Effects of Non-Ablative Solid-State Vaginal Laser (SSVL) for the Treatment of Vulvovaginal Atrophy in Breast Cancer Survivors after Adjuvant Aromatase Inhibitor Therapy: Preliminary Results
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Protocol
2.3. Assessment Tools
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Portman, D.J.; Gass, M.L. Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: New terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North. American Menopause Society. Menopause 2014, 21, 1063–1068. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, J.; Chen, A.; Dagur, G.; Suh, Y.; Smith, N.; Cali, B.; Khan, S.A. Genitourinary syndrome of menopause: An overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am. J. Obstet. Gynecol. 2016, 215, 704–711. [Google Scholar] [CrossRef]
- Fallowfield, L.; Cella, D.; Cuzick, J.; Francis, S.; Locker, G.; Howell, A. Quality of life of postmenopausal women in the Arimidex, Tamoxifen, Alone or in Combination (ATAC) Adjuvant Breast Cancer Trial. J. Clin. Oncol. 2004, 22, 4261–4271. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Keen, J.C.; Davidson, N.E. The biology of breast carcinoma. Cancer 2003, 97 (Suppl. S3), 825–833. [Google Scholar] [CrossRef]
- Marino, J.L.; Saunders, C.M.; Emery, L.I.; Green, H.; Doherty, D.A.; Hickey, M. Nature and severity of menopausal symptoms and their impact on quality of life and sexual function in cancer survivors compared with women without a cancer history. Menopause 2014, 21, 267–274. [Google Scholar] [CrossRef]
- Biglia, N.; Bounous, V.E.; D’Alonzo, M.; Ottino, L.; Tuninetti, V.; Robba, E.; Perrone, T. Vaginal Atrophy in Breast Cancer Survivors: Attitude and Approaches Among Oncologists. Clin. Breast. Cancer 2017, 17, 611–617. [Google Scholar] [CrossRef]
- Nappi, R.E.; Kokot-Kierepa, M. Vaginal Health: Insights, Views & Attitudes (VIVA)—Results from an international survey. Climacteric 2012, 15, 36–44. [Google Scholar] [CrossRef]
- Wiśniewska, I.; Jochymek, B.; Lenart-Lipińska, M.; Chabowski, M. The pharmacological and hormonal therapy of hot flushes in breast cancer survivors. Breast Cancer 2016, 23, 178–182. [Google Scholar] [CrossRef][Green Version]
- Baum, M.; Budzar, A.U.; Cuzick, J.; Forbes, J.; Houghton, J.H.; Klijn, J.G.; Sahmoud, T. ATAC Trialists’ Group. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: First results of the ATAC randomised trial. Lancet 2002, 359, 2131–2139. [Google Scholar]
- Baumgart, J.; Nilsson, K.; Stavreus-Evers, A.; Kask, K.; Villman, K.; Lindman, H.; Kallak, T.; Sundström-Poromaa, I. Urogenital disorders in women with adjuvant endocrine therapy after early breast cancer. Am. J. Obstet. Gynecol. 2011, 204, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Lubián-López, D.M.; Butrón-Hinojo, C.A.; Sánchez-Prieto, M.; Mendoza, N.; Sánchez-Borrego, R. Sexual Dysfunction in Postmenopausal Women with Breast Cancer on Adjuvant Aromatase Inhibitor Therapy. Breast Care 2020, 16, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Naumova, I.; Castelo-Branco, C. Current treatment options for postmenopausal vaginal atrophy. Int. J. Womens Health 2018, 10, 387–395. [Google Scholar] [CrossRef]
- Holmberg, L.; Anderson, H. HABITS steering and data monitoring committees. HABITS (hormonal replacement therapy after breast cancer--is it safe?), a randomised comparison: Trial stopped. Lancet 2004, 363, 453–455. [Google Scholar] [CrossRef] [PubMed]
- Lu, R.; Serrero, G. Mediation of estrogen mitogenic effect in human breast cancer MCF-7 cells by PC-cell-derived growth factor (PCDGF/granulin precursor). Proc. Natl. Acad. Sci. USA 2001, 98, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Lubián-López, D.M. Management of genitourinary syndrome of menopause in breast cancer survivors: An update. World J. Clin. Oncol. 2022, 13, 71–100. [Google Scholar] [CrossRef] [PubMed]
- FDA Warns Against Use of Energy-Based Devices to Perform Vaginal ‘Rejuvenation’ or Vaginal Cosmetic Procedures: FDA Safety Communication. Available online: https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm615013.htm (accessed on 2 August 2018).
- Elective Female Genital Cosmetic Surgery. ACOGCommitee Opinion No. 795. American College of Obstetricians and Gynecologists. Obstet. Gynecol. 2020, 135, e36–e42. [Google Scholar]
- Alshiek, J.; Garcia, B.; Minassian, V.; Iglesia, C.B.; Clark, A.; Sokol, E.R.; Murphy, M.; Malik, S.A.; Tran, A.; Shobeiri, S.A. Vaginal Energy-Based Devices. Female Pelvic. Med. Reconstr. Surg. 2020, 26, 287–298. [Google Scholar] [CrossRef]
- Bachmann, G.A.; Notelovitz, M.; Kelly, S.J.; Thompson, C.; Owens, A. Long-term non-hormonal treatment of vaginal dryness. Clin. Pr. Sex. 1992, 8, 3–8. [Google Scholar]
- Palacios, S.; Cancelo, M.J.; Castelo Branco, C.; Llaneza, P.; Molero, F.; Borrego, R.S. Vulvar and vaginal atrophy as viewed by the Spanish REVIVE participants: Symptoms, management and treatment perceptions. Climacteric 2017, 20, 55–61. [Google Scholar] [CrossRef]
- Meisels, A. The maturation value. Acta Cytol. 1967, 11, 249. [Google Scholar]
- Roy, S.; Caillouette, J.C.; Roy, T.; Faden, J.S. Vaginal pH is similar to follicle stimulating hormone for menopause diagnosis. Am. J. Obstet. Gynecol. 2004, 190, 272–277. [Google Scholar] [CrossRef]
- Rosen, R.; Brown, C.; Heiman, J.; Leiblum, S.; Meston, C.; Shabsigh, R.; Ferguson, D.; D’Agostino, R., Jr. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J. Sex. Marital. Ther. 2000, 26, 191–208. [Google Scholar] [CrossRef]
- Baser, R.E.; Li, Y.; Carter, J. Psychometric validation of the Female Sexual Function Index (FSFI) in cancer survivors. Cancer 2012, 118, 4606–4618. [Google Scholar] [CrossRef]
- Sprangers, M.A.; Groenvold, M.; Arraras, J.I.; Franklin, J.; Velde, A.T.; Muller, M.; Franzini, L.; Williams, A.; de Haes, H.C.J.M.; Hopwood, P.; et al. The European Organisation for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: First results from a three-country field study. J. Clin. Oncol. 1996, 10, 2756–2768. [Google Scholar] [CrossRef]
- Hutchinson-Colas, J.; Segal, S. Genitourinary syndrome of menopause and the use of laser therapy. Maturitas 2015, 82, 342–345. [Google Scholar] [CrossRef]
- Khamis, Y.; Abdelhakim, A.M.; Labib, K.; Islam, B.A.; Nassar, S.A.; Motaal, A.O.A.; Saleh, D.M.; Abdou, H.; Abbas, A.M.; Mojahed, E.M. Vaginal CO2 laser therapy versus sham for genitourinary syndrome of menopause management: A systematic review and meta-analysis of randomized controlled trials. Menopause 2021, 28, 1316–1322. [Google Scholar] [CrossRef]
- Quick, A.M.; Dockter, T.; Le-Rademacher, J.; Salani, R.; Hudson, C.; Hundley, A.; Terstriep, S.; Streicher, L.; Faubion, S.; Loprinzi, C.L.; et al. Pilot study of fractional CO2 laser therapy for genitourinary syndrome of menopause in gynecologic cancer survivors. Maturitas 2021, 144, 37–44. [Google Scholar] [CrossRef]
- Filippini, M.; Porcari, I.; Ruffolo, A.F.; Casiraghi, A.; Farinelli, M.; Uccella, S.; Franchi, M.; Candiani, M.; Salvatore, S. CO2-Laser therapy and Genitourinary Syndrome of Menopause: A Systematic Review and Meta-Analysis. J. Sex Med. 2022, 19, 452–470. [Google Scholar] [CrossRef]
- Quick, A.M.; Hundley, A.; Evans, C.; Stephens, J.A.; Ramaswamy, B.; Reinbolt, R.E.; Noonan, A.M.; Van Deusen, J.B.; Wesolowski, R.; Stover, D.G.; et al. Long-Term Follow-Up of Fractional CO2 Laser Therapy for Genitourinary Syndrome of Menopause in Breast Cancer Survivors. J. Clin. Med. 2022, 11, 774. [Google Scholar] [CrossRef]
- Salvatore, S.; Nappi, R.E.; Casiraghi, A.; Ruffolo, A.F.; Degliuomini, R.; Parma, M.; Maggiore, U.L.R.; Athanasiou, S.; Candiani, M. Microablative Fractional CO2 Laser for Vulvovaginal Atrophy in Women With a History of Breast Cancer: A Pilot Study at 4-week Follow-up. Clin. Breast Cancer 2021, 21, e539–e546. [Google Scholar] [CrossRef]
- Athanasiou, S.; Pitsouni, E.; Douskos, A.; Salvatore, S.; Loutradis, D.; Grigoriadis, T. Intravaginal energy-based devices and sexual health of female cancer survivors: A systematic review and meta-analysis. Lasers Med. Sci. 2020, 35, 1–11. [Google Scholar] [CrossRef]
- Gold, D.; Nicolay, L.; Avian, A.; Greimel, E.; Balic, M.; Pristauz-Telsnigg, G.; Tamussino, K.; Trutnovsky, G. Vaginal laser therapy versus hyaluronic acid suppositories for women with symptoms of urogenital atrophy after treatment for breast cancer: A randomized controlled trial. Maturitas 2023, 167, 1–7. [Google Scholar] [CrossRef]
- Mension, E.; Alonso, I.; Anglès-Acedo, S.; Ros, C.; Otero, J.; Villarino, Á.; Farré, R.; Saco, A.; Vega, N.; Castrejón, N.; et al. Effect of Fractional Carbon Dioxide vs Sham Laser on Sexual Function in Survivors of Breast Cancer Receiving Aromatase Inhibitors for Genitourinary Syndrome of Menopause: The LIGHT Randomized Clinical Trial. JAMA Netw. Open. 2023, 6, e2255697. [Google Scholar] [CrossRef]
- Pitsouni, E.; Grigoriadis, T.; Falagas, M.E.; Salvatore, S.; Athanasiou, S. Laser therapy for the genitourinary syndrome of menopause. A systematic review and meta-analysis. Maturitas 2017, 103, 78–88. [Google Scholar] [CrossRef]
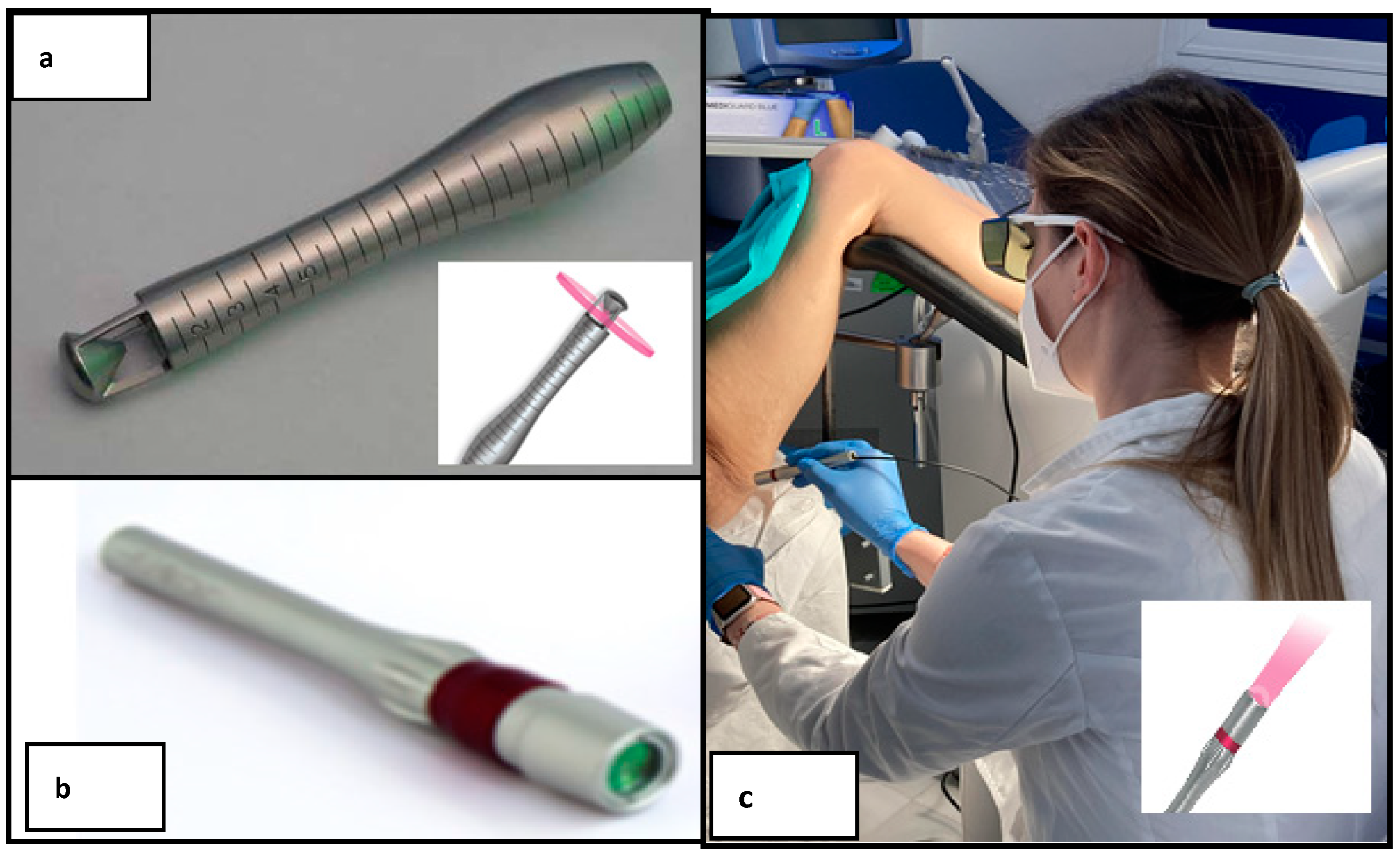
- Mendoza, N.; Quereda, F. Treatment of Female Sexual Dysfunction Due to Dyspareunia with Solid-State Vaginal Laser and Recombinant Platelet-Derived Epidermal Growth Factors: A Viable Possibility? Clin. Exp. Obstet. Gynecol. 2023, 50, 40. [Google Scholar] [CrossRef]
- Dodero, D.; Frascani, F.; Angelucci, M.; Bernabei, G.; Merlo, E.; Locatelli, F.; Murina, F. Solid State Vaginal Laser for the Treatment of Genitourinary Syndrome of Menopause: A Preliminary Report. Open J. Obstet. Gynecol. 2018, 8, 113–121. [Google Scholar] [CrossRef][Green Version]
- Dodero, D.; Frascani, F.; Angelucci, M.; Bernabei, G.; Merlo, E.; Locatelli, F.; Recalcati, D.; Murina, F. Histological Modifications of Postmenopausal Vaginal Mucosa after Regenerative Solid State Laser Treatment: A Multicenter Study. Int. J. Womens Health Wellness 2019, 5, 99. [Google Scholar] [CrossRef]
- Stabile, G.; Scalia, M.S.; Carlucci, S.; De Seta, F. Ladylift® non-ablative laser technology for the treatment of menopausal vestibulodynia and genitourinary syndrome. PrzMenopauzalny 2022, 21, 253–258. [Google Scholar] [CrossRef]
- Mension, E.; Alonso, I.; Tortajada, M.; Matas, I.; Gómez, S.; Ribera, L.; Ros, C.; Anglès-Acedo, S.; Castelo-Branco, C. Genitourinary Syndrome of Menopause Assessment Tools. J. Midlife Health 2021, 12, 99–102. [Google Scholar] [CrossRef]
- Veron, L.; Wehrer, D.; Annerose-Zéphir, G.; Suciu, V.; Delaloge, S.; Pistilli, B.; Chaltiel, D.; Pautier, P. Effects of local laser treatment on vulvovaginal atrophy among women with breast cancer: A prospective study with long-term follow-up. Breast Cancer Res. Treat. 2021, 188, 501–509. [Google Scholar] [CrossRef]
- Sturdee, D.W.; Panay, N. Recommendations for the management of postmenopausal vaginal atrophy. Climacteric 2010, 13, 509–522. [Google Scholar] [CrossRef]
- Balica, A.C.; Cooper, A.M.; McKevitt, M.K.; Schertz, K.; Wald-Spielman, D.; Egan, S.; Bachmann, G.A. Dyspareunia Related to GSM: Association of Total Vaginal Thickness via Transabdominal Ultrasound. J. Sex Med. 2019, 16, 2038–2042. [Google Scholar] [CrossRef]
- Athanasiou, S.; Pitsouni, E.; Antonopoulou, S.; Zacharakis, D.; Salvatore, S.; Falagas, M.E.; Grigoriadis, T. The effect of microablative fractional CO2 laser on vaginal flora of postmenopausal women. Climacteric 2016, 19, 512–518. [Google Scholar] [CrossRef]
- Sipos, A.G.; Pákozdy, K.; Jäger, S.; Larson, K.; Takacs, P.; Kozma, B. Fractional CO2 laser treatment effect on cervicovaginallavage zinc and copper levels: A prospective cohort study. BMC Womens Health 2021, 21, 235. [Google Scholar] [CrossRef]
| Characteristic | Participants, No. (%) 27 (100%) | |
|---|---|---|
| Age at enrollment, mean (SD), y | 57.17 (3.69) | |
| Age at menopause, mean (SD), y | 46.88 (3.98) | |
| Age at BC diagnosis, mean (SD), y | 45.78 (3.62) | |
| Time since BC diagnosis, mean (SD), y | 11.39 (3.31) | |
| Type of menopause | Natural | 6 (22.22) |
| Induced | 21 (77.77) | |
| Parity (have children) | 22 (81.40) | |
| Smokers | 2 (7.40) | |
| Education level | Elementary degree | 6 (13.3) |
| High school degree | 16 (59.25) | |
| College degree | 5 (18.51) | |
| Household income (EUR/month) | <600 | 0 (0) |
| 601–1200 | 4 (14.81) | |
| 1200–3600 | 19 (70.38) | |
| >3600 | 4 (14.81) | |
| Breast cancer stage | I | 13 (48.14) |
| II | 14 (51.86) | |
| Surgery | Conservative surgery | 17 (62.96) |
| Mastectomy | 10 (37.03) | |
| Breast reconstruction | Yes | 4 (4.81) |
| No | 6 (22.22) | |
| History of adjuvant therapy | Hormone therapy (IAs) | 27 (100) |
| Radiotherapy | 19 (70.37) | |
| Chemotherapy | 22 (82.48) |
| Outcome | Baseline (n = 27) | 10-Week Follow-Up (n = 27) | 24-Week Follow-Up (n = 24) | ||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Difference, Mean (SD) [95% CI] | p Value a | Difference, Mean (SD) [95% CI] | p Value a | |||
| Subjective outcomes | |||||||
| Dyspareunia (VAS) b | 7.5 (1.6) | 3.4 (2.4) | −4.1 (2.2) [−5.6 to −3.4] | <0.001 | 2.4 (2.4) | −5.2 (3.8) [−7.1 to −4.0] | <0.001 |
| Vaginal Health Index (VHI) c | 10.6 (3.3) | 17.1 (3.9) | 6.5 (3.6) [5.2 to 8.3] | <0.001 | 14.6 (3.6) | 4.2 (0.5) [3.1 to 5.2] | <0.001 |
| Vulvar Health Index (VuHI) d | 9.7 (3.1) | 3.9 (3.2) | −5.8(3.6) [−7.6 to −4.5] | <0.001 | 2.1(1.8) | −7.6 (3.5) [−8.6 to −3.7] | <0.001 |
| EORTC QLQ-BR23 e | 39.1 (8.4) | 37.8 (6.4) | −1.3 (4.5) [−7.7 to −0.8] | 0.29 | 43.3 (3.4) | 4.1 (4.2) [0.6 to 7.9] | <0.001 |
| FSFI f Lubrication g | 18.8 (5.1) | 21.05 (4.2) | 2.2 (0.7) [1.9 to 4.3] | 0.13 | 23.7 (6.2) | 5.2 (2.2) [4.3 to 9.1] | <0.001 |
| 2.7 (1.4) | 3.1 (1.5) | 0.4 (1.2) [0.5 to 1.9] | 0.19 | 4.3 (1.7) | 1.5 (1.1) [0.9 to 2.3] | <0.001 | |
| Objective outcomes | |||||||
| Vaginal pH | 6.5 (0.8) | 6.3 (1.0) | −0.2 (0.1) [−0.9 to −0.4] | <0.001 | 5.0 (2.1) | −1.3 (0.8) [−2.3 to −0.7] | <0.001 |
| Vaginal Maturation Index (VMI) h | 5.7 (9.2) | 17.2 (16.7) | 11.5 (3.23) [7.4 to 15.6] | <0.001 | 18.4 (17.5) | 12.5 (8.3) [8.2 to 17.4] | <0.001 |
| Measure | T1 a n = 27 | T2 b n = 27 | T3 c n = 27 | T4 d n = 27 | T5 e n = 27 | T6 f n = 24 | p Value |
|---|---|---|---|---|---|---|---|
| Vaginal burns (%) | 0 (0) | NA | NA | NA | 0 (0) | 0 (0) | >0.99 j |
| Vulvar burns (%) | 0 (0) | NA | NA | NA | 0 (0) | 0 (0) | >0.99 j |
| Vaginitis (%) | 0 (0) | NA | NA | NA | 1 (3.7) | 0 (0) | 0.32 j |
| Vaginal bleeding during laser application (%) | 19 (70.3) | 4(14.8) | 1(3.7) | 0 (0) | NA | NA | <0.001 j |
| Vaginal pain during laser application g (mean, SD) | 4.1 (2.4) | NA | NA | 2.2 (2.3) | NA | NA | <0.001 j |
| Vulvar pain during laser application g (mean, SD) | 3.8 (2.1) | NA | NA | 1.8 (0.9) | NA | NA | <0.001 j |
| Satisfaction with the treatment h (mean, SD) | NA | NA | NA | NA | 3.9 (1.4) | 4.7 (1.5) | <0.001 j |
| Satisfaction grade with the treatment i (n, %) | Not at all Satisfied | 1 (3.7) | 0 (0) | ||||
| Partly Satisfied | 1 (3.7) | 1 (4.1) | |||||
| Satisfied | 4 (14.8) | 5 (20.8) | |||||
| More than Satisfied | 9 (33.3) | 7 (29.1) | |||||
| Very Satisfied | 12 (44.4) | 11 (45.8) | 0.19 k | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lubián-López, D.M.; Butrón-Hinojo, C.A.; Menjón-Beltrán, S.; González-Mesa, E.; Tapiador-Albertos, S.; Rodríguez-Jiménez, B.; Fiol-Ruiz, G. Effects of Non-Ablative Solid-State Vaginal Laser (SSVL) for the Treatment of Vulvovaginal Atrophy in Breast Cancer Survivors after Adjuvant Aromatase Inhibitor Therapy: Preliminary Results. J. Clin. Med. 2023, 12, 5669. https://doi.org/10.3390/jcm12175669
Lubián-López DM, Butrón-Hinojo CA, Menjón-Beltrán S, González-Mesa E, Tapiador-Albertos S, Rodríguez-Jiménez B, Fiol-Ruiz G. Effects of Non-Ablative Solid-State Vaginal Laser (SSVL) for the Treatment of Vulvovaginal Atrophy in Breast Cancer Survivors after Adjuvant Aromatase Inhibitor Therapy: Preliminary Results. Journal of Clinical Medicine. 2023; 12(17):5669. https://doi.org/10.3390/jcm12175669
Chicago/Turabian StyleLubián-López, Daniel M., Carmen A. Butrón-Hinojo, Salomón Menjón-Beltrán, Ernesto González-Mesa, Silvia Tapiador-Albertos, Bibiana Rodríguez-Jiménez, and Gabriel Fiol-Ruiz. 2023. "Effects of Non-Ablative Solid-State Vaginal Laser (SSVL) for the Treatment of Vulvovaginal Atrophy in Breast Cancer Survivors after Adjuvant Aromatase Inhibitor Therapy: Preliminary Results" Journal of Clinical Medicine 12, no. 17: 5669. https://doi.org/10.3390/jcm12175669
APA StyleLubián-López, D. M., Butrón-Hinojo, C. A., Menjón-Beltrán, S., González-Mesa, E., Tapiador-Albertos, S., Rodríguez-Jiménez, B., & Fiol-Ruiz, G. (2023). Effects of Non-Ablative Solid-State Vaginal Laser (SSVL) for the Treatment of Vulvovaginal Atrophy in Breast Cancer Survivors after Adjuvant Aromatase Inhibitor Therapy: Preliminary Results. Journal of Clinical Medicine, 12(17), 5669. https://doi.org/10.3390/jcm12175669







