Abstract
Combining systematic biopsy (SB) with targeted biopsy (TB) in the case of a positive result from multiparametric magnetic resonance imaging (mpMRI) is a matter of debate. The Prostate Imaging Reporting and Data System (PIRADS) score of 5 indicates the highest probability of clinically significant prostate cancer (csPC) detection in TB. Potentially, omitting SB in the case of PIRADS 5 may have a marginal impact on the csPC detection rate. The aim of this study was to determine whether SB can be avoided in the case of PIRADS 5 and to identify potential factors allowing for performing TB only. This cohort study involved n = 225 patients with PIRADS 5 on mpMRI (PIRADS 2.0/2.1) who underwent transperineal or transrectal combined biopsy (CB). CsPC was diagnosed in 51.6% (n = 116/225) of cases. TB and SB resulted in the detection of csPC in 48% (n = 108/225) and 20.4% (n = 46/225) of cases, respectively (TB vs. SB, p < 0.001). When the TB was positive, SB detected csPC in n = 38 of the cases (38/108 = 35%). SB added to TB significantly improved csPC detection in 6.9% of cases in absolute terms (n = 8/116) (TB vs. CB, p = 0.008). The multivariate regression model proved that the significant predictors of csPC detection via SB were the densities of the prostate-specific antigen—PSAD > 0.17 ng/mL2 (OR = 4.038, 95%CI: 1.568–10.398); primary biopsy setting (OR = 2.818, 95%CI: 1.334–5.952); and abnormal digital rectal examination (DRE) (OR = 2.746, 95%CI: 1.328–5.678). In a primary biopsy setting (n = 103), SB detected 10% (n = 6/60) of the additional cases of csPC (p = 0.031), while in a repeat biopsy setting (n = 122), SB detected 3.5% (n = 2/56) of the additional cases of csPC (p = 0.5). In the case of PSAD > 0.17 ng/mL2 (n = 151), SB detected 7.4% (n = 7/95) of additional cases of csPC (p = 0.016), while in the case of PSAD < 0.17 ng/mL2 (n = 74), SB detected 4.8% (n = 1/21) of the additional cases of csPC (p = 1.0). The omission of SB had an impact on the csPC diagnosis rate in patients with PIRADS 5 score lesions. Patients who have already undergone prostate biopsy and those with low PSAD are at a lower risk of missing csPC when SB is avoided. However, performing TB only may result in missing other csPC foci located outside the index lesion, which can alter treatment decisions.
1. Introduction
Prostate cancer is diagnosed in 1.1 million men annually [1]. Multiparametric magnetic resonance imaging (mpMRI) belongs nowadays to the mainstay diagnostic tools for its management. According to the recommendations of the European Association of Urology (EAU), every biopsy should be preceded by mpMRI [2]. The Prostate Imaging Reporting and Data System version 2 (PIRADS), developed and published in 2015, propelled its use and made its interpretation and reporting uniform [3]. The PIRADS score in current practice is used to stratify the risk before making a definitive decision about biopsy. According to a large Cochrane review, PIRADS scores 4 and 5 are highly suggestive of csPC (clinically significant prostate cancer, defined as International Society of Urological Pathology (ISUP) grade ≥2), with positive predictive values of 48% and 72%, respectively [4]. On the other hand, PIRADS scores 1–2 denote a negative mpMRI result and offer the potential avoidance of prostate biopsy [4].
A prostate biopsy can be performed with a transrectal or transperineal approach. The latest EUA guidelines recommend the transperineal approach over a transrectal approach because of its higher detection rate of csPC and lower infective complications [5]. The fusion of mpMRI and TRUS is the basis of targeted biopsy (TB). MpMRI fusion may be obtained cognitively, with software, or with direct in-bore guidance [6]. TB involves three to five targeted cores obtained from the suspicious area of the prostate gland [7]. The biopsy cores from the rest of the prostate gland are obtained via systematic biopsy (SB). SB involves at least 10 to 12 biopsy cores from both lobes, from apex to base, as far posterior and lateral as possible [8]. The main advantage of TB over SB is the higher detection of csPC and the lower detection of non-significant PC regardless of the biopsy approach (transrectal vs. transperineal) [9]. However, the EAU guidelines recommend a combined biopsy (CB), including TB and SB, in the case of positive mpMRI results [2]. The benefits of additive SB are still not clear. The arguments for CB include better tumor grading and compensation for targeting errors or PC lesions invisible in mpMRI. According to the EAU guidelines, TB may be performed without SB in a repeat biopsy setting [2]. SB alone is still recommended in the case of a negative PIRADS score (1–2) and a high suspicion of prostate cancer, such as when there is a high PSA/PSAD (prostate-specific antigen/density of prostate-specific antigen) or abnormal DRE (digital rectal examination) [4].
There is growing interest in diagnosing csPC with a low number of biopsy cores. Limiting the number of biopsy cores decreases pain, which is cumulative in nature [10]. Moreover, even in the setting of a transperineal biopsy, the number of biopsy cores has proven to influence infective complications [11]. As for the more obsolete transrectal biopsy, urinary tract infection and prostatitis are much more common in 18-core biopsy than in 12-core biopsy [12]. Decreasing the number of biopsy cores may also limit bleeding complications from the procedure, including bladder tamponade [13]. Interestingly, extensive biopsies may impact the course of radical prostatectomy and result in higher blood loss [14]. The omission of SB would significantly reduce the number of biopsy cores. On the other hand, SB may still contribute to the diagnosis of a non-negligible number of csPC cases, and omitting it may lead to misdiagnosis [9].
The aim of this study was to determine whether SB can be avoided in PIRADS 5 and to identify potential factors that would allow performing TB only. The outcomes of this study were the rates of csPC detection in SB, TB, and overall (CB = SB + TB).
2. Materials and Methods
2.1. Materials and MRI–Ultrasound Fusion Biopsy
This retrospective study involved 225 patients with PIRADS 5 on mpMRI (PIRADS 2.0/2.1, images from external radiological centers) who underwent transperineal or transrectal CB using the Trinity Koelis® navigation system (Koelis, Meylan, France) under local anesthesia. Biopsies involved at least three targeted cores from the mpMRI lesion and ten to twelve systematic cores from non-targeted areas. Procedures were performed under local anesthesia by a single experienced operator. If more than one lesion was present at mpMRI, the index lesion was defined as one having the highest PIRADS assessment category or as the largest lesion in the case of there being more than one within the same category. CsPC was defined as a Gleason score of 3 + 4 or higher (ISUP grade ≥2).
2.2. Statistical Analysis
Non-normally distributed continuous variables were reported as medians (Me) with the interquartile range (IQR) and compared using the Mann–Whitney U test. PSAD (density of prostate-specific antigen) was calculated using PSA divided by the MRI-derived prostate volume (ellipsoid method). The receiver operating characteristic (ROC) curves for diagnosis of csPC via PSAD were analyzed. Youde’s index (sensitivity + specificity-1) for identification of the optimum cut-off point for PSAD was used as a predictor of csPC detection. Categorical variables were reported as frequencies and proportions. Differences in rates were tested using the chi-squared test or McNemar test. Univariable and multivariable regression models were performed to evaluate predictors of csPC detection in SB and TB. Odds ratio (OR), 95% confidence interval (95%CI) of the odds ratio, and p values were recorded. A p value of <0.05 was considered significant. SPSS© software (SPSS statistics 25) was used for statistical analysis.
3. Results
We retrospectively analyzed the total number of n = 794 patients who underwent MRI ultrasound fusion biopsies of their prostate at the ECZ Hospital Otwock, Poland, between November 2016 and June 2021. Data were collected from medical patient records, which included the following: age, previous medical history, pre-biopsy PSA, PSAD, MRI report, biopsy procedure report, and pathology report.
3.1. Characteristics of the Group and Comparison of Clinical Data between the csPC Group and No-csPC Group
The total number of n = 225 men with a PIRADS score of 5 who underwent CB were included in this study. CB detected n = 116/225 (52%) cases of csPC. Patients with csPC significantly differed statistically from those without csPC in the following parameters: PSA level—10.5 ng/mL (6.0–15.0) vs. 7.6 ng/mL (5.0–11.1) (p < 0.001); PSAD—0.25 ng/mL2 (0.16–0.45) vs. 0.15 ng/mL2 (0.10–0.23) (p < 0.005); prostate volume—38.8 mL (31.6–49.5) vs. 48.0 mL (37.0–66.0) (p = 0.048); and abnormal DRE: n = 50/116 (43.1%) vs. normal DRE n = 23/109 (21.1%) (p < 0.05). There were no differences between the above groups in terms of age (p > 0.05); biopsy variant—transperineal vs. transrectal (p = 0.5); the zone location of the dominant lesion—peripheral vs. non-peripheral (p = 0.05); or biopsy history—primary vs. repeat (p = 0.07). The results are presented in Table 1. The AUC for diagnosis of csPC via PSAD was 0.704 (95%CI: 0.636–0.771, p < 0.001) (Figure 1). The highest Youden’s index was at a PSAD level of 0.17 ng/mL2. At this point, the diagnosis of csPC had 68% sensitivity and 61% specificity.

Table 1.
Descriptive characteristics. (csPC—clinically significant prostate cancer; PSA—prostate-specific antigen; PSAD—density of prostate-specific antigen; DRE—digital rectal examination; mpMRI—multiparametric magnetic resonance imaging; Me—median; IQR—interquartile range; n—number of cases).
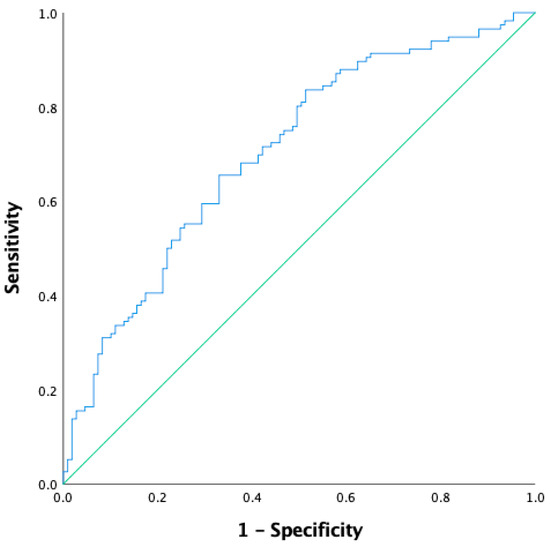
Figure 1.
The receiver operating characteristic (ROC) curve for diagnosis of clinically significant prostate cancer (csPC) via PSAD (density of prostate-specific antigen). AUC–0.704 (95%CI: 0.636–0.771), p < 0.001.
3.2. MRI Targeted Biopsy vs. Combined Biopsy
We analyzed the detection rate of csPC by the type of biopsy performed, i.e., TB, SB, or CB. csPC was detected via TB in 48.0% (n = 108/225) of cases, via SB in 20.4% (n = 46/225) of cases (SB vs. TB, p < 0.001), and via CB in 52.0% (n = 116/225) of cases. When TB was positive (n = 108), SB detected csPC in 35% of cases (n = 38/108). SB added to TB significantly improved csPC detection in the absolute number of 6.9% csPC cases (n = 8/116) (TB vs. CB, p = 0.008).
3.3. Clinical Factors Impacting the Detection of csPC in SB and TB
We analyzed which clinical factors impact the risk of csPC detection separately for SB and TB. For SB, the multivariate regression model proved that the following clinical parameters were significantly increasing the probability of csPC detection: PSAD > 0.17 ng/mL2 (OR = 4.038; 95%CI: 1.568–10.398) primary biopsy setting (OR = 2.818; 95%CI: 1.334–5.952), and abnormal DRE (OR = 2.746; 95%CI: 1.328–5.678). For TB, a multivariate regression model provided that the following clinical parameters were increasing the probability of csPC detection: PSAD > 0.17 ng/mL2 (OR = 3.759; 95%CI: 2.002–7.060) and abnormal DRE (OR = 2.911; 95%CI: 1.576–5.377). The biopsy-naive status was not a significant predictor of csPC detection in TB (OR = 1.388; 95%CI: 0.820–2.349). The results are presented in Table 2.

Table 2.
Univariate and multivariable analysis of the clinical factors predictive for clinically significant prostate cancer detection (csPC) using systematic biopsy (SB) and targeted biopsy (TB). PSA—prostate-specific antigen; PSAD—density of prostate-specific antigen; DRE—digital rectal examination; mpMRI—multiparametric magnetic resonance imaging; OR—odds ratio; CI—confidence interval; ref—reference.
3.4. Role of Clinical Factors: PSAD and Primary vs. Repeat Biopsy for csPC Detection in SB
Clinical parameters, primary vs. repeat biopsy and PSAD (low vs. high), were analyzed to assess the csPC detection rate in SB, TB, and CB and the risk of missing csPC when SB is omitted. The results are presented in Table 3.

Table 3.
Comparison of clinically significant prostate cancer (csPC) detection and missed rate between targeted biopsy (TB) alone, systematic biopsy (SB) alone, and combined biopsy (CB) in the whole cohort; in primary vs. repeat biopsy setting; and in low PSAD vs. high PSAD level. csPC—clinically significant prostate cancer; TB—targeted biopsy; SB—systematic biopsy; CB—combined biopsy; PSAD—density of prostate-specific antigen; n—number of cases.
3.4.1. Biopsy Setting—Primary vs. Repeat
In a cohort of biopsy-naive patients n = 103, csPC was diagnosed in 58.3% (n = 60/103) of the cases via CB. SB detected 30.0% (n = 31/103) of csPC cases, and TB detected 52.4% (n = 54/103) of csPC. SB added to TB significantly improved csPC detection in the absolute number of 10% (n = 6/60) of csPC cases (p = 0.031).
In a cohort of n = 122 patients with repeat biopsy, csPC was diagnosed in 45.9% (n = 56/122) of the cases via CB. SB detected 12.3% (n = 15/122) of csPC cases, and TB detected 44.3% (n = 54/122) of the csPC cases. SB added to TB improved csPC detection in the absolute number of 3.6% (n = 2/56) of the csPC cases (p = 0.5).
The detection of csPC via SB in the biopsy-naive cohort was significantly higher than in the cohort with repeat biopsy (30.0% vs. 12.3%; p = 0.001). Omitting SB in the primary biopsy is associated with a higher risk of missing csPC than in the cohort with previous biopsy (10% vs. 3.6%; p = 0.09).
3.4.2. Low PSAD (<0.17 ng/mL2) vs. High PSAD (>0.17 ng/mL2)
In a cohort of n = 74 patients with low PSAD (<0.17 ng/mL2), csPC was diagnosed in 28.4% (n = 21/74) of the cases via CB. SB detected 8.1% (n = 6/74) of csPC cases, and TB detected 27.0% (n = 20/74) of the csPC cases. SB added to TB improved csPC detection in the absolute number of 4.8% (n = 1/21) of csPC cases (p = 1.0).
In a cohort of n = 151 patients with high PSAD (>0.17 ng/mL2), csPC was diagnosed in 62.9% (n = 95/151) of the cases via CB. SB detected 26.5% (n = 40/151) of csPC cases, and TB detected 58.3% (n = 88/151) of the csPC cases. SB added to TB significantly improved csPC detection in the absolute number of 7.4% (n = 7/95) of csPC cases (p = 0.016).
The detection of csPC via SB in the cohort with high PSAD was significantly higher than in the cohort with low PSAD (26.5% vs. 8.1%; p < 0.001). Omitting SB in the cohort with high PSAD values is associated with a higher risk of missing csPC than in the cohort with low PSAD values (7.4% vs. 4.8%; p = 0.21).
4. Discussion
The main goal of our study was to assess whether omitting SB in PIRADS 5 lesions could impact the csPC detection rate. Our results confirmed that in PIRADS 5, TB has a significantly higher csPC detection rate compared to SB, 48% vs. 20%, respectively. We also confirmed that omitting SB may contribute to a significant reduction in the csPC detection rate by 6.9%. Our results are consistent with data from recent studies. Ahdoot et al. found that TB-only biopsy misses 5.8% of csPC [15]. In a Cochrane meta-analysis, the added value of SB in csPC detection in a biopsy-naive setting was 4.3% [9]. Similarly, in both the 4M trial and MRI-FIRST, the added value of systematic biopsy was estimated at a level of 5% [16,17]. Porpiglia et al. compared the detection rate of csPCa between TB alone and TB combined with SB. This non-inferiority designed study concluded that TB alone was not inferior to the fusion biopsy combined with SB for the detection of csPCa [18]. However, the above results apply to all mpMRI-positive men. The PIRADS 5 score is particularly associated with the highest probability of detecting csPC in TB. Recent studies have confirmed that in PIRADS 5, the risk of missing csPC with the TB-only approach may be even lower than in PIRADS 3 and 4 [19,20,21,22,23,24]. In a study by Nakanishi et al., TB only missed 4.6% of csPC in PIRADS 5 patients vs. 22% for the remaining men with PIRADS 3 and 4 scores [19]. Similarly, in another study by Gomez et al., SB improved csPC detection in PIRADS 3 and 4 patients by 26.3% and 9.5%, respectively, but there was no improvement in PIRADS 5 patients [20]. In the next study, Drobish et al. demonstrated that in PIRADS 5 patients, there would be no improvement in csPC detection when SB was omitted [21]. Additionally, in another study by Tafuri et al., only 4% of csPC was missed when omitting SB in PIRADS 5 patients [22].
The results from our study and those cited above indicate that concomitant SB has a marginal impact on csPC detection in PIRADS 5 patients. However, on the other hand, there are several arguments that advise against SB omission. First of all, we should take into consideration the limited sensitivity of mpMRI in detecting all csPC foci, as approximately 30% of csPC is invisible on mpMRI [25]. Moreover, prostate cancer is characterized by multifocal growth, which concerns about 20% of cases [26]. In the study by Checcucci et al., prostate cancer was detected via concomitant SB contralaterally to index lesions in 36% of csPC cases detected via TB [27]. It has also been proven that a higher PIRADS score increases the likelihood of csPC presence outside the index lesion [28]. In PIRADS 5 patients, csPC presence outside the index lesion can be seen in up to 60% of cases [29]. This relationship was also confirmed in our study, as SB detected csPC outside the index lesion in 35% of cases.
In addition to the PIRADS score, there are also other potential predictors of csPC detection via SB which are under investigation, such as PSA, PSAD, biopsy setting (primary vs. repeat), DRE status, lesion location, and prostate volume. However, any risk-adapted strategy or nomogram has already been proposed to avoid concomitant SB. In our study, we confirmed that the risk of csPC detection in SB is significantly lower in repeat biopsy than in primary biopsy by 12.3% vs. 30.0%, respectively. We found that SB added to TB in the primary biopsy significantly improved csPC detection in contrast to the repeat biopsy. The risk of missing csPC when SB is omitted is lower in repeat biopsy in comparison to primary biopsy by 3.5% vs. 10%, respectively. Our results reflect the data available in other publications. Extercate et al. detected only 1.3% of csPC cases via SB in repeat biopsies [30]. A Cochrane meta-analysis proved that the added value of SB in repeat biopsy is low, with estimates of 2.3% [9]. The above and our results are consistent with EAU recommendations, which state that SB may be omitted in repeat biopsy; however, it should be noted that the amount of evidence for this recommendation is weak [2].
In our work, we also confirmed that PSAD is another significant predictor increasing the detection rate of csPC in PIRADS 5 patients. We confirmed that a PSAD level of 0.17 ng/mL2 is optimal for detecting csPC. The results of our analysis are consistent with the available literature, which indicate that PSAD and PIRADS scores are complementary in the detection of csPC. In a clinical scenario, the PSAD value may influence the decision to perform a prostate biopsy [31]. For example, in non-suspicious mpMRI results, it is recommended to perform SB at high PSAD values (>0.15 ng/mL2) because the risk of csPC detection is significantly increased [32]. An analogous strategy is also adopted in patients with intermediate lesions, i.e., PIRADS 3, where CB should be performed in high PSAD [32]. Additionally, in PIRADS 4 and 5 patients, the impact of PSAD on the csPC detection rate has been demonstrated [33]. The results of our analysis confirmed that omitting SB at high PSAD values increases the risk of missing csPC from 4.7% to 7.4%. The absolute detection rate of csPC in SB was increased from 8.1% to 26.5% for the PSAD 0.17 ng/mL2 threshold. Recent publications based on a comparison of histopathology reports from a biopsy and radical prostatectomy indicate that high PSAD values are also associated with higher tumor volume and a higher probability of underestimating the Gleason score [34,35]. It should, therefore, be concluded that in high PSAD values, SB should not be omitted in PIRADS 5 lesions.
Our results confirmed that clinical data such as PSAD and biopsy settings are significant predictors of csPC detection via SB. However, in our study, we did not analyze the effects of omitting SB and clinical predictors on the underestimation of the Gleason score, and this is also a clinically relevant issue considering the justification for performing SB. Several recent studies indicate that SB may reduce the likelihood of Gleason score underestimation [36,37]. Moreover, taking cores from areas surrounding a suspicious lesion (focal systematic biopsy) can overlap sampling error and may provide a better estimation of the Gleason score [38]. Similarly, several technical issues of TB are also under investigation. For example, the number of targeted cores taken per lesion may impact csPC detection and Gleason score estimation [39]. In particular, obtaining three/four cores (current standard) from high-volume lesions, such as PIRADS 5, may not be sufficient to adequately estimate the Gleason score [40]. Moreover, mpMRI alone has a limited ability to predict local stage and extra-prostatic extension [41,42]. As a result, a TB-only approach may impact clinical decisions, such as qualification for local treatment or planning the extension of surgical intervention. For example, the presence of a PC outside index lesion should preclude focal treatment [43]. The local stage of prostate cancer also provides implications regarding neurovascular bundle sparing during radical prostatectomy [44]. It is also worth noting that the percentage of PC involvement in the systematic cores is an important prognostic factor, indicating the risk of biochemical progression or pelvic lymph node involvement [45,46]. In conclusion, the omission of SB may have a negative impact on adequate PC local staging and prognostic group determination.
Limitations
Our study was single-center and retrospective. We did not verify the histopathological report from the radical prostatectomy. The study population was heterogeneous, as it included both transperineal and transrectal biopsies. The analysis did not include epidemiological factors such as body mass index (BMI) or comorbidities. Recently, BMI was proven to correlate with the detection of high-grade prostate cancer in biopsies [47]. In this regard, comparing such factors with the potential omission of systematic biopsy would be very interesting. The mpMRI images were obtained from external radiological centers, and they were described by radiologists with different experiences; therefore, there may have been certain discrepancies in the assessment of the PIRADS scores. In our study, we did not analyze the effects of omitting SB on the underestimation of the Gleason score. Comparisons in patients with multiple MRI suspicious lesions were not available in this study. The comparisons of biopsy methods were performed per patient rather than per lesion.
5. Conclusions
The results of our study indicate that in PIRADS 5 lesions, the probability of detecting csPC in SB is significantly lower than in TB (20% vs. 48%, respectively). Omitting SB is also associated with the risk of missing csPC in 6.9% of cases. SB, however, contributed to the detection of distinct csPC foci in 35% of patients with csPC diagnosed simultaneously via TB. The omission of SB may impact local staging by failing to detect multifocal csPC and thus may affect therapeutic decisions. We also showed that significant predictive factors increasing the risk of csPC detection outside the index lesion via SB include high PSAD (>0.17 ng/mL2) and primary prostate biopsy. Our study suggests that SB might be omitted in patients with PIRADS 5 scores and low PSAD or secondary biopsy settings. However, further prospective studies, especially those correlating biopsy results with whole-mount radical prostatectomy specimens, are needed to set firm recommendations.
Author Contributions
Conceptualization, W.M. and T.M.; Methodology, W.M and T.M.; Validation, W.M., T.M. and S.S.; Formal Analysis, T.M.; Investigation, W.M. T.M., O.T., Ł.K. and P.K.; Resources, S.S.; Data Curation, S.S.; Writing—Original Draft Preparation, W.M., T.M., O.T. and Ł.K.; Writing—Review and Editing, W.M. and T.M.; Visualization, W.M and T.M.; Supervision, Ł.N. and P.K.; Project Administration, Ł.N. and P.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
All patients signed the informed consent that their medical data might be used in the future as part of a retrospective study. The analyzed datasets were anonymized before being used for the purposes of this current study. According to the Act of 6 September 2001 Pharmaceutical Law, this study qualified as a non-interventional observation study. Thus, this study did not require approval by an ethics committee or registration in the Central Register of Clinical Studies.
Data Availability Statement
The data analyzed in this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization International Agency for Research on Cancer (IARC). GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Homepage on the Internet. 2012. Available online: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx (accessed on 23 April 2016).
- EAU Guidelines: Edn. Presented at the EAU Annual Congress Amsterdam, 2022; EAU Guidelines Office: Arnhem, The Netherlands, 2022; ISBN 978-94-92671-16-51.
- Weinreb, J.C.; Barentsz, J.O.; Choyke, P.L.; Cornud, F.; Haider, M.A.; Macura, K.J.; Margolis, D.; Schnall, M.D.; Shtern, F.; Tempany, C.M.; et al. PI-RADS Prostate Imaging—Reporting and Data System: 2015, Version 2. Eur. Urol. 2016, 69, 16–40. [Google Scholar] [CrossRef] [PubMed]
- Panebianco, V.; Barchetti, G.; Simone, G.; Del Monte, M.; Ciardi, A.; Grompone, M.D.; Campa, R.; Indino, E.L.; Barchetti, F.; Sciarra, A.; et al. Negative Multiparametric Magnetic Resonance Imaging for Prostate Cancer: What’s Next? Eur. Urol. 2018, 74, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Tu, X.; Liu, Z.; Chang, T.; Qiu, S.; Xu, H.; Bao, Y.; Yang, L.; Wei, Q. Transperineal Magnetic Resonance Imaging–Targeted Biopsy May Perform Better Than Transrectal Route in the Detection of Clinically Significant Prostate Cancer: Systematic Review and Meta-analysis. Clin. Genitourin. Cancer 2019, 17, e860–e870. [Google Scholar] [CrossRef]
- Wegelin, O.; van Melick, H.H.; Hooft, L.; Bosch, J.R.; Reitsma, H.B.; Barentsz, J.O.; Somford, D.M. Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal Ultrasound fusion versus Cognitive Registration. Is There a Preferred Technique? Eur. Urol. 2017, 71, 517–531. [Google Scholar] [CrossRef]
- Kenigsberg, A.P.; Renson, A.; Rosenkrantz, A.B.; Huang, R.; Wysock, J.S.; Taneja, S.S.; Bjurlin, M.A. Optimizing the Number of Cores Targeted During Prostate Magnetic Resonance Imaging Fusion Target Biopsy. Eur. Urol. Oncol. 2018, 1, 418–425. [Google Scholar] [CrossRef]
- Donovan, J.; Hamdy, F.; Neal, D.; Peters, T.; Oliver, S.; Brindle, L.; Jewell, D.; Powell, P.; Gillatt, D.; Dedman, D.; et al. Prostate Testing for Cancer and Treatment (ProtecT) feasibility study. Health Technol. Assess 2003, 7, 1–88. [Google Scholar] [CrossRef]
- Drost, F.J.H.; Osses, D.F.; Nieboer, D.; Steyerberg, E.W.; Bangma, C.H.; Roobol, M.J.; Schoots, I.G. Prostate MRI with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Syst. Rev. 2019, 2019, CD012663. [Google Scholar] [CrossRef]
- Lee, D.J.; Mallin, K.; Graves, A.J.; Chang, S.S.; Penson, D.F.; Resnick, M.J.; Barocas, D.A. Recent Changes in Prostate Cancer Screening Practices and Epidemiology. J. Urol. 2017, 198, 1230–1240. [Google Scholar] [CrossRef] [PubMed]
- Kaver, I.; Mabjeesh, N.J.; Matzkin, H. Randomized prospective study of periprostatic local anesthesia during transrectal ultrasound-guided prostate biopsy. Urology 2002, 59, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.-F.; Luan, Y.; Lu, S.-M.; Zhou, G.-C.; Huang, T.-B.; Zhu, L.-Y.; Guo, C.-H. Risk factors for infection complications after transrectal ultrasound-guided transperineal prostate biopsy. World J. Urol. 2021, 39, 2463–2467. [Google Scholar] [CrossRef]
- Ghafoori, M.; Velayati, M.; Aliyari Ghasabeh, M.; Shakiba, M.; Alavi, M. Prostate Biopsy Using Transrectal Ultrasonography; The Optimal Number of Cores Regarding Cancer Detection Rate and Complications. Iran. J. Radiol. 2015, 12, e13257. [Google Scholar] [CrossRef]
- Carneiro, A.; Sivaraman, A.; Sanchez-Salas, R.; Nunes-Silva, I.; Baghdadi, M.; Srougi, V.; di Trapani, E.; Pizzaro, F.U.; Doizi, S.; Barret, E.; et al. Un mayor número de cilindros de biopsia transrectal de próstata guiada por ultrasonido se asocia con una mayor pérdida de sangre y complicaciones perioperatorias en la prostatectomía radical asistida por robot. Actas Urológicas Españolas 2017, 41, 155–161. [Google Scholar] [CrossRef]
- Ahdoot, M.; Wilbur, A.R.; Reese, S.E.; Lebastchi, A.H.; Mehralivand, S.; Gomella, P.T.; Bloom, J.; Gurram, S.; Siddiqui, M.; Pinsky, P.; et al. MRI-Targeted, Systematic, and Combined Biopsy for Prostate Cancer Diagnosis. N. Engl. J. Med. 2020, 382, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Wegelin, O.; Exterkate, L.; van der Leest, M.; Kummer, J.A.; Vreuls, W.; de Bruin, P.C.; Bosch, J.; Barentsz, J.O.; Somford, D.M.; van Melick, H.H. The FUTURE Trial: A Multicenter Randomised Controlled Trial on Target Biopsy Techniques Based on Magnetic Resonance Imaging in the Diagnosis of Prostate Cancer in Patients with Prior Negative Biopsies. Eur. Urol. 2019, 75, 582–590. [Google Scholar] [CrossRef]
- Rouvière, O.; Puech, P.; Renard-Penna, R.; Claudon, M.; Roy, C.; Mège-Lechevallier, F.; Decaussin-Petrucci, M.; Dubreuil-Chambardel, M.; Magaud, L.; Remontet, L.; et al. Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): A prospective, multicentre, paired diagnostic study. Lancet Oncol. 2019, 20, 100–109. [Google Scholar] [CrossRef]
- Porpiglia, F.; Checcucci, E.; De Cillis, S.; Piramide, F.; Amparore, D.; Piana, A.; Volpi, G.; Granato, S.; Zamengo, D.; Stura, I.; et al. A prospective randomized controlled trial comparing target prostate biopsy alone approach vs. target plus standard in naïve patients with positive mpMRI. Minerva Urol. Nephrol. 2023, 75, 31–41. [Google Scholar] [CrossRef]
- Nakanishi, Y.; Ito, M.; Fukushima, H.; Yokoyama, M.; Kataoka, M.; Ikuta, S.; Sakamoto, K.; Takemura, K.; Suzuki, H.; Tobisu, K.; et al. Who Can Avoid Systematic Biopsy Without Missing Clinically Significant Prostate Cancer in Men Who Undergo Magnetic Resonance Imaging-Targeted Biopsy? Clin. Genitourin. Cancer 2019, 17, e664–e671. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Gomez, E.; Sorribas, S.M.; Valero-Rosa, J.; Blanca, A.; Mesa, J.; Salguero, J.; Carrasco-Valiente, J.; López-Ruiz, D.; Anglada-Curado, F.J. Does Adding Standard Systematic Biopsy to Targeted Prostate Biopsy in PI-RADS 3 to 5 Lesions Enhance the Detection of Clinically Significant Prostate Cancer? Should All Patients with PI-RADS 3 Undergo Targeted Biopsy? Diagnostics 2021, 11, 1335. [Google Scholar] [CrossRef]
- Drobish, J.N.; Bevill, M.D.; Tracy, C.R.; Sexton, S.M.; Rajput, M.; Metz, C.M.; Gellhaus, P.T. Do patients with a PI-RADS 5 lesion identified on magnetic resonance imaging require systematic biopsy in addition to targeted biopsy? Urol. Oncol. Semin. Orig. Investig. 2021, 39, e1–e235. [Google Scholar] [CrossRef] [PubMed]
- Tafuri, A.; Iwata, A.; Shakir, A.; Iwata, T.; Gupta, C.; Sali, A.; Sugano, D.; Mahdi, A.S.; Cacciamani, G.E.; Kaneko, M.; et al. Systematic Biopsy of the Prostate can Be Omitted in Men with PI-RADSTM 5 and Prostate Specific Antigen Density Greater than 15%. J. Urol. 2021, 206, 289–297. [Google Scholar] [CrossRef]
- Arabi, A.; Deebajah, M.; Yaguchi, G.; Pantelic, M.; Williamson, S.; Gupta, N.; Park, H.; Peabody, J.; Menon, M.; Dabaja, A.; et al. Systematic Biopsy Does Not Contribute to Disease Upgrading in Patients Undergoing Targeted Biopsy for PI-RADS 5 Lesions Identified on Magnetic Resonance Imaging in the Course of Active Surveillance for Prostate Cancer. Urology 2019, 134, 168–172. [Google Scholar] [CrossRef]
- Cheng, X.; Xu, J.; Chen, Y.; Liu, Z.; Sun, G.; Yang, L.; Yao, J.; Zeng, H.; Song, B. Is Additional Systematic Biopsy Necessary in All Initial Prostate Biopsy Patients With Abnormal MRI? Front. Oncol. 2021, 11, 643051. [Google Scholar] [CrossRef]
- Johnson, D.C.; Raman, S.S.; Mirak, S.A.; Kwan, L.; Bajgiran, A.M.; Hsu, W.; Maehara, C.K.; Ahuja, P.; Faiena, I.; Pooli, A.; et al. Detection of Individual Prostate Cancer Foci via Multiparametric Magnetic Resonance Imaging. Eur. Urol. 2019, 75, 712–720. [Google Scholar] [CrossRef] [PubMed]
- Andreoiu, M.; Cheng, L. Multifocal prostate cancer: Biologic, prognostic, and therapeutic implications. Hum. Pathol. 2010, 41, 781–793. [Google Scholar] [CrossRef]
- Checcucci, E.; De Cillis, S.; Piramide, F.; Amparore, D.; Kasivisvanathan, V.; Giganti, F.; Fiori, C.; Moore, C.M.; Porpiglia, F. The role of additional standard biopsy in the MRI-targeted biopsy era. Minerva Urol. Nefrol. 2020, 72, 637–639. [Google Scholar] [CrossRef]
- Cash, H.; Maxeiner, A.; Stephan, C.; Fischer, T.; Durmus, T.; Holzmann, J.; Asbach, P.; Haas, M.; Hinz, S.; Neymeyer, J.; et al. The detection of significant prostate cancer is correlated with the Prostate Imaging Reporting and Data System (PI-RADS) in MRI/transrectal ultrasound fusion biopsy. World J. Urol. 2016, 34, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Stabile, A.; Dell’oglio, P.; De Cobelli, F.; Esposito, A.; Gandaglia, G.; Fossati, N.; Brembilla, G.; Cristel, G.; Cardone, G.; Deho’, F.; et al. Association Between Prostate Imaging Reporting and Data System (PI-RADS) Score for the Index Lesion and Multifocal, Clinically Significant Prostate Cancer. Eur. Urol. Oncol. 2018, 1, 29–36. [Google Scholar] [CrossRef]
- Exterkate, L.; Wegelin, O.; Barentsz, J.O.; van der Leest, M.G.; Kummer, J.A.; Vreuls, W.; de Bruin, P.C.; Bosch, J.R.; van Melick, H.H.; Somford, D.M. Is There Still a Need for Repeated Systematic Biopsies in Patients with Previous Negative Biopsies in the Era of Magnetic Resonance Imaging-targeted Biopsies of the Prostate? Eur. Urol. Oncol. 2020, 3, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Stevens, E.; Truong, M.; Bullen, J.A.; Ward, R.D.; Purysko, A.S.; Klein, E.A. Clinical utility of PSAD combined with PI-RADS category for the detection of clinically significant prostate cancer. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 846.e9–846.e16. [Google Scholar] [CrossRef]
- Zhang, Y.; Zeng, N.; Zhang, F.; Huang, Y.; Tian, Y. How to make clinical decisions to avoid unnecessary prostate screening in biopsy-naïve men with PI-RADs v2 score ≤ 3? Int. J. Clin. Oncol. 2020, 25, 175–186. [Google Scholar] [CrossRef]
- Girometti, R.; Giannarini, G.; Panebianco, V.; Maresca, S.; Cereser, L.; De Martino, M.; Pizzolitto, S.; Pecoraro, M.; Ficarra, V.; Zuiani, C.; et al. Comparison of different thresholds of PSA density for risk stratification of PI-RADSv2.1 categories on prostate MRI. BJR 2022, 95, 20210886. [Google Scholar]
- Magheli, A.; Hinz, S.; Hege, C.; Stephan, C.; Jung, K.; Miller, K.; Lein, M. Prostate Specific Antigen Density to Predict Prostate Cancer Upgrading in a Contemporary Radical Prostatectomy Series: A Single Center Experience. J. Urol. 2010, 183, 126–132. [Google Scholar] [CrossRef]
- Sfoungaristos, S.; Katafigiotis, I.; Perimenis, P. The role of PSA density to predict a pathological tumour upgrade between needle biopsy and radical prostatectomy for low risk clinical prostate cancer in the modified Gleason system era. Can. Urol. Assoc. J. 2013, 7, 722. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.; Yamany, T.; Mojtahed, A.; Hanna, N.; Nicaise, E.; Harisinghani, M.; Wu, C.-L.; Dahl, D.M.; Wszolek, M.; Blute, M.L.; et al. Combination MRI-targeted and systematic prostate biopsy may overestimate gleason grade on final surgical pathology and impact risk stratification. Urol. Oncol. Semin. Orig. Investig. 2022, 40, e1–e59. [Google Scholar]
- Mischinger, J.; Schöllnast, H.; Zurl, H.; Geyer, M.; Fischereder, K.; Adelsmayr, G.; Igrec, J.; Fritz, G.; Merdzo-Hörmann, M.; Elstner, J.; et al. Combining targeted and systematic prostate biopsy improves prostate cancer detection and correlation with the whole mount histopathology in biopsy naïve and previous negative biopsy patients. Front. Surg. 2022, 9, 1013389. [Google Scholar]
- Chung, J.H.; Park, B.K.; Song, W.; Kang, M.; Sung, H.H.; Jeon, H.G.; Jeong, B.C.; Seo, S.I.; Jeon, S.S.; Lee, H.M. TRUS-Guided Target Biopsy for a PI-RADS 3–5 Index Lesion to Reduce Gleason Score Underestimation: A Propensity Score Matching Analysis. Front. Oncol. 2022, 11, 824204. [Google Scholar] [PubMed]
- Cata, E.; Andras, I.; Ferro, M.; Kadula, P.; Leucuta, D.; Musi, G.; Matei, D.-V.; De Cobelli, O.; Tamas-Szora, A.; Caraiani, C.; et al. Systematic sampling during MRI-US fusion prostate biopsy can overcome errors of targeting—Prospective single center experience after 300 cases in first biopsy setting. Transl. Androl. Urol. 2020, 9, 2510–2518. [Google Scholar] [CrossRef] [PubMed]
- Hansen, N.L.; Barrett, T.; Lloyd, T.; Warren, A.; Samel, C.; Bratt, O.; Kastner, C. Optimising the number of cores for magnetic resonance imaging—Guided targeted and systematic transperineal prostate biopsy. BJU Int. 2020, 125, 260–269. [Google Scholar] [CrossRef]
- Pooli, A.; Johnson, D.C.; Shirk, J.; Markovic, D.; Sadun, T.Y.; Sisk, A.E.J.; Bajgiran, A.M.; Mirak, S.A.; Felker, E.R.; Hughes, A.K.; et al. Predicting Pathological Tumor Size in Prostate Cancer Based on Multiparametric Prostate Magnetic Resonance Imaging and Preoperative Findings. J. Urol. 2021, 205, 444–451. [Google Scholar]
- Triquell, M.; Regis, L.; Winkler, M.; Valdés, N.; Cuadras, M.; Celma, A.; Planas, J.; Morote, J.; Trilla, E. Multiparametric MRI for Staging of Prostate Cancer: A Multicentric Analysis of Predictive Factors to Improve Identification of Extracapsular Extension before Radical Prostatectomy. Cancers 2022, 14, 3966. [Google Scholar] [CrossRef]
- Lee, A.Y.; Chen, K.; Tan, Y.G.; Lee, H.J.; Shutchaidat, V.; Fook-Chong, S.; Cheng, C.W.; Ho, H.S.; Yuen, J.S.; Ngo, N.T.; et al. Reducing the number of systematic biopsy cores in the era of MRI targeted biopsy—Implications on clinically-significant prostate cancer detection and relevance to focal therapy planning. Prostate Cancer Prostatic Dis. 2022, 25, 720–726. [Google Scholar] [PubMed]
- Zapała, P.; Dybowski, B.; Bres-Niewada, E.; Lorenc, T.; Powała, A.; Lewandowski, Z.; Gołębiowski, M.; Radziszewski, P. Predicting side-specific prostate cancer extracapsular extension: A simple decision rule of PSA biopsy, and MRI parameters. Int. Urol. Nephrol. 2019, 51, 1545–1552. [Google Scholar] [PubMed]
- Gandaglia, G.; Ploussard, G.; Valerio, M.; Marra, G.; Moschini, M.; Martini, A.; Roumiguié, M.; Fossati, N.; Stabile, A.; Beauval, J.-B.; et al. Prognostic Implications of Multiparametric Magnetic Resonance Imaging and Concomitant Systematic Biopsy in Predicting Biochemical Recurrence after Radical Prostatectomy in Prostate Cancer Patients Diagnosed with Magnetic Resonance Imaging-Targeted Biopsy. Eur. Urol. Oncol. 2020, 3, 739–747. [Google Scholar] [PubMed]
- Gandaglia, G.; Martini, A.; Ploussard, G.; Fossati, N.; Stabile, A.; De Visschere, P.; Borgmann, H.; Heidegger, I.; Steinkohl, F.; Kretschmer, A.; et al. External Validation of the 2019 Briganti Nomogram for the Identification of Prostate Cancer Patients Who Should Be Considered for an Extended Pelvic Lymph Node Dissection. Eur. Urol. 2020, 78, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Baio, R.; Napodano, G.; Caruana, C.; Molisso, G.; Di Mauro, U.; Intilla, O.; Pane, U.; D’Angelo, C.; Francavilla, A.B.; Guarnaccia, C.; et al. Association between obesity and frequency of high-grade prostate cancer on biopsy in men: A single-center retrospective study. Mol. Clin. Oncol. 2022, 17, 127. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).