Mid- to Long-Term Outcomes of Arthroscopic Shoulder Stabilization in Athletes: A Systematic Review
Abstract
:1. Introduction
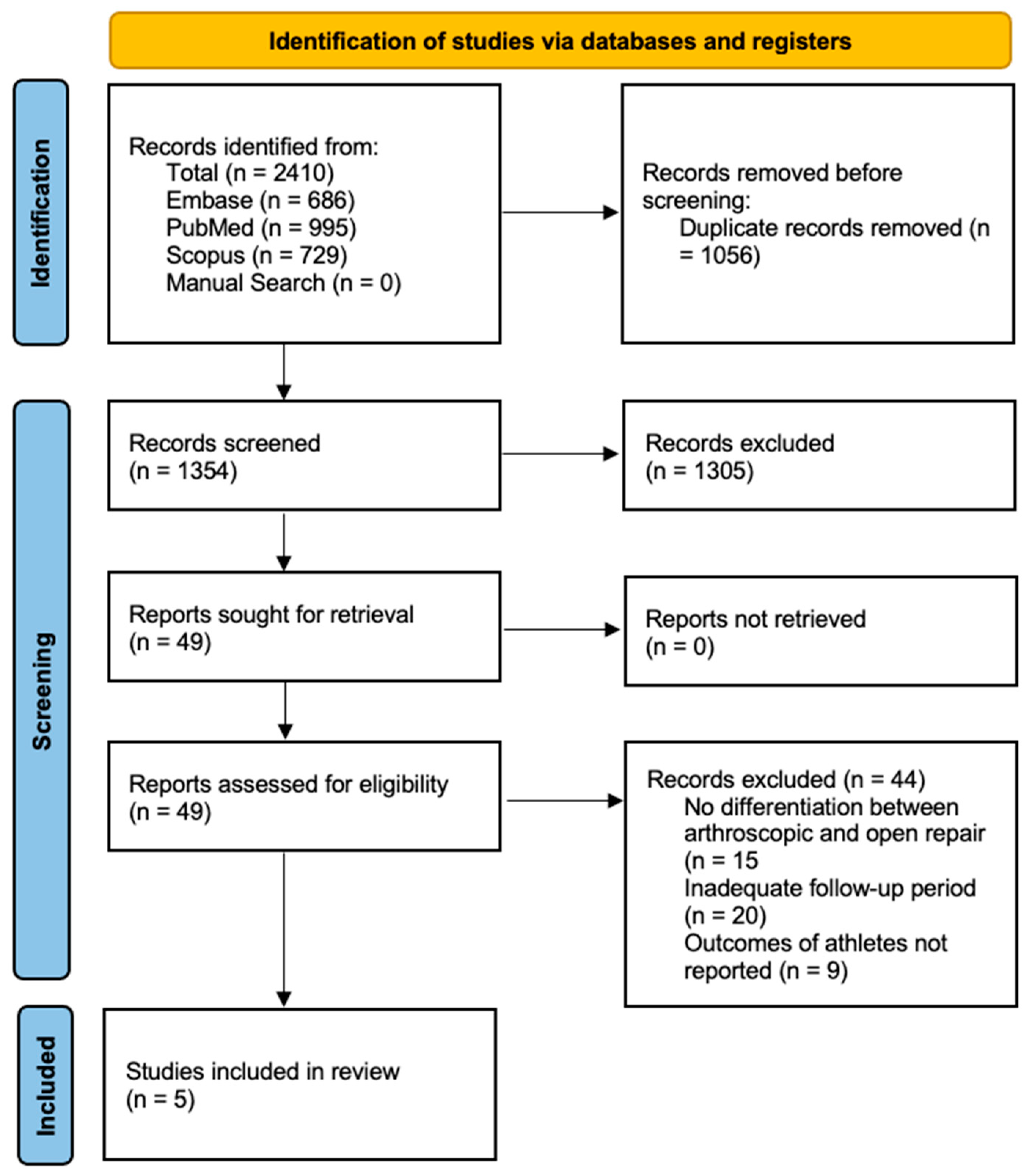
2. Materials and Methods
3. Results
3.1. Results of the Literature Search
3.2. Methodological Quality and Risk of Bias
3.3. Demographics and Level of Sports Involvement
3.4. Intraoperative and Radiographic Findings, and Surgical Outcomes
3.5. Factors Associated with Surgical Outcome or Satisfaction
3.6. Factors Associated with Radiographic Outcomes at Follow-Up
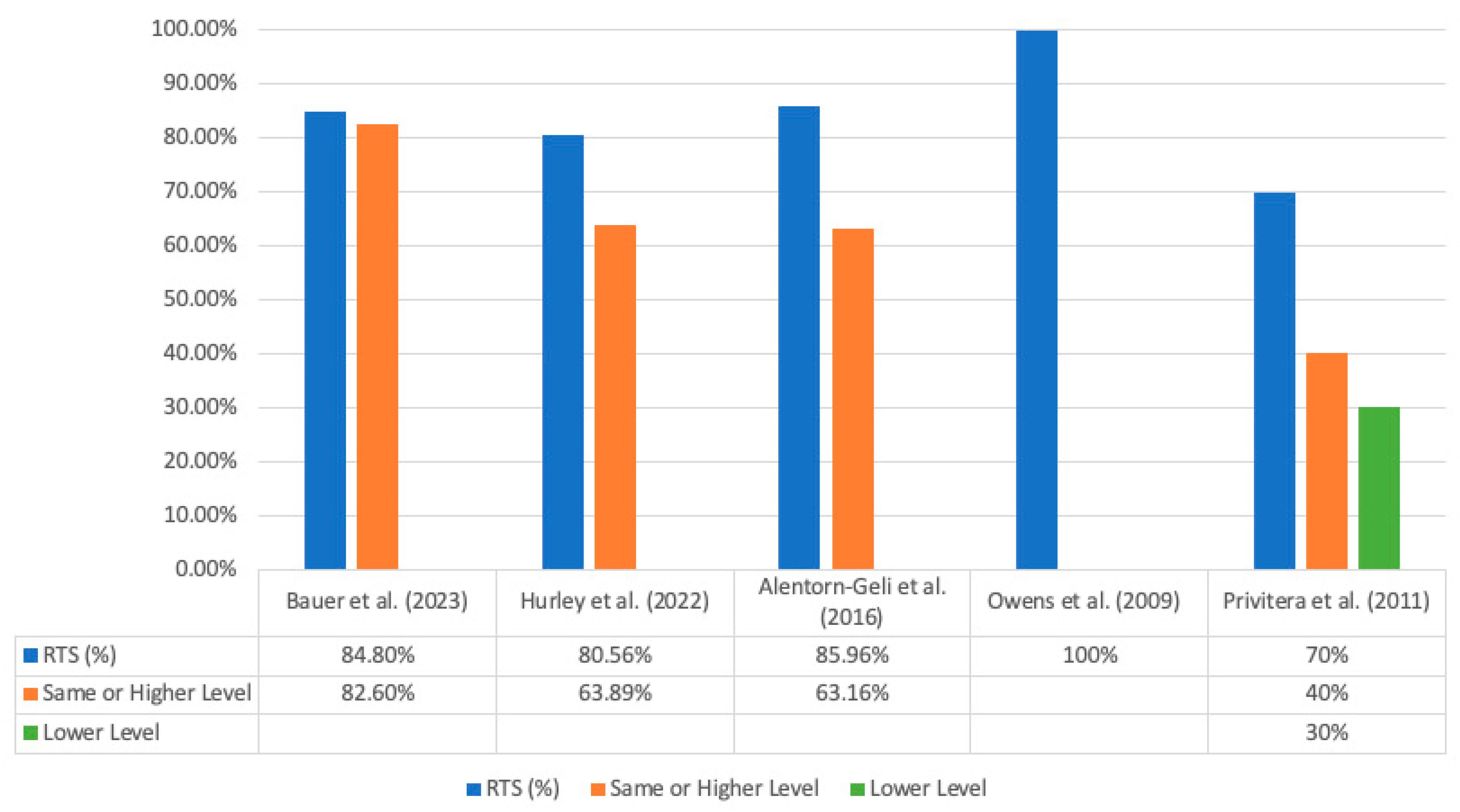
3.7. Rates of Return to Sport and Recurrent Instability
3.8. Return to Sport and Activity Level at Follow-Up
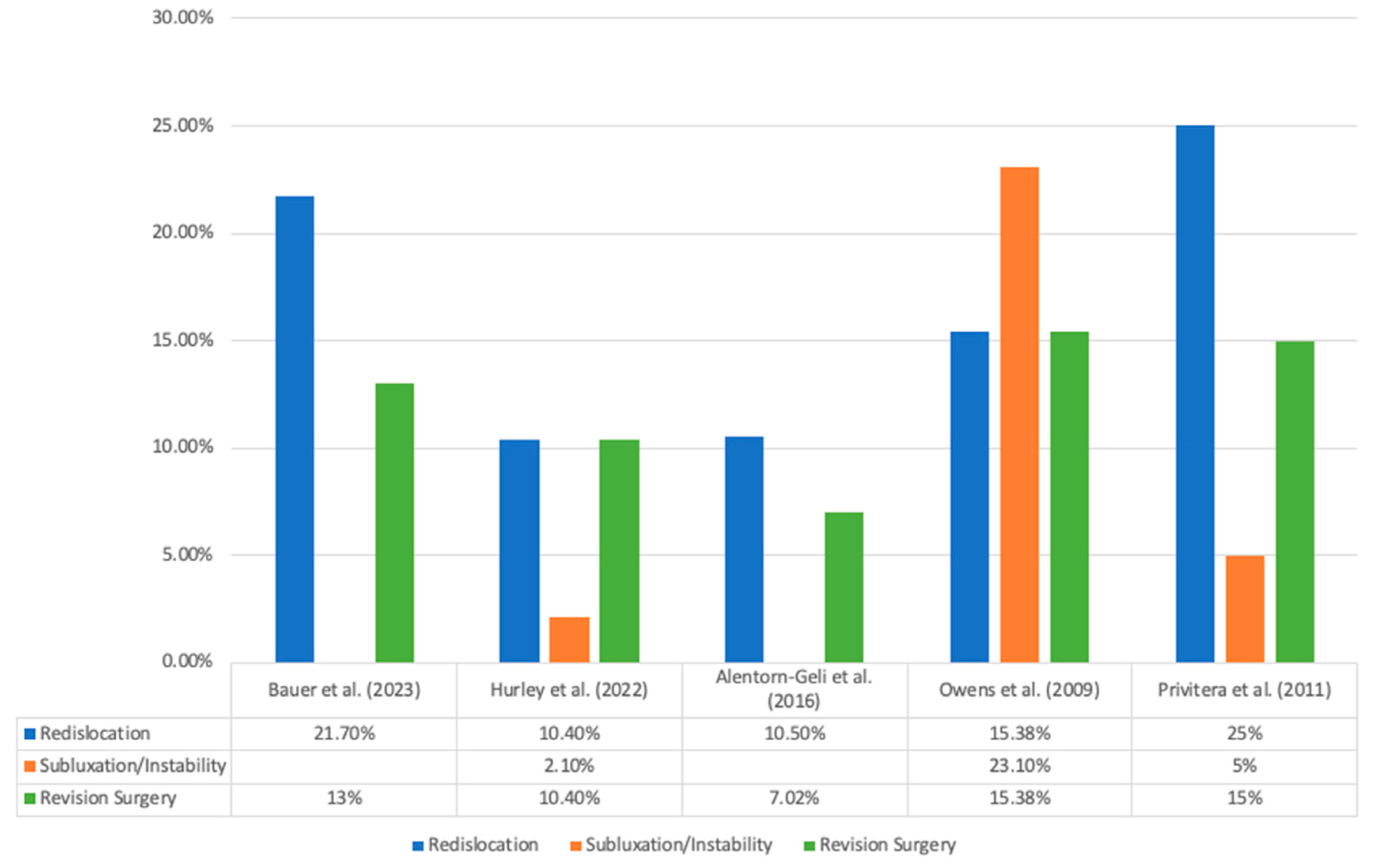
3.9. Redislocations and Revision Surgeries
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vargas, L.; Charen, D.; Huang, H.-H.; Poeran, J.; Colvin, A. Analysis of common shoulder injuries in collegiate baseball players. Physician Sportsmed. 2022, 50, 394–399. [Google Scholar] [CrossRef]
- Gibbs, D.B.; Lynch, T.S.; Nuber, E.D.; Nuber, G.W. Common Shoulder Injuries in American Football Athletes. Curr. Sports Med. Rep. 2015, 14, 413–419. [Google Scholar] [CrossRef]
- Yancey, J.R.; Szczepanik, M. Acromioclavicular Joint Dislocation: Surgical vs. Conservative Interventions. Am. Fam. Physician 2021, 104, 28–29. [Google Scholar] [PubMed]
- Hinds, N.; Angioi, M.; Birn-Jeffery, A.; Twycross-Lewis, R. A systematic review of shoulder injury prevalence, proportion, rate, type, onset, severity, mechanism and risk factors in female artistic gymnasts. Phys. Ther. Sport 2019, 35, 106–115. [Google Scholar] [CrossRef] [PubMed]
- Sytema, R.; Dekker, R.; Dijkstra, P.U.; Duis, H.J.T.; van der Sluis, C.K. Upper extremity sports injury: Risk factors in comparison to lower extremity injury in more than 25,000 cases. Clin. J. Sport Med. 2010, 20, 256–263. [Google Scholar] [CrossRef]
- Green, M.R.; Christensen, K.P. Arthroscopic versus open Bankart procedures: A comparison of early morbidity and complications. Arthrosc. J. Arthrosc. Relat. Surg. 1993, 9, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Murray, I.R.; Ahmed, I.; White, N.J.; Robinson, C.M. Traumatic anterior shoulder instability in the athlete. Scand. J. Med. Sci. Sports 2013, 23, 387–405. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Song, Y.; Li, H.; Chen, J.; Chen, J.; Chen, S. Outcomes for Arthroscopic Repair of Combined Bankart/SLAP Lesions in the Treatment of Anterior Shoulder Instability: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2019, 7, 2325967119877804. [Google Scholar] [CrossRef]
- Widjaja, A.B.; Tran, A.; Bailey, M.; Proper, S. Correlation between Bankart and Hill-Sachs lesions in anterior shoulder dislocation. ANZ J. Surg. 2006, 76, 436–438. [Google Scholar] [CrossRef]
- DeBerardino, T.M.; Arciero, R.A.; Taylor, D.C.; Uhorchak, J.M. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes. Am. J. Sports Med. 2001, 29, 586–592. [Google Scholar] [CrossRef]
- Harada, Y.; Iwahori, Y.; Kajita, Y.; Takahashi, R.; Yokoya, S.; Sumimoto, Y.; Deie, M.; Adachi, N. Return to sports after arthroscopic bankart repair on the dominant shoulder in overhead athletes. J. Orthop. Sci. 2021, 27, 1240–1245. [Google Scholar] [CrossRef]
- Gerometta, A.; Rosso, C.; Klouche, S.; Hardy, P. Arthroscopic Bankart shoulder stabilization in athletes: Return to sports and functional outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1877–1883. [Google Scholar] [CrossRef] [PubMed]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Hohmann, E.; Feldman, M.; Hunt, T.J.; Cote, M.P.; Brand, J.C. Research Pearls: How Do We Establish the Level of Evidence? Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 3271–3277. [Google Scholar] [CrossRef] [PubMed]
- Bauer, A.; Engel, G.; Huth, J.; Mauch, F. Fourteen years of follow-up after first arthroscopic Bankart repair in athletes: Functional outcomes and magnetic resonance imaging findings. J. Shoulder Elb. Surg. 2023, 32, 546–554. [Google Scholar] [CrossRef]
- Hurley, E.T.; Davey, M.S.; Mojica, E.S.; Fried, J.W.; Gaafar, M.; Pauzenberger, L.; Mullett, H. Evaluation of factors associated with successful 5-year outcomes following arthroscopic Bankart repair in athletes. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2092–2098. [Google Scholar] [CrossRef]
- Alentorn-Geli, E.; Álvarez-Díaz, P.; Doblas, J.; Steinbacher, G.; Seijas, R.; Ares, O.; Boffa, J.J.; Cuscó, X.; Cugat, R. Return to sports after arthroscopic capsulolabral repair using knotless suture anchors for anterior shoulder instability in soccer players: Minimum 5-year follow-up study. Knee Surg. Sports Traumatol. Arthrosc. 2015, 24, 440–446. [Google Scholar] [CrossRef]
- Owens, B.D.; DeBerardino, T.M.; Nelson, B.J.; Thurman, J.; Cameron, K.L.; Taylor, D.C.; Uhorchak, J.M.; Arciero, R.A. Long-term follow-up of acute arthroscopic bankart repair for initial anterior shoulder dislocations in young athletes. Am. J. Sports Med. 2009, 37, 669–673. [Google Scholar] [CrossRef] [PubMed]
- Privitera, D.M.; Bisson, L.J.; Marzo, J.M. Minimum 10-year follow-up of arthroscopic intra-articular Bankart repair using bioabsorbable tacks. Am. J. Sports Med. 2011, 40, 100–107. [Google Scholar] [CrossRef]
- Vermeulen, A.E.; Landman, E.B.; Veen, E.J.; Nienhuis, S.; Koorevaar, C.T. Long-term clinical outcome of arthroscopic Bankart repair with suture anchors. J. Shoulder Elb. Surg. 2019, 28, e137–e143. [Google Scholar] [CrossRef]
- Valderrabano, V.; Pagenstert, G.; Horisberger, M.; Knupp, M.; Hintermann, B. Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am. J. Sports Med. 2006, 34, 993–999. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Kijima, H.; Nagamoto, H.; Kurokawa, D.; Takahashi, H.; Sano, H.; Itoi, E. Outcome of Bankart repair in contact versus non-contact athletes. Orthop. Traumatol. Surg. Res. 2015, 101, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Uribe, J.W.; Hechtman, K.S. Arthroscopically assisted repair of acute Bankart lesion. Orthopedics 1993, 16, 1019–1023. [Google Scholar] [CrossRef]
- Uhring, J.; Rey, P.-B.; Rochet, S.; Obert, L. Interest of emergency arthroscopic stabilization in primary shoulder dislocation in young athletes. Orthop. Traumatol. Surg. Res. 2014, 100, S401–S408. [Google Scholar] [CrossRef]
- Funk, L.; Tambe, A.; Badge, R. Arthroscopic rotator cuff repair in elite rugby players. Int. J. Shoulder Surg. 2009, 3, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Stein, T.; Linke, R.D.; Buckup, J.; Efe, T.; von Eisenhart-Rothe, R.; Hoffmann, R.; Jäger, A.; Welsch, F. Shoulder sport-specific impairments after arthroscopic bankart repair. Am. J. Sports Med. 2011, 39, 2404–2414. [Google Scholar] [CrossRef]
- Rangavajjula, A.; Hyatt, A.; Raneses, E.; McCrossin, J.; Cohen, S.; DeLuca, P. Return to play after treatment of shoulder labral tears in professional hockey players. Physician Sportsmed. 2016, 44, 119–125. [Google Scholar] [CrossRef]
- Petrera, M.; Dwyer, T.; Tsuji, M.R.S.; Theodoropoulos, J.S. Outcomes of arthroscopic Bankart repair in collision versus noncollision athletes. Orthopedics 2013, 36, e621–e626. [Google Scholar] [CrossRef]
- Murphy, A.I.; Hurley, E.T.; Hurley, D.J.; Pauzenberger, L.; Mullett, H. Long-term outcomes of the arthroscopic Bankart repair: A systematic review of studies at 10-year follow-up. J. Shoulder Elb. Surg. 2019, 28, 2084–2089. [Google Scholar] [CrossRef]
- Rollick, N.C.; Ono, Y.; Kurji, H.M.; Nelson, A.; Boorman, R.S.; Thornton, G.M.; Lo, I.K. Long-term outcomes of the Bankart and Latarjet repairs: A systematic review. Open Access J. Sports Med. 2017, 8, 97–105. [Google Scholar] [CrossRef]
- Hurley, E.T.; Jamal, M.S.; Ali, Z.S.; Montgomery, C.; Pauzenberger, L.; Mullett, H. Long-term outcomes of the Latarjet procedure for anterior shoulder instability: A systematic review of studies at 10-year follow-up. J. Shoulder Elb. Surg. 2019, 28, e33–e39. [Google Scholar] [CrossRef] [PubMed]
- Wilbur, R.R.; Shirley, M.B.; Nauert, R.F.; LaPrade, M.D.; Okoroha, K.R.; Krych, A.J.; Camp, C.L. Anterior Shoulder Instability in Throwers and Overhead Athletes: Long-term Outcomes in a Geographic Cohort. Am. J. Sports Med. 2021, 50, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Till, S.E.; Lu, Y.; Reinholz, A.K.; Boos, A.M.; Krych, A.J.; Okoroha, K.R.; Camp, C.L. Artificial Intelligence Can Define and Predict the “Optimal Observed Outcome” After Anterior Shoulder Instability Surgery: An Analysis of 200 Patients With 11-Year Mean Follow-Up. Arthrosc. Sports Med. Rehabil. 2023, 5, 100773. [Google Scholar] [CrossRef] [PubMed]
| PubMed | ((shoulder arthroscop*) AND ((athlete) OR (sport))) AND ((((((((outcome) OR (survivorship)) OR (5-year)) OR (10-year)) OR (mid-term)) OR (long-term)) OR (five year)) OR (ten year)) |
| Embase | (‘shoulder’/exp OR shoulder) AND arthroscop* AND (‘athlete’/exp OR athlete OR ‘sport’/exp OR sport) AND (‘outcome’/exp OR outcome OR ‘survivorship’/exp OR survivorship OR ‘5 year’ OR ‘10 year’ OR ‘mid term’ OR ‘long term’ OR ‘five year’ OR (five AND year) OR ‘ten year’ OR (ten AND year)) |
| Scopus | TITLE-ABS-KEY ((shoulder AND arthroscop*) AND (athlete OR sport) AND (outcome OR survivorship OR 5-year OR 10-year OR mid-term OR long-term OR ( five AND year) OR (ten AND year))) |
| Author | Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Data Collection | Endpoints Appropriate to Study Aim | Unbiased Assessment of Study Endpoint | Follow-Up Period Appropriate to Study Aim | Loss to Follow-Up Less than 5% | Prospective Calculation of Study Size | Total Score |
|---|---|---|---|---|---|---|---|---|---|
| Bauer et al. (2023) [15] | 2 | 1 | 2 | 2 | 1 | 2 | 0 | 0 | 10/16 |
| Hurley et al. (2022) [6] | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 2 | 13/16 |
| Alentorn-Geli et al. (2016) [17] | 2 | 1 | 0 | 2 | 1 | 2 | 2 | 0 | 10/16 |
| Owens et al. (2009) [18] | 2 | 1 | 2 | 2 | 1 | 2 | 0 | 0 | 10/16 |
| Privitera et al. (2011) [19] | 2 | 0 | 0 | 2 | 2 | 2 | 0 | 0 | 8/16 |
| Author | LOE | Study Type | Study Period | Number of Shoulders | Mean Follow-Up Time | Average Age at Surgery | Sport Type and Competition Level |
|---|---|---|---|---|---|---|---|
| Bauer et al. (2023) [15] | IV | Case Series | 2001–2008 | 46 | 14.0 ± 1.8 years (11–18 years) | 21.6 ± 4.5 years (18–30 years) | Not Reported |
| Hurley et al. (2022) [16] | III | Retrospective Cohort Study | 2012–2015 | 144 | 75.7 ± 13.6 months (60–96) | 26.9 ± 8.1 | 9 professional athletes, 95 competitive athletes, and 40 recreational athletes; 102 of the 144 total patients were collision athletes |
| Alentorn-Geli et al. (2016) [17] | IV | Cross Sectional Case Series | 2002–2009 | 57 | 8 years 1 (5–10 years) | 22 years 1 (16–28 years) | All competitive soccer players (Tegner score of 9) |
| Owens et al. (2009) [18] | IV | Case Series | March 1992–November 1998 | 40 | 11.7 years (9.1–13.9 years) | 20.3 years (17–23 years) | 1 collegiate soccer player, 39 unspecified athletes in the military |
| Privitera et al. (2011) [19] | IV | Case Series | 1992–1999 | 20 | 13.5 years (10.75–17.5 years) | 25 years (15–56 years) 2 | All recreational |
| Author | Surgical Indication | Surgical Intervention | Intraoperative Findings | PROMs at Latest Follow-Up | Radiographic Findings at Latest Follow-Up | Patient Satisfaction |
|---|---|---|---|---|---|---|
| Bauer et al. (2023) [15] | Primary traumatic anterior-inferior shoulder instability | Bankart repair | Complete labral lesion (16), SLAP lesion (4), Hill–Sachs lesion (27) | Constant score: 96.8 ± 5.1 Rowe score: 83.4 ± 24.4 WOSI: 90.7 ± 12.4 | Anchors still visible: 12 Bone marrow edema: 11 Joint effusion: 14 Cysts: 9 Osteoarthritis: 9 2 | 42 satisfied 4 dissatisfied (all 4 had redislocation and 1 also had developed osteoarthritis) |
| Hurley et al. (2022) [16] | Traumatic anterior shoulder instability | Bankart repair | Off-track Hill–Sachs lesion (11) | VAS: 2.1 ± 2 SIRSI: 63.7 ± 25.7 SSV: 85.8 ± 14.4 | Glenoid bone loss: 1.9% ± 4.1% | Satisfaction on scale of 1–5: 1 (1 patient) 2 (6 patients) 3 (18 patients) 4 (43 patients) 5 (76 patients) 121/144 would undergo surgery again |
| Alentorn-Geli et al. (2016) [17] | Anterior glenohumeral instability | Bankart repair | Bankart lesions (46), anterior labroligamentous periosteal sleeve avulsion (11), Hill–Sachs lesions (all), type I SLAP lesion (5), type II SLAP lesion (3), Buford complex (2) | Rowe: 80 (25–100) 1 QuickDASH: 2.3 (0–12.5) 1 QuickDASH sports score: 0 (0–18.8) 1 | Not Reported | Not Reported |
| Owens et al. (2009) [18] | First-time traumatic anterior glenohumeral dislocation | Bankart repair | Not Reported | SANE: 91.7 (40–100) WOSI: 371.7/82.3% (9–1875) ROWE subjective: 25.3 (0–30) SST: 11.1 (6–12) ASES: 90.9 (31.7–100) SF-36 Physical Component: 94.4 (25–100) | Not Reported | Would have surgery again: mean of 9.1 (1–10-point scale) |
| Privitera et al. (2011) [19] | Anterior shoulder instability | Bankart repair; concomitant radiofrequency capsulorrhaphy due to capsular laxity (2) | Bankart lesion (18), glenoid chondromalacia (5) | WOSI: 80% (physical: 77%, sports/rec: 80%, lifestyle: 87%, emotions: 77%) DASH Main: 7.3 (0–39.2) DASH Work: 7.64 (0–44) DASH sports/arts: 14.17 (0–69) | Absent arthrosis: 4/20 Mild arthrosis: 8/20 Moderate arthrosis: 5/20 Severe arthrosis: 3/20 Drill holes used to implant tacks invisible in 8 shoulders, hardly visible in 3 shoulders, and clearly visible in 9 shoulders (less than 3 mm in 5 shoulders and greater than 3 mm in 4 shoulders) Absent Hill–Sachs lesions: 9/20 Small Hill–Sachs lesions: 10/20 Moderate Hill–Sachs lesions: 1/20 | Not Reported |
| Author | Number of Patients Returning to Sports | Number of Patients Returning to Sports at Pre-Injury Level | Time to RTS | Sports Level at Follow-Up | Rate of Recurrent Instability | Time from Surgery to Recurrent Instability |
|---|---|---|---|---|---|---|
| Bauer et al. (2023) [15] | 39/46 (84.8%) | 38/46 (82.6%) | 6.3 ± 3.0 months | Valderrabano Sports Level: 1.6 ± 1.1 (1–5 h of sports activity per week) | Redislocations: 10 Revision surgery: 6 | 31.8 ± 32.5 months (7–108 months) to first redislocation |
| Hurley et al. (2022) [16] | 116/144 (80.6%) | 92/144 (63.9%) | 6.2 ± 2.7 months | Not Reported | Redislocations: 15 Subluxations: 3 Revision surgery: 15 | Not Reported |
| Alentorn-Geli et al. (2016) [17] | 49/57 (86%) 8 who did not RTS quit because of non-shoulder reasons | 36/57 (63.2%) | 4 months (3–5 months) 1 | Not Reported | Redislocations: 6 Revision surgery: 4 All redislocations of traumatic origin | Not Reported |
| Owens et al. (2009) [18] | 39/39 (100%) | Percentage of pre-injury shoulder function: 93.3% (40–105%) | Not Reported | Tegner: 6.5 (3–10) APFT: 287.45 Number of push-ups in two minutes: 72.8 (20–100) | Redislocations: 6 Subluxations: 9 Revision surgery: 6 | 37 months to redislocation, 22 months to subluxation |
| Privitera et al. (2011) [19] | 14/20 (70%) 4 quit because of shoulder problems; 2 not interested in sports without shoulder problems | 8/20 (40%) (6/20 at limited level) | Not Reported | Not Reported | Redislocations: 5 Subluxations: 1 Instability: 1 Revision surgery: 3 6/7 instances due to trauma | 4.2 years (0.25–14.7 years) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akhtar, M.; Wen, J.; Razick, D.; Shehabat, M.; Saeed, A.; Baig, O.; Asim, M.; Tokhi, I.; Aamer, S.; Akhtar, M.B. Mid- to Long-Term Outcomes of Arthroscopic Shoulder Stabilization in Athletes: A Systematic Review. J. Clin. Med. 2023, 12, 5730. https://doi.org/10.3390/jcm12175730
Akhtar M, Wen J, Razick D, Shehabat M, Saeed A, Baig O, Asim M, Tokhi I, Aamer S, Akhtar MB. Mid- to Long-Term Outcomes of Arthroscopic Shoulder Stabilization in Athletes: A Systematic Review. Journal of Clinical Medicine. 2023; 12(17):5730. https://doi.org/10.3390/jcm12175730
Chicago/Turabian StyleAkhtar, Muzammil, Jimmy Wen, Daniel Razick, Mouhamad Shehabat, Ali Saeed, Osamah Baig, Maaz Asim, Ilham Tokhi, Sonia Aamer, and Muhammad Bilal Akhtar. 2023. "Mid- to Long-Term Outcomes of Arthroscopic Shoulder Stabilization in Athletes: A Systematic Review" Journal of Clinical Medicine 12, no. 17: 5730. https://doi.org/10.3390/jcm12175730
APA StyleAkhtar, M., Wen, J., Razick, D., Shehabat, M., Saeed, A., Baig, O., Asim, M., Tokhi, I., Aamer, S., & Akhtar, M. B. (2023). Mid- to Long-Term Outcomes of Arthroscopic Shoulder Stabilization in Athletes: A Systematic Review. Journal of Clinical Medicine, 12(17), 5730. https://doi.org/10.3390/jcm12175730