Changes in Iron Status Biomarkers with Advancing Age According to Sex and Menopause: A Population-Based Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Menopausal Categories
2.3. Iron Measurements
2.4. Covariates
2.5. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. Iron Biomarkers by Sex and Age
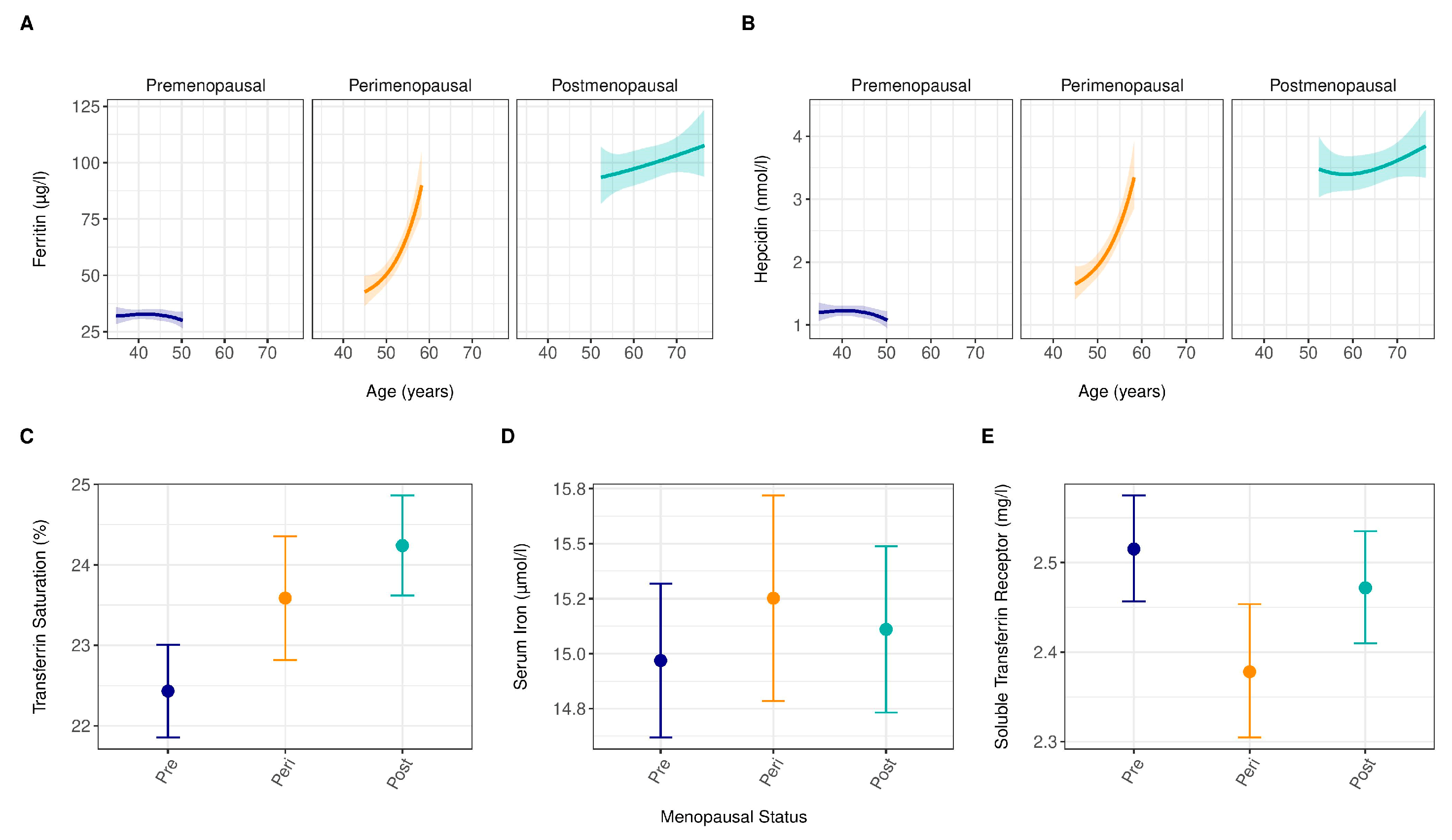
3.3. Iron Biomarkers by Menopausal Status and Age
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zacharski, L.R.; Ornstein, D.L.; Woloshin, S.; Schwartz, L.M. Association of age, sex, and race with body iron stores in adults: Analysis of NHANES III data. Am. Heart J. 2000, 140, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Nan, B.; Kong, S.; Harlow, S. Changes in iron measures over menopause and associations with insulin resistance. J Womens Health 2012, 21, 872–877. [Google Scholar] [CrossRef] [PubMed]
- Ossewaarde, M.E.; Bots, M.L.; Verbeek, A.L.; Peeters, P.H.; van der Graaf, Y.; Grobbee, D.E.; van der Schouw, Y.T. Age at menopause, cause-specific mortality and total life expectancy. Epidemiology 2005, 16, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, J.L. Iron and the sex difference in heart disease risk. Lancet 1981, 1, 1293–1294. [Google Scholar] [CrossRef]
- Kannel, W.B.; Hjortland, M.C.; McNamara, P.M.; Gordon, T. Menopause and risk of cardiovascular disease: The Framingham study. Ann. Intern. Med. 1976, 85, 447–452. [Google Scholar] [CrossRef]
- Basuli, D.; Stevens, R.G.; Torti, F.M.; Torti, S.V. Epidemiological associations between iron and cardiovascular disease and diabetes. Front. Pharmacol. 2014, 5, 117. [Google Scholar] [CrossRef]
- Chen, B.; Li, G.F.; Shen, Y.; Huang, X.I.; Xu, Y.J. Reducing iron accumulation: A potential approach for the prevention and treatment of postmenopausal osteoporosis. Exp. Ther. Med. 2015, 10, 7–11. [Google Scholar] [CrossRef]
- Moksnes, M.R.; Graham, S.E.; Wu, K.H.; Hansen, A.F.; Gagliano Taliun, S.A.; Zhou, W.; Thorstensen, K.; Fritsche, L.G.; Gill, D.; Mason, A.; et al. Genome-wide meta-analysis of iron status biomarkers and the effect of iron on all-cause mortality in HUNT. Commun. Biol. 2022, 5, 591. [Google Scholar] [CrossRef]
- Wieringa, F.T.; Berger, J.; Dijkhuizen, M.A.; Hidayat, A.; Ninh, N.X.; Utomo, B.; Wasantwisut, E.; Winichagoon, P. Sex differences in prevalence of anaemia and iron deficiency in infancy in a large multi-country trial in South-East Asia. Br. J. Nutr. 2007, 98, 1070–1076. [Google Scholar] [CrossRef]
- Milman, N.; Kirchhoff, M.; Jørgensen, T. Iron status markers, serum ferritin and hemoglobin in 1359 Danish women in relation to menstruation, hormonal contraception, parity, and postmenopausal hormone treatment. Ann. Hematol. 1992, 65, 96–102. [Google Scholar] [CrossRef]
- Milman, N.; Kirchhoff, M. Iron stores in 1359, 30- to 60-year-old Danish women: Evaluation by serum ferritin and hemoglobin. Ann. Hematol. 1992, 64, 22–27. [Google Scholar] [CrossRef]
- Ganz, T.; Olbina, G.; Girelli, D.; Nemeth, E.; Westerman, M. Immunoassay for human serum hepcidin. Blood 2008, 112, 4292–4297. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Jian, J.; Katz, S.; Abramson, S.B.; Huang, X. 17β-Estradiol inhibits iron hormone hepcidin through an estrogen responsive element half-site. Endocrinology 2012, 153, 3170–3178. [Google Scholar] [CrossRef] [PubMed]
- Groothof, D.; Post, A.; Polinder-Bos, H.A.; Erler, N.S.; Flores-Guerrero, J.L.; Kootstra-Ros, J.E.; Pol, R.A.; de Borst, M.H.; Gansevoort, R.T.; Gans, R.O.B.; et al. Muscle mass and estimates of renal function: A longitudinal cohort study. J. Cachexia Sarcopenia Muscle 2022, 13, 2031–2043. [Google Scholar] [CrossRef]
- McKinlay, S.M. The normal menopause transition: An overview. Maturitas 1996, 23, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Kroot, J.J.; Laarakkers, C.M.; Geurts-Moespot, A.J.; Grebenchtchikov, N.; Pickkers, P.; van Ede, A.E.; Peters, H.P.; van Dongen-Lases, E.; Wetzels, J.F.; Sweep, F.C.; et al. Immunochemical and mass-spectrometry-based serum hepcidin assays for iron metabolism disorders. Clin. Chem. 2010, 56, 1570–1579. [Google Scholar] [CrossRef]
- Pfeiffer, C.M.; Cook, J.D.; Mei, Z.; Cogswell, M.E.; Looker, A.C.; Lacher, D.A. Evaluation of an automated soluble transferrin receptor (sTfR) assay on the Roche Hitachi analyzer and its comparison to two ELISA assays. Clin. Chim. Acta 2007, 382, 112–116. [Google Scholar] [CrossRef]
- Sterne, J.A.; White, I.R.; Carlin, J.B.; Spratt, M.; Royston, P.; Kenward, M.G.; Wood, A.M.; Carpenter, J.R. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ 2009, 338, b2393. [Google Scholar] [CrossRef]
- Rubin, D.B. Inference and Missing Data. Biometrika 1976, 63, 581–592. [Google Scholar] [CrossRef]
- Mascitelli, L.; Pezzetta, F.; Goldstein, M.R. Iron and sex difference in longevity. Int. J. Clin. Pract. 2010, 64, 1458. [Google Scholar] [CrossRef]
- Cook, J.D.; Finch, C.A.; Smith, N.J. Evaluation of the iron status of a population. Blood 1976, 48, 449–455. [Google Scholar] [CrossRef]
- Milman, N.; Byg, K.E.; Ovesen, L.; Kirchhoff, M.; Jürgensen, K.S. Iron status in Danish women, 1984-1994: A cohort comparison of changes in iron stores and the prevalence of iron deficiency and iron overload. Eur. J. Haematol. 2003, 71, 51–61. [Google Scholar] [CrossRef]
- Cho, G.J.; Shin, J.H.; Yi, K.W.; Park, H.T.; Kim, T.; Hur, J.Y.; Kim, S.H. Serum ferritin levels are associated with metabolic syndrome in postmenopausal women but not in premenopausal women. Menopause 2011, 18, 1120–1124. [Google Scholar] [CrossRef]
- Aregbesola, A.; de Mello, V.D.; Lindström, J.; Voutilainen, S.; Virtanen, J.K.; Keinänen-Kiukaanniemi, S.; Tuomainen, T.-P.; Tuomilehto, J.; Uusitupa, M. Serum adiponectin/Ferritin ratio in relation to the risk of type 2 diabetes and insulin sensitivity. Diabetes Res. Clin. Pract. 2018, 141, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Jaeggi, T.; Moretti, D.; Kvalsvig, J.; Holding, P.A.; Tjalsma, H.; Kortman, G.A.; Joosten, I.; Mwangi, A.; Zimmermann, M.B. Iron status and systemic inflammation, but not gut inflammation, strongly predict gender-specific concentrations of serum hepcidin in infants in rural Kenya. PLoS ONE 2013, 8, e57513. [Google Scholar] [CrossRef] [PubMed]
- Waldvogel-Abramowski, S.; Waeber, G.; Gassner, C.; Buser, A.; Frey, B.M.; Favrat, B.; Tissot, J.D. Physiology of iron metabolism. Transfus. Med. Hemother 2014, 41, 213–221. [Google Scholar] [CrossRef]
- Zhu, S.; Liu, C.; Zhao, C.; Chen, G.; Meng, S.; Hong, M.; Xiang, M.; Xie, Y. Increased Serum Soluble Transferrin Receptor Levels Were Associated With High Prevalence of Cardiovascular Diseases: Insights From the National Health and Nutrition Examination Survey 2017–2018. Front. Cell Dev. Biol. 2022, 10, 874846. [Google Scholar] [CrossRef] [PubMed]
- Grisotto, G.; Raguindin, P.F.; Glisic, M.; Bally, L.; Bano, A.; Franco, O.H.; Marques-Vidal, P.; Muka, T. Menopausal Transition Is Not Associated with Dietary Change in Swiss Women. J. Nutr. 2021, 151, 1269–1276. [Google Scholar] [CrossRef]
- Behboudi-Gandevani, S.; Abtahi, H.; Saadat, N.; Tohidi, M.; Ramezani Tehrani, F. Effect of phlebotomy versus oral contraceptives containing cyproterone acetate on the clinical and biochemical parameters in women with polycystic ovary syndrome: A randomized controlled trial. J. Ovarian Res. 2019, 12, 78. [Google Scholar] [CrossRef]
- Equitani, F.; Fernandez-Real, J.M.; Menichella, G.; Koch, M.; Calvani, M.; Nobili, V.; Mingrone, G.; Manco, M. Bloodletting ameliorates insulin sensitivity and secretion in parallel to reducing liver iron in carriers of HFE gene mutations. Diabetes Care 2008, 31, 3–8. [Google Scholar] [CrossRef]
- Fernández-Real, J.M.; Peñarroja, G.; Castro, A.; García-Bragado, F.; López-Bermejo, A.; Ricart, W. Blood letting in high-ferritin type 2 diabetes: Effects on vascular reactivity. Diabetes Care 2002, 25, 2249–2255. [Google Scholar] [CrossRef] [PubMed][Green Version]


| Menopausal Status † | ||||||||
|---|---|---|---|---|---|---|---|---|
| Total Population (n = 5222) | Men (n = 2542) | Women (n = 2680) | p for Difference | Premenopausal (n = 907) | Perimenopausal (n = 529) | Postmenopausal (n = 785) | p for Trend | |
| Sociodemographic characteristics | ||||||||
| Age, mean (SD), years | 53.4 (12.0) | 54.3 (12.4) | 52.6 (11.5) | <0.001 | 42.1 (4.8) | 52.1 (4.2) | 64.0 (7.2) | <0.001 |
| Categories of age, no. (%) *, years | ||||||||
| <40 | 768 (14.7) | 369 (14.5) | 399 (14.9) | <0.001 | 326 (35.9) | 5 (0.9) | 0 (0.0) | <0.001 |
| 40–50 | 1502 (28.8) | 679 (26.7) | 823 (30.7) | 531 (58.5) | 146 (27.6) | 15 (1.9) | ||
| 50–60 | 1439 (27.6) | 664 (26.1) | 775 (28.9) | 50 (5.5) | 366 (69.2) | 246 (31.3) | ||
| 60–70 | 897 (17.2) | 464 (18.3) | 433 (16.2) | 0 (0.0) | 12 (2.3) | 354 (45.1) | ||
| >70 | 616 (11.8) | 366 (14.4) | 250 (9.3) | 0 (0.0) | 0 (0.0) | 170 (21.7) | ||
| Race, no. (%) | ||||||||
| Caucasian | 5016 (96.3) | 2434 (95.8) | 2582 (96.3) | 0.43 | 859 (94.7) | 513 (97.0) | 780 (99.4) | <0.001 |
| Negroid | 46 (0.9) | 21 (0.8) | 25 (0.9) | 12 (1.3) | 4 (0.8) | 1 (0.1) | ||
| Asian | 103 (2.0) | 54 (2.1) | 49 (1.8) | 23 (2.5) | 9 (1.7) | 4 (0.5) | ||
| Other | 57 (1.1) | 33 (1.3) | 24 (0.9) | 13 (1.4) | 3 (0.6) | 0 (0.0) | ||
| Education, no. (%) | ||||||||
| Low | 2248 (43.0) | 983 (38.7) | 1265 (47.2) | <0.001 | 236 (26.0) | 238 (45.0) | 548 (69.8) | <0.001 |
| Middle | 1324 (25.4) | 704 (27.7) | 620 (23.1) | 270 (29.7) | 119 (22.5) | 120 (15.3) | ||
| High | 1650 (31.6) | 855 (33.6) | 795 (29.7) | 401 (44.2) | 172 (32.5) | 117 (14.9) | ||
| Current smoking, no. (%) | 1446 (27.7) | 692 (27.2) | 754 (28.1) | 0.46 | 256 (28.2) | 151 (28.5) | 191 (24.3) | 0.08 |
| Alcohol consumption, ≥10 g/day, no. (%) | 1381 (26.4) | 847 (33.3) | 534 (19.9) | <0.001 | 178 (19.6) | 128 (24.2) | 159 (20.3) | 0.70 |
| Prevalent cardiovascular disease, no. (%) | 313 (6.0) | 223 (8.8) | 90 (3.4) | <0.001 | 15 (1.7) | 14 (2.6) | 38 (4.8) | <0.001 |
| Prevalent type 2 diabetes, no. (%) | 291 (5.6) | 167 (6.6) | 124 (4.6) | 0.002 | 7 (0.8) | 18 (3.4) | 66 (8.4) | <0.001 |
| Waist circumference, mean (SD), cm | 91.8 (12.7) | 96.9 (11.0) | 87.0 (12.2) | <0.001 | 83.0 (11.1) | 87.1 (11.7) | 91.2 (12.2) | <0.001 |
| Hemodynamics | ||||||||
| Systolic blood pressure, mean (SD), mm Hg | 125.7 (18.6) | 130.0 (17.6) | 121.5 (18.6) | <0.001 | 113.6 (12.7) | 120.4 (17.3) | 130.1 (20.3) | <0.001 |
| Diastolic blood pressure, mean (SD), mm Hg | 73.1 (9.0) | 76.0 (8.6) | 70.4 (8.5) | <0.001 | 67.9 (8.0) | 71.7 (8.7) | 72.4 (8.3) | <0.001 |
| Lipid spectrum | ||||||||
| Total cholesterol, mean (SD), mmol/L | 5.4 (1.0) | 5.4 (1.0) | 5.5 (1.1) | 0.23 | 4.9 (0.9) | 5.7 (1.0) | 5.9 (1.0) | <0.001 |
| HDL cholesterol, mean (SD), mmol/L | 1.3 (0.3) | 1.1 (0.3) | 1.4 (0.3) | <0.001 | 1.4 (0.3) | 1.4 (0.3) | 1.4 (0.3) | 0.28 |
| Total cholesterol/HDL cholesterol, mean (SD) | 4.5 (1.3) | 5.0 (1.3) | 4.1 (1.1) | <0.001 | 3.7 (1.0) | 4.2 (1.1) | 4.4 (1.1) | <0.001 |
| Triglycerides, median (IQR), mmol/L | 1.1 (0.8 to 1.6) | 1.2 (0.9 to 1.8) | 1.0 (0.7 to 1.4) | <0.001 | 0.8 (0.6 to 1.1) | 1.1 (0.8 to 1.4) | 1.2 (0.9 to 1.6) | <0.001 |
| Haematologic parameters | ||||||||
| Haemoglobin, mean (SD), mmol/L | 8.5 (0.8) | 9.0 (0.6) | 8.1 (0.6) | <0.001 | 7.9 (0.6) | 8.1 (0.6) | 8.2 (0.6) | <0.001 |
| Mean corpuscular volume, mean (SD), fl | 90.5 (4.6) | 90.9 (4.3) | 90.1 (4.8) | <0.001 | 89.7 (5.2) | 90.6 (4.2) | 90.4 (4.6) | 0.001 |
| Inflammation | ||||||||
| High-sensitivity C-reactive protein, median (IQR), mg/L | 1.3 (0.6 to 2.9) | 1.3 (0.6 to 2.7) | 1.4 (0.6 to 3.2) | >0.99 | 1.0 (0.4 to 2.8) | 1.3 (0.7 to 2.7) | 1.8 (0.9 to 3.6) | <0.001 |
| Renal function parameters | ||||||||
| Cystatin C-based eGFR, mean (SD), mL/min per 1.73 m2 | 90.4 (19.4) | 89.7 (20.2) | 91.0 (18.5) | 0.013 | 102.5 (13.1) | 92.7 (14.6) | 79.1 (16.6) | <0.001 |
| Urinary albumin excretion, mg/day | 8.3 (6.0 to 14.4) | 9.3 (6.5 to 17.8) | 7.5 (5.6 to 11.8) | <0.001 | 7.1 (5.5 to 10.7) | 7.8 (5.7 to 12.1) | 8.1 (5.7 to 13.3) | <0.001 |
| Categories of urinary albumin excretion, no. (%) | ||||||||
| <15 mg/day | 3981 (76.1) | 1775 (69.8) | 2206 (82.3) | <0.001 | 787 (86.8) | 433 (81.9) | 613 (78.1) | <0.001 |
| 15–29.9 mg/day | 642 (12.3) | 359 (14.1) | 283 (10.6) | 76 (8.4) | 58 (11.0) | 98 (12.5) | ||
| 30–300 mg/day | 531 (10.2) | 355 (14.0) | 176 (6.6) | 37 (4.1) | 37 (7.0) | 71 (9.0) | ||
| >300 mg/day | 68 (1.3) | 53 (2.1) | 15 (0.6) | 7 (0.8) | 1 (0.2) | 3 (0.4) | ||
| Iron Parameters | ||||||||
| Ferritin, median (IQR), µg/L | 97 (48 to 172) | 145 (87 to 232) | 60 (30 to 113) | <0.001 | 33 (17 to 61) | 61 (35 to 106) | 106 (63 to 161) | <0.001 |
| Transferrin saturation, mean (SD), % | 25.0 (9.4) | 26.8 (9.2) | 23.4 (9.2) | <0.001 | 22.6 (10.7) | 23.7 (8.2) | 24.4 (8.0) | <0.001 |
| Serum iron, mean (SD), µmol/L | 15.8 (5.6) | 16.6 (5.5) | 15.1 (5.6) | <0.001 | 15.0 (6.7) | 15.3 (4.9) | 15.2 (4.6) | 0.55 |
| Hepcidin, median (IQR), nmol/L | 3.0 (1.7 to 4.9) | 3.8 (2.4 to 5.6) | 2.4 (1.2 to 4.1) | <0.001 | 1.3 (0.6 to 2.3) | 2.6 (1.5 to 3.9) | 3.7 (2.4 to 5.6) | <0.001 |
| Soluble transferrin receptor, median (IQR), mg/L | 2.47 (2.08 to 2.97) | 2.45 (2.05 to 2.96) | 2.50 (2.11 to 2.97) | 0.001 | 2.48 (2.01 to 3.08) | 2.37 (2.00 to 2.84) | 2.48 (2.12 to 2.94) | 0.52 |
| Medication | ||||||||
| Antihypertensive drugs, no. (%) | 1083 (20.7) | 578 (22.7) | 505 (18.8) | 0.001 | 59 (6.5) | 93 (17.6) | 256 (32.6) | <0.001 |
| Lipid-lowering drugs, no. (%) | 485 (9.3) | 285 (11.2) | 200 (7.5) | <0.001 | 22 (2.4) | 21 (4.0) | 118 (15.0) | <0.001 |
| Hormones for climacteric, no. (%) | - | - | 97 (4) | 3 (0) | 51 (10) | 29 (4) | <0.001 | |
| Hormones for other reasons, no. (%) | - | - | 68 (3) | 20 (2) | 14 (3) | 21 (3) | 0.49 | |
| Menopausal Status † | ||||||
|---|---|---|---|---|---|---|
| Iron Parameters * | Total Population | Premenopausal (n = 989) | Perimenopausal (n = 555) | Postmenopausal (n = 849) | p for Trend | Reference Values |
| Ferritin, median (IQR), µg/L | 97 (47 to 171) | 33 (17 to 61) | 61 (35 to 105) | 106 (63 to 162) | <0.001 | ♂ 30–400; ♀ 15–130 |
| Transferrin saturation, mean (SD), % | 25.0 (9.4) | 22.4 (10.7) | 23.6 (8.2) | 24.2 (8.0) | <0.001 | ♂ 16–45%; ♀ 14–35 |
| Serum iron, mean (SD), µmol/L | 15.8 (5.6) | 15.0 (6.7) | 15.3 (4.9) | 15.1 (4.6) | 0.61 | ♂ 14–35; ♀ 10–25 |
| Hepcidin, median (IQR), nmol/L | 3.0 (1.7 to 4.9) | 1.3 (0.6 to 2.3) | 2.6 (1.5 to 3.8) | 3.8 (2.4 to 5.7) | <0.001 | ♂ 0.5–14.7; ♀ 0.5–14.6 |
| Soluble transferrin receptor, median (IQR), mg/L | 2.47 (2.09 to 2.97) | 2.47 (2.01 to 3.08) | 2.38 (2.02 to 2.84) | 2.47 (2.11 to 2.95) | 0.61 | ♂ 2.2–5; ♀ 1.9–4.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Merlo, F.; Groothof, D.; Khatami, F.; Ahanchi, N.S.; Wehrli, F.; Bakker, S.J.L.; Eisenga, M.F.; Muka, T. Changes in Iron Status Biomarkers with Advancing Age According to Sex and Menopause: A Population-Based Study. J. Clin. Med. 2023, 12, 5338. https://doi.org/10.3390/jcm12165338
Merlo F, Groothof D, Khatami F, Ahanchi NS, Wehrli F, Bakker SJL, Eisenga MF, Muka T. Changes in Iron Status Biomarkers with Advancing Age According to Sex and Menopause: A Population-Based Study. Journal of Clinical Medicine. 2023; 12(16):5338. https://doi.org/10.3390/jcm12165338
Chicago/Turabian StyleMerlo, Francesco, Dion Groothof, Farnaz Khatami, Noushin Sadat Ahanchi, Faina Wehrli, Stephan J. L. Bakker, Michele F. Eisenga, and Taulant Muka. 2023. "Changes in Iron Status Biomarkers with Advancing Age According to Sex and Menopause: A Population-Based Study" Journal of Clinical Medicine 12, no. 16: 5338. https://doi.org/10.3390/jcm12165338
APA StyleMerlo, F., Groothof, D., Khatami, F., Ahanchi, N. S., Wehrli, F., Bakker, S. J. L., Eisenga, M. F., & Muka, T. (2023). Changes in Iron Status Biomarkers with Advancing Age According to Sex and Menopause: A Population-Based Study. Journal of Clinical Medicine, 12(16), 5338. https://doi.org/10.3390/jcm12165338








