The Impact of Diffuse Idiopathic Skeletal Hyperostosis on Nutritional Status, Neurological Outcome, and Perioperative Complications in Patients with Cervical Spinal Cord Injury
Abstract
:1. Introduction
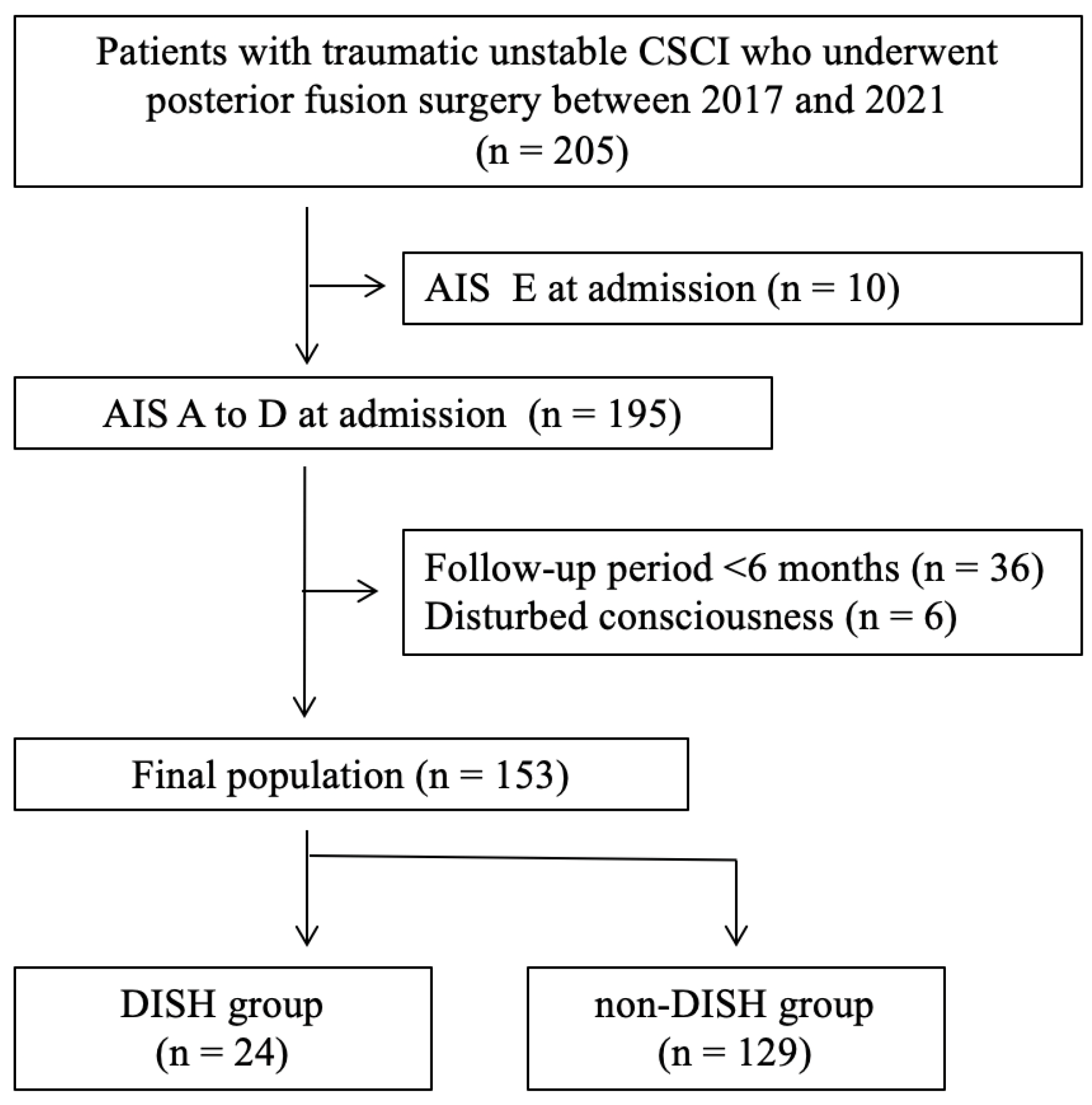
2. Materials and Methods
- Patient selection
- Variables
- Surgical indication
- Grouping
- Statistical analyses
3. Results
- Patient characteristics
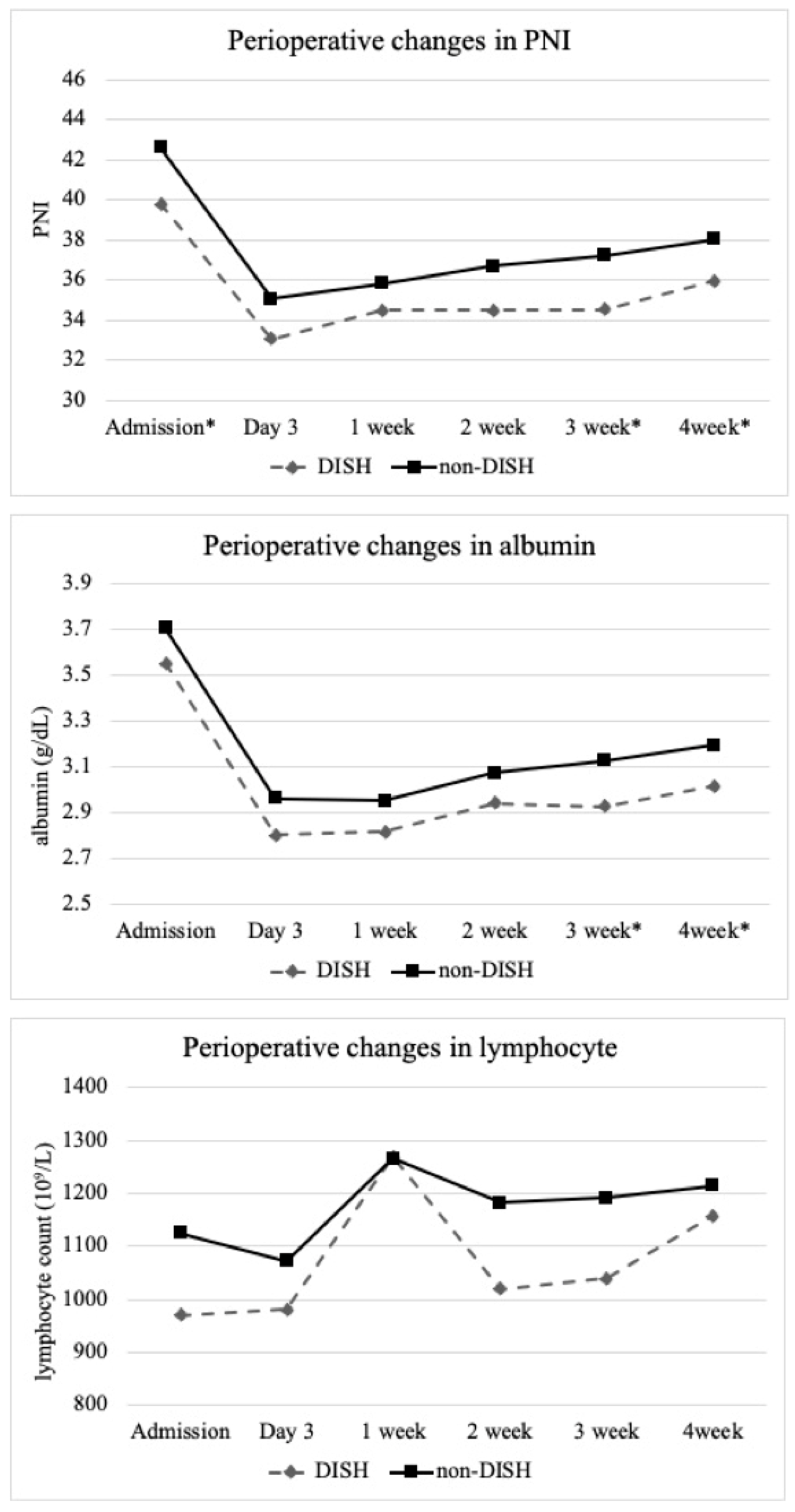
- Perioperative changes in laboratory data
- Clinical outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Resnick, D.; Niwayama, G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology 1976, 119, 559–568. [Google Scholar] [CrossRef]
- Kuperus, J.S.; Mohamed Hoesein, F.A.A.; de Jong, P.A.; Verlaan, J.J. Diffuse idiopathic skeletal hyperostosis: Etiology and clinical relevance. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101527. [Google Scholar] [CrossRef] [PubMed]
- Westerveld, L.A.; Verlaan, J.J.; Oner, F.C. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur. Spine J. 2009, 18, 145–156. [Google Scholar] [CrossRef]
- Teunissen, F.R.; Verbeek, B.M.; Cha, T.D.; Schwab, J.H. Spinal cord injury after traumatic spine fracture in patients with ankylosing spinal disorders. J. Neurosurg. Spine 2017, 27, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Caron, T.; Bransford, R.; Nguyen, Q.; Agel, J.; Chapman, J.; Bellabarba, C. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976) 2010, 35, E458–E464. [Google Scholar] [CrossRef]
- Bransford, R.J.; Koller, H.; Caron, T.; Zenner, J.; Hitzl, W.; Tomasino, A.; Mayer, M. Cervical spine trauma in diffuse idiopathic skeletal hyperostosis: Injury characteristics and outcome with surgical treatment. Spine (Phila Pa 1976) 2012, 37, 1923–1932. [Google Scholar] [CrossRef]
- Ull, C.; Yilmaz, E.; Hoffmann, M.F.; Reinke, C.; Aach, M.; Schildhauer, T.A.; Kruppa, C. Factors Associated With Major Complications and Mortality During Hospitalization in Patients With Ankylosing Spondylitis Undergoing Surgical Management for a Spine Fracture. Glob. Spine J. 2021, 12, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Richard-Denis, A.; Feldman, D.E.; Thompson, C.; Mac-Thiong, J.M. The impact of acute management on the occurrence of medical complications during the specialized spinal cord injury acute hospitalization following motor-complete cervical spinal cord injury. J. Spinal Cord. Med. 2018, 41, 388–396. [Google Scholar] [CrossRef]
- Galeiras Vázquez, R.; Rascado Sedes, P.; Mourelo Fariña, M.; Montoto Marqués, A.; Ferreiro Velasco, M.E. Respiratory management in the patient with spinal cord injury. Biomed. Res. Int. 2013, 2013, 168757. [Google Scholar] [CrossRef] [PubMed]
- Cifu, D.X.; Seel, R.T.; Kreutzer, J.S.; McKinley, W.O. A multicenter investigation of age-related differences in lengths of stay, hospitalization charges, and outcomes for a matched tetraplegia sample. Arch. Phys. Med. Rehabil. 1999, 80, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Chikuda, H.; Koyama, Y.; Matsubayashi, Y.; Ogata, T.; Ohtsu, H.; Sugita, S.; Sumitani, M.; Kadono, Y.; Miura, T.; Tanaka, S.; et al. Effect of Early vs. Delayed Surgical Treatment on Motor Recovery in Incomplete Cervical Spinal Cord Injury with Preexisting Cervical Stenosis: A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2133604. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Vaccaro, A.; Wilson, J.R.; Singh, A.; WCadotte, D.; Harrop, J.S.; Aarabi, B.; Shaffrey, C.; Dvorak, M.; Fisher, C.; et al. Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS ONE 2012, 7, e32037. [Google Scholar] [CrossRef] [PubMed]
- Khorasanizadeh, M.; Yousefifard, M.; Eskian, M.; Lu, Y.; Chalangari, M.; Harrop, J.S.; Jazayeri, S.B.; Seyedpour, S.; Khodaei, B.; Hosseini, M.; et al. Neurological recovery following traumatic spinal cord injury: A systematic review and meta-analysis. J. Neurosurg. Spine 2019, 30, 683–699. [Google Scholar] [CrossRef] [PubMed]
- Tong, B.; Jutzeler, C.R.; Cragg, J.J.; Grassner, L.; Schwab, J.M.; Casha, S.; Geisler, F.; Kramer, J.L.K. Serum Albumin Predicts Long-Term Neurological Outcomes After Acute Spinal Cord Injury. Neurorehabilit. Neural Repair 2018, 32, 7–17. [Google Scholar] [CrossRef]
- Rupp, R.; Biering-Sørensen, F.; Burns, S.P.; Graves, D.E.; Guest, J.; Jones, L.; Read, M.S.; Rodriguez, G.M.; Schuld, C.; Tansey-Md, K.E.; et al. International Standards for Neurological Classification of Spinal Cord Injury: Revised. Top. Spinal Cord. Inj. Rehabil. 2021, 27, 1–22. [Google Scholar] [CrossRef]
- Acarbas, A. A Novel Prognostic Marker in Patients Undergoing Spinal Surgery: Prognostic Nutritional Index. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2019, 80, 470–474. [Google Scholar] [CrossRef]
- Mangram, A.J.; Horan, T.C.; Pearson, M.L.; Silver, L.C.; Jarvis, W.R. Guideline for Prevention of Surgical Site Infection, Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am. J. Infect. Control 1999, 27, 97–132. [Google Scholar] [CrossRef]
- Grossman, R.G.; Frankowski, R.F.; Burau, K.D.; Toups, E.G.; Crommett, J.W.; Johnson, M.M.; Fehlings, M.G.; Tator, C.H.; Shaffrey, C.I.; Harkema, S.J.; et al. Incidence and severity of acute complications after spinal cord injury. J. Neurosurg. Spine 2012, 17, 119–128. [Google Scholar] [CrossRef]
- Inouye, S.K.; van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann. Intern. Med. 1990, 113, 941–948. [Google Scholar] [CrossRef]
- Vaccaro, A.R.; Hulbert, R.J.; Patel, A.A.; Fisher, C.; Dvorak, M.; Lehman, R.A., Jr.; Anderson, P.; Harrop, J.; Oner, F.C.; Arnold, P.; et al. The subaxial cervical spine injury classification system: A novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007, 32, 2365–2374. [Google Scholar] [CrossRef]
- Cruz, H.Y.; Joaquim, A.F.; Tedeschi, H.; Patel, A.A. Evaluation of the SLICS use in the treatment of subaxial cervical spine injuries. Arq. Neuropsiquiatr. 2015, 73, 445–449. [Google Scholar] [CrossRef]
- Murakami, Y.; Mashima, N.; Morino, T.; Fukuda, T.; Iwase, M.; Hino, M.; Misaki, H.; Miura, H. Association Between Vertebral Fracture and Diffuse Idiopathic Skeletal Hyperostosis. Spine (Phila Pa 1976) 2019, 44, E1068–E1074. [Google Scholar] [CrossRef]
- Rabin, J.C.; Ramirez, K. Hydroxychloroquine Ocular Toxicity: Lessons Learned. J. Rheumatol. 2019, 46, 1640–1641. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, H.; Terai, H.; Yamada, K.; Suzuki, A.; Dohzono, S.; Matsumoto, T.; Nakamura, H. Prevalence of Diffuse Idiopathic Skeletal Hyperostosis in Patients with Spinal Disorders. Asian Spine J. 2017, 11, 63–70. [Google Scholar] [CrossRef]
- Hirasawa, A.; Wakao, N.; Kamiya, M.; Takeuchi, M.; Kawanami, K.; Murotani, K.; Matsuo, T.; Deie, M. The prevalence of diffuse idiopathic skeletal hyperostosis in Japan—The first report of measurement by CT and review of the literature. J. Orthop. Sci. 2016, 21, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Vo, A.K.; Geisler, F.; Grassner, L.; Schwab, J.; Whiteneck, G.; Jutzeler, C.; Kramer, J.L.K. Serum albumin as a predictor of neurological recovery after spinal cord injury: A replication study. Spinal Cord. 2021, 59, 282–290. [Google Scholar] [CrossRef]
- Weaving, G.; Batstone, G.F.; Jones, R.G. Age and sex variation in serum albumin concentration: An observational study. Ann. Clin. Biochem. 2016, 53, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Mader, R.; Pappone, N.; Baraliakos, X.; Eshed, I.; Sarzi-Puttini, P.; Atzeni, F.; Bieber, A.; Novofastovski, I.; Kiefer, D.; Verlaan, J.J.; et al. Diffuse Idiopathic Skeletal Hyperostosis (DISH) and a Possible Inflammatory Component. Curr. Rheumatol. Rep. 2021, 23, 6. [Google Scholar] [CrossRef]
- Nguyen, T.C.; Yahara, Y.; Yasuda, T.; Seki, S.; Suzuki, K.; Watanabe, K.; Makino, H.; Kamei, K.; Mori, K.; Kawaguchi, Y. Morphological characteristics of DISH in patients with OPLL and its association with high-sensitivity CRP: Inflammatory DISH. Rheumatology 2022, 61, 3981–3988. [Google Scholar] [CrossRef] [PubMed]
- Reinhold, M.; Knop, C.; Kneitz, C.; Disch, A. Spine Fractures in Ankylosing Diseases: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018, 8, 56s–68s. [Google Scholar] [CrossRef]
- Hishiya, T.; Ishikawa, T.; Ota, M. Posterior spinal fixation using penetrating endplate screws in patients with diffuse idiopathic skeletal hyperostosis-related thoracolumbar fractures. J. Neurosurg. Spine 2021, 34, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Oudkerk, S.F.; Hoesein, F.A.; Öner, F.C.; Verlaan, J.J.; de Jong, P.A.; Kuperus, J.S.; Cho, M.; McDonald, M.L.; Lynch, D.A.; Silverman, E.K.; et al. Diffuse Idiopathic Skeletal Hyperostosis in Smokers and Restrictive Spirometry Pattern: An Analysis of the COPDGene Cohort. J. Rheumatol. 2020, 47, 531–538. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Total | DISH Group n = 24 | Non-DISH Group n = 129 | p Value |
|---|---|---|---|---|
| Age (mean ± SD), years | 67.0 ± 13.2 | 72.1 ± 9.7 | 65.9 ± 13.6 | 0.036 * |
| Sex male/female, n | 130/23 | 24/0 | 106/23 | 0.026 * |
| Height (mean ± SD), cm | 165.3 ± 8.4 | 166.8 ± 6.5 | 165.0 ± 8.8 | 0.336 |
| Body weight (mean ± SD), kg | 65.5 ± 14.3 | 70.4 ± 12.5 | 64.6 ± 14.6 | 0.069 |
| BMI (mean ± SD), kg/m2 | 23.9 ± 4.3 | 25.2 ± 3.4 | 23.6 ± 4.4 | 0.099 |
| Time to examination (mean ± SD), hours | 20.8 ± 34.5 | 24.2 ± 37.3 | 20.2 ± 34.2 | 0.605 |
| Comorbidities, n | ||||
| OPLL | 47 (30.7%) | 10 (41.7%) | 37 (28.7%) | 0.205 |
| Alcohol | 72 (45.8%) | 12 (50.0%) | 60 (45.0%) | 0.663 |
| Smoking | 35 (22.9%) | 3 (12.5%) | 32 (24.8%) | 0.188 |
| Hypertension | 68 (43.1%) | 15 (62.5%) | 51 (39.5%) | 0.037 * |
| Hyperlipidemia | 19 (12.4%) | 4 (16.7%) | 15 (11.6%) | 0.503 |
| Ischemic heart disease | 12 (7.8%) | 3 (12.5%) | 9 (7.0%) | 0.403 |
| Diabetes mellitus | 34 (22.2%) | 7 (29.2%) | 27 (20.9%) | 0.373 |
| Malignancy | 27 (17.6%) | 6 (25.0%) | 21 (16.3%) | 0.380 |
| Mental disease | 9 (5.9%) | 1 (4.2%) | 8 (6.2%) | 1.000 |
| Chronic renal disfunction | 32 (20.9%) | 5 (20.8%) | 27 (20.9%) | 0.991 |
| Traumatic impact, n | 0.009 * | |||
| Low | 59 (38.6%) | 15 (62.5%) | 44 (34.1%) | |
| High | 94 (61.4%) | 9 (37.5%) | 85 (65.9%) | |
| AIS grade on admission, n | 0.352 | |||
| A | 37 | 7 | 30 | |
| B | 19 | 5 | 14 | |
| C | 54 | 8 | 46 | |
| D | 43 | 4 | 39 | |
| NLI, n | 0.309 | |||
| C2 | 27 | 5 | 22 | |
| C3 | 37 | 8 | 29 | |
| C4 | 59 | 8 | 51 | |
| C5 | 14 | 0 | 14 | |
| C6 | 5 | 0 | 5 | |
| C7 | 5 | 2 | 3 | |
| C8 | 6 | 1 | 5 | |
| MIS on admission, mean ± SD | ||||
| Upper extremity | 19.6 ± 15.0 | 20.7 ± 16.7 | 19.4 ± 14.7 | 0.696 |
| Lower extremity | 17.7 ± 18.4 | 14.8 ± 18.8 | 183 ± 18.4 | 0.404 |
| Total | 37.3 ± 29.6 | 35.5 ± 29.8 | 37.6 ± 29.8 | 0.748 |
| Time to surgery (mean ± SD), hours | 22.8 ± 34.5 | 26.2 ± 37.3 | 22.2 ± 34.2 | 0.605 |
| Number of fusion levels | 2.2 ± 1.4 | 4.2 ± 1.5 | 1.8 ± 0.9 | <0.001 * |
| Length of surgery (minutes) | 146 ± 52 | 200 ± 60 | 136 ± 44 | <0.001 * |
| Estimated blood loss (mL) | 210 ± 277 | 438 ± 444 | 169 ± 212 | 0.008 * |
| Perioperative transfusion | 25 (16.3%) | 10 (41.7%) | 15 (11.6%) | <0.001 * |
| Laboratory Data, Mean ± SD | DISH Group n = 24 | Non-DISH Group n = 129 | p Value |
|---|---|---|---|
| Serum albumin at admission, g/dL | 3.55 ± 0.43 | 3.70 ± 0.41 | 0.118 |
| Serum albumin at day 3, g/dL | 2.80 ± 0.28 | 2.96 ± 0.38 | 0.057 |
| Serum albumin at 1 week, g/dL | 2.82 ± 0.32 | 2.95 ± 0.43 | 0.156 |
| Serum albumin at 2 weeks, g/dL | 2.94 ± 0.40 | 3.07 ± 0.46 | 0.199 |
| Serum albumin at 3 weeks, g/dL | 2.93 ± 0.42 | 3.13 ± 0.46 | 0.049 * |
| Serum albumin at 4 weeks, g/dL | 3.02 ± 0.37 | 3.20 ± 0.50 | 0.042 * |
| Lymphocyte at admission, count ×109/L | 971 ± 325 | 1127 ± 454 | 0.134 |
| Lymphocyte at day 3, count ×109/L | 980 ± 378 | 1073 ± 396 | 0.300 |
| Lymphocyte at 1 week, count ×109/L | 1269 ± 554 | 1270 ± 496 | 0.996 |
| Lymphocyte at 2 weeks, count ×109/L | 1020 ± 305 | 1184 ± 414 | 0.068 |
| Lymphocyte at 3 weeks, count ×109/L | 1040 ± 350 | 1198 ± 415 | 0.088 |
| Lymphocyte at 4 weeks, count ×109/L | 1158 ± 329 | 1221 ± 360 | 0.423 |
| PNI at admission | 39.8 ± 4.6 | 42.5 ± 4.6 | 0.014 * |
| PNI at day 3 | 33.1 ± 3.4 | 35.1 ± 4.9 | 0.063 |
| PNI at 1 week | 34.5 ± 4.0 | 35.8 ± 5.3 | 0.257 |
| PNI at 2 weeks | 34.5 ± 4.4 | 36.7 ± 5.6 | 0.077 |
| PNI at 3 weeks | 34.5 ± 5.0 | 37.2 ± 5.6 | 0.031 * |
| PNI at 4 weeks | 35.9 ± 4.1 | 38.1 ± 5.8 | 0.032 * |
| AIS Grade at Discharge | ||||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | Total | |
| AIS grade at admission | ||||||
| A | 6 | 1 | 0 | 0 | 0 | 7 |
| B | 0 | 1 | 1 | 3 | 0 | 5 |
| C | 0 | 0 | 1 | 7 | 0 | 8 |
| D | 0 | 0 | 0 | 3 | 1 | 4 |
| Total | 6 | 2 | 2 | 13 | 1 | 24 |
| AIS Grade at Discharge | ||||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | Total | |
| AIS grade at admission | ||||||
| A | 14 | 6 | 6 | 4 | 0 | 30 |
| B | 0 | 0 | 8 | 6 | 0 | 14 |
| C | 0 | 0 | 5 | 41 | 0 | 46 |
| D | 0 | 0 | 0 | 33 | 6 | 39 |
| Total | 14 | 6 | 19 | 84 | 6 | 129 |
| Perioperative Complications | DISH Group n = 24 | Non-DISH Group n = 129 | p Value |
|---|---|---|---|
| Ventilator management | 4 (16.7%) | 4 (3.1%) | 0.022 * |
| Surgical site infection | 0 (0%) | 3 (2.3%) | 1.000 |
| Pneumonia | 7 (29.2%) | 11 (8.5%) | 0.010 * |
| Urinary tract infection | 10 (41.7%) | 35 (27.1%) | 0.151 |
| Cardiopulmonary dysfunction | 5 (20.9%) | 25 (19.4%) | 0.869 |
| Deep venous thrombosis | 7 (29.2%) | 54 (41.9%) | 0.244 |
| Delirium | 2 (8.3%) | 16 (12.4%) | 0.740 |
| Medical costs (USD) | |||
| First month after admission (A; n = 148) | 2474 ± 878 | 2233 ± 568 | 0.217 |
| First 2 months after admission (B, n = 134) | 3232 ± 937 | 2937 ± 588 | 0.179 |
| First 3 months after admission (C, n = 120) | 3965 ± 1033 | 3569 ± 642 | 0.131 |
| Second month (B-A; n = 134) | 646 ± 251 | 677 ± 152 | 0.454 |
| Third month (C-B; n = 120) | 622 ± 118 | 613 ± 117 | 0.757 |
| AIS grade at discharge, n | 0.329 | ||
| A | 6 (25.0%) | 14 (10.6%) | |
| B | 2 (8.3%) | 6 (4.5%) | |
| C | 2 (8.3%) | 19 (14.7%) | |
| D | 13 (54.2%) | 84 (65.1%) | |
| E | 1 (4.2%) | 6 (4.5%) | |
| AIS improvement (≥1 grade improvement) | 13 (54.2%) | 79 (61.2%) | 0.516 |
| MIS at discharge, mean ± SD | |||
| Upper extremity | 31.7 ± 18.8 | 32.9 ± 15.2 | 0.738 |
| Lower extremity | 25.7 ± 21.5 | 31.8 ± 19.4 | 0.170 |
| Total | 57.4 ± 37.9 | 65.2 ± 32.4 | 0.298 |
| Improvement of MIS, mean ± SD | |||
| Upper extremity | 11.0 ± 14.1 | 13.9 ± 12.2 | 0.305 |
| Lower extremity | 10.9 ± 12.9 | 13.7 ± 16.4 | 0.431 |
| Total | 21.9 ± 25.1 | 27.5 ± 21.7 | 0.258 |
| Length of hospital stay (days) | 208 ± 101 | 202 ± 126 | 0.833 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shimizu, T.; Suda, K.; Harmon, S.M.; Komatsu, M.; Ota, M.; Ushirozako, H.; Minami, A.; Takahata, M.; Iwasaki, N.; Takahashi, H.; et al. The Impact of Diffuse Idiopathic Skeletal Hyperostosis on Nutritional Status, Neurological Outcome, and Perioperative Complications in Patients with Cervical Spinal Cord Injury. J. Clin. Med. 2023, 12, 5714. https://doi.org/10.3390/jcm12175714
Shimizu T, Suda K, Harmon SM, Komatsu M, Ota M, Ushirozako H, Minami A, Takahata M, Iwasaki N, Takahashi H, et al. The Impact of Diffuse Idiopathic Skeletal Hyperostosis on Nutritional Status, Neurological Outcome, and Perioperative Complications in Patients with Cervical Spinal Cord Injury. Journal of Clinical Medicine. 2023; 12(17):5714. https://doi.org/10.3390/jcm12175714
Chicago/Turabian StyleShimizu, Tomoaki, Kota Suda, Satoko Matsumoto Harmon, Miki Komatsu, Masahiro Ota, Hiroki Ushirozako, Akio Minami, Masahiko Takahata, Norimasa Iwasaki, Hiroshi Takahashi, and et al. 2023. "The Impact of Diffuse Idiopathic Skeletal Hyperostosis on Nutritional Status, Neurological Outcome, and Perioperative Complications in Patients with Cervical Spinal Cord Injury" Journal of Clinical Medicine 12, no. 17: 5714. https://doi.org/10.3390/jcm12175714
APA StyleShimizu, T., Suda, K., Harmon, S. M., Komatsu, M., Ota, M., Ushirozako, H., Minami, A., Takahata, M., Iwasaki, N., Takahashi, H., & Yamazaki, M. (2023). The Impact of Diffuse Idiopathic Skeletal Hyperostosis on Nutritional Status, Neurological Outcome, and Perioperative Complications in Patients with Cervical Spinal Cord Injury. Journal of Clinical Medicine, 12(17), 5714. https://doi.org/10.3390/jcm12175714





