Changes in Antibiotic Resistance of Acinetobacter baumannii and Pseudomonas aeruginosa Clinical Isolates in a Multi-Profile Hospital in Years 2017–2022 in Wroclaw, Poland
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacterial Strains
2.2. Microbiological Assays
2.2.1. Automated Systems
2.2.2. The Disk Diffusion Method
2.2.3. Enzyme and Immunochromatographic Tests
2.3. Statistical Analysis
3. Results
3.1. The Place of Isolate Pseudomonas aeruginosa and Acinetobacter baumanii Strains in Infections Detected at the Hospital during Period of 2017–2022
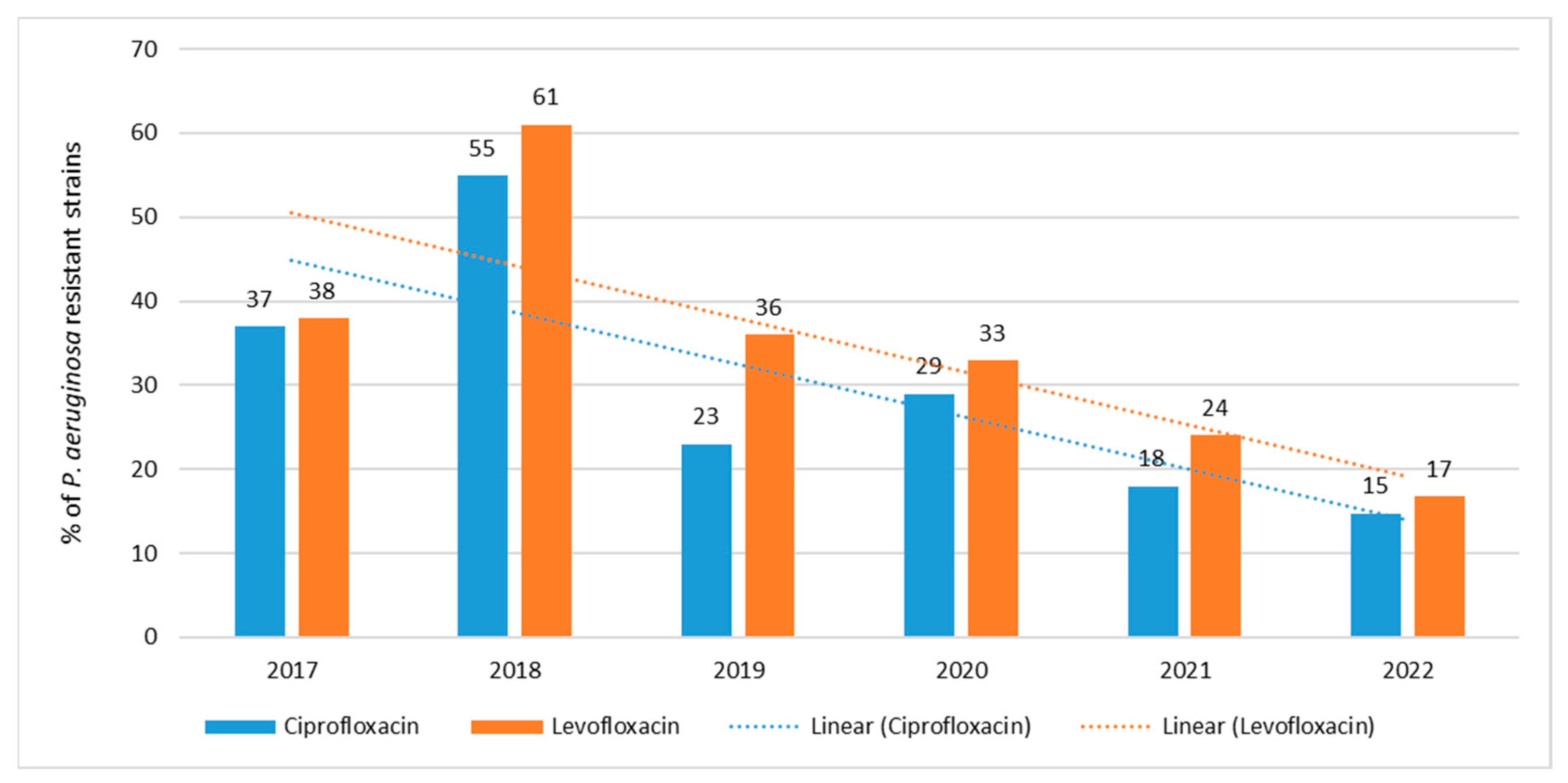
3.2. Antibiotic Resistance of P. aeruginosa Strains in 2017–2022
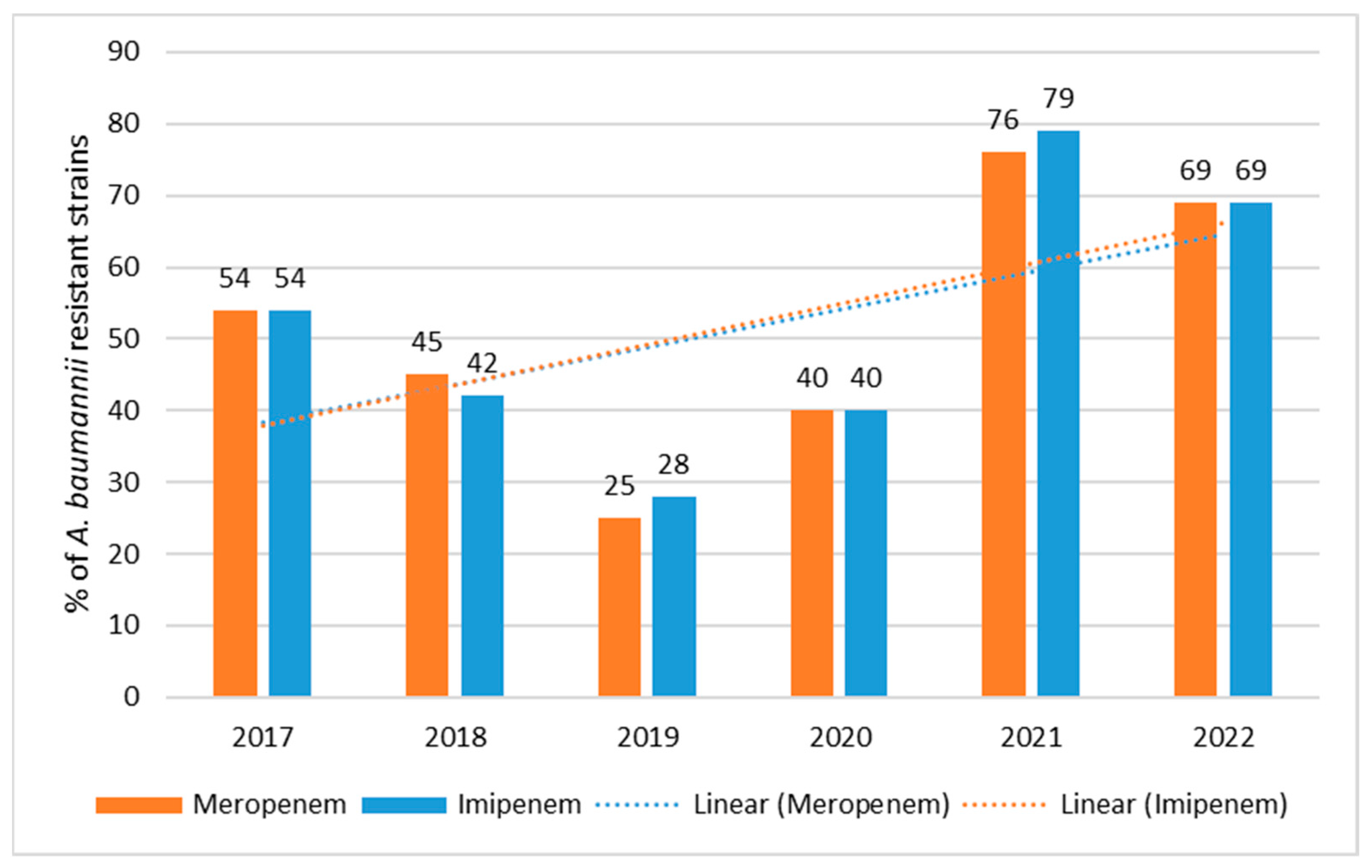
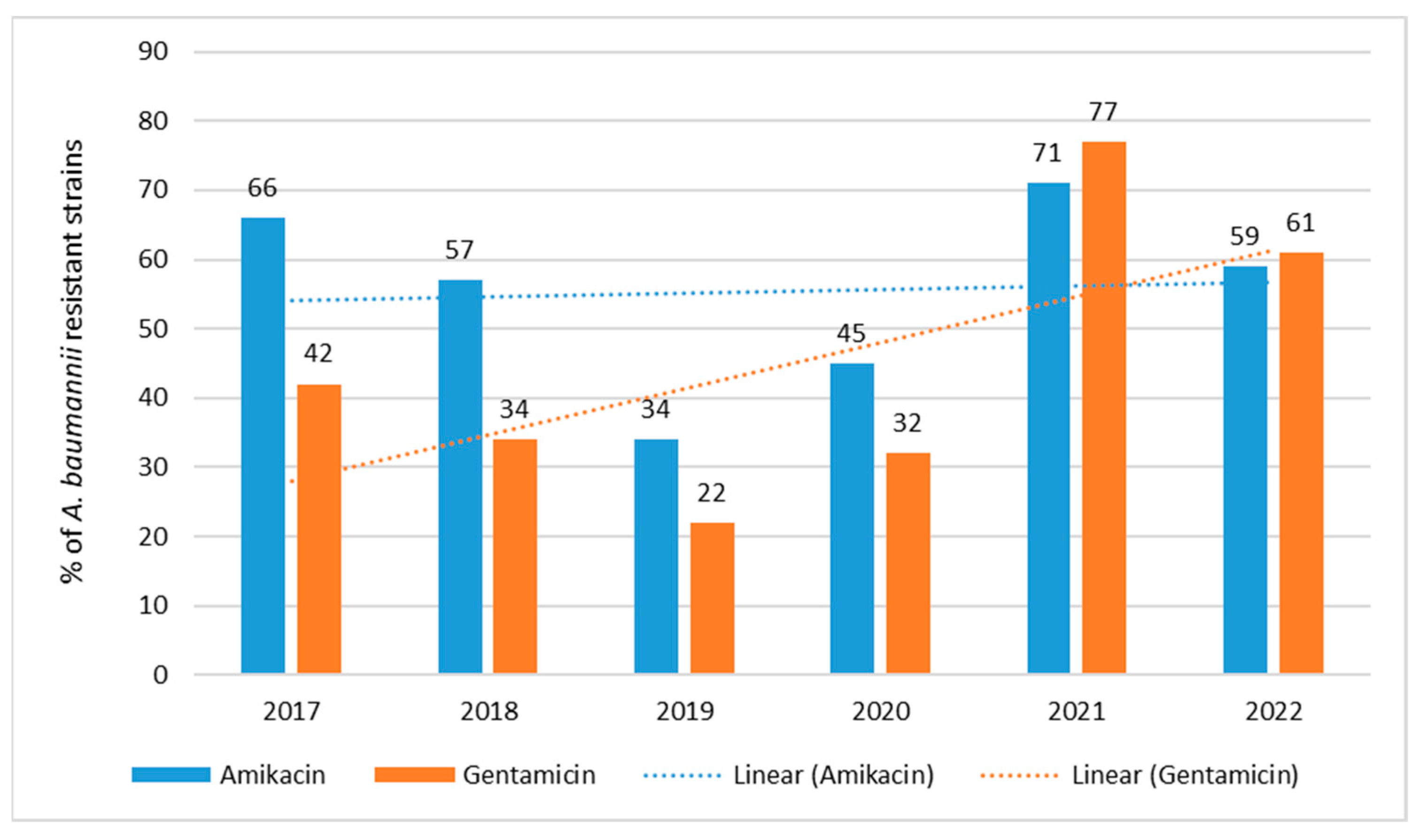
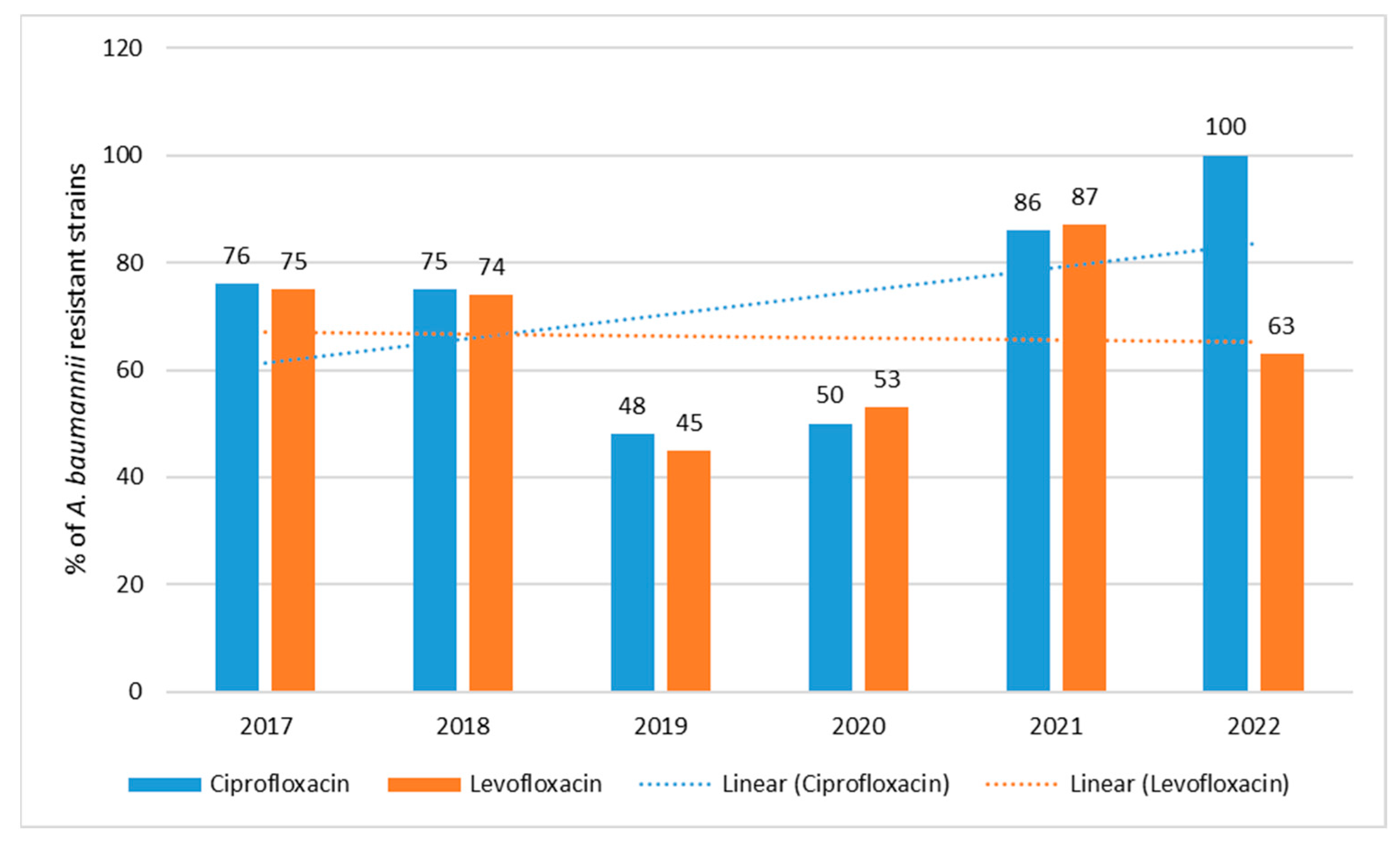
3.3. Antibiotic Resistance of A. baumannii Strains in 2017–2022
4. Discussion
5. Conclusions
- Between 2020 and 2022, the highest consumption of antibiotics in the hospital was observed, most likely due to the COVID-19 pandemic and a greater number of patients in severe condition requiring hospitalization.
- Unfortunately, during the period under review, the number of multi-resistant strains of A. baumanii was increasing successively, which seems to be related to the increased use, especially during the pandemic, of broad-spectrum antibiotics, mainly penicillins with inhibitors, third-generation cephalosporins and carbapenems.
- The simultaneous programmatic reduction in the use of some antibiotics, such as quinolones and third-generation cephalosporins in the post-pandemic period, seems to have had an impact on the renewed increase in strain susceptibility, especially for P. aeruginosa.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- de Kraker, M.E.; Stewardson, A.J.; Harbarth, S. Will 10 Million People Die a Year due to Antimicrobial Resistance by 2050? PLoS Med. 2016, 13, e1002184. [Google Scholar] [CrossRef] [PubMed]
- Basak, S.; Singh, P.; Rajurkar, M. Multidrug Resistant and Extensively Drug Resistant Bacteria: A Study. J. Pathog. 2016, 2016, 4065603. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, G.; Midiri, A.; Gerace, E.; Biondo, C. Bacterial Antibiotic Resistance: The Most Critical Pathogens. Pathogens 2021, 10, 1310. [Google Scholar] [CrossRef] [PubMed]
- Rocha, A.J.; de Oliveira Barsottini, M.R.; Rocha, R.R.; Laurindo, M.V.; de Moraes, F.L.L.; da Rocha, S.L. Pseudomonas Aeruginosa: Virulence Factors and Antibiotic Resistance Genes. Rev. Hum. Anim. Health 2019, 62, e19180503. [Google Scholar] [CrossRef]
- Morita, Y.; Tomida, J.; Kawamura, Y. Responses of Pseudomonas aeruginosa to antimicrobials. Front. Microbiol. 2014, 8, 422. [Google Scholar] [CrossRef]
- Glen, K.A.; Lamont, I.L. β-lactam Resistance in Pseudomonas aeruginosa: Current Status, Future Prospects. Pathogens 2021, 10, 1638. [Google Scholar] [CrossRef]
- Howard, A.; O’Donoghue, M.; Feeney, A.; Sleator, R.D. Acinetobacter baumannii: An emerging opportunistic pathogen. Virulence 2012, 3, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Bagińska, N.; Pichlak, A.; Górski, A.; Jończyk-Matysiak, E. Specific and Selective Bacteriophages in the Fight against Multidrug-resistant Acinetobacter baumannii. Virol. Sin. 2019, 34, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Dijkshoorn, L.; Nemec, A.; Seifert, H. An increasing threat in hospitals: Multidrug-resistant Acinetobacter baumannii. Nat. Rev. Microbiol. 2007, 5, 939–951. [Google Scholar] [CrossRef] [PubMed]
- Penwell, W.F.; Shapiro, A.B.; Giacobbe, R.A.; Gu, R.F.; Gao, N.; Thresher, J.; McLaughlin, R.E.; Huband, M.D.; DeJonge, B.L.; Ehmann, D.E.; et al. Molecular mechanisms of sulbactam antibacterial activity and resistance determinants in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2015, 59, 1680–1689. [Google Scholar] [CrossRef] [PubMed]
- Kyriakidis, I.; Vasileiou, E.; Pana, Z.D.; Tragiannidis, A. Acinetobacter baumannii Antibiotic Resistance Mechanisms. Pathogens 2021, 10, 373. [Google Scholar] [CrossRef]
- Martínez-Trejo, A.; Ruiz-Ruiz, J.M.; Gonzalez-Avila, L.U.; Saldaña-Padilla, A.; Hernández-Cortez, C.; Loyola-Cruz, M.A.; Bello-López, J.M.; Castro-Escarpulli, G. Evasion of Antimicrobial Activity in Acinetobacter baumannii by Target Site Modifications: An Effective Resistance Mechanism. Int. J. Mol. Sci. 2022, 23, 6582. [Google Scholar] [CrossRef] [PubMed]
- Tamma, P.D.; Avdic, E.; Li, D.X.; Dzintars, K.; Cosgrove, S.E. Association of Adverse Events With Antibiotic Use in Hospitalized Patients. JAMA Intern. Med. 2017, 177, 1308–1315. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, A.W. Control of hospital acquired infections and antimicrobial resistance in Europe: The way to go. main topic. Wien. Med. Wochenschr. 2019, 169 (Suppl. S1), S25–S30. [Google Scholar] [CrossRef]
- Criteria for Diagnosis of an Outbreak in a Hospital/Health Care Facility Caused by Carbapenamase-Producing Strains of Enterobacteriaceae (CPE). Guidelines of the National Antibiotic Protection Program. Available online: http://antybiotyki.edu.pl/wpcontent/uploads/dokumenty/CPE_NDM-Ognisko-epidemiczne.pdf (accessed on 31 May 2021).
- EUCAST. The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters; Version 10.0; The European Committee on Antimicrobial Susceptibility Testing: Basel, Switzerland, 2020. [Google Scholar]
- EUCAST. The European Committee on Antimicrobial Susceptibility Testing. Routine and Extended Internal Quality Control for MIC Determination and Disk Diffusion as Recommended by EUCAST; Version 10.0; The European Committee on Antimicrobial Susceptibility Testing: Basel, Switzerland, 2020. [Google Scholar]
- Skov, R.; Skov, G. EUCAST Guidelines for Detection of Resistance Mechanisms and Specific Resistances of Clinical and/or Epidemiological Importance. 2017, 6, 1–47. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Resistance_mechanisms/EUCAST_detection_of_resistance_mechanisms_170711.pdf (accessed on 1 June 2022).
- Van Dijk, K.; Voets, G.M.; Scharringa, J.; Voskuil, S.; Fluit, A.C.; Rottier, W.C.; Leverstein-Van Hall, M.A.; Cohen Stuart, J.W. A disc diffusion assay for detection of class A, B and OXA-48 carbapenemases in Enterobacteriaceae using phenyl bo ronic acid, dipicolinic acid and temocillin. Clin. Microbiol. Infect. 2014, 20, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Baraniak, A.; Grabowska, A.; Izdebski, R.; Fiett, J.; Herda, M.; Bojarska, K.; Zabicka, D.; Kania-Pudło, M.; Młynarczyk, G.; Zak-Puławska, Z.; et al. KPC-PL Study Group. Molecular characteristics of KPC-producing Enterobacteriaceae at the early stage of their dissemination in Poland, 2008–2009. Antimicrob. Agents Chemother. 2011, 55, 5493–5499. [Google Scholar] [CrossRef] [PubMed]
- Dortet, L.; Poirel, L.; Errera, C.; Nordmann, P. CarbAcineto NP test for rapid detection of carbapenemase-producing Acinetobacter spp. J. Clin. Microbiol. 2014, 52, 2359–2364. [Google Scholar] [CrossRef]
- De Oliveira, D.M.P.; Forde, B.M.; Kidd, T.J.; Harris, P.N.A.; Schembri, M.A.; Beatson, S.A.; Paterson, D.L.; Walker, M.J. Antimicrobial Resistance in ESKAPE Pathogens. Clin. Microbiol. Rev. 2020, 33, e00181-19. [Google Scholar] [CrossRef]
- Liang, C.; Zhang, X.; Zhou, L.; Meng, G.; Zhong, L.; Peng, P. Trends and correlation between antibacterial consumption and carbapenem resistance in gram-negative bacteria in a tertiary hospital in China from 2012 to 2019. BMC Infect. Dis. 2021, 21, 444. [Google Scholar] [CrossRef]
- Ayobami, O.; Brinkwirth, S.; Eckmanns, T.; Markwart, R. Antibiotic resistance in hospital-acquired ESKAPE-E infections in low- and lower-middle-income countries: A systematic review and meta-analysis. Emerg. Microbes Infect. 2022, 11, 443–451. [Google Scholar] [CrossRef]
- Hu, F.; Zhu, D.; Wang, F.; Wang, M. Current Status and Trends of Antibacterial Resistance in China. Clin. Infect. Dis. 2018, 67, 128–134. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report 2017; ECDC: Stockholm, Sweden, 2018. [Google Scholar]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report 2018; ECDC: Stockholm, Sweden, 2019. [Google Scholar]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report 2019; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report 2020; ECDC: Stockholm, Sweden, 2021. [Google Scholar]
- Mączyńska, B.; Frej-Mądrzak, M.; Sarowska, J.; Woronowicz, K.; Choroszy-Król, I.; Jama-Kmiecik, A. Evolution of Antibiotic Resistance in Escherichia coli and Klebsiella pneumoniae Clinical Isolates in a Multi-Profile Hospital over 5 Years (2017–2021). J. Clin. Med. 2023, 12, 2414. [Google Scholar] [CrossRef] [PubMed]
- Thacharodi, A.; Lamont, I.L. Aminoglycoside resistance in Pseudomonas aeruginosa: The contribution of the MexXY-OprM efflux pump varies between isolates. J. Med. Microbiol. 2022, 71. [Google Scholar] [CrossRef]
- Dou, Q.; Zhu, Y.; Li, C.; Bian, Z.; Song, H.; Zhang, R.; Wang, Y.; Zhang, X.; Wang, Y. 4F-Indole Enhances the Susceptibility of Pseudomonas aeruginosa to Aminoglycoside Antibiotics. Microbiol. Spectr. 2023, 11, e0451922. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance Surveillance in Europe 2012. In Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net); ECDC: Stockholm, Sweden, 2013. [Google Scholar]
- Yang, P.; Chen, Y.; Jiang, S.; Shen, P.; Lu, X.; Xiao, Y. Association between the rate of fluoroquinolones-resistant gram-negative bacteria and antibiotic consumption from China based on 145 tertiary hospitals data in 2014. BMC Infect. Dis. 2020, 20, 269. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report 2021; ECDC: Stockholm, Sweden, 2022. [Google Scholar]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net): Annual Epidemiological Report for 2022; ECDC: Stockholm, Sweden, 2023. [Google Scholar]
- Hooper, D.C. Emerging mechanisms of fluoroquinolone resistance. Emerg. Infect. Dis. 2001, 7, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Izdebski, R.; Fiett, J.; Hryniewicz, W.; Gniadkowski, M. Molecular analysis of Acinetobacter baumannii isolates from invasive infections in 2009 in Poland. J. Clin. Med. 2012, 50, 3813–3815. [Google Scholar] [CrossRef]
- Hou, J.; Long, X.; Wang, X.; Li, L.; Mao, D.; Luo, Y.; Ren, H. Global trend of antimicrobial resistance in common bacterial pathogens in response to antibiotic consumption. J. Hazard. Mater. 2023, 442, 130042. [Google Scholar] [CrossRef]
- Zhao, W.H.; Hu, Z.Q. Acinetobacter: A potential reservoir and dispenser for β-lactamases. Crit. Rev. Microbiol. 2012, 38, 30–51. [Google Scholar] [CrossRef]
- Hammoudi Halat, D.; Ayoub Moubareck, C. The Current Burden of Carbapenemases: Review of Significant Properties and Dissemination among Gram-Negative Bacteria. Antibiotics 2020, 9, 186. [Google Scholar] [CrossRef]
- Camargo, C.H.; Cunha, M.P.V.; de Barcellos, T.A.F.; Bueno, M.S.; Bertani, A.M.J.; Dos Santos, C.A.; Nagamori, F.O.; Takagi, E.H.; Chimara, E.; de Carvalho, E.; et al. Genomic and phenotypic characterisation of antimicrobial resistance in carbapenem-resistant Acinetobacter baumannii hyperendemic clones CC1, CC15, CC79 and CC25. Int. J. Antimicrob. Agents 2020, 56, 106195. [Google Scholar] [CrossRef] [PubMed]
- Bush, K.; Bradford, P.A. Epidemiology of β-Lactamase-Producing Pathogens. Clin. Microbiol. Rev. 2020, 33, e00047-19. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-López, R.; Solano-Gálvez, S.G.; Juárez Vignon-Whaley, J.J.; Abello Vaamonde, J.A.; Padró Alonzo, L.A.; Rivera Reséndiz, A.; Muleiro Álvarez, M.; Vega López, E.N.; Franyuti-Kelly, G.; Álvarez-Hernández, D.A.; et al. Acinetobacter baumannii Resistance: A Real Challenge for Clinicians. Antibiotics 2020, 9, 205. [Google Scholar] [CrossRef] [PubMed]
- Serio, A.W.; Keepers, T.; Andrews, L.; Krause, K.M. Aminoglycoside Revival: Review of a Historically Important Class of Antimicrobials Undergoing Rejuvenation. EcoSal Plus 2018, 8. [Google Scholar] [CrossRef]
- Fàbrega, A.; Madurga, S.; Giralt, E.; Vila, J. Mechanism of action of and resistance to quinolones. Microb. Biotechnol. 2009, 2, 40–61. [Google Scholar] [CrossRef]
- Novović, K.; Jovčić, B. Colistin Resistance in Acinetobacter baumannii: Molecular Mechanisms and Epidemiology. Antibiotics 2023, 12, 516. [Google Scholar] [CrossRef]
- Pustijanac, E.; Hrenović, J.; Vranić-Ladavac, M.; Močenić, M.; Karčić, N.; Lazarić Stefanović, L.; Hrstić, I.; Lončarić, J.; Šeruga Musić, M.; Drčelić, M.; et al. Dissemination of Clinical Acinetobacter baumannii Isolate to Hospital Environment during the COVID-19 Pandemic. Pathogens 2023, 12, 410. [Google Scholar] [CrossRef]
- Mantzana, P.; Protonotariou, E.; Kassomenaki, A.; Meletis, G.; Tychala, A.; Keskilidou, E.; Arhonti, M.; Katsanou, C.; Daviti, A.; Vasilaki, O.; et al. In Vitro Synergistic Activity of Antimicrobial Combinations against Carbapenem- and Colistin-Resistant Acinetobacter baumannii and Klebsiella pneumoniae. Antibiotics 2023, 12, 93. [Google Scholar] [CrossRef]
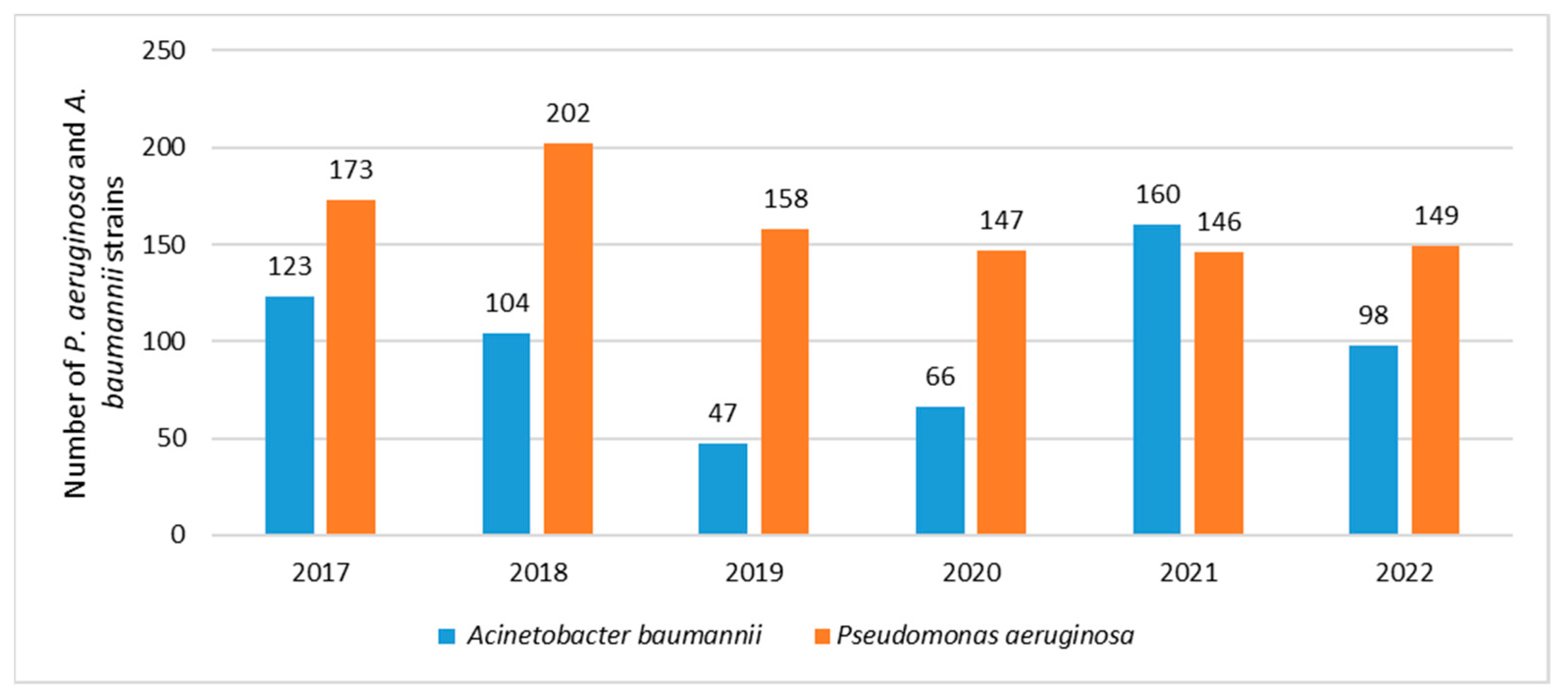




| Year/Strains | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|---|
| Pseudomonas aeruginosa | 173 | 202 | 158 | 147 | 146 | 149 |
| Acinetobacter baumannii | 123 | 104 | 47 | 66 | 160 | 98 |
| Total | 296 | 306 | 205 | 213 | 306 | 247 |
| Strain | Selected Antibiotics |
|---|---|
| Pseudomonas aeruginosa | Gentamicin, amikacin, ciprofloxacin, levofloxacin, meropenem, imipenem, ceftazidime, cefepime, piperacillin/tazobactam |
| Acinetobacter baumanii | Gentamicin, amikacin, ciprofloxacin, levofloxacin, meropenem, imipenem |
| Year/Strain | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|---|
| Escherichia coli | 791 | 917 | 851 | 742 | 770 | 822 |
| Klebsiella pneumoniae | 320 | 404 | 303 | 270 | 338 | 473 |
| Pseudomonas aeruginosa | 173 | 202 | 158 | 147 | 146 | 149 |
| Acinetobacter baumannii | 123 | 104 | 47 | 66 | 160 | 98 |
| Staphylococcus aureus | 532 | 627 | 445 | 365 | 348 | 324 |
| Enterococcus faecalis | 318 | 284 | 243 | 249 | 350 | 295 |
| Enterococcus faecium | 49 | 97 | 68 | 73 | 87 | 105 |
| Streptococcus pneumoniae | 38 | 61 | 45 | 37 | 30 | 32 |
| Other microorganisms | 23 | 41 | 39 | 47 | 89 | 34 |
| Total | 2367 | 2737 | 2199 | 1996 | 2318 | 2332 |
| Year/Strain | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
|---|---|---|---|---|---|---|
| Pseudomonas aeruginosa | 7.3 | 7.4 | 7.2 | 7.4 | 6.2 | 6.4 |
| Acinetobacter baumannii | 5.2 | 3.8 | 2.1 | 3.3 | 6.9 | 4.2 |
| Antibiotic Consumption in the Hospital (in DDD/100 Patient Days) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | TET | PES | PES+in. | C II | C III | C IV | KARB | MAK | LINK | AM | CH | GP | POL | Total |
| 2017 | 1.0 | 0.8 | 7.3 | 9.3 | 2.6 | 0.1 | 0.9 | 3.4 | 0.2 | 0.8 | 5,7 | 0.6 | 0.3 | 42.4 |
| 2018 | 0.6 | 0.7 | 7.2 | 11.0 | 3.1 | 0.2 | 1.2 | 0.6 | 0.6 | 0.6 | 9,3 | 0.9 | 0.4 | 44.0 |
| 2019 | 2.4 | 1.3 | 8.4 | 1.4 | 2.7 | 0.2 | 2.4 | 2.4 | 0.8 | 0.7 | 2,5 | 1.3 | 0.2 | 34.7 |
| 2020 | 0.8 | 1.4 | 8.3 | 2.6 | 15.7 | 0.3 | 2.0 | 0.6 | 1.1 | 1.0 | 12.7 | 1.1 | 0.4 | 58.3 |
| 2021 | 0.7 | 3.9 | 22.3 | 1.8 | 7.4 | 0.2 | 2.1 | 0.8 | 1.0 | 1.0 | 8.3 | 1.4 | 1.8 | 60.5 |
| 2022 | 0.7 | 3.3 | 25.3 | 1.8 | 4.7 | 0.2 | 2.8 | 0.8 | 1.2 | 1.5 | 7.3 | 1.4 | 1.6 | 62.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mączyńska, B.; Jama-Kmiecik, A.; Sarowska, J.; Woronowicz, K.; Choroszy-Król, I.; Piątek, D.; Frej-Mądrzak, M. Changes in Antibiotic Resistance of Acinetobacter baumannii and Pseudomonas aeruginosa Clinical Isolates in a Multi-Profile Hospital in Years 2017–2022 in Wroclaw, Poland. J. Clin. Med. 2023, 12, 5020. https://doi.org/10.3390/jcm12155020
Mączyńska B, Jama-Kmiecik A, Sarowska J, Woronowicz K, Choroszy-Król I, Piątek D, Frej-Mądrzak M. Changes in Antibiotic Resistance of Acinetobacter baumannii and Pseudomonas aeruginosa Clinical Isolates in a Multi-Profile Hospital in Years 2017–2022 in Wroclaw, Poland. Journal of Clinical Medicine. 2023; 12(15):5020. https://doi.org/10.3390/jcm12155020
Chicago/Turabian StyleMączyńska, Beata, Agnieszka Jama-Kmiecik, Jolanta Sarowska, Krystyna Woronowicz, Irena Choroszy-Król, Daniel Piątek, and Magdalena Frej-Mądrzak. 2023. "Changes in Antibiotic Resistance of Acinetobacter baumannii and Pseudomonas aeruginosa Clinical Isolates in a Multi-Profile Hospital in Years 2017–2022 in Wroclaw, Poland" Journal of Clinical Medicine 12, no. 15: 5020. https://doi.org/10.3390/jcm12155020
APA StyleMączyńska, B., Jama-Kmiecik, A., Sarowska, J., Woronowicz, K., Choroszy-Król, I., Piątek, D., & Frej-Mądrzak, M. (2023). Changes in Antibiotic Resistance of Acinetobacter baumannii and Pseudomonas aeruginosa Clinical Isolates in a Multi-Profile Hospital in Years 2017–2022 in Wroclaw, Poland. Journal of Clinical Medicine, 12(15), 5020. https://doi.org/10.3390/jcm12155020






