Unveiling the Challenges in Tandem Ureteral Stent Management for Malignant Ureteral Obstruction: Failure Rate, Risk Factors, and Durability of Their Replacement
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Surgical Technique
2.3. Statistical Analysis
3. Results
3.1. The Successful TUS Drainage Group
3.2. The Failed TUS Group
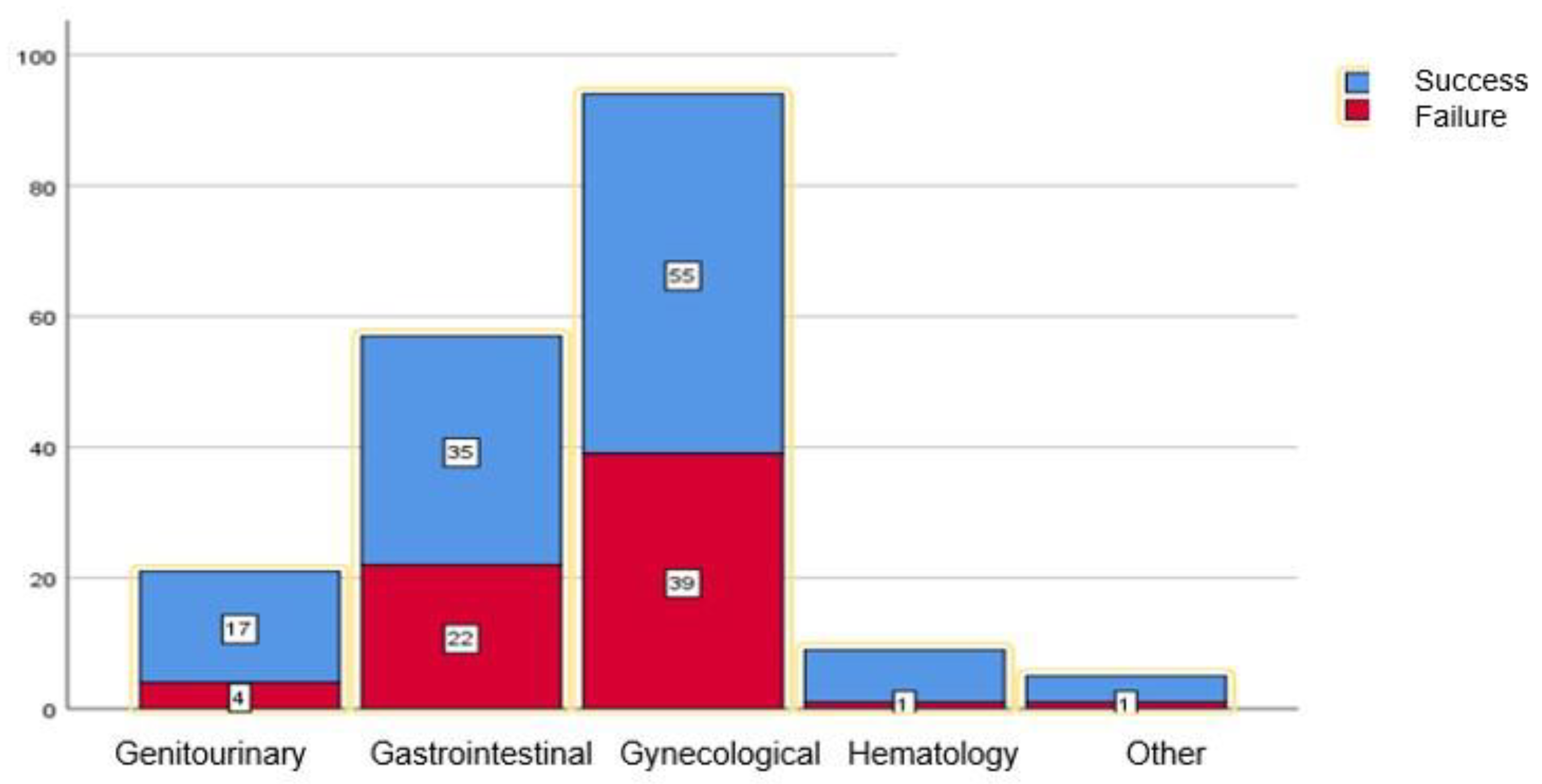
3.3. Oncological Background
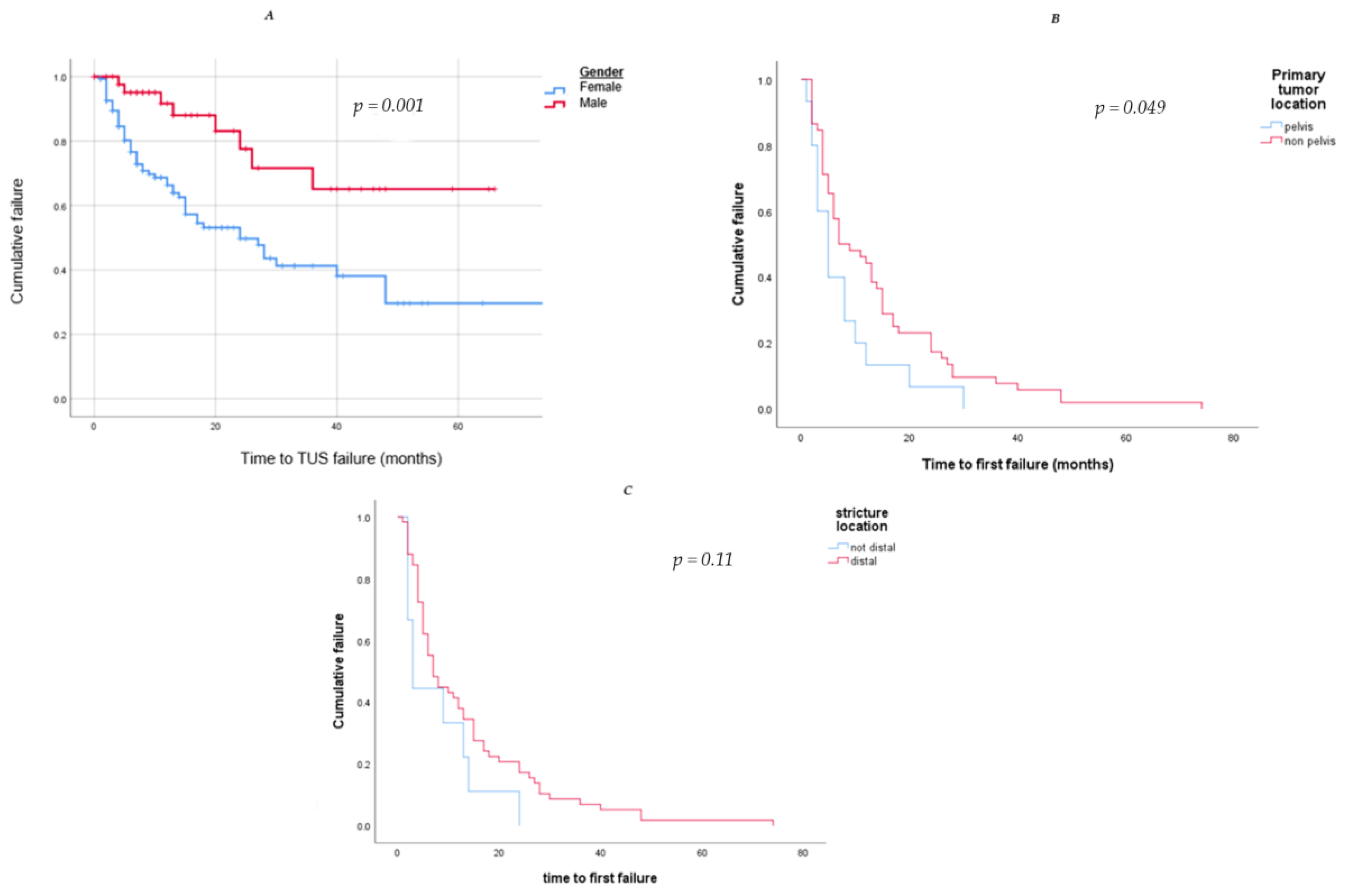
3.4. Risk Factors for TUS First Failure
3.5. Treatment after First TUS Drainage Failure
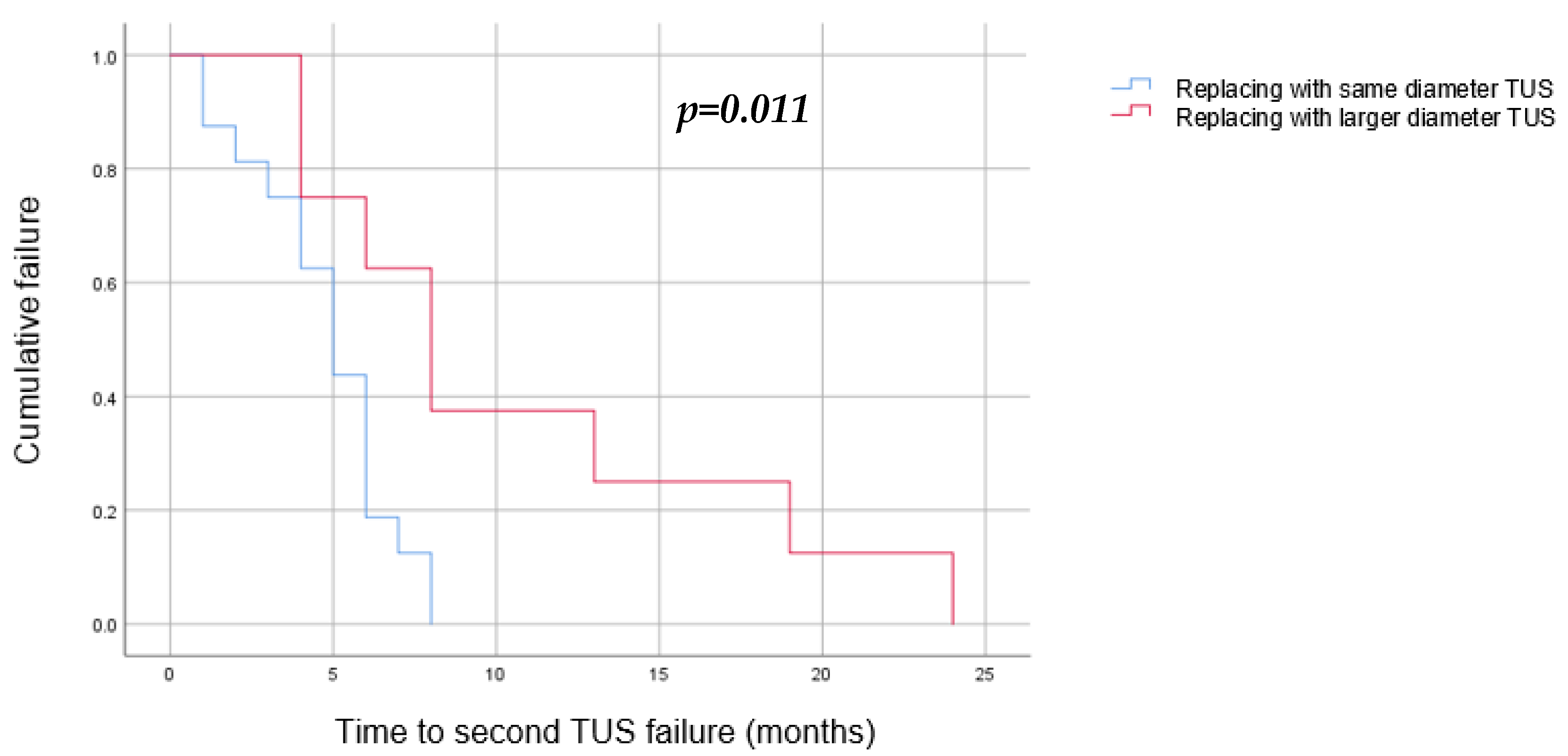
3.6. Outcomes of Replacing TUSs with a New Pair after One Failure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ganatra, A.M.; Loughlin, K.R. The management of malignant ureteral obstruction treated with ureteral stents. J. Urol. 2005, 174, 2125–2128. [Google Scholar] [CrossRef] [PubMed]
- Lienert, A.; Ing, A.; Mark, S. Prognostic factors in malignant ureteric obstruction. BJU Int. 2009, 104, 938–941. [Google Scholar] [CrossRef] [PubMed]
- Elsamra, S.E.; Leavitt, D.A.; Motato, H.A.; Friedlander, J.I.; Siev, M.; Keheila, M.; Hoenig, D.M.; Smith, A.D.; Okeke, Z. Stenting for malignant ureteral obstruction: Tandem, metal or metal-mesh stents. Int. J. Urol. 2015, 22, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.Y.; Stein, R.J.; Landsittel, D.; Davies, B.J.; Cuellar, D.C.; Hrebinko, R.L.; Tarin, T.; Averch, T.D. 15-year experience with the management of extrinsic ureteral obstruction with indwelling ureteral stents. J. Urol. 2004, 172, 592–595. [Google Scholar] [CrossRef]
- Plesinac-Karapandzic, V.; Masulovic, D.; Markovic, B.; Djuric-Stefanovic, A.; Plesinac, S.; Vucicevic, D.; Milovanovic, Z.; Milosevic, Z. Percutaneous nephrostomy in the management of advanced and terminal-stage gynecologic malignancies: Outcome and complications. Eur. J. Gynaecol. Oncol. 2010, 31, 645–650. [Google Scholar]
- Russo, P. Urologic emergencies in the cancer patient. Semin. Oncol. 2000, 27, 284–298. [Google Scholar]
- Wong, L.M.; Cleeve, L.K.; Milner, A.D.; Pitman, A.G. Malignant ureteral obstruction: Outcomes after intervention. Have things changed? J. Urol. 2007, 178, 178–183, discussion 183. [Google Scholar] [CrossRef]
- Donat, S.M.; Russo, P. Ureteral decompression in advanced nonurologic malignancies. Ann. Surg. Oncol. 1996, 3, 393–399. [Google Scholar] [CrossRef]
- Hyams, E.S.; Shah, O. Malignant extrinsic ureteral obstruction: A survey of urologists and medical oncologists regarding treatment patterns and preferences. Urology 2008, 72, 51–56. [Google Scholar] [CrossRef]
- Heo, J.E.; Jeon, D.Y.; Lee, J.; Ham, W.S.; Choi, Y.D.; Jang, W.S. Clinical Outcomes After Urinary Diversion for Malignant Ureteral Obstruction Secondary to Non-urologic Cancer: An Analysis of 778 Cases. Ann. Surg. Oncol. 2021, 28, 2367–2373. [Google Scholar] [CrossRef]
- Wu, Y.; Cao, Y.; Liu, H.; Pan, X.; Wang, J.; Huang, Y.; Qi, J.; Cui, X.; Zhang, L.; Ding, J. Comparison of the effects of extrinsic compression on the drainage performance of three ureteric stents. BJU Int. 2022, 130, 343–349. [Google Scholar] [CrossRef]
- Gu, A.; Oyo, L.; Grossmann, N.C.; Wettstein, M.S.; Kaufmann, B.; Bieri, U.; Poyet, C.; Hermanns, T.; Sulser, T.; Eberli, D.; et al. Tumor Stent for Chronic Ureteral Obstruction: Which Are Predictors of Stent Failure? J. Endourol. 2022, 36, 819–826. [Google Scholar] [CrossRef]
- Elsamra, S.E.; Motato, H.; Moreira, D.M.; Waingankar, N.; Friedlander, J.I.; Weiss, G.; Smith, A.D.; Okeke, Z. Tandem ureteral stents for the decompression of malignant and benign obstructive uropathy. J. Endourol. 2013, 27, 1297–1302. [Google Scholar] [CrossRef] [PubMed]
- Haifler, M.; Shvero, A.; Zilberman, D.; Ramon, J.; Winkler, H.; Margel, D.; Kleinmann, N. Tandem Ureteral Stents for Malignant Ureteral Obstruction. J. Endourol. 2020, 34, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Tabib, C.; Nethala, D.; Kozel, Z.; Okeke, Z. Management and treatment options when facing malignant ureteral obstruction. Int. J. Urol. 2020, 27, 591–598. [Google Scholar] [CrossRef]
- Hafron, J.; Ost, M.C.; Tan, B.J.; Fogarty, J.D.; Hoenig, D.M.; Lee, B.R.; Smith, A.D. Novel dual-lumen ureteral stents provide better ureteral flow than single ureteral stent in ex vivo porcine kidney model of extrinsic ureteral obstruction. Urology 2006, 68, 911–915. [Google Scholar] [CrossRef] [PubMed]
- Dror, I.; Harris, T.; Kalchenko, V.; Shilo, Y.; Berkowitz, B. Magnetic resonance imaging of in vitro urine flow in single and tandem stented ureters subject to extrinsic ureteral obstruction. Int. J. Urol. 2022, 29, 1221–1226. [Google Scholar] [CrossRef]
- Liu, K.L.; Lee, B.C.; Ye, J.D.; Chang, Y.H.; Chang, C.C.; Huang, K.H.; Lee, Y.J.; Chang, Y.C. Comparison of single and tandem ureteral stenting for malignant ureteral obstruction: A prospective study of 104 patients. Eur. Radiol. 2019, 29, 628–635. [Google Scholar] [CrossRef]
- Haifler, M.; Kleinmann, N.; Weiss, D. Tandem ureteral stents drainage lowers renal pelvis pressure in malignant ureteral obstruction: Experimental and computational models. J. Biomech. 2021, 117, 110237. [Google Scholar] [CrossRef]
- Gadelkareem, R.A.; Abdelraouf, A.M.; El-Taher, A.M.; Ahmed, A.I. Acute kidney injury due to bilateral malignant ureteral obstruction: Is there an optimal mode of drainage? World J. Nephrol. 2022, 11, 146–163. [Google Scholar] [CrossRef]
- Lu, C.; Zhang, W.; Peng, Y.; Li, L.; Gao, X.; Liu, M.; Fang, Z.; Wang, Z.; Ming, S.; Dong, H.; et al. Endoscopic Balloon Dilatation in the Treatment of Benign Ureteral Strictures: A Meta-Analysis and Systematic Review. J. Endourol. 2019, 33, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Reus, C.; Brehmer, M. Minimally invasive management of ureteral strictures: A 5-year retrospective study. World J. Urol. 2019, 37, 1733–1738. [Google Scholar] [CrossRef] [PubMed]
- Izumi, K.; Shima, T.; Shigehara, K.; Sawada, K.; Naito, R.; Kato, Y.; Ofude, M.; Kano, H.; Iwamoto, H.; Yaegashi, H.; et al. A novel risk classification score for malignant ureteral obstruction: A multicenter prospective validation study. Sci. Rep. 2021, 11, 4455. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, M.D.; Coelho, R.F.; Chade, D.C.; Pessoa, R.R.; Chaib, M.S.; Colombo-Junior, J.R.; Pontes-Junior, J.; Guglielmetti, G.B.; Srougi, M. A prognostic model for survival after palliative urinary diversion for malignant ureteric obstruction: A prospective study of 208 patients. BJU Int. 2016, 117, 266–271. [Google Scholar] [CrossRef]
- Ben-David, R.; Veredgorn, Y.; Savin, Z.; Bar-Yosef, Y.; Yossepowitch, O.; Sofer, M.; Mano, R. External validation of a simplified prognostic model for survival in patients with extrinsic malignant ureteral obstruction treated with tandem ureteral stents—A retrospective cohort study. Scand. J. Urol. 2023, 57, 90–96. [Google Scholar] [CrossRef]
- Amitay-Rosen, T.; Shilo, Y.; Dror, I.; Berkowitz, B. Influence of Single Stent Size and Tandem Stents Subject to Extrinsic Ureteral Obstruction and Stent Occlusion on Stent Failure. J. Endourol. 2022, 36, 236–242. [Google Scholar] [CrossRef]
- Richter, F.; Irwin, R.J., Jr.; Watson, R.A.; Lang, E.K. Endourologic management of malignant ureteral strictures. J. Endourol. 2000, 14, 583–587. [Google Scholar] [CrossRef]
- Wang, B.; Gao, W.; Yang, K.; Liu, H.; Han, Y.; Diao, M.; Zuo, C.; Zhang, M.; Diao, Y.; Li, Z.; et al. Analysis of the Efficacy and Risk Factors for Failure of Balloon Dilation for Benign Ureteral Stricture. J. Clin. Med. 2023, 12, 1655. [Google Scholar] [CrossRef]
- Hu, J.; Lai, C.; Gao, M.; Li, K.; He, W.; Zhu, D.; Xie, W.; Wu, H.; Xu, M.; Huang, J.; et al. A nomogram to predict stricture-free survival in patients with ureteral stricture after balloon dilation. BMC Urol. 2021, 21, 129. [Google Scholar] [CrossRef]
- Varnavas, M.; Bolgeri, M.; Mukhtar, S.; Anson, K. The Role of Tandem Double-J Ureteral Stents in the Management of Malignant Ureteral Obstruction. J. Endourol. 2016, 30, 465–468. [Google Scholar] [CrossRef]
- Vogt, B.; Blanchet, L.H. 10-Year Experience with Reinforced Ureteral Stents for Malignant Ureteral Obstruction. Res. Rep. Urol. 2021, 13, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Pickersgill, N.A.; Wahba, B.M.; Vetter, J.M.; Cope, S.J.; Barashi, N.S.; Henning, G.M.; Du, K.; Figenshau, R.S.; Desai, A.C.; Venkatesh, R. Factors Associated with Ureteral Stent Failure in Patients with Malignant Ureteral Obstruction. J. Endourol. 2022, 36, 814–818. [Google Scholar] [CrossRef] [PubMed]
- Savin, Z.; Herzberg, H.; Ben-David, R.; Dekalo, S.; Mintz, I.; Marom, R.; Barghouthy, Y.; Mano, R.; Yossepowitch, O.; Sofer, M. Long-Term Follow-Up of Yearly Replaced Double Internal Stents for Extrinsic Malignant Ureteral Obstruction. J. Endourol. 2021, 35, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Goldsmith, Z.G.; Wang, A.J.; Banez, L.L.; Lipkin, M.E.; Ferrandino, M.N.; Preminger, G.M.; Inman, B.A. Outcomes of metallic stents for malignant ureteral obstruction. J. Urol. 2012, 188, 851–855. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Song, T.; Peng, L.; Yuan, C.; Wang, W.; Chen, J.; Xiao, K.; Wei, X. Self-expanding metal ureteral stent for ureteral stricture: Experience of a large-scale prospective study from a high-volume center—Cross-sectional study. Int. J. Surg. 2021, 95, 106161. [Google Scholar] [CrossRef]
- Shvero, A.; Haifler, M.; Mahmud, H.; Dotan, Z.; Winkler, H.; Kleinmann, N. Quality of life with tandem ureteral stents compared to percutaneous nephrostomy for malignant ureteral obstruction. Support Care Cancer 2022, 30, 9541–9548. [Google Scholar] [CrossRef]
- Shoshany, O.; Erlich, T.; Golan, S.; Kleinmann, N.; Baniel, J.; Rosenzweig, B.; Eisner, A.; Mor, Y.; Ramon, J.; Winkler, H.; et al. Ureteric stent versus percutaneous nephrostomy for acute ureteral obstruction—Clinical outcome and quality of life: A bi-center prospective study. BMC Urol. 2019, 19, 79. [Google Scholar] [CrossRef]
- Hendlin, K.; Korman, E.; Monga, M. New metallic ureteral stents: Improved tensile strength and resistance to extrinsic compression. J. Endourol. 2012, 26, 271–274. [Google Scholar] [CrossRef]
- Miyaoka, R.; Hendlin, K.; Monga, M. Resistance to extrinsic compression and maintenance of intraluminal flow in coil-reinforced stents (Silhouette Scaffold Device): An in vitro study. J. Endourol. 2010, 24, 595–598. [Google Scholar] [CrossRef]
- Corrales, M.; Doizi, S.; Barghouthy, Y.; Kamkoum, H.; Somani, B.; Traxer, O. A systematic review of long-duration stents for ureteral stricture: Which one to choose? World J. Urol. 2021, 39, 3197–3205. [Google Scholar] [CrossRef]
- Lloyd, S.N.; Tirukonda, P.; Biyani, C.S.; Wah, T.M.; Irving, H.C. The detour extra-anatomic stent--a permanent solution for benign and malignant ureteric obstruction? Eur. Urol. 2007, 52, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.W.; Ghiraldi, E.; Ellis, J.; Friedlander, J.I. Endoscopic Management of Ureteral Strictures: An Update. Curr. Urol. Rep. 2018, 19, 24. [Google Scholar] [CrossRef]
- Gnessin, E.; Yossepowitch, O.; Holland, R.; Livne, P.M.; Lifshitz, D.A. Holmium laser endoureterotomy for benign ureteral stricture: A single center experience. J. Urol. 2009, 182, 2775–2779. [Google Scholar] [CrossRef] [PubMed]
- Hibi, H.; Ohori, T.; Taki, T.; Yamada, Y.; Honda, N. Long-term results of endoureterotomy using a holmium laser. Int. J. Urol. 2007, 14, 872–874. [Google Scholar] [CrossRef] [PubMed]
- Tyritzis, S.I.; Wiklund, N.P. Ureteral strictures revisited…Trying to see the light at the end of the tunnel: A comprehensive review. J. Endourol. 2015, 29, 124–136. [Google Scholar] [CrossRef]
- Hemal, A.K.; Nayyar, R.; Gupta, N.P.; Dorairajan, L.N. Experience with robot assisted laparoscopic surgery for upper and lower benign and malignant ureteral pathologies. Urology 2010, 76, 1387–1393. [Google Scholar] [CrossRef] [PubMed]
- Vasudevan, V.P.; Johnson, E.U.; Wong, K.; Iskander, M.; Javed, S.; Gupta, N.; McCabe, J.E.; Kavoussi, L. Contemporary management of ureteral strictures. J. Clin. Urol. 2019, 12, 20–31. [Google Scholar] [CrossRef]


| Number of patients | 186 |
|---|---|
| Number of renal units | 240 (54 bilateral TUS) |
| Age (years), median (IQR) | 65 (52–74) |
| Gender (female), n (%) | 140 (75.3%) |
| Primary tumor site, n (%) | |
| Gynecologic | 94 (50.5%) |
| Gastrointestinal | 57 (30.6%) |
| Genitourinary | 21 (11.3%) |
| Hematology | 9 (4.8%) |
| Other | 5 (2.7%) |
| Metastasis at presentation, n (%) | 141 (75.8%) |
| Previous radiation therapy, n (%) | |
| Pelvic | 86 (46.2%) |
| Retroperitoneal | 6 (3.2%) |
| None | 94 (50.5%) |
| Serum Creatinine before drainage, median (IQR) | 1.3 (0.89–1.72) |
| Prior nephrostomy tube, n (%) | 33 (17.7%) |
| Side of stricture, n (%) | |
| Right | 65 (34.9%) |
| Left | 67 (36%) |
| Bilateral | 54 (29%) |
| Stricture length, mm, median (IQR) | 20 (10–30) |
| Stricture location, n (%) | |
| Proximal | 7 (3.8%) |
| Medial | 33 (17.7%) |
| Distal | 146 (78.5%) |
| Univariate Analysis | Multivariate Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| Risk Factor | Success n = 18 | Failure n = 24 | OR | 95% CI | p | OR | 95% CI | p |
| Age, years, median (IQR) | 64 (54, 66.5) | 56.6 (50, 71) | 0.991 | 0.94, 1.04 | 0.736 | |||
| Gender, Female, n (%) | 16 (88.9%) | 18 (75%) | 0.375 | 0.06, 2.12 | 0.268 | |||
| Weight, kg, median (IQR) | 63 (53, 74) | 63 (55, 68) | 0.999 | 0.96, 1.03 | 0.961 | |||
| Primary tumor system, n, (%) | ||||||||
| Gynecological | 12 (66.6%) | 10 (41.7%) | 0.83 | 0.08, 2.1 | 0.670 | |||
| Gastrointestinal | 5 (27.8%) | 11 (45.8%) | 0.379 | 0.09, 1.4 | 0.159 | |||
| Genitourinary | 1 (5.6%) | 3 (12.5%) | 0.278 | 0.02, 3.1 | 0.298 | |||
| Other | 0 | 0 | ||||||
| Stricture Location-Distal, n, (%) | 15 (83.3%) | 20 (83.3%) | 1 | 0.19, 5.15 | 1 | |||
| Stricture longer than 30mm, n, (%) | 1 (5.6%) | 10 (41.7%) | 12.14 | 1.38, 106.7 | 0.024 | 11.8 | 0.66, 210 | 0.04 |
| Same TUS size placed upon first TUS failure, n, (%) | 3 (16.7%) | 16 (66.6%) | 10 | 2.22, 44.91 | 0.003 | 43 | 3.27, 565 | 0.004 |
| Early first TUS failure, n, (%) | 4 (22.2%) | 16 (66.7%) | 7 | 1.72, 28.33 | 0.006 | 19.2 | 1.59, 230 | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carmona, O.; Shvero, A.; Zilberman, D.E.; Dotan, Z.A.; Kleinmann, N. Unveiling the Challenges in Tandem Ureteral Stent Management for Malignant Ureteral Obstruction: Failure Rate, Risk Factors, and Durability of Their Replacement. J. Clin. Med. 2023, 12, 5251. https://doi.org/10.3390/jcm12165251
Carmona O, Shvero A, Zilberman DE, Dotan ZA, Kleinmann N. Unveiling the Challenges in Tandem Ureteral Stent Management for Malignant Ureteral Obstruction: Failure Rate, Risk Factors, and Durability of Their Replacement. Journal of Clinical Medicine. 2023; 12(16):5251. https://doi.org/10.3390/jcm12165251
Chicago/Turabian StyleCarmona, Orel, Asaf Shvero, Dorit E. Zilberman, Zohar A. Dotan, and Nir Kleinmann. 2023. "Unveiling the Challenges in Tandem Ureteral Stent Management for Malignant Ureteral Obstruction: Failure Rate, Risk Factors, and Durability of Their Replacement" Journal of Clinical Medicine 12, no. 16: 5251. https://doi.org/10.3390/jcm12165251
APA StyleCarmona, O., Shvero, A., Zilberman, D. E., Dotan, Z. A., & Kleinmann, N. (2023). Unveiling the Challenges in Tandem Ureteral Stent Management for Malignant Ureteral Obstruction: Failure Rate, Risk Factors, and Durability of Their Replacement. Journal of Clinical Medicine, 12(16), 5251. https://doi.org/10.3390/jcm12165251









