Sex Differences in Quality of Life in Patients with Ischemia with No Obstructive Coronary Artery Disease (INOCA): A Patient Self-Report Retrospective Survey from INOCA International
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Characteristics of the Respondents
3.2. Medical Evaluation of INOCA
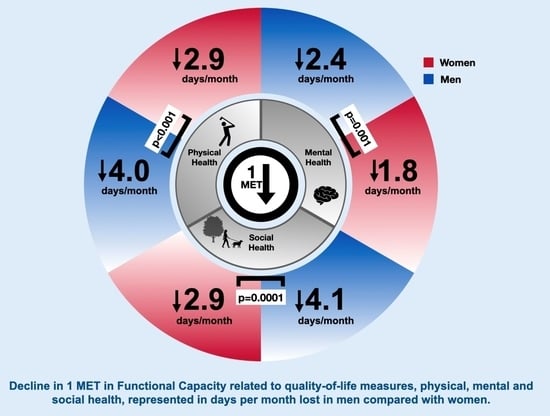
3.3. Quality of Life Measures
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Douglas, P.S.; Hoffmann, U.; Patel, M.R.; Mark, D.B.; Al-Khalidi, H.R.; Cavanaugh, B.; Cole, J.; Dolor, R.J.; Fordyce, C.B.; Huang, M.; et al. Outcomes of Anatomical versus Functional Testing for Coronary Artery Disease. N. Engl. J. Med. 2015, 372, 1291–1300. [Google Scholar] [CrossRef] [PubMed]
- Pepine, C.J.; Ferdinand, K.C.; Shaw, L.J.; Light-McGroary, K.A.; Shah, R.U.; Gulati, M.; Duvernoy, C.; Walsh, M.N.; Bairey Merz, C.N. Emergence of Nonobstructive Coronary Artery Disease. J. Am. Coll. Cardiol. 2015, 66, 1918–1933. [Google Scholar] [CrossRef]
- Maddox, T.M.; Stanislawski, M.A.; Grunwald, G.K.; Bradley, S.M.; Ho, P.M.; Tsai, T.T.; Patel, M.R.; Sandhu, A.; Valle, J.; Magid, D.J.; et al. Nonobstructive Coronary Artery Disease and Risk of Myocardial Infarction. JAMA 2014, 312, 1754. [Google Scholar] [CrossRef] [PubMed]
- Jespersen, L.; Hvelplund, A.; Abildstrom, S.Z.; Pedersen, F.; Galatius, S.; Madsen, J.K.; Jorgensen, E.; Kelbaek, H.; Prescott, E. Stable Angina Pectoris with No Obstructive Coronary Artery Disease Is Associated with Increased Risks of Major Adverse Cardiovascular Events. Eur. Heart J. 2012, 33, 734–744. [Google Scholar] [CrossRef]
- Bairey Merz, C.N.; Pepine, C.J.; Walsh, M.N.; Fleg, J.L.; Camici, P.G.; Chilian, W.M.; Clayton, J.A.; Cooper, L.S.; Crea, F.; Di Carli, M.; et al. Ischemia and No Obstructive Coronary Artery Disease (INOCA): Developing Evidence-Based Therapies and Research Agenda for the Next Decade. Circulation 2017, 135, 1075–1092. [Google Scholar] [CrossRef]
- Patel, M.R.; Peterson, E.D.; Dai, D.; Brennan, J.M.; Redberg, R.F.; Anderson, H.V.; Brindis, R.G.; Douglas, P.S. Low Diagnostic Yield of Elective Coronary Angiography. N. Engl. J. Med. 2010, 362, 886–895. [Google Scholar] [CrossRef]
- Johnson, B.D. Persistent Chest Pain Predicts Cardiovascular Events in Women without Obstructive Coronary Artery Disease: Results from the NIH-NHLBI-Sponsored Women’s Ischaemia Syndrome Evaluation (WISE) Study. Eur. Heart J. 2005, 27, 1408–1415. [Google Scholar] [CrossRef]
- Gulati, M.; Levy, P.D.; Mukherjee, D.; Amsterdam, E.; Bhatt, D.L.; Birtcher, K.K.; Blankstein, R.; Boyd, J.; Bullock-Palmer, R.P.; Conejo, T.; et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 144, e368–e454. [Google Scholar] [CrossRef]
- Ford, T.J.; Stanley, B.; Good, R.; Rocchiccioli, P.; McEntegart, M.; Watkins, S.; Eteiba, H.; Shaukat, A.; Lindsay, M.; Robertson, K.; et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina. J. Am. Coll. Cardiol. 2018, 72, 2841–2855. [Google Scholar] [CrossRef]
- Wei, J.; Mehta, P.K.; Johnson, B.D.; Samuels, B.; Kar, S.; Anderson, R.D.; Azarbal, B.; Petersen, J.; Sharaf, B.; Handberg, E.; et al. Safety of Coronary Reactivity Testing in Women With No Obstructive Coronary Artery Disease. JACC Cardiovasc. Interv. 2012, 5, 646–653. [Google Scholar] [CrossRef]
- Norris, C.M.; Spertus, J.A.; Jensen, L.; Johnson, J.; Hegadoren, K.M.; Ghali, W.A. Sex and Gender Discrepancies in Health-Related Quality of Life Outcomes Among Patients With Established Coronary Artery Disease. Circ. Cardiovasc. Qual. Outcomes 2008, 1, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Maas, A.H.E.M. Characteristic Symptoms in Women with Ischemic Heart Disease. Curr. Cardiovasc. Risk Rep. 2019, 13, 17. [Google Scholar] [CrossRef]
- Gulati, M.; Khan, N.; George, M.; Berry, C.; Chieffo, A.; Camici, P.G.; Crea, F.; Kaski, J.-C.; Marzilli, M.; Merz, C.N.B. Ischemia with No Obstructive Coronary Artery Disease (INOCA): A Patient Self-Report Quality of Life Survey from INOCA International. Int. J. Cardiol. 2023, 371, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Bairey Merz, C.N.; Olson, M.; McGorray, S.; Pakstis, D.L.; Zell, K.; Rickens, C.R.; Kelsey, S.F.; Bittner, V.; Sharaf, B.L.; Sopko, G. Physical Activity and Functional Capacity Measurement in Women: A Report from the NHLBI-Sponsored WISE Study. J. Womens Health Gend. Based Med. 2000, 9, 769–777. [Google Scholar] [CrossRef]
- Hlatky, M.A.; Boineau, R.E.; Higginbotham, M.B.; Lee, K.L.; Mark, D.B.; Califf, R.M.; Cobb, F.R.; Pryor, D.B. A Brief Self-Administered Questionnaire to Determine Functional Capacity (The Duke Activity Status Index). Am. J. Cardiol. 1989, 64, 651–654. [Google Scholar] [CrossRef]
- Gulati, M.; Black, H.R.; Shaw, L.J.; Arnsdorf, M.F.; Merz, C.N.B.; Lauer, M.S.; Marwick, T.H.; Pandey, D.K.; Wicklund, R.H.; Thisted, R.A. The Prognostic Value of a Nomogram for Exercise Capacity in Women. N. Engl. J. Med. 2005, 353, 468–475. [Google Scholar] [CrossRef]
- Morris, C.K.; Myers, J.; Froelicher, V.F.; Kawaguchi, T.; Ueshima, K.; Hideg, A. Nomogram Based on Metabolic Equivalents and Age for Assessing Aerobic Exercise Capacity in Men. J. Am. Coll. Cardiol. 1993, 22, 175–182. [Google Scholar] [CrossRef]
- Vanhees, L.; Fagard, R.; Thijs, L.; Staessen, J.; Amery, A. Prognostic Significance of Peak Exercise Capacity in Patients with Coronary Artery Disease. J. Am. Coll. Cardiol. 1994, 23, 358–363. [Google Scholar] [CrossRef]
- Hambrecht, R.; Wolf, A.; Gielen, S.; Linke, A.; Hofer, J.; Erbs, S.; Schoene, N.; Schuler, G. Effect of Exercise on Coronary Endothelial Function in Patients with Coronary Artery Disease. N. Engl. J. Med. 2000, 342, 454–460. [Google Scholar] [CrossRef]
- Shimokawa, H.; Suda, A.; Takahashi, J.; Berry, C.; Camici, P.G.; Crea, F.; Escaned, J.; Ford, T.; Yii, E.; Kaski, J.C.; et al. Clinical Characteristics and Prognosis of Patients with Microvascular Angina: An International and Prospective Cohort Study by the Coronary Vasomotor Disorders International Study (COVADIS) Group. Eur. Heart J. 2021, 42, 4592–4600. [Google Scholar] [CrossRef]
- Groepenhoff, F.; Eikendal, A.L.M.; Rittersma, Z.H.S.; Gijsberts, C.M.; Asselbergs, F.W.; Hoefer, I.E.; Pasterkamp, G.; Rutten, F.H.; Onland-Moret, N.C.; Den Ruijter, H.M. Persistent Symptoms and Health Needs of Women and Men With Non-Obstructed Coronary Arteries in the Years Following Coronary Angiography. Front. Cardiovasc. Med. 2021, 8, 670843. [Google Scholar] [CrossRef] [PubMed]
- Gulati, M.; Cooper-DeHoff, R.M.; McClure, C.; Johnson, B.D.; Shaw, L.J.; Handberg, E.M.; Zineh, I.; Kelsey, S.F.; Arnsdorf, M.F.; Black, H.R.; et al. Adverse Cardiovascular Outcomes in Women With Nonobstructive Coronary Artery Disease: A Report From the Women’s Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch. Intern. Med. 2009, 169, 843. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, H.R.; Picard, M.H.; Spertus, J.A.; Peteiro, J.; Lopez Sendon, J.L.; Senior, R.; El-Hajjar, M.C.; Celutkiene, J.; Shapiro, M.D.; Pellikka, P.A.; et al. Natural History of Patients With Ischemia and No Obstructive Coronary Artery Disease: The CIAO-ISCHEMIA Study. Circulation 2021, 144, 1008–1023. [Google Scholar] [CrossRef] [PubMed]
- Dreyer, R.P.; Dharmarajan, K.; Kennedy, K.F.; Jones, P.G.; Vaccarino, V.; Murugiah, K.; Nuti, S.V.; Smolderen, K.G.; Buchanan, D.M.; Spertus, J.A.; et al. Sex Differences in 1-Year All-Cause Rehospitalization in Patients After Acute Myocardial Infarction: A Prospective Observational Study. Circulation 2017, 135, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Van Der Meer, R.E.; Maas, A.H. The Role of Mental Stress in Ischaemia with No Obstructive Coronary Artery Disease and Coronary Vasomotor Disorders. Eur. Cardiol. Rev. 2021, 16, e37. [Google Scholar] [CrossRef]
- Mommersteeg, P.M.C.; Roeters Van Lennep, J.; Widdershoven, J. Cardiac Medication Use in Patients with Suspected Ischaemia without Obstructive Coronary Arteries: Sex Differences and Psychological Distress. Neth. Heart J. 2021, 29, 506–517. [Google Scholar] [CrossRef]
- Jansen, T.P.J.; Elias-Smale, S.E.; Van Den Oord, S.; Gehlmann, H.; Dimitiriu-Leen, A.; Maas, A.H.E.M.; Konst, R.E.; Van Royen, N.; Damman, P. Sex Differences in Coronary Function Test Results in Patient With Angina and Nonobstructive Disease. Front. Cardiovasc. Med. 2021, 8, 750071. [Google Scholar] [CrossRef]
- Reriani, M.; Flammer, A.J.; Duhé, J.; Li, J.; Gulati, R.; Rihal, C.S.; Lennon, R.; Tilford, J.M.; Prasad, A.; Lerman, L.O.; et al. Coronary Endothelial Function Testing May Improve Long-Term Quality of Life in Subjects with Microvascular Coronary Endothelial Dysfunction. Open Heart 2019, 6, e000870. [Google Scholar] [CrossRef]
- Kunadian, V.; Chieffo, A.; Camici, P.G.; Berry, C.; Escaned, J.; Maas, A.H.E.M.; Prescott, E.; Karam, N.; Appelman, Y.; Fraccaro, C.; et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. Eur. Heart J. 2020, 41, 3504–3520. [Google Scholar] [CrossRef]
| Men | Women | p-Value | |
|---|---|---|---|
| Total, N, % | 26 | 253 | |
| Overall Health After Symptom Onset | |||
| Excellent | 0 (0) | 6 (2.4) | 0.4336 |
| Very Good | 3 (11.5) | 42 (16.6) | 0.5636 |
| Good | 8 (30.8) | 75 (29.6) | 0.9303 |
| Fair | 11 (42.3) | 80 (31.6) | 0.4452 |
| Poor | 4 (15.4) | 50 (19.8) | 0.6539 |
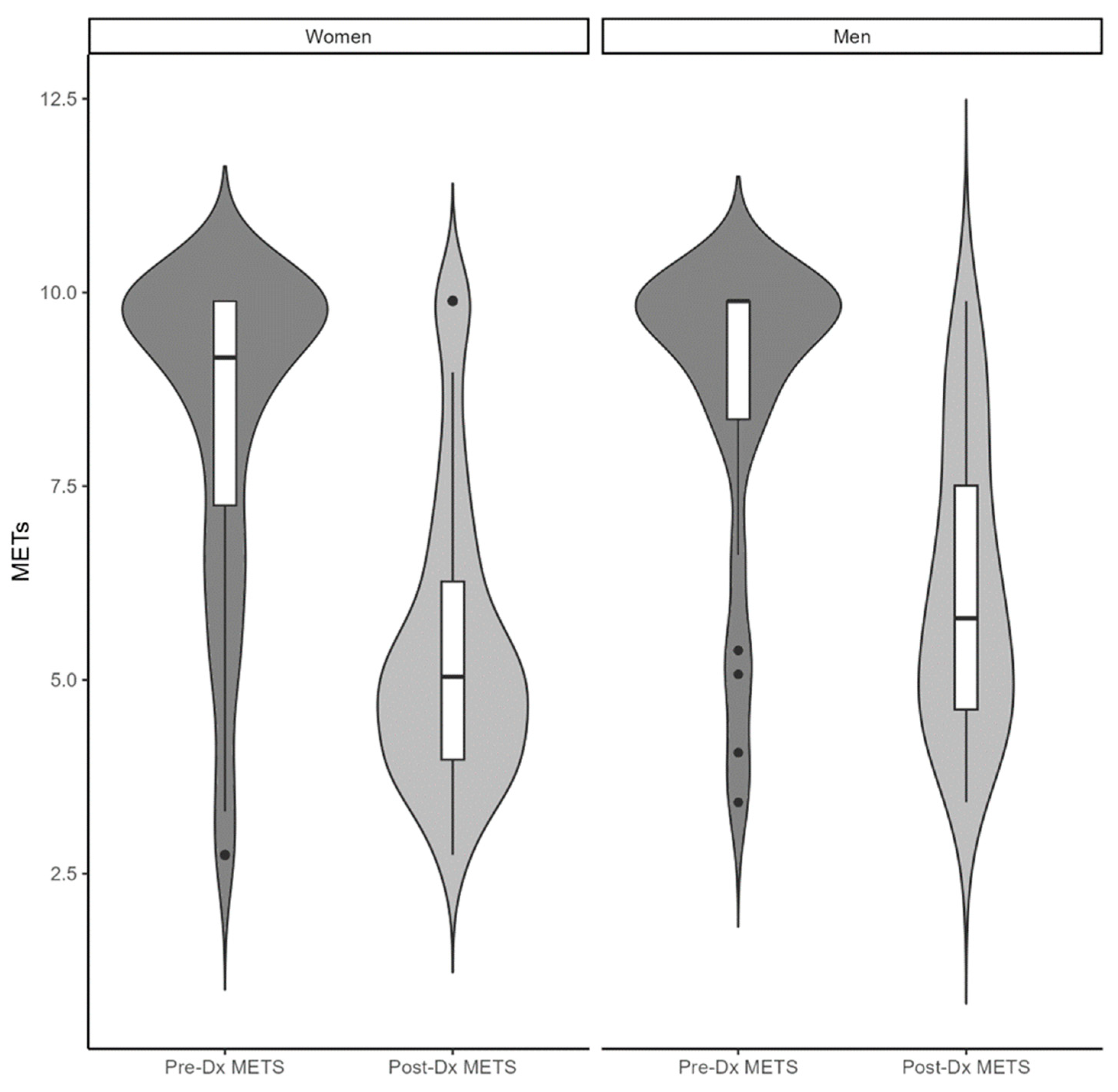
| Functional Capacity Level by DASI Score before onset of INOCA symptoms | |||
| <5 METs | 2 (7.7) | 23 (9.1) | 0.8273 |
| 5–8 METs | 3 (11.5) | 58 (22.9) | 0.2657 |
| >8 METs | 21 (80.8) | 172 (68.0) | 0.5779 |
| Estimated Exercise Capacity (METs) | 8.7 ± 2.0 | 8.6 ± 1.8 | 0.7857 |
| Functional Capacity Level by DASI Score after onset of INOCA symptoms | |||
| <5 METs | 9 (34.6) | 116 (45.8) | 0.4845 |
| 5–8 METs | 12 (46.2) | 110 (43.5) | 0.8710 |
| >8 METs | 5 (19.2) | 27 (10.7) | 0.2602 |
| Estimated Exercise Capacity (METs) | 6.1 ± 1.8 | 5.6 ± 1.8 | 0.1785 |
| Mental Health After Onset of Symptoms | |||
| INOCA adversely affected your Mental Health | 18 (69.2) | 191 (75.5) | 0.7876 |
| INOCA Negatively affected your outlook on life | 22 (84.6) | 185 (73.1) | 0.6328 |
| Social Health After Onset of Symptoms | |||
| INOCA Adversely affected home life | 21 (80.8) | 218 (86.2) | 0.8336 |
| INOCA adversely affected your relationship with partner/spouse | 14 (53.8) | 146 (57.7) | 0.8421 |
| INOCA adversely affected your social life | 21 (80.8) | 217 (85.8) | 0.8453 |
| INOCA Adversely affected your sex life | 15 (57.7) | 149 (58.9) | 0.9518 |
| Work and disability after onset of symptoms | |||
| INOCA Adversely affecting work life | 21 (80.8) | 184 (72.7) | 0.7345 |
| Reduced Work hours due to INOCA symptoms | 18 (69.2) | 148 (58.5) | 0.6028 |
| Retired early because of INOCA | 10 (38.5) | 130 (51.4) | 0.4540 |
| Changed job/roles for less stressful position due to INOCA symptoms | 7 (26.9) | 104 (41.1) | 0.3354 |
| Changed job/roles resulting in lower pay due to INOCA symptoms | 6 (23.1) | 90 (35.6) | 0.3539 |
| Applied for disability because of INOCA symptoms | 11 (42.3) | 103 (40.7) | 0.9191 |
| Successful Application for disability benefits | 9 (34.6) | 79 (31.2) | 0.8006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ranasinghe, S.; Merz, C.N.B.; Khan, N.; Wei, J.; George, M.; Berry, C.; Chieffo, A.; Camici, P.G.; Crea, F.; Kaski, J.C.; et al. Sex Differences in Quality of Life in Patients with Ischemia with No Obstructive Coronary Artery Disease (INOCA): A Patient Self-Report Retrospective Survey from INOCA International. J. Clin. Med. 2023, 12, 5646. https://doi.org/10.3390/jcm12175646
Ranasinghe S, Merz CNB, Khan N, Wei J, George M, Berry C, Chieffo A, Camici PG, Crea F, Kaski JC, et al. Sex Differences in Quality of Life in Patients with Ischemia with No Obstructive Coronary Artery Disease (INOCA): A Patient Self-Report Retrospective Survey from INOCA International. Journal of Clinical Medicine. 2023; 12(17):5646. https://doi.org/10.3390/jcm12175646
Chicago/Turabian StyleRanasinghe, Sachini, C. Noel Bairey Merz, Najah Khan, Janet Wei, Maria George, Colin Berry, Alaide Chieffo, Paolo G. Camici, Filippo Crea, Juan Carlos Kaski, and et al. 2023. "Sex Differences in Quality of Life in Patients with Ischemia with No Obstructive Coronary Artery Disease (INOCA): A Patient Self-Report Retrospective Survey from INOCA International" Journal of Clinical Medicine 12, no. 17: 5646. https://doi.org/10.3390/jcm12175646
APA StyleRanasinghe, S., Merz, C. N. B., Khan, N., Wei, J., George, M., Berry, C., Chieffo, A., Camici, P. G., Crea, F., Kaski, J. C., Marzilli, M., & Gulati, M. (2023). Sex Differences in Quality of Life in Patients with Ischemia with No Obstructive Coronary Artery Disease (INOCA): A Patient Self-Report Retrospective Survey from INOCA International. Journal of Clinical Medicine, 12(17), 5646. https://doi.org/10.3390/jcm12175646