypertension. Int. J. Ophthalmol. 2020, 13, 794–800. [Google Scholar] [CrossRef]
- De Bernardo, M.; Capasso, L.; Caliendo, L.; Vosa, Y.; Rosa, N. Intraocular Pressure Evaluation after Myopic Refractive Surgery: A Comparison of Methods in 121 Eyes. Semin. Ophthalmol. 2016, 31, 233–242. [Google Scholar] [CrossRef] [PubMed]
- De Bernardo, M.; Cembalo, G.; Rosa, N. Reliability of Intraocular Pressure Measurement by Goldmann Applanation Tonometry After Refractive Surgery: A Review of Different Correction Formulas. Clin. Ophthalmol. 2020, 14, 2783–2788. [Google Scholar] [CrossRef] [PubMed]
- Heijl, A.; Leske, M.C.; Bengtsson, B.; Hyman, L.; Bengtsson, B.; Hussein, M.; Early Manifest Glaucoma Trial Group. Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: Results from the Early Manifest Glaucoma Trial. Arch. Ophthalmol. 2002, 120, 1268–1279. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.P.Y.; Broadway, D.C.; Khawaja, A.P.; Yip, J.L.Y.; Garway-Heath, D.F.; Burr, J.M.; Luben, R.; Hayat, S.; Dalzell, N.; Khaw, K.-T.; et al. Glaucoma and intraocular pressure in EPIC-Norfolk eye study: Cross sectional study. BMJ 2017, 358. [Google Scholar] [CrossRef] [PubMed]
- Boland, M.V.; Ervin, A.-M.; Friedman, D.S.; Jampel, H.D.; Hawkins, B.S.; Vollenweider, D.; Chelladurai, Y.; Ward, D.; Suarez-Cuervo, C.; Robinson, K.A. Comparative effectiveness of treatments for open-angle glaucoma: A systematic review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2013, 158, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Song, B.J.; Aiello, L.P.; Pasquale, L.R. Presence and Risk Factors for Glaucoma in Patients with Diabetes. Curr. Diab Rep. 2016, 16, 124. [Google Scholar] [CrossRef]
- Roddy, G.W. Metabolic Syndrome Is Associated with Ocular Hypertension and Glaucoma. J. Glaucoma 2020, 29, 726–731. [Google Scholar] [CrossRef]
- Shi, Y.; Liu, P.; Guan, J.; Lu, Y.; Su, K. Association between glaucoma and obstructive sleep apnea syndrome: A meta-analysis and systematic review. PLoS ONE 2015, 10, e0115625. [Google Scholar] [CrossRef] [PubMed]
- Cheung, N.; Wong, T.Y. Obesity and eye diseases. Surv. Ophthalmol. 2007, 52, 180–195. [Google Scholar] [CrossRef] [PubMed]
- World Health Organizarion. Health Topics, Obesity. Available online: https://www.who.int/health-topics/obesity#tab=tab_1 (accessed on 1st August 2023).
- Van Leiden, H.A.; Dekker, J.M.; Moll, A.C.; Nijpels, G.; Heine, R.J.; Bouter, L.M.; Stehouwer, C.D.A.; Polak, B.C.P. Blood pres-sure, lipids, and obesity are associated with retinopathy: The hoorn study. Diabetes Care 2002, 25, 1320–1325. [Google Scholar] [CrossRef] [PubMed]
- Glynn, R.J.; Christen, W.G.; Manson, J.E.; Bernheimer, J.; Hennekens, C.H. Body mass index an independent predictor of cataract. Arch. Ophthalmol. 1995, 113, 1131–1137. [Google Scholar] [CrossRef] [PubMed]
- Seddon, J.M.; Cote, J.; Davis, N.; Rosner, B. Progression of age-related macular degeneration: Association with body mass index, waist circumference and waist-hip ratio. Arch. Ophthalmol. 2003, 121, 785–792. [Google Scholar] [CrossRef]
- Leske, M.C.; Connell, A.M.S.; Wu, S.Y.; Hyman, L.G.; Schachat, A.P. Risk factors for open-angle glaucoma. The Barbados Eye Study. Arch. Ophthalmol. 1995, 113, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Maimonides Emergency Medicine. How to Use the Reichert Tobo-Pen Avia. Available online: https://www.maimonidesem.org/blog/how-to-use-the-reichert-tono-pen-avia#:~:text=Try%20calibrating%20it%20before%20using,hear%205%20beeps%20in%20succession (accessed on 1st August 2023).
- Cione, F.; De Bernardo, M.; Gioia, M.; Oliviero, M.; Santoro, A.G.; Caputo, A.; Capasso, L.; Pagliarulo, S.; Rosa, N. A No-History Multi-Formula Approach to Improve the IOL Power Calculation after Laser Refractive Surgery: Preliminary Results. J. Clin. Med. 2023, 12, 2890. [Google Scholar] [CrossRef] [PubMed]
- De Bernardo, M.; Borrelli, M.; Cembalo, G.; Rosa, N. Intraocular Pressure Measurements in Standing Position with a Rebound Tonometer. Medicina 2019, 55, 701. [Google Scholar] [CrossRef]
- De Bernardo, M.; Salerno, G.; Gioia, M.; Capasso, L.; Russillo, M.C.; Picillo, M.; Erro, R.; Amboni, M.; Barone, P.; Rosa, N.; et al. Intraocular pressure and choroidal thickness postural changes in multiple system atrophy and Parkinson’s disease. Sci. Rep. 2021, 11, 8936. [Google Scholar] [CrossRef]
- Geloneck, M.M.; Crowell, E.L.; Wilson, E.B.; Synder, B.E.; Chuang, A.Z.; Baker, L.A.; Bell, N.P.; Feldman, R.M. Correlation between intraocular pressure and body mass index in the seated and supine positions. J. Glaucoma 2015, 24, 130–134. [Google Scholar] [CrossRef]
- Malihi, M.; Sit, A.J. Effect of head and body position on intraocular pressure. Ophthalmology 2012, 119, 987–991. [Google Scholar] [CrossRef]
- Friberg, T.R.; Sanborn, G.; Weinreb, R.N. Intraocular and episcleral venous pressure increase during inverted posture. Am. J. Ophthalmol. 1987, 103, 523–526. [Google Scholar] [CrossRef]
- Kiel, J.W. Choroidal myogenic autoregulation and intraocular pressure. Exp. Eye Res. 1994, 58, 529–543. [Google Scholar] [CrossRef]
- Bloomfield, G.L.; Ridings, P.C.; Blocher, C.R.B.; Marmarou, A.; Sugerman, H.J. A proposed relationship between increased intra-abdominal, intrathoracic, and intracranial pressure. Crit. Care Med. 1997, 25, 496–503. [Google Scholar] [CrossRef]
- Lam, C.T.; Trope, G.E.; Buys, Y.M. Effect of Head Position and Weight Loss on Intraocular Pressure in Obese Subjects. J. Glaucoma 2017, 26, 107–112. [Google Scholar] [CrossRef]
- Williams, B.I.; Peart, W.S.; Letley, E. Abnormal intraocular pressure control in systemic hypertension and diabetic mellitus. Br. J. Ophthalmol. 1980, 64, 845–851. [Google Scholar] [CrossRef]
- Yamabayashi, S.; Aguilar, R.N.; Hosoda, M.; Tsukahara, S. Postural change of intraocular and blood pressures in ocular hyper-tension and low-tension glaucoma. Br. J. Ophthalmol. 1991, 75, 652–655. [Google Scholar] [CrossRef]
- Leonard, T.J.; Muir, M.G.K.; Kirkby, G.R.; Hitchings, R.A. Ocular hypertension and posture. Br. J. Ophthalmol. 1983, 67, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Jung, S.W.; Nam, G.E.; Do Han, K.; Bok, A.R.; Baek, S.J.; Cho, K.-H.; Choi, Y.H.; Kim, S.-M.; Ju, S.-Y.; et al. High intraocular pressure is associated with cardiometabolic risk factors in South Korean men: Korean National Health and Nutrition Examination Survey, 2008–2010. Eye 2014, 28, 672–679. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oh, S.W.; Lee, S.; Park, C.; Kim, D.J. Elevated intraocular pressure is associated with insulin resistance and metabolic syndrome. Diabets Metab. Res. Rev. 2005, 21, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Imai, K.; Hamaguchi, M.; Mori, K.; Takeda, N.; Fukui, M.; Kato, T.; Kawahito, Y.; Kinoshita, S.; Kojima, T. Metabolic Syndrome as a risk factor for high-ocular tension. Int. J. Obes. 2010, 34, 1209–1217. [Google Scholar] [CrossRef] [PubMed]
- Bouloumié, A.; Marumo, T.; Lafontan, M.; Busse, R. Leptin induces oxidative stress in human endothelial cells. FASEB J. 1999, 13, 1231–1238. [Google Scholar] [CrossRef]
- Karadag, R.; Arslanyilmaz, Z.; Aydin, B.; Hepsen, I.F. Effects of body mass index on intraocular Pressure and ocular pulse amplitude. Int. J. Ophthalmol. 2012, 5, 605–608. [Google Scholar]
- Aslam, D.W.; James, W.P. Obesity. Lancet 2005, 366, 1197–1209. [Google Scholar] [CrossRef] [PubMed]
- Panon, N.; Luangsawang, K.; Rugaber, C.; Tongchit, T.; Thongsepee, N.; Cheaha, D.; Kongjaidee, P.; Changtong, A.; Daradas, A.; Chotimol, P. Correlation between body mass index and ocular parameters. Clin. Ophthalmol. 2019, 13, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Çekiç, B.; Toslak, İ.E.; Doğan, B.; Çakır, T.; Erol, M.K.; Bülbüller, N. Effects of obesity on retrobulbar flow hemodynamics: Color Doppler ultrasound evaluation. Arq. Bras. Oftalmol. 2017, 80, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Stojanov, O.; Stokic, E.; Sveljo, O.; Naumovic, N. The influence of retrobulbar adipose tissue volume upon intraocular pressure in obesity. Vojnosanit. Pregl. 2013, 70, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Kaskan, B.; Ramezani, K.; Harris, A.; Siesky, B.; Olinde, C.; WuDunn, D.; Eikenberry, J.; Tobe, L.A.; Racette, L. Differences in ocular blood flow between people of African and European descent with healthy eyes. J. Glaucoma 2016, 25, 709–715. [Google Scholar] [CrossRef]
- Buys, Y.M.; Alasbali, T.; Jin, Y.P. Effect of sleeping in a head-up position on intraocular pressure in patients with glaucoma. Ophthalmology 2010, 117, 1348–5123. [Google Scholar] [CrossRef] [PubMed]
- Berk, T.A.; Yang, P.T.; Chan, C.C. Prospective comparative analysis of 4 different intraocular pressure measurement techniques and their effects on pressure readings. J. Glaucoma 2016, 25, e897–e904. [Google Scholar] [CrossRef]
- Wong, B.; Parikh, D.; Rosen, L.; Gorski, M.; Angelilli, A.; Shih, C. Comparison of Disposable Goldmann Applanation Tonometer, ICare ic100, and Tonopen XL to Standards of Care Goldmann Nondisposable Applanation Tonometer for Measuring Intraocular Pressure. J. Glaucoma 2018, 27, 1119–1124. [Google Scholar] [CrossRef] [PubMed]
- Young, M.T.; Phelan, M.J.; Nguyen, N.T. A Decade Analysis of Trends and Outcomes of Male vs Female Patients Who Underwent Bariatric Surgery. J. Am. Coll. Surg. 2016, 222, 226–231. [Google Scholar] [CrossRef] [PubMed]
- De Bernardo, M.; Abbinante, G.; Borrelli, M.; Di Stasi, M.; Cione, F.; Rosa, N. Intraocular Pressure Measurements in Standing, Sitting, and Supine Position: Comparison between Tono-Pen Avia and Icare Pro Tonometers. J. Clin. Med. 2022, 11, 6234. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Standing 5′ | Sitting | Supine | Supine 5′ | Immediately Standing |
|---|---|---|---|---|---|
| IOP in different Positions—Obese Subjects | |||||
| Mean ± SD | 15.01 ± 2.29 mmHg | 15.52 ± 2.84 mmHg | 17.13 ± 3.27 mmHg | 17.25 ± 2.95 mmHg | 15.29 ± 2.38 mmHg |
| CI 95% | 15.01–15.95 mmHg | 14.93–16.11 mmHg | 16.45–17.81 mmHg | 16.64–17.86 mmHg | 14.80–15.79 mmHg |
| Median | 15.00 mmHg | 15.00 mmHg | 16.00 mmHg | 16.50 mmHg | 15.00 mmHg |
| Min/Max | 11.00/21.00 mmHg | 10.00/27.00 mmHg | 11.00/26.00 mmHg | 13.00/28.00 mmHg | 10.00/24.00 mmHg |
| IQR | 3.00 mmHg | 3.00 mmHg | 4.00 mmHg | 4.00 mmHg | 2.00 mmHg |
| KS | 0.094 | 0.002 | 0.010 | 0.001 | 0.039 |
| IOP in different Positions—Non obese Controls | |||||
| Mean ± SD | 14.88 ± 2.83 mmHg | 14.31 ± 2.27 mmHg | 15.60 ± 2.90 mmHg | 15.81 ± 2.70 mmHg | 14.23 ± 2.17 mmHg |
| CI | 14.05/15.70 mmHg | 13.65/14.97 mmHg | 14.76/16.45 mmHg | 15.03/16.60 mmHg | 13.60/14.86 mmHg |
| Median | 15.00 mmHg | 14.00 mmHg | 16.00 mmHg | 16.00 mmHg | 14.00 mmHg |
| Min/Max | 10.00–21.00 mmHg | 9.00–18.00 mmHg | 10.00–21.00 mmHg | 10.00–20.00 mmHg | 9.00–19.00 mmHg |
| IQR | 5.00 mmHg | 3.00 mmHg | 5.00 mmHg | 4.00 mmHg | 3.00 mmHg |
| KS | 0.736 | 0.059 | 0.370 | 0.215 | 0.716 |
| IOP in Different Positions—Obese Subjects | ||||||||
| Parameter | Standing 5′ | Sitting | Supine | Supine 5′ | Immediately Standing | |||
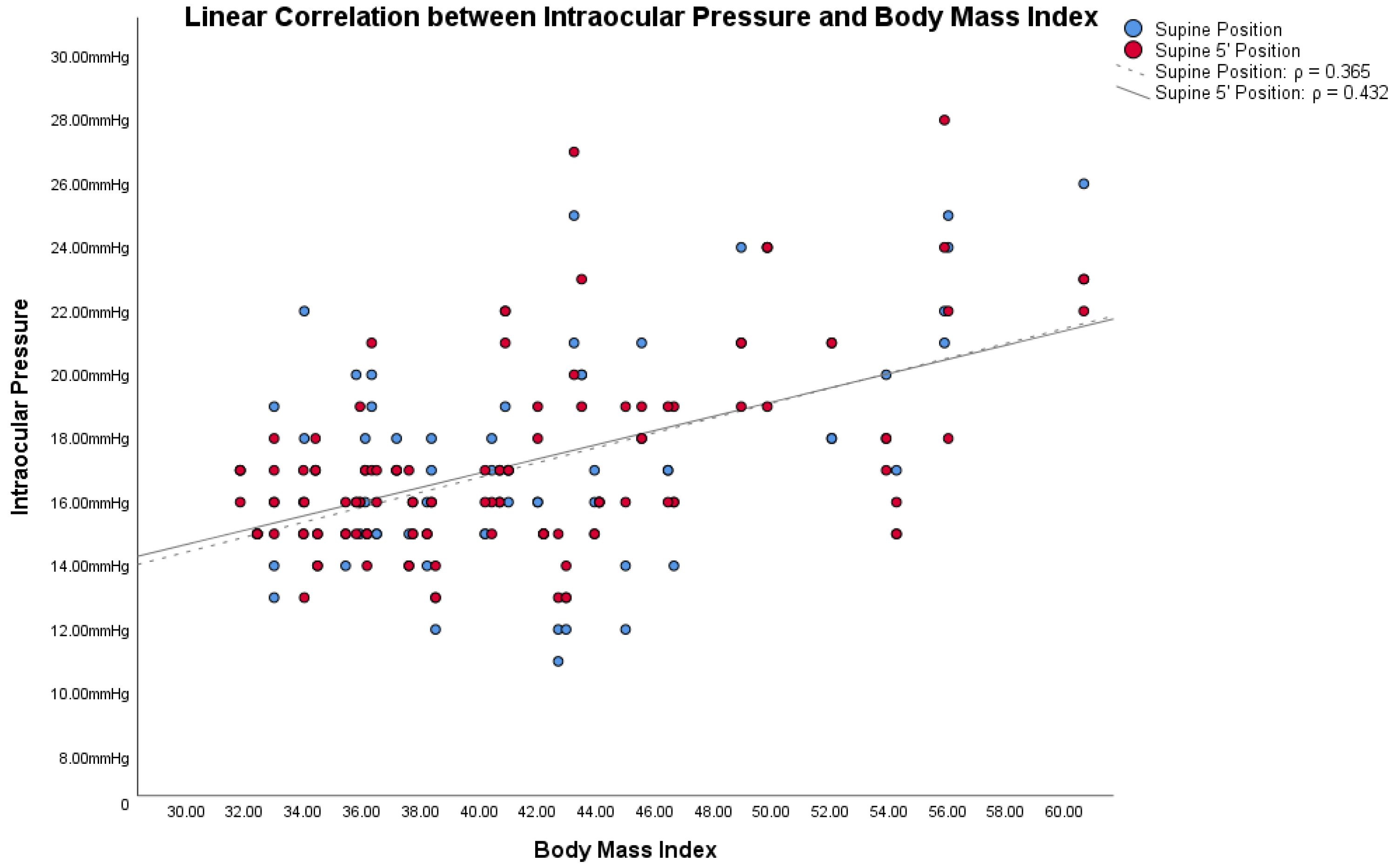
| BMI | 0.207 | 0.231 | 0.365 | 0.432 | 0.316 | |||
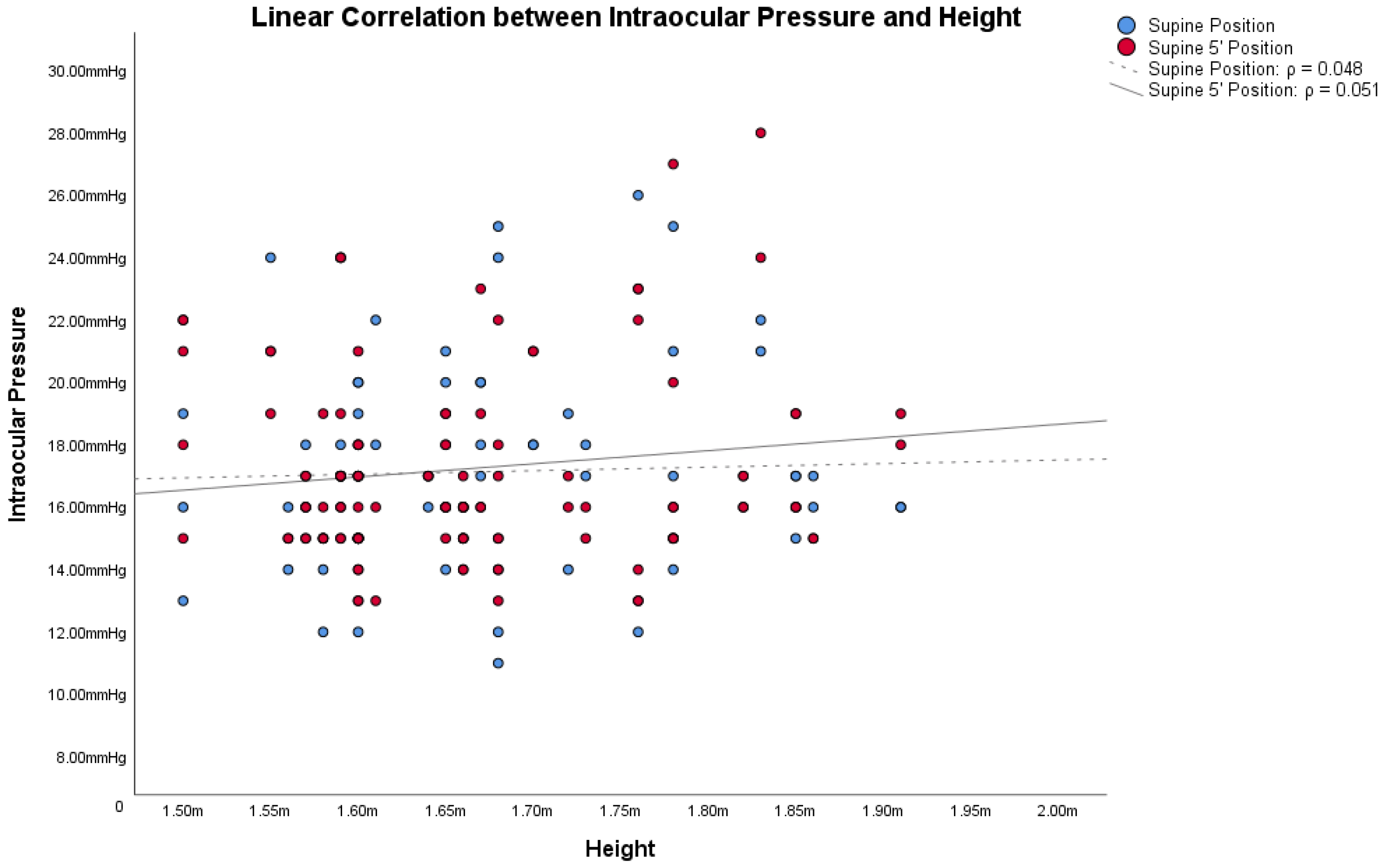
| Height | 0.086 | 0.044 | 0.051 | 0.048 | 0.040 | |||
| Weight | 0.196 | 0.083 | 0.291 | 0.355 | 0.264 | |||
| ΔIOP in Different Positions—Obese Subjects | ||||||||
| Parameter | ΔIOP Supine/ Standing | ΔIOP Supine/ Standing 5′ | ΔIOP Supine/ Sitting | ΔIOP Supine/ Immediately Standing | ΔIOP Supine 5′/ Standing | ΔIOP Supine 5′/ Standing 5′ | ΔIOP Supine 5′/ Sitting | ΔIOP Supine 5′/ Immediately Standing |
| BMI | 0.330 | 0.314 | 0.325 | 0.131 | 0.282 | 0.311 | 0.291 | 0.227 |
| Height | 0.076 | −0.040 | −0.053 | −0.046 | 0.109 | −0.012 | 0.018 | 0.023 |
| Weight | 0.282 | 0.202 | 0.195 | 0.60 | 0.252 | 0.208 | 0.204 | 0.163 |
| Parameter | ΔIOP Supine/ Standing 5′ | ΔIOP Supine/ Sitting | ΔIOP Supine/ Immediately Standing | ΔIOP Supine 5′/ Standing 5′ | ΔIOP Supine 5′/ Sitting | ΔIOP Supine 5′/ Immediately Standing |
|---|---|---|---|---|---|---|
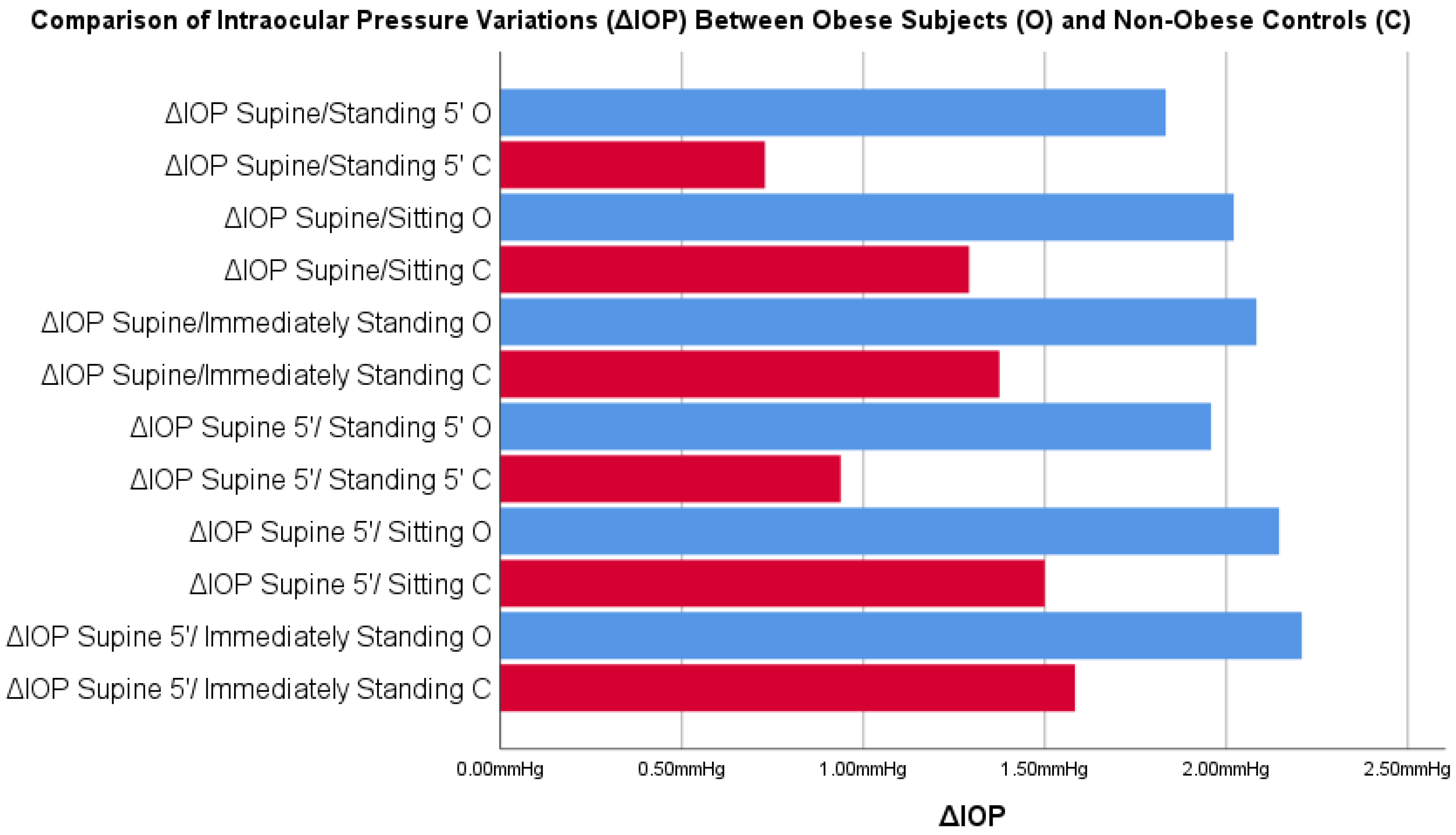
| ΔIOP in different Positions—Obese Subjects | ||||||
| Mean ± SD | 1.83 ± 2.47 mmHg | 2.02 ± 2.88 mmHg | 2.08 ± 2.55 mmHg | 1.96 ± 2.44 mmHg | 2.15 ± 2.74 mmHg | 2.21 ± 2.17 mmHg |
| CI 95% | 1.12–2.55 mmHg | 1.18–2.86 mmHg | 1.34–2.82 mmHg | 1.25–2.67 mmHg | 1.35–2.94 mmHg | 1.58–2.84 mmHg |
| Median | 1.50 mmHg | 1.50 mmHg | 1.50 mmHg | 2.00 mmHg | 2.00 mmHg | 2.00 mmHg |
| Min/Max | −3.00/9.00 mmHg | −7.00/11.00 mmHg | −2.00/10.00 mmHg | −3.00/8.00 mmHg | −7.00/8.00 mmHg | −1.00/7.00 mmHg |
| IQR | 3.00 mmHg | 2.00 mmHg | 3.00 mmHg | 3.00 mmHg | 3.00 mmHg | 4.00 mmHg |
| KS | 0.062 | 0.049 | 0.068 | 0.008 | 0.041 | 0.101 |
| ΔIOP in different Positions—Non-obese Controls | ||||||
| Mean ± SD | 0.73 ± 1.83 mmHg | 1.29 ± 1.54 mmHg | 1.38 ± 1.90 mmHg | 0.94 ± 1.90 mmHg | 1.50 ± 1.64 mmHg | 1.58 ± 1.76 mmHg |
| CI | 0.20–1.26 mmHg | 0.84–1.74 mmHg | 0.82–1.93 mmHg | 0.39–1.49 mmHg | 1.02–1.98 mmHg | 1.07–2.09 mmHg |
| Median | 1.00 mmHg | 1.00 mmHg | 1.00 mmHg | 1.00 mmHg | 1.00 mmHg | 1.00 mmHg |
| Min/Max | −3.00/5.00 mmHg | −3.00/5.00 mmHg | −3.00/5.00 mmHg | −3.00/6.00 mmHg | −2.00/4.00 mmHg | −3.00/6.00 mmHg |
| IQR | 3.00 mmHg | 2.00 mmHg | 2.00 mmHg | 2.00 mmHg | 3.00 mmHg | 3.00 mmHg |
| KS | 0.140 | 0.093 | 0.105 | 0.291 | 0.146 | 0.204 |
| ΔIOP Patients – ΔIOP controls | 1.10 mmHg | 0.73 mmHg | 0.70 mmHg | 1.02 mmHg | 0.65 mmHg | 0.63 mmHg |
| P | 0.015 | 0.272 | 0.280 | 0.027 | 0.336 | 0.213 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Bernardo, M.; Pilone, V.; Di Paola, I.; Cione, F.; Cembalo, G.; Calabrese, P.; Rosa, N. Intraocular Pressure Variations in Postural Changes: Comparison between Obese and Non-Obese Controls. J. Clin. Med. 2023, 12, 5883. https://doi.org/10.3390/jcm12185883
De Bernardo M, Pilone V, Di Paola I, Cione F, Cembalo G, Calabrese P, Rosa N. Intraocular Pressure Variations in Postural Changes: Comparison between Obese and Non-Obese Controls. Journal of Clinical Medicine. 2023; 12(18):5883. https://doi.org/10.3390/jcm12185883
Chicago/Turabian StyleDe Bernardo, Maddalena, Vincenzo Pilone, Ilenia Di Paola, Ferdinando Cione, Giovanni Cembalo, Pietro Calabrese, and Nicola Rosa. 2023. "Intraocular Pressure Variations in Postural Changes: Comparison between Obese and Non-Obese Controls" Journal of Clinical Medicine 12, no. 18: 5883. https://doi.org/10.3390/jcm12185883
APA StyleDe Bernardo, M., Pilone, V., Di Paola, I., Cione, F., Cembalo, G., Calabrese, P., & Rosa, N. (2023). Intraocular Pressure Variations in Postural Changes: Comparison between Obese and Non-Obese Controls. Journal of Clinical Medicine, 12(18), 5883. https://doi.org/10.3390/jcm12185883








