Completion of the Emergency Department “Big 6” in Patients with an Acute Hip Fracture Is Associated with a Lower Mortality Risk and Shorter Length of Hospital Stay
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Outcomes
2.3. Statistical Anlysis
3. Results
3.1. Rate of Completion of the Big 6
3.2. Mortality
3.3. Length of Stay
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Welford, P.; Jones, C.S.; Davies, G.; Kunutsor, S.K.; Costa, M.L.; Sayers, A.; Whitehouse, M.R. The association between surgical fixation of hip fractures within 24 hours and mortality: A systematic review and meta-analysis. Bone Jt. J. 2021, 103, 1176–1186. [Google Scholar] [CrossRef] [PubMed]
- Moja, L.; Piatti, A.; Pecoraro, V.; Ricci, C.; Virgili, G.; Salanti, G.; Germagnoli, L.; Liberati, A.; Banfi, G. Timing Matters in Hip Fracture Surgery: Patients Operated within 48 Hours Have Better Outcomes. A Meta-Analysis and Meta-Regression of over 190,000 Patients. PLoS ONE 2012, 7, e46175. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, R.; Babu, S.; Dixon, P.; Freeman, N.; Hurford, D.; Kelleher, E.; Moppett, I.; Ray, D.; Sahota, O.; Shields, M.; et al. Guideline for the management of hip fractures 2020: Guideline by the Association of Anaesthetists. Anaesthesia 2021, 76, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Tewari, P.; Sweeney, B.F.; Lemos, J.L.; Shapiro, L.; Gardner, M.J.; Morris, A.M.; Baker, C.B.; Harris, A.S.; Kamal, R.N. Evaluation of Systemwide Improvement Programs to Optimize Time to Surgery for Patients with Hip Fractures: A Systematic Review. JAMA Network Open. 2022, 5, e2231911. [Google Scholar] [CrossRef] [PubMed]
- Full Guideline|Hip Fracture: Management|Guidance|NICE. Available online: https://www.nice.org.uk/guidance/cg124/resources/cg124-hip-fracture-full-guideline (accessed on 3 January 2023).
- The Scottish Hip Fracture Audit. Available online: https://www.shfa.scot.nhs.uk/index.htm (accessed on 8 May 2023).
- Scottish Government. Scottish Standards of Care for Hip Fracture Patients. Available online: https://www.shfa.scot.nhs.uk/_docs/2020/Scottish-standards-of-care-for-hip-fracture-patients-2020.pdf (accessed on 23 August 2023).
- Alderwick, H. Is the NHS overwhelmed? BMJ 2022, 376, o51. [Google Scholar] [CrossRef] [PubMed]
- Scottish Hip Fracture Audit 2022 Dashboard—Scottish Hip Fracture Audit—Reporting on 2021—Publications—Public Health Scotland. Available online: https://publichealthscotland.scot/publications/scottish-hip-fracture-audit/scottish-hip-fracture-audit-reporting-on-2021/scottish-hip-fracture-audit-2022-dashboard/ (accessed on 25 April 2023).
- Riemen, A.H.K.; Hutchison, J.D. The multidisciplinary management of hip fractures in older patients. Orthop. Trauma 2016, 30, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Scottish Index of Multiple Deprivation 2020—gov.scot. Available online: https://www.gov.scot/collections/scottish-index-of-multiple-deprivation-2020/ (accessed on 30 March 2022).
- Borges, F.K.; Bhandari, M.; Guerra-Farfan, E.; Patel, A.; Sigamani, A.; Umer, M.; Tiboni, M.E.; Viller-Casares, M.D.M.; Tandon, V.; Tomas-Hernandez, J.; et al. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): An international, randomised, controlled trial. Lancet 2020, 395, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.J.; Clement, N.D.; Abdul-Jabar, H.; Abu-Rajab, R.; Abugarja, A.; Adam, K.; Hernandez, H.J.A.; Lazcano, G.A.; Anderson, S.; Ansar, M.; et al. IMPACT-Global Hip Fracture Audit: Nosocomial infection, risk prediction and prognostication, minimum reporting standards and global collaborative audit: Lessons from an international multicentre study of 7090 patients conducted in 14 nations during the C. Surgery 2022, 20, e429–e446. [Google Scholar]
- Hall, A.J.; Clement, N.D.; Maclullich, A.M.J.; White, T.O.; Duckworth, A.D. IMPACT-Scot 2 report on COVID-19 in hip fracture patients. Bone Joint J. 2021, 103, 888–897. [Google Scholar] [CrossRef] [PubMed]
- Sen-Crowe, B.; Sutherland, M.; McKenney, M.; Elkbuli, A. A Closer Look into Global Hospital Beds Capacity and Resource Shortages During the COVID-19 Pandemic. J. Surg. Res. 2021, 260, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.J.; Clement, N.D.; MacLullich, A.M.J.; Ojeda-Thies, C.; Hoefer, C.; Brent, L.; White, T.O.; Duckworth, A.D. IMPACT of COVID-19 on hip fracture services: A global survey by the International Multicentre Project Auditing COVID-19 in Trauma & Orthopaedics. Surgeon 2022, 20, 237–240. [Google Scholar] [PubMed]
- Porter, S.B.; Pla, R.; Chow, J.H.; Keneally, R.; Douglas, R.; Desvarieux, T.; Crowe, M.M.; Mazzeffi, M.A. Preoperative Pressure Ulcers, Mortality, and Complications in Older Hip Fracture Surgery Patients. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2022, 6. [Google Scholar] [CrossRef] [PubMed]
- Zeelenberg, M.L.; Den Hartog, D.; Panneman, M.J.M.; Polinder, S.; Verhofstad, M.H.J.; Van Lieshout, E.M.M. Trends in incidence, health care consumption, and costs for proximal femoral fractures in the Netherlands between 2000 and 2019: A nationwide study. Osteoporos. Int. 2023, 1, 1–11. [Google Scholar]
- Ward, K.; Scottish Hip Fracture Audit, NHS National Services Scotland, UK. Personal communication, 2021.
- Bano, G.; Dianin, M.; Biz, C.; Bedogni, M.; Alessi, A.; Bordignon, A.; Bizzotto, M.; Birizzi, A.; Ruggieri, P.; Manzato, E.; et al. Efficacy of an interdisciplinary pathway in a first level trauma center orthopaedic unit: A prospective study of a cohort of elderly patients with hip fractures. Arch. Gerontol. Geriatr. 2020, 86, 103957. [Google Scholar] [CrossRef] [PubMed]
- Kay, R.S.; Hughes, M.; Williamson, T.R.; Hall, A.J.; Duckworth, A.D.; Clement, N.D. The Clinical Frailty Scale can be used retrospectively to assess the frailty of patients with hip fracture: A validation study. Eur. Geriatr. Med. 2022, 13, 1101–1107. [Google Scholar] [CrossRef] [PubMed]
| Component of the Big 6 | Completed in ED (n, %) | |
|---|---|---|
| Yes | No | |
| Pain relief | 3282 (90.8) | 331 (9.2) |
| Delirium | 2183 (60.4) | 1430 (39.6) |
| NEWS | 3235 (89.5) | 378 (10.5) |
| Bloods/ECG | 3201 (88.6) | 412 (11.4) |
| IV Fluids | 2560 (70.9) | 1053 (29.1) |
| Pressure Areas | 2080 (57.6) | 1533 (42.4) |
| Demographic | Descriptive | Completion of the “Big 6” | Difference/ Odds Ratio (95% CI) | p-Value | |
|---|---|---|---|---|---|
| No (n = 2433) | Yes (n = 1180) | ||||
| Sex (n, % of group) | Male | 737 (30.3) | 312 (26.4) | Reference | |
| Female | 1696 (69.7) | 868 (73.6) | 1.21 (1.04 to 1.41) | 0.017 * | |
| Age (years: mean, SD) | 80.8 (10.2) | 81.2 (9.9) | 0.4 (0.4 to 1.1) | 0.328 ** | |
| SIMD (n, % of group) | 1 (Most deprived) | 276 (11.3) | 129 (10.9) | 0.345 * | |
| 2 | 543 (22.3) | 284 (24.1) | |||
| 3 | 374 (15.4) | 189 (16.0) | |||
| 4 | 402 (16.5) | 211 (17.9) | |||
| 5 (Least) | 835 (34.3) | 366 (31) | |||
| Missing | 3 | 1 | |||
| ASA Grade (n, % of group) | 1 | 46 (1.9) | 22 (1.9) | 0.87 (0.52 to 1.47) | 0.532 * |
| 2 | 476 (19.6) | 313 (26.5) | 1.20 (1.01 to1.43) | 0.034 * | |
| 3 | 1237 (50.8) | 676 (57.3) | Reference | ||
| 4 | 191 (7.9) | 96 (8.1) | 0.92 (0.71 to 1.20) | 0.532 * | |
| Missing | 483 (19.9) | 73 (6.2) | |||
| Fracture Management (n, % of group) | DHS | 684 (28.1) | 351 (29.7) | 0.076 * | |
| Hemiarthroplasty | 1088 (44.7) | 545 (46.2) | |||
| IM Nail | 293 (12.0) | 141 (11.9) | |||
| Cannulated screw | 141 (5.8) | 55 (4.7) | |||
| THA | 171 (7) | 79 (6.7) | |||
| Other | 56 (2.3) | 12 (1) | |||
| Time in ED (hours: mean, SD) | 4.7 (3.0) | 4.7 (3.0) | 0.1 (−0.1 to 0.3) | 0.568 ** | |
| Time to Theatre (hours: mean, SD) | 29.2 (22.1) | 26.8 (18.4) | 2.4 (0.9 to 3.8) | 0.002 ** | |
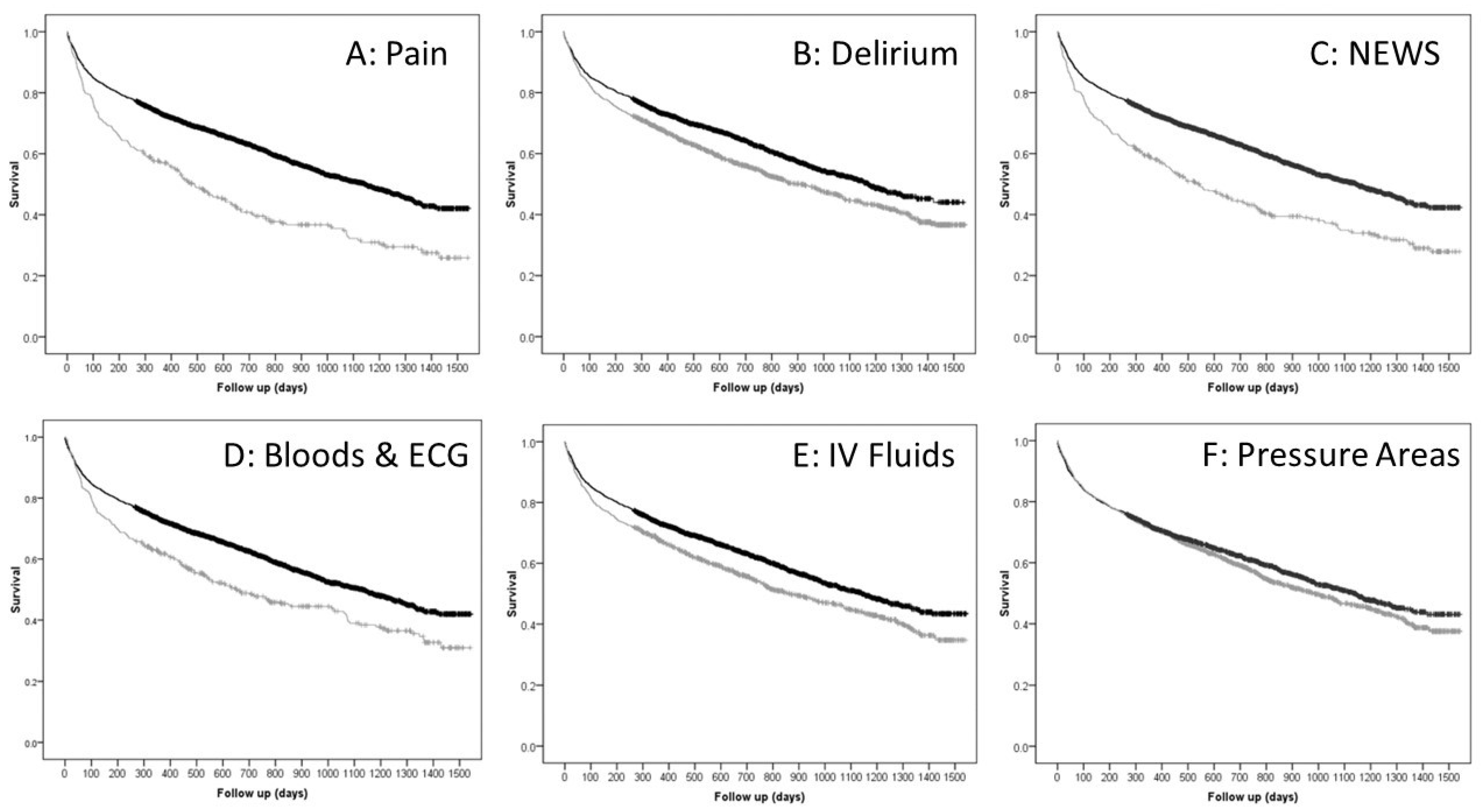
| Component of the “Big 6” | Completed in ED | Percentage Suvival (95% confidence interval) | ||||
|---|---|---|---|---|---|---|
| N (%) | 30 Days | 90 Days | 1 Year | Final | ||
| Pain Relief | Yes | 3282 (90.8) | 93.6 (+/−0.8) | 85.9 (+/−1.2) | 72.9 (+/−1.6) | 42.9 (+/−2.7) |
| No | 331 (9.2) | 91.5 (+/−3.1) | 78.9 (+/−4.3) | 57.0 (+/−5.3) | 25.9 (+/−6.5) | |
| p-value * | 0.148 | <0.001 | <0.001 | <0.001 | ||
| Delirium (4AT) | Yes | 2183 (60.4) | 93.9 (+/−1.0) | 86.2 (+/−1.4) | 73.6 (+/−1.8) | 44.0 (+/−4.1) |
| No | 1430 (39.6) | 92.7 (+/−1.4) | 83.6 (+/−2.0) | 68.1 (+/−2.4) | 36.6 (+/−3.5) | |
| p-value * | 0.215 | 0.033 | <0.001 | <0.001 | ||
| NEWS | Yes | 3235 (89.5) | 93.8 (+/−0.8) | 85.9 (+/−1.2) | 73.0 (+/−1.6) | 42.3 (+/−2.9) |
| No | 378 (10.5) | 90.5 (+/−2.9) | 79.6 (+/−4.1) | 58.3 (+/−4.9) | 27.9 (+/−5.9) | |
| p-value * | 0.013 | 0.001 | <0.001 | <0.001 | ||
| Bloods and ECG | Yes | 3201 (88.6) | 93.3 (+/−7.8) | 85.7 (+/−1.2) | 72.7 (+/−1.6) | 41.9 (+/−2.9) |
| No | 412 (11.4) | 93.9 (+/−2.4) | 81.8 (+/−3.7) | 61.7 (+/−4.7) | 30.9 (+/−6.9) | |
| p-value * | 0.650 | 0.041 | <0.001 | <0.001 | ||
| IV Fluids | Yes | 2560 (70.9) | 93.7 (+/−1.0) | 86.1 (+/−1.4) | 73.1 (+/−1.8) | 43.4 (+/−3.1) |
| No | 1053 (29.1) | 92.5 (+/−1.6) | 83.0 (+/−2.4) | 67.5 (+/−2.7) | 34.7 (+/−4.5) | |
| p-value * | 0.184 | 0.014 | 0.001 | <0.001 | ||
| Pressure Areas | Yes | 2080 (57.6) | 93.1 (+/−1.2) | 85.0 (+/−1.6) | 71.4 (+/−2.0) | 43.1 (+/−3.5) |
| No | 1533 (42.4) | 93.9 (+/−1.2) | 85.5 (+/−1.8) | 71.6 (+/−2.4) | 37.6 (+/−3.9) | |
| p-value * | 0.363 | 0.623 | 0.906 | 0.105 | ||
| Demographic | Descriptive | Alive (n = 2013) | Deceased (n = 1600) | Difference/ Odds Ratio (95% CI) | p-Value |
|---|---|---|---|---|---|
| Sex (n, % of group) | Male | 511 (25.4) | 538 (33.6) | Reference | |
| Female | 1502 (74.6) | 1062 (66.4) | 0.67 (0.58 to 0.78) | <0.001 * | |
| Age (years: mean, SD) | 78.3 (10.5) | 84.2 (8.6) | 6.0 (5.3 to 6.6) | <0.001 * | |
| SIMD (n, % of group) | 1 (Most) | 234 (11.6) | 171 (10.7) | 0.097 * | |
| 2 | 466 (23.1) | 361 (22.6) | |||
| 3 | 340 (16.9) | 224 (14) | |||
| 4 | 326 (16.2) | 287 (17.9) | |||
| 5 (Least) | 645 (32) | 556 (34.8) | |||
| Missing | 2 (0.1) | 1 (0.1) | |||
| ASA Grade (n, % of group) | 1 | 62 (3.1) | 6 (0.4) | <0.001 * | |
| 2 | 642 (31.9) | 147 (9.2) | |||
| 3 | 1014 (50.4) | 899 (56.2) | |||
| 4 | 84 (4.2) | 203 (12.7) | |||
| Missing | 211 (10.5) | 345 (21.6) | |||
| Fracture Management (n, % of group) | DHS | 541 (26.9) | 494 (30.9) | <0.001 * | |
| Hemiarthroplasty | 868 (43.1) | 762 (47.6) | |||
| IM Nail | 227 (11.3) | 207 (12.9) | |||
| Cannulated screw | 134 (6.7) | 62 (3.9) | |||
| THA | 234 (11.6) | 16 (1) | |||
| Other | 9 (0.4) | 59 (3.7) | |||
| Time in ED (hours: mean, SD) | 4.9 (3.2) | 4.5 (2.7) | 0.4 (0.2 to 0.6) | <0.001 ** | |
| Component of Big 6 Completed (n, % of group) | Pain relief | 1891 (93.9) | 1391 (86.9) | 0.43 (0.34 to 0.54) | <0.001 * |
| Delirium | 1296 (64.4) | 887 (55.4) | 0.69 (0.60 to 0.79) | <0.001 * | |
| NEWS | 1872 (93.0) | 1363 (85.2) | 0.43 (0.35 to 0.54) | <0.001 * | |
| Bloods/ECG | 1831 (91.0) | 1370 (85.6) | 0.59 (0.48 to 0.73) | <0.001 * | |
| IV Fluids | 1495 (74.3) | 1065 (66.6) | 0.69 (0.60 to 0.80) | <0.001 * | |
| Pressure Areas | 1181 (58.7) | 899 (56.2) | 0.90 (0.79 to 1.03) | 0.134 * | |
| Completion of Big 6 (n, % of group) | Yes | 683 (33.9) | 497 (31.1) | Reference | |
| No | 1330 (66.1) | 1103 (68.9) | 0.88 (0.76 to 1.0) | 0.068 * | |
| Time to Theatre (hours: mean, SD) | 27.2 (19.2) | 30.1 (23.1) | 3.9 (1.5 to 4.3) | <0.001 ** | |
| Variable | Descriptive | Hazard Ratio | 95.0% CI | p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Sex (n, % of group) | Male | Reference | |||
| Female | 0.67 | 0.60 | 0.74 | <0.001 | |
| Age (years: mean, SD) | 1.05 | 1.04 | 1.05 | <0.001 | |
| SIMD | 1 | Reference | 0.276 | ||
| 2 | 0.89 | 0.72 | 1.09 | 0.259 | |
| 3 | 0.77 | 0.61 | 0.96 | 0.021 | |
| 4 | 0.94 | 0.76 | 1.17 | 0.580 | |
| 5 | 0.90 | 0.75 | 1.10 | 0.311 | |
| Missing | 0.00 | 0.00 | N/A | 0.861 | |
| ASA Grade (n, % of group) | 1 | 0.32 | 0.14 | 0.71 | 0.005 |
| 2 | 0.43 | 0.36 | 0.51 | <0.001 | |
| 3 | Reference | ||||
| 4 | 2.07 | 1.77 | 2.42 | <0.001 | |
| Missing | 0.90 | 0.78 | 1.03 | 0.134 | |
| Fracture Management (n, % of group) | DHS | Reference | <0.001 | ||
| Hemiarthroplasty | 0.98 | 0.87 | 1.12 | 0.812 | |
| IMN | 1.09 | 0.91 | 1.30 | 0.366 | |
| Cannulated Screws | 0.85 | 0.64 | 1.15 | 0.293 | |
| THA | 0.29 | 0.16 | 0.52 | <0.001 | |
| Other | 2.48 | 1.39 | 4.44 | 0.002 | |
| Time to Theatre (hours: mean, SD) | 1.003 | 1.001 | 1.005 | 0.017 | |
| Number of Big 6 completed in ED (n, % of group) | 0 | Reference | |||
| 1 | 0.69 | 0.32 | 1.48 | 0.345 | |
| 2 | 0.53 | 0.32 | 0.88 | 0.014 | |
| 3 | 0.73 | 0.54 | 0.98 | 0.038 | |
| 4 | 0.65 | 0.52 | 0.82 | <0.001 | |
| 5 | 0.60 | 0.49 | 0.74 | <0.001 | |
| 6 | 0.64 | 0.52 | 0.78 | <0.001 | |
| Demographic | Descriptive | Length of Stay (Days) | p-Value |
|---|---|---|---|
| Sex (mean, SD) | Male | 11.9 (10.0) | 0.225 ** |
| Female | 11.5 (10.0) | ||
| Age (correlation coefficient) | r = 0.102 | <0.001 * | |
| SIMD (n, % of group) | 1 (Most) | 12.3 (11.6) | 0.306 *** |
| 2 | 11.1 (9.1) | ||
| 3 | 11.9 (9.7) | ||
| 4 | 11.8 (10.3) | ||
| 5 (Least) | 11.5 (10.0) | ||
| Missing | 4.7 (4.1) | ||
| ASA Grade (n, % of group) | 1 | 5.5 (3.8) | <0.001 *** |
| 2 | 9.7 (7.5) | ||
| 3 | 13.1 (10.8) | ||
| 4 | 13.1 (10.5) | ||
| Missing | 6.1 (8.5) | ||
| Fracture Management (n, % of group) | DHS | 12.2 (10.3) | <0.001 *** |
| Hemiarthroplasty | 12.3 (10.4) | ||
| IM Nail | 12.7 (9.4) | ||
| Cannulated screw | 8.6 (8.0) | ||
| THA | 6.4 (5.5) | ||
| Other | 7.2 (6.8) | ||
| Time in ED (correlation coefficient) | r = 0.101 | <0.001 * | |
| Pain relief | No | 12.8 (10.1) | 0.025 ** |
| Yes | 11.5 (10.0) | ||
| Delirium | No | 11.8 (11.8) | 0.231 ** |
| Yes | 11.4 (9.7) | ||
| NEWS | No | 12.4 (10.4) | 0.122 ** |
| Yes | 11.5 (10.0) | ||
| Bloods/ECG | No | 12.9 (11.0) | 0.007 ** |
| Yes | 11.4 (9.9) | ||
| IV Fluids | No | 11.8 (10.8) | 0.390 ** |
| Yes | 11.5 (9.7) | ||
| Pressure Areas | No | 11.9 (9.7) | 0.137 ** |
| Yes | 11.4 (10.2) | ||
| Completion of Big 6 (n, % of group) | 0 | 13.8 (10.6) | 0.005 *** |
| 1 | 12.3 (10.3) | ||
| 2 | 8.8 (6.0) | ||
| 3 | 11.1 (11.2) | ||
| 4 | 11.3 (10.9) | ||
| 5 | 11.6 (8.5) | ||
| 6 | 11.4 (10.6) | ||
| Time to Theatre (correlation coefficient) | 0.153 | <0.001 * | |
| Variable | Descriptive | Beta (Days) | 95.0% CI | p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age | 0.05 | 0.01 | 0.08 | 0.005 | |
| ASA Grade | 1 | Reference | |||
| 2 | 1.05 | −0.04 | 2.15 | 0.058 | |
| 3 | 3.23 | 2.27 | 4.19 | <0.001 | |
| 4 | 2.60 | 1.15 | 4.05 | <0.001 | |
| Missing | |||||
| Fracture Management | DHS | Reference | |||
| Hemiarthroplasty | −0.02 | −0.79 | 0.74 | 0.950 | |
| IMN | 0.43 | −0.68 | 1.53 | 0.450 | |
| Cannulated Screws | −3.11 | −4.64 | −1.59 | <0.001 | |
| THA | −4.11 | −5.58 | −2.65 | <0.001 | |
| Other | 1.21 | −3.94 | 6.35 | 0.646 | |
| Time in Emergency Department | 0.17 | 0.06 | 0.28 | 0.003 | |
| Time to Theatre | 0.04 | 0.03 | 0.06 | <0.001 | |
| Number of Big 6 completed | 0 | Reference | |||
| 1 | 0.48 | −3.63 | 4.60 | 0.817 | |
| 2 | −4.09 | −6.85 | −1.34 | 0.004 | |
| 3 | −1.65 | −3.52 | 0.23 | 0.085 | |
| 4 | −1.85 | −3.40 | −0.30 | 0.019 | |
| 5 | −1.88 | −3.33 | −0.43 | 0.011 | |
| 6 | −2.34 | −3.81 | −0.88 | 0.002 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clement, N.D.; Penfold, R.S.; Duffy, A.; Murthy, K.; MacLullich, A.M.J.; Duckworth, A.D. Completion of the Emergency Department “Big 6” in Patients with an Acute Hip Fracture Is Associated with a Lower Mortality Risk and Shorter Length of Hospital Stay. J. Clin. Med. 2023, 12, 5559. https://doi.org/10.3390/jcm12175559
Clement ND, Penfold RS, Duffy A, Murthy K, MacLullich AMJ, Duckworth AD. Completion of the Emergency Department “Big 6” in Patients with an Acute Hip Fracture Is Associated with a Lower Mortality Risk and Shorter Length of Hospital Stay. Journal of Clinical Medicine. 2023; 12(17):5559. https://doi.org/10.3390/jcm12175559
Chicago/Turabian StyleClement, Nick D., Rose S. Penfold, Andrew Duffy, Krishna Murthy, Alasdair M. J. MacLullich, and Andrew D. Duckworth. 2023. "Completion of the Emergency Department “Big 6” in Patients with an Acute Hip Fracture Is Associated with a Lower Mortality Risk and Shorter Length of Hospital Stay" Journal of Clinical Medicine 12, no. 17: 5559. https://doi.org/10.3390/jcm12175559
APA StyleClement, N. D., Penfold, R. S., Duffy, A., Murthy, K., MacLullich, A. M. J., & Duckworth, A. D. (2023). Completion of the Emergency Department “Big 6” in Patients with an Acute Hip Fracture Is Associated with a Lower Mortality Risk and Shorter Length of Hospital Stay. Journal of Clinical Medicine, 12(17), 5559. https://doi.org/10.3390/jcm12175559






