Everyday Cardiac Surgery in Jehovah‘s Witnesses of Typically Advanced Age: Clinical Outcome and Matched Comparison
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Surgical Management
2.3. Statistical Methods
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jehovah’s Witnesses. Why Don’t Jehovah’s Witnesses Accept Blood Transfusions? Available online: https://www.jw.org/en/jehovahs-witnesses/faq/jehovahs-witnesses-why-no-blood-transfusions/ (accessed on 29 December 2022).
- Chae, C.; Okocha, O.; Sweitzer, B. Preoperative considerations for Jehovah’s Witness patients: A clinical guide. Curr. Opin. Anaesthesiol. 2020, 33, 432–440. [Google Scholar] [CrossRef]
- Scharman, C.D.; Burger, D.; Shatzel, J.J.; Kim, E.; DeLoughery, T.G. Treatment of individuals who cannot receive blood products for religious or other reasons. Am. J. Hematol. 2017, 92, 1370–1381. [Google Scholar] [CrossRef]
- Lawson, T.; Ralph, C. Perioperative Jehovah’s Witnesses: A review. Br. J. Anaesth. 2015, 115, 676–687. [Google Scholar] [CrossRef]
- Remmers, P.A.; Speer, A.J. Clinical strategies in the medical care of Jehovah’s Witnesses. Am. J. Med. 2006, 119, 1013–1018. [Google Scholar] [CrossRef] [PubMed]
- Pavlikova, B.; van Dijk, J.P. Jehovah’s Witnesses and Their Compliance with Regulations on Smoking and Blood Treatment. Int. J. Environ. Res. Public. Health 2021, 19, 387. [Google Scholar] [CrossRef] [PubMed]
- Chambault, A.L.; Brown, L.J.; Mellor, S.; Harky, A. Outcomes of cardiac surgery in Jehovah’s Witness patients: A review. Perfusion 2021, 36, 661–671. [Google Scholar] [CrossRef]
- Wade, P. Treating Jehovah’s Witnesses. Br. J. Perioper. Nurs. 2004, 14, 254–257. [Google Scholar] [CrossRef]
- Moraca, R.J.; Wanamaker, K.M.; Bailey, S.H.; McGregor, W.E.; Benckart, D.H.; Maher, T.D.; Magovern, G.J., Jr. Strategies and outcomes of cardiac surgery in Jehovah’s Witnesses. J. Card. Surg. 2011, 26, 135–143. [Google Scholar] [CrossRef]
- Crowe, E.P.; DeSimone, R.A. Transfusion support and alternatives for Jehovah’s Witness patients. Curr. Opin. Hematol. 2019, 26, 473–479. [Google Scholar] [CrossRef]
- Düsseldorf, K.E.D.U. Handlungsempfehlungen für Die BEHANDLUNG von Zeugen Jehovas bei Bluttransfusionen. Available online: https://www.uniklinik-duesseldorf.de/fileadmin/Ausbildung_und_Karriere/KEK/Handlungsempfehlungen_fuer_den_Umgang_mit_Jehovas_Zeugen_Patienten_bei_geplanter_oder_unvorhergesehener_Bluttransfusion.pdf (accessed on 29 December 2022).
- Vasques, F.; Kinnunen, E.M.; Pol, M.; Mariscalco, G.; Onorati, F.; Biancari, F. Outcome of Jehovah’s Witnesses after adult cardiac surgery: Systematic review and meta-analysis of comparative studies. Transfusion 2016, 56, 2146–2153. [Google Scholar] [CrossRef] [PubMed]
- Marinakis, S.; Van der Linden, P.; Tortora, R.; Massaut, J.; Pierrakos, C.; Wauthy, P. Outcomes from cardiac surgery in Jehovah’s witness patients: Experience over twenty-one years. J. Cardiothorac. Surg. 2016, 11, 67. [Google Scholar] [CrossRef] [PubMed]
- Jehovah’s Witnesses. How Many of Jehovah’s Witnesses are There Worldwide? Available online: https://www.jw.org/en/jehovahs-witnesses/faq/how-many-jw/ (accessed on 3 February 2023).
- Müller, H.; Ratschiller, T.; Schimetta, W.; Meier, J.; Gombotz, H.; Zierer, A. Open Heart Surgery in Jehovah’s Witnesses: A Propensity Score Analysis. Ann. Thorac. Surg. 2020, 109, 526–533. [Google Scholar] [CrossRef] [PubMed]
- Wauthy, P.; Pierrakos, C.; Chebli, L.; Tortora, R. Long-term survival and quality of life in Jehovah’s witnesses after cardiac surgery: A case control study. BMC Cardiovasc. Disord. 2019, 19, 73. [Google Scholar] [CrossRef] [PubMed]
- Emmert, M.Y.; Salzberg, S.P.; Theusinger, O.M.; Felix, C.; Plass, A.; Hoerstrup, S.P.; Falk, V.; Gruenenfelder, J. How good patient blood management leads to excellent outcomes in Jehovah’s witness patients undergoing cardiac surgery. Interact. Cardiovasc. Thorac. Surg. 2011, 12, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Boer, C.; Meesters, M.I.; Milojevic, M.; Benedetto, U.; Bolliger, D.; von Heymann, C.; Jeppsson, A.; Koster, A.; Osnabrugge, R.L.; Ranucci, M.; et al. 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery. J. Cardiothorac. Vasc. Anesth. 2018, 32, 88–120. [Google Scholar] [CrossRef]
- Jung, J.; Lee, M.; Kang, Y.; Cho, S.H. Patient blood management when blood is not an option: A report of two cases. Ann. Palliat. Med. 2022, 11, 2768–2772. [Google Scholar] [CrossRef]
- Shander, A.; Goodnough, L.T. Management of anemia in patients who decline blood transfusion. Am. J. Hematol. 2018, 93, 1183–1191. [Google Scholar] [CrossRef]
- Tanaka, A.; Ota, T.; Uriel, N.; Asfaw, Z.; Onsager, D.; Lonchyna, V.A.; Jeevanandam, V. Cardiovascular surgery in Jehovah’s Witness patients: The role of preoperative optimization. J. Thorac. Cardiovasc. Surg. 2015, 150, 976–983.e3. [Google Scholar] [CrossRef]
- Dhir, A.; Tempe, D.K. Anemia and Patient Blood Management in Cardiac Surgery-Literature Review and Current Evidence. J. Cardiothorac. Vasc. Anesth. 2018, 32, 2726–2742. [Google Scholar] [CrossRef]
- Nanni, G.; Vitolo, M.; Imberti, J.F.; Girolami, D.; Bonini, N.; Valenti, A.C.; Cimato, P.; Boriani, G. Short and long-term outcomes after cardiac surgery in Jehovah’s Witnesses patients: A case-control study. Intern. Emerg. Med. 2022, 18, 151–162. [Google Scholar] [CrossRef]
- Jassar, A.S.; Ford, P.A.; Haber, H.L.; Isidro, A.; Swain, J.D.; Bavaria, J.E.; Bridges, C.R. Cardiac surgery in Jehovah’s Witness patients: Ten-year experience. Ann. Thorac. Surg. 2012, 93, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Stamou, S.C.; White, T.; Barnett, S.; Boyce, S.W.; Corso, P.J.; Lefrak, E.A. Comparisons of cardiac surgery outcomes in Jehovah’s versus Non-Jehovah’s Witnesses. Am. J. Cardiol. 2006, 98, 1223–1225. [Google Scholar] [CrossRef] [PubMed]
- Bhaskar, B.; Jack, R.K.; Mullany, D.; Fraser, J. Comparison of outcome in Jehovah’s Witness patients in cardiac surgery: An Australian experience. Heart Lung Circ. 2010, 19, 655–659. [Google Scholar] [CrossRef]
- Spahn, D.R.; Schoenrath, F.; Spahn, G.H.; Seifert, B.; Stein, P.; Theusinger, O.M.; Kaserer, A.; Hegemann, I.; Hofmann, A.; Maisano, F.; et al. Effect of ultra-short-term treatment of patients with iron deficiency or anaemia undergoing cardiac surgery: A prospective randomised trial. Lancet 2019, 393, 2201–2212. [Google Scholar] [CrossRef] [PubMed]
- Vlot, E.A.; Verwijmeren, L.; van de Garde, E.M.W.; Kloppenburg, G.T.L.; van Dongen, E.P.A.; Noordzij, P.G. Intra-operative red blood cell transfusion and mortality after cardiac surgery. BMC Anesthesiol. 2019, 19, 65. [Google Scholar] [CrossRef] [PubMed]
- Veenith, T.; Sharples, L.; Gerrard, C.; Valchanov, K.; Vuylsteke, A. Survival and length of stay following blood transfusion in octogenarians following cardiac surgery. Anaesthesia 2010, 65, 331–336. [Google Scholar] [CrossRef]
- Horvath, K.A.; Acker, M.A.; Chang, H.; Bagiella, E.; Smith, P.K.; Iribarne, A.; Kron, I.L.; Lackner, P.; Argenziano, M.; Ascheim, D.D.; et al. Blood transfusion and infection after cardiac surgery. Ann. Thorac. Surg. 2013, 95, 2194–2201. [Google Scholar] [CrossRef] [PubMed]
- Bahrainwala, Z.S.; Grega, M.A.; Hogue, C.W.; Baumgartner, W.A.; Selnes, O.A.; McKhann, G.M.; Gottesman, R.F. Intraoperative hemoglobin levels and transfusion independently predict stroke after cardiac operations. Ann. Thorac. Surg. 2011, 91, 1113–1118. [Google Scholar] [CrossRef][Green Version]
- McGrath, T.; Koch, C.G.; Xu, M.; Li, L.; Mihaljevic, T.; Figueroa, P.; Blackstone, E.H. Platelet transfusion in cardiac surgery does not confer increased risk for adverse morbid outcomes. Ann. Thorac. Surg. 2008, 86, 543–553. [Google Scholar] [CrossRef]
- Frank, S.M.; Sikorski, R.A.; Konig, G.; Tsilimigras, D.I.; Hartmann, J.; Popovsky, M.A.; Pawlik, T.M.; Waters, J.H. Clinical Utility of Autologous Salvaged Blood: A Review. J. Gastrointest. Surg. 2020, 24, 464–472. [Google Scholar] [CrossRef]
- Leahy, M.F.; Hofmann, A.; Towler, S.; Trentino, K.M.; Burrows, S.A.; Swain, S.G.; Hamdorf, J.; Gallagher, T.; Koay, A.; Geelhoed, G.C.; et al. Improved outcomes and reduced costs associated with a health-system-wide patient blood management program: A retrospective observational study in four major adult tertiary-care hospitals. Transfusion 2017, 57, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Mazer, C.D.; Whitlock, R.P.; Fergusson, D.A.; Hall, J.; Belley-Cote, E.; Connolly, K.; Khanykin, B.; Gregory, A.J.; de Médicis, É.; McGuinness, S.; et al. Restrictive or Liberal Red-Cell Transfusion for Cardiac Surgery. N. Engl. J. Med. 2017, 377, 2133–2144. [Google Scholar] [CrossRef] [PubMed]
- Rashid, M.; Kromah, F.; Cooper, C. Blood transfusion and alternatives in Jehovah’s Witness patients. Curr. Opin. Anaesthesiol. 2021, 34, 125–130. [Google Scholar] [CrossRef] [PubMed]
| Norm | JW n = 32 | NW n > 20,000 | p Value | SMD | ||
|---|---|---|---|---|---|---|
| Age | years | + | 68.1 ± 9.4 69.0 (62.8–74.8) | 67.6 ± 10.0 69.0 (61.0–75.0) | 0.786 | −0.048 |
| Gender | male | 53.1% (17) | 72.4% (17,571) | 0.015 | ||
| Height | cm | + | 169 ± 9 170 (163–176) | 171 ± 9 171 (165–177) | 0.200 | 0.227 |
| Weight | kg | + | 76 ± 14 78 (64–88) | 83 ± 16 82 (72–92) | 0.011 | 0.452 |
| BMI | kg/m2 | - | 26.43 ± 4.73 25.14 (23.07–29.57) | 28.50 ± 4.82 27.92 (25.15–31.22) | 0.005 | 0.431 |
| BSA | m2 | + | 1.88 ± 0.21 1.93 (1.73–2.03) | 1.81 ± 0.59 1.95 (1.79–2.10) | 0.510 | −0.116 |
| log ES | % | - | 10.25 ± 14.89 6.73 (2.87–11.97) | 10.50 ± 14.79 5.02 (2.27–11.58) | 0.293 | 0.017 |
| Emergency | 9.4% (3) | 9.2% (2236) | 0.976 | |||
| Redo | 6.7% (2) | 4.4% (1072) | 0.549 |
| Norm | JW n = 32 | NW n = 64 | p Value | SMD | ||
|---|---|---|---|---|---|---|
| Age | years | - | 68.1 ± 9.4 68.5 (61.0–74.0) | 67.4 ± 9.6 69.0 (62.8–74.8) | 0.735 | 0.074 |
| Gender | male | 53.1% (17) | 57.8% (37) | 0.663 | ||
| Height | cm | + | 168 ± 9 169 (160–178) | 168 ± 12 169 (163–174) | 0.995 | 0.001 |
| Weight | kg | + | 76 ± 14 78 (66–85) | 77 ± 15 78 (64–88) | 0.772 | 0.063 |
| BMI | kg/m2 | + | 26.84 ± 4.79 26.08 (24.08–31.24) | 27.16 ± 4.59 26.37 (23.07–29.79) | 0.746 | 0.070 |
| BSA | m2 | + | 1.86 ± 0.19 1.88 (1.69–2.02) | 1.87 ± 0.23 1.90 (1.73–1.99) | 0.811 | 0.052 |
| log ES | % | - | 10.18 ± 14.91 4.74 (2.58–8.13) | 8.07 ± 10.92 6.51 (2.87–11.97) | 0.214 | −0.171 |
| ES II | % | - | 7.59 ± 15.97 2.08 (1.42–3.55) | 5.30 ± 11.24 2.97 (1.61–6.56) | 0.087 | −0.176 |
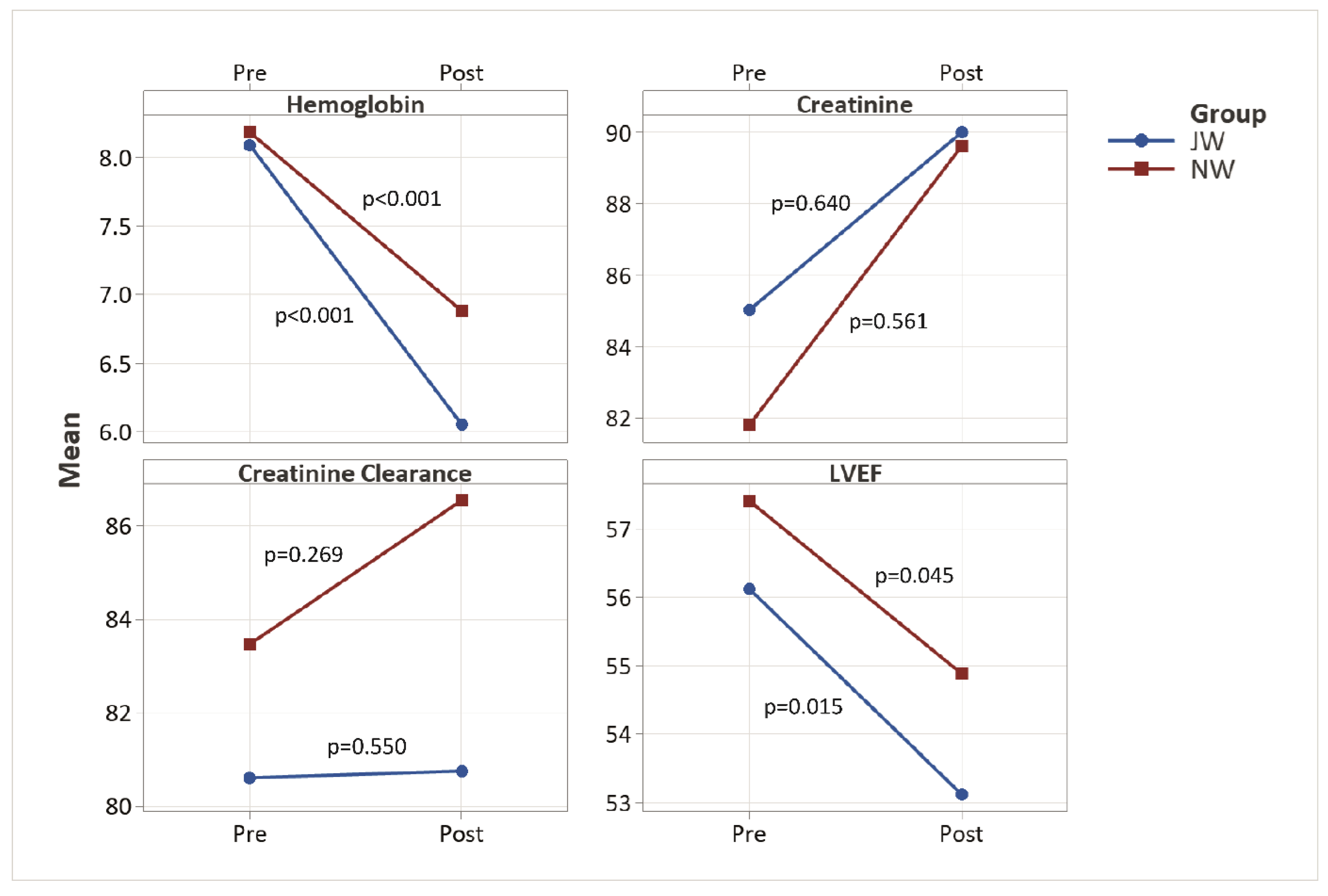
| LVEF preop | % | - | 56 ± 11 60.0 (50.0–60.0) | 57 ± 11 58.5 (50.0–61.0) | 0.749 | 0.118 |
| Emergency | 9.4% (3) | 6.3% (4) | 0.579 | |||
| Redo surgery | 6.3% (2) | 7.8% (5) | 0.781 | |||
| Hemoglobin | mmol/L | + | 8.09 ± 0.99 8.30 (7.55–9.00) | 8.18 ± 1.06 8.10 (7.60–8.75) | 0.683 | 0.089 |
| g/dL | 13.04 ± 1.60 13.37 (12.16–14.49) | 13.18 ± 1.71 13.04 (12.24–14.09) | ||||
| Hematocrit | + | 0.39 ± 0.05 0.39 (0.36–0.43) | 0.39 ± 0.05 0.38 (0.35–0.42) | 0.645 | 0.100 | |
| Creatinine | µmol/L | + | 85.0 ± 21.6 79.50 (70.00–97.00) | 81.8 ± 18.6 79.50 (72.25–103.50) | 0.452 | −0.164 |
| Crea Clearance | mL/min | - | 80.6 ± 39.7 77.74 (64.41–96.80) | 83.5 ± 31.9 78.64 (53.38–90.98) | 0.499 | 0.082 |
| Endocarditis | 12.5% (4) | 3.1% (2) | 0.074 | |||
| Malignant disease | 3.1% (1) | 4.7% (3) | 0.718 | |||
| Arterial hypertension | 59.4% (19) | 78.1% (50) | 0.054 | |||
| Hyperlipidemia | 50.0% (16) | 46.9% (30) | 0.773 | |||
| Smoking history | 3.1% (1) | 14.1% (9) | 0.098 | |||
| NIDDM | 12.5% (4) | 25.0% (16) | 0.155 | |||
| IDDM | 9.4% (3) | 9.4% (6) | 1.000 | |||
| Stroke | 3.1% (1) | 1.6% (1) | 0.613 | |||
| PVD | 6.3% (2) | 10.9% (7) | 0.458 | |||
| CVD | 3.1% (1) | 3.1% (2) | 1.000 | |||
| Myocardial infarction | 9.4% (3) | 25.0% (16) | 0.070 | |||
| COPD | 9.4% (3) | 9.4% (6) | 1.000 | |||
| Atrial fibrillation | 25.0% (8) | 10.9% (7) | 0.074 | |||
| Pacemaker | 3.1% (1) | 6.3% (4) | 0.516 |
| Norm | JW n = 32 | NW n = 64 | p Value | SMD | ||
|---|---|---|---|---|---|---|
| Preoperative EPO | 34.4% (11) | 0.0% (0) | 0.006 | |||
| Valve surgery | 56.3% (18) | 48.4% (31) | 0.470 | |||
| CABG | 56.3% (18) | 67.2% (43) | 0.294 | |||
| Ascending aorta | 15.6% (5) | 4.7% (3) | 0.068 | |||
| Aortic arch | 6.3% (2) | 1.6% (1) | 0.213 | |||
| Other cardiac procedures | 9.4% (3) | 10.9% (7) | 0.813 | |||
| Temperature | °C | - | 34.1 ± 3.3 35 (34–36) | 34.3 ± 3.0 36 (32–36) | 0.444 | 0.070 |
| Duration of surgery | min | - | 226 ± 74 225 (170–277) | 227 ± 88 209 (166–263) | 0.661 | 0.011 |
| ECC time | min | - | 132 ± 64 138 (89–173) | 124 ± 60 112 (90–139) | 0.341 | −0.123 |
| Clamp time | min | - | 81 ± 40 82 (57–105) | 73 ± 32 66 (55–81) | 0.159 | −0.227 |
| Total length of stay | days | - | 20.8 ± 10.1 20.0 (12.5–26.8) | 18.4 ± 8.2 15.6 (12.3–23.2) | 0.343 | −0.268 |
| ICU length of stay | days | - | 4.0 ± 6.5 1.0 (0.9–1.9) | 3.0 ± 6.5 1.0 (0.7–2.3) | 0.252 | −0.145 |
| Postop length of stay | days | - | 16.4 ± 8.4 14.8 (10.2–22.8) | 14.7 ± 7.5 13.0 (9.7–17.0) | 0.351 | −0.227 |
| Norm | JW n = 32 | NW n = 64 | p Value | SMD | ||
|---|---|---|---|---|---|---|
| LVEF postop | % | - | 53 ± 11 60.0 (46.3–60.0) | 55 ± 11 60.0 (50.0–60.0) | 0.521 | 0.166 |
| Hemoglobin | mmol/L | + | 6.05 ± 1.00 6.10 (5.43–6.78) | 6.88 ± 0.87 6.75 (6.20–7.40) | <0.001 | 0.903 |
| g/dL | 9.75 ± 1.61 9.82 (8.74–10.92) | 11.09 ± 1.40 10.87 (9.98–11.92) | ||||
| Hematocrit | + | 0.29 ± 0.04 0.30 (0.26–0.32) | 0.33 ± 0.04 0.32 (0.30–0.36) | <0.001 | 0.767 | |
| Creatinine | µmol/L | - | 90.0 ± 41.3 78.00 (68.75–95.75) | 89.6 ± 70.7 80.00 (60.00–94.00) | 0.614 | −0.006 |
| Crea Clearance | mL/min | - | 80.8 ± 34.6 76.83 (56.60–102.07) | 86.5 ± 38.2 79.01 (57.57–105.91) | 0.603 | 0.156 |
| Red blood cell administration | units | - | 0.1 ± 0.7 0 (0) | 2.5 ± 3.1 2 (0–4) | <0.001 | 0.948 |
| Platelet administration | units | - | 0.0 ± 0.0 0 (0) | 0.3 ± 0.8 0 (0) | 0.018 | 0.506 |
| Postoperative EPO | 15.6% (5) | 0.0% (0) | 0.001 | |||
| Rethoracotomy (bleeding, tamponade) | 6.3% (2) | 6.3% (4) | 1.000 | |||
| Pericardiocentesis | 6.3% (2) | 1.6% (1) | 0.213 | |||
| New onset atrial fibrillation | 12.5% (4) | 21.9% (14) | 0.267 | |||
| New pacemaker | 6.3% (2) | 0.0% (0) | 0.043 | |||
| Myocardial infarction | 0.0% (0) | 1.6% (1) | 0.477 | |||
| Wound healing disorders | 6.3% (2) | 7.8% (5) | 0.781 | |||
| New onset dialysis | 9.4% (3) | 3.1% (2) | 0.194 | |||
| Pneumonia | 6.3% (2) | 0.0% (0) | 0.043 | |||
| Tracheostomy | 6.3% (2) | 3.1% (2) | 0.470 | |||
| Septicemia | 0.0% (0) | 3.1% (2) | 0.312 | |||
| Stroke | 0.0% (0) | 1.6% (1) | 0.477 | |||
| Delirium | 18.8% (6) | 20.3% (13) | 0.856 | |||
| Early Mortality | 6.3% (2) | 4.7% (3) | 0.745 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hartrumpf, M.; Kuehnel, R.-U.; Ostovar, R.; Schroeter, F.; Albes, J.M. Everyday Cardiac Surgery in Jehovah‘s Witnesses of Typically Advanced Age: Clinical Outcome and Matched Comparison. J. Clin. Med. 2023, 12, 5110. https://doi.org/10.3390/jcm12155110
Hartrumpf M, Kuehnel R-U, Ostovar R, Schroeter F, Albes JM. Everyday Cardiac Surgery in Jehovah‘s Witnesses of Typically Advanced Age: Clinical Outcome and Matched Comparison. Journal of Clinical Medicine. 2023; 12(15):5110. https://doi.org/10.3390/jcm12155110
Chicago/Turabian StyleHartrumpf, Martin, Ralf-Uwe Kuehnel, Roya Ostovar, Filip Schroeter, and Johannes M. Albes. 2023. "Everyday Cardiac Surgery in Jehovah‘s Witnesses of Typically Advanced Age: Clinical Outcome and Matched Comparison" Journal of Clinical Medicine 12, no. 15: 5110. https://doi.org/10.3390/jcm12155110
APA StyleHartrumpf, M., Kuehnel, R.-U., Ostovar, R., Schroeter, F., & Albes, J. M. (2023). Everyday Cardiac Surgery in Jehovah‘s Witnesses of Typically Advanced Age: Clinical Outcome and Matched Comparison. Journal of Clinical Medicine, 12(15), 5110. https://doi.org/10.3390/jcm12155110








