Abstract
The prognosis of patients with coronavirus disease 2019 (COVID-19) and pre-existing interstitial lung disease (preILD) is poor, and no effective treatment strategy has been determined. The aim of this study was to assess the effectiveness of a steroid-based treatment strategy for patients with COVID-19 and preILD. We retrospectively reviewed the medical records of 610 consecutive patients with COVID-19 treated at our institution between 1 March 2020 and 30 October 2021 and identified 7 patients with preILD, all of whom were treated with corticosteroids and remdesivir. All the patients were men with a median age of 63 years. Three of four patients with severe disease required invasive positive-pressure ventilation (n = 2) or nasal high-flow therapy (n = 1). All three patients could be weaned from respiratory support; however, one died in hospital. The remaining patient with severe COVID-19 had a do-not-resuscitate order in place and died while hospitalized. All three patients with moderate COVID-19 were discharged. The 30-day mortality was 0%, and the mortality rate during the entire observation period was 28.5%. The prognosis of our patients with COVID-19 and preILD has been better than in previous reports. Our management strategy using corticosteroids may have improved these patients’ prognosis.
1. Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and mainly affects the lung parenchyma [1,2]. Patients with interstitial lung disease (ILD) who develop COVID-19 are reported to have poor outcomes [3,4,5,6]. According to the RECOVERY trial, dexamethasone improves the prognosis of patients with COVID-19 who require supplemental oxygen [7]. There are some data suggesting that SARS-CoV-2 infection may trigger acute exacerbation of ILD (AE-ILD) in patients with pre-existing ILD (preILD) [8,9,10,11]. Hence, the treatment strategy for AE-ILD, namely, the use of high-dose corticosteroids [12] with a tapering of doses over several months, may be effective in patients who are hospitalized with COVID-19 and preILD and who fulfilled the diagnostic criteria of AE-ILD [12,13]. The purpose of this study was to assess the effectiveness of this treatment strategy in patients with COVID-19 and preILD at our institution.
2. Materials and Methods
This study was approved by the National Hospital Organization Kinki-Chuo Chest Medical Center’s Institutional Review Board (approval number Rin2021-086, date of approval: 3 February 2022) and was performed in accordance with the Declaration of Helsinki. The requirement to obtain written informed consent was waived due to this study’s retrospective design.
We retrospectively reviewed the medical records of 610 consecutive patients with COVID-19 who were treated at our institution between 1 March 2020 and 30 October 2021; we identified 7 patients from this sample with preILD. Our facility is designated for the management of patients with COVID-19 with mild-to-moderate symptoms. Patients who deteriorate to the point of requiring mechanical ventilation are usually transferred to a hospital designated for the treatment of patients with severe COVID-19 symptoms. Recovered patients who are completely weaned from mechanical ventilation usually come back to our hospital.
2.1. Diagnosis of PreILD
In all seven cases, ILD had been diagnosed before the onset of COVID-19. The diagnosis of ILD was based on the diagnostic criteria for the different types of ILD, such as idiopathic interstitial pneumonias (IIPs) [14] and idiopathic pulmonary fibrosis (IPF) [15]. Patients with IIPs except for IPF diagnosed without surgical lung biopsy (SLB) were classified as unclassifiable ILD (UN-ILD). IPF, in which pathological usual interstitial pneumonia (UIP) was confirmed by SLB specimens, was described as IPF/UIP. ILD complicated by collagen vascular disease was diagnosed according to the specific diagnostic criteria for each type of collagen vascular disorder [16,17,18]. Hypersensitivity pneumonitis was not considered a preILD in this study.
2.2. Severity of COVID-19
The severity of COVID-19 was defined according to the guidelines for its management in Japan [19] and classified as mild (not requiring supplemental oxygen), moderate (with pneumonia and/or requiring supplemental oxygen), or severe (requiring mechanical ventilation and/or extracorporeal membrane oxygenation or admission to the intensive care unit).
2.3. Treatment Strategy for COVID-19 with PreILD
All patients with COVID-19 and preILD who fulfilled the diagnostic criteria for AE-ILD [12,13] were treated with corticosteroids and remdesivir as an antiviral agent [20]. High-dose corticosteroids, usually methylprednisolone at a dose of 500–1000 mg/day for three successive days, followed by 0.5–1.0 mg/kg of prednisolone, were administered according to the severity or extent of ground-glass opacities. Dexamethasone was administered before prednisolone in some cases. The prednisolone dose was usually reduced to half of the starting dose within 2 or 3 months and tapered off according to the clinical course of the illness. In our clinical practice, the treatment strategy for COVID-19 with preILD is similar to that for AE-ILD [12], although immunosuppressants, including cyclosporine A, azathioprine, and tacrolimus, were not usually administered for COVID-19 with preILD. Some patients with COVID-19 were treated with baricitinib (oral administration), a selective inhibitor of Janus kinase 1 and 2, as an immunomodulatory drug coupled with remdesivir [21]; however, barcicinib was not used for the treatment of AE-ILD.
2.4. Diagnosis of SARS-CoV-2
Diagnosis of COVID-19 was based on a polymerase chain reaction test or an antigen test for SARS-CoV-2 from saliva, sputum, or nasopharyngeal swabs [2]. Strains of SARS-CoV-2 in each patient were not confirmed; however, we could suspect the strains (wild type, alpha strain, or delta strain) according to their epidemiological frequency at the disease onset [22,23,24,25].
2.5. Data Collection
Using the patients’ electronic medical records, we collected data on age; sex; body weight; height; body mass index; disease severity; smoking history; comorbidities; and laboratory data (including lactate dehydrogenase, ferritin, and Krebs von den Lungen-6 levels) at admission. Pulmonary function test results, including the percent predicted forced vital capacity (%FVC) and percent predicted diffusing capacity of carbon monoxide (%DLco), high-resolution computed tomography (HRCT) findings, and data on the introduction of long-term oxygen therapy before and after the onset of COVID-19, were also collected. HRCT patterns of preILDs in each patient before the onset of COVID-19 were evaluated according to the IPF guidelines [15].
We also collected treatment details, including the management of ventilation, and outcomes data. Serum Krebs von den Lungen-6 levels were measured using commercial enzyme-linked immunosorbent assay kits (Eizai, Tokyo, Japan) with a cut-off level of 500 U/mL [26]. HRCT patterns of preILDs were evaluated according to the international guideline of IPF [15].
2.6. Description of the Clinical Course
The time course of the respiratory support, steroid treatment, and outcome, including the hospital stay and survival period, were recorded. The clinical courses of severe cases and relapsed cases were explained coupled with HRCT findings. However, the changes in HRCT findings in severe and deceased cases could not be evaluated.
2.7. Comparison of the Clinical Course between Our Study and Previous Studies
We compared the outcome between patients with COVID-19 and preILD in our study and that in other reports [3,4,5,6]. The subjects of two previous studies [3,4] were in-hospital patients with COVID-19 and preILD and those of the other two previous studies were all patients with COVID-19 and preILD [5,6]. In the latter studies, the mortality rate, 30-day mortality rate, and frequency of corticosteroid-treated in-patients were calculated, and it was hypothesized that all such patients were hospitalized. Statistical analysis was not performed because our study included a limited number of patients.
3. Results
3.1. Patient Demographics
Seven patients with COVID-19 had preILD (Table 1, Figure 1). All the patients were men with a median age of 63 years (range, 49–77). Three patients were non-smokers, three were ex-smokers, and one was a current smoker. Cardiovascular diseases and emphysema were co-occurring in three and four patients, respectively; however, active malignant diseases or diabetes mellitus were not diagnosed in any patients. The preILD was IPF in two cases; unclassifiable IIP in two; and ILD associated with collagen vascular disease in three (rheumatoid arthritis, n = 2; dermatomyositis, n = 1).

Table 1.
Demographics of patients with COVID-19 and preILD.
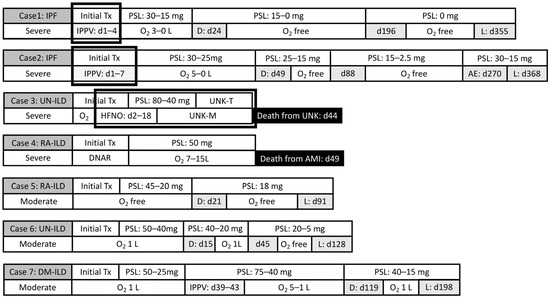
Figure 1.
Clinical course of seven patients with COVID-19 and pre-existing interstitial lung diseases: respiratory support and steroid therapy. Abbreviations: AE, acute exacerbation; AMI, acute myocardial infarction; D, discharge; d, day; DM, dermatomyositis; DNAR, do not attempt resuscitation; ILD, interstitial lung disease; IPF, idiopathic pulmonary fibrosis; IPPV, invasive positive-pressure ventilation; L, last follow-up; HFNO, high-flow nasal oxygen; PSL, prednisolone; RA, rheumatoid arthritis; UC, unclassifiable; UNK, unknown cause; UNK-S, unknown respiratory support; UNK-T, unknown steroid therapy. Initial Tx means initial steroid therapy including methylprednisolone pulse therapy and post-pulse steroid therapy, as shown in Table 2. Periods during which Cases 1, 2, and 3 were treated for intensive respiratory support in the other hospitals are shown by bold squares.
PreILD was treated with corticosteroids and/or immunosuppressive agents in three patients and an antifibrotic drug, nintedanib, in one patient before the onset of COVID-19. Long-term oxygen therapy had been introduced in the patient with preILD associated with dermatomyositis before the onset of COVID-19 (Table 1). Pulmonary function tests were performed in all cases except for one of the two patients with rheumatoid arthritis, and the median predicted percent forced vital capacity (%FVC) before the onset of COVID-19 was 91.1%.
At the onset of COVID-19, C-reactive protein and lactate dehydrogenase levels were elevated in all patients. Serum ferritin levels were elevated in five out of seven patients (Table 1).
3.2. Severity of COVID-19 and Treatment
COVID-19 symptoms were severe in four patients and moderate in three. All patients fulfilled the diagnostic criteria for AE-ILD [12,13] and received remdesivir as an antiviral agent and corticosteroids as immunosuppressive therapy. Five of the seven patients received high-dose intravenous corticosteroid therapy (methylprednisolone ≥ 500 mg). Five patients received dexamethasone and the other two patients received a tapered dose of methylprednisolone (125 mg daily). After this therapy, all patients received oral prednisolone (more than 30 mg daily). Baricitinib was administered to one patient with moderate symptoms of COVID-19 (Table 2).

Table 2.
Treatment of patients with COVID-19 and preILD.
3.3. Outcomes
One of the four patients with severe COVID-19 (Case 4) had a do-not-resuscitate order in place and was managed by standard oxygen inhalation (Figure 1). Two of the remaining three patients with severe COVID-19 required invasive positive-pressure ventilation, which was able to be withdrawn in both cases (Figure 2). These two patients were discharged after the tapering of their prednisolone dose and discontinuation of supplemental oxygen; the third patient improved after 16 days of nasal high-flow oxygen therapy but died suddenly of an unknown cause on day 44 of in-patient treatment. The patient with the do-not-resuscitate order died of acute myocardial infarction on day 49 (Figure 1).
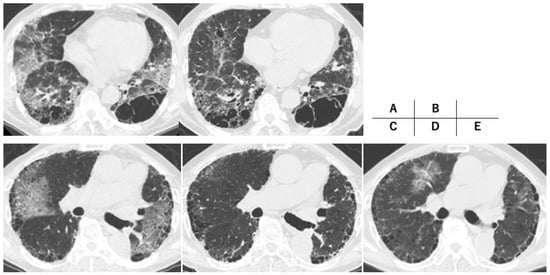
Figure 2.
High-resolution computed tomography findings of severe cases. Case 1 (A,B): idiopathic pulmonary fibrosis (IPF), a 67-year-old man ((A): onset of COVID-19, (B): one year after onset of COVID-19); Case 2 (C–E): IPF, a 73-year-old man ((C): onset of COVID-19, (D): five months after onset of COVID-19, (E): acute exacerbation nine months after onset of COVID-19).
All three patients with moderate COVID-19 improved rapidly after the initiation of corticosteroid therapy (Table 2, Figure 1). At discharge, one of these patients required supplemental oxygen at a rate of 1 L/min. The patient with ILD as a complication of dermatomyositis developed ground-glass opacities involving both lungs and a relapse of hypoxemia approximately one month after the onset of COVID-19 (Figure 1 and Figure 3). This patient’s condition improved after further treatment with corticosteroids and invasive positive-pressure ventilation (Figure 1).
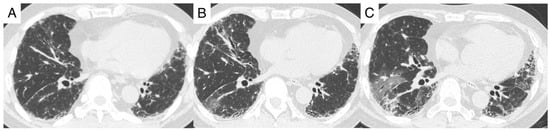
Figure 3.
High-resolution computed tomography findings of Case 7. Dermatomyositis interstitial lung diseases, a 53-year-old man ((A): three months before onset of COVID-19, (B): onset of COVID-19, (C): one month after onset of COVID-19).
All seven patients survived for at least 30 days, and both the 60-day mortality rate and the mortality rate during the entire observation period were 28.5% (Table 2). FVC was evaluated before and after COVID-19 in four patients, all of whom had a decline of >5% (Table 3). Reticular shadows increased after COVID-19 (Figure 2 and Figure 3), although it was unclear whether this radiological change reflected the natural course of preILD or was a sequela of COVID-19. None of the seven patients had an infection or diabetes mellitus after the induction of steroid therapy.

Table 3.
Pulmonary function test (FVC) before and after onset of COVID-19.
3.4. Comparison with Other Studies
We summarized the details of the four studies [3,4,5,6] and our study and compared the seven patients with COVID-19 and preILDs with those of other studies (Table 4). The in-hospital mortality rate of our study (28.5%) was lower than that of the studies of Drake et al. [4] (49.1%) and Esposito et al. [5] (44.1%).

Table 4.
Outcome of patients with COVID-19 and preILD in our study and other studies.
4. Discussion
Thus far, we have treated seven patients with a diagnosis of COVID-19 and preILD. All patients showed transient improvement, and five were discharged from the hospital alive. Previous studies have found that patients with COVID-19 and preILD have a poor prognosis and a high mortality rate [3,4,5,6,10]. However, the outcomes in our cohort have not been as bleak as previously reported.
Several studies have identified preILD to be a risk factor for developing a severe outcome of COVID-19 [27]. Drake et al. reported that 49.1% of their patients with COVID-19 and preILD died while hospitalized [4]. Another study reported a 30-day mortality rate of 35% for in-patients with COVID-19 and preILD [6]. Naqvi et al. reported 30-day and 60-day mortality rates of 27.93% and 30.63%, respectively, in in-patients with COVID-19 and IPF [3]. Esposito et al. found that 34 of 46 patients with COVID-19 and ILD required admission to the hospital and that 15 (44.1%) of these hospitalized patients died [5]. In contrast with those reports, our 30-day and 60-day mortality rates in patients with COVID-19 and preILD were 0% and 28.5%, respectively. The mortality rate during the entire observation period was also 28.5%.
Although our experience is based on a limited number of patients, these patients’ prognoses seem better than those reported elsewhere [4,5,6]. This difference in outcome might reflect the fact that our patients with COVID-19 and preILD received frequent doses of corticosteroids in addition to remdesivir, whereas fewer such patients in the previous reports received corticosteroids. In addition, the previous reports mainly included patients before the approval of remdesivir by the U.S. Food and Drugs Administration in October, 2020 [28]. Gallay et al. [6] and Esposito et al. [5] reported that approximately 10% of their patients with COVID-19 and preILD were treated with corticosteroids for COVID-19. Drake et al. [4] reported that 45 of 161 in-hospital patients with COVID-19 and preILD (28.0%) were treated with corticosteroids and their mortality rate (48.8%) was clearly worse than our study (28.5%). Although the dose and duration of corticosteroid treatment was not clarified in their study, our steroid-based treatment strategy might be better than the steroid treatment of Drake et al. [4]. Kondoh et al. reported a 30-day mortality of 50% in 12 patients with COVID-19-associated AE-ILD [10]; however, the participating institutions in their study did not provide information on the severity of COVID-19, and the clinical parameters and treatment—including possible corticosteroid use—were not described in detail.
New ground-glass opacities and an elevated oxygen requirement in patients with COVID-19 and preILD suggest a diagnosis of AE-ILD [13]. Acute deterioration of respiratory status in association with influenza in patients with ILD is diagnosed as AE [29] in view of the rarity of influenza-associated pneumonia [30]. COVID-19 also has a high mortality rate in patients without ILD [1,2]; thus, COVID-19 can be treated simply as a complication in patients with preILD. Therefore, whether acute deterioration caused by an apparent infection can be accurately called “triggered AE-ILD” is controversial [8]. However, AE-ILD and COVID-19 have some pathophysiological similarities. Accelerated alveolar epithelial apoptosis is thought to be the main pathophysiological mechanism in AE-ILD [15]. SARS-CoV-2 infection occurs via angiotensin-converting enzyme receptors, and alveolar apoptosis is a feature of COVID-19 [31]. The cytokine dynamics associated with prognosis are similar between AE-IIP [32] and COVID-19 with preILD [33,34]. Therefore, it seems likely that a management strategy for COVID-19 with preILD that is similar to that for AE-ILD could improve survival, regardless of whether these two diagnoses are the same entity.
In the RECOVERY trial [7], the 28-day mortality rate was lower in patients who received dexamethasone for up to 10 days in addition to usual care than in those who received usual care alone. Patients with COVID-19 are usually treated with dexamethasone and an antiviral agent, typically remdesivir. In our hospital, we usually treat AE-ILD with intravenous high-dose methylprednisolone—so-called “pulse therapy”—followed by a maintenance dose of prednisolone that is gradually tapered [12]. In patients with COVID-19 and preILD, we have used dexamethasone after pulse therapy and then switched to prednisolone. Immunosuppressants, including cyclosporine A, azathioprine, and tacrolimus [12,35,36], which are often used for AE-ILD [12], are not used in patients with COVID-19 and preILD at our institution. However, these agents may be useful in view of a report by Gálvez-Romero et al. indicating that cyclosporine A plus low-dose steroids improves the survival rate in patients with COVID-19 [37].
There may be some disagreements regarding the treatment strategy for COVID-19, in particular the value of long-term steroid therapy. Fonseca et al. published a report on a patient with rheumatoid-arthritis-associated ILD and COVID-19, which relapsed after approximately one week of steroid therapy and needed non-invasive positive-pressure ventilation [38]. Case 7 in our series also experienced a relapse requiring invasive positive-pressure ventilation one month after onset of COVID-19, purportedly because of a rapid reduction in the patient’s steroid dose. Patients without ILD who develop COVID-19 show persistent inflammatory abnormalities after the acute period, and post-COVID interstitial fibrosis in the chronic phase is an important problem [39]. Myall et al. suggested that prednisolone should be used at a maximum initial dose of 0.5 mg/kg for persistent inflammatory ILD that lasts for more than a month after COVID-19 [40]. Their report recommended a tapering of the prednisolone dose over approximately three weeks. In our Case 1, we tapered the prednisolone dose over approximately six months. However, the appropriate treatment duration for corticosteroids in patients with COVID-19 and preILD remains to be determined.
The progression of pulmonary fibrosis after COVID-19 in patients with preILD is another problem. We could not compare the exact FVC before and after COVID-19 because FVC was not evaluated immediately before the onset of the illness; however, there were definite decreases in FVC (Table 2) and in the radiographically confirmed progression of fibrotic lesions in our cases. The early administration of an antifibrotic agent might be able to inhibit late-phase COVID-related fibrosis after steroid therapy [41].
We managed our patients with COVID-19 and preILD using our standard treatment strategy for AE-ILD; however, the prognosis of patients with COVID-19 and preILD may be better than that of patients with AE-ILD or AE-IIP. We previously reported a 30-day mortality rate of 40% (34/85) in patients with AE-IIP [12], and Suzuki et al. found a 30-day mortality rate of 23.8% (46/193) in patients with AE-ILD [42]. In contrast, the 30-day mortality rate in patients with COVID-19 and preILD in our study was 0%. This finding might reflect differences in the histological features of AE-ILD and COVID-19. In both diseases, the main finding in the lungs at autopsy is diffuse alveolar damage [43,44]. Churg et al. also reported that surgical lung biopsy specimens showed diffuse alveolar damage (n = 4), organizing pneumonia (OP) (n = 5), and fibrosis (n = 3) [45]. Lung biopsy specimens cannot be obtained easily from patients with COVID-19 because of the risk of infection to others; however, Doglioni et al. recently reported that none of their cryobiopsy specimens, mostly obtained within two weeks after symptom onset, showed a typical pattern of diffuse alveolar damage [46]. Pogatchnik et al. reported that patients with COVID-19 whose transbronchial lung biopsy specimens showed an organizing pneumonia (OP) pattern had a good prognosis [47]. Kory et al. suggested that the prevalence of OP in early disease might be higher than previously reported [48]. Hence, the difference in frequency of the OP pattern might explain the better short-term outcome in our patients than in their counterparts with AE-ILD despite the use of the same treatment strategy.
This study has several limitations. First, it had a single-center, retrospective observational design and included a small number of cases. We have insufficiently compared the survival of our COVID-19 patients with preILD with that of the patients in the previous reports. In addition, our treatment strategy was quite different from the current standard strategy of dexamethasone therapy for COVID-19. Therefore, a large-scale multicenter study comparing dexamethasone treatment and our treatment strategy is needed to reach definitive conclusions. Second, the higher %FVC in six of our patients with preILD before the onset of COVID-19 might have contributed to the survival rate of patients with COVID-19 and preILD being better than in previous reports. Drake et al. [4] reported that a %FVC > 80% suggests a greater likelihood of survival in patients with preILD. Third, preILD in this study comprised only two cases of IPF, which might have led to these patients’ better prognosis of COVID-19 with preILD. However, Suzuki et al. reported similarly poor prognoses in patents with AE of IPF or other fibrosing types of ILD [40]. Fourth, this study did not include patients with COVID-19 and other pre-existing interstitial lung abnormalities [49]. Fifth, this study did not include cases of COVID-19 caused by the Omicron variant [50] and preILD, and the treatment strategy for such cases needs to be evaluated in another study because Omicron infection has been associated with lower mortality and hospitalization [51].
5. Conclusions
Out of 610 consecutive patients with COVID-19 diagnosed at our institution, 7 also had preILD. All seven of these patients were treated with long-term corticosteroids using the management strategy for AE-ILD in addition to remdesivir. The prognosis of these patients might have been better than that described in previous reports, although large-scale prospective studies are needed to draw definite conclusions about the efficacy of our management strategy.
Author Contributions
Conceptualization, T.A. and Y.I.; resources, Y.K., M.M., T.K. (Takehiko Kobayashi), T.K. (Tomoko Kagawa), Y.M., R.S. and T.A.; writing—original draft preparation, T.A.; writing—review and editing, Y.K., M.M., T.K. (Takehiko Kobayashi), T.K. (Tomoko Kagawa), Y.M., R.S., K.T., Y.I. and T.A.; supervision, Y.K. and K.T.; funding acquisition, T.A. and Y.I. All authors have read and agreed to the published version of the manuscript.
Funding
This work was partially supported by a JSPS KAKENHI grant (number JP17K09636) awarded to T.A., a National Hospital Organization grant (H28-NHO [Kokyu]-2) awarded to T.A., and a grant from the Japanese Ministry of Health, Labour, and Welfare (20316791) awarded to Y.I.
Institutional Review Board Statement
This study was approved by the National Hospital Organization Kinki-Chuo Chest Medical Center’s Institutional Review Board (approval number Rin2021-086, date of approval: 3 February 2022) and was performed in accordance with the Declaration of Helsinki.
Informed Consent Statement
Patient consent was waived due to this study’s retrospective design.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding authors upon reasonable request, if ethical and legal concerns are not present.
Conflicts of Interest
Y.I. is a consultant or a Steering/Advisory Committee Member of Boehringer Ingelheim, Roche, and Taiho (unrelated to this study). Y.I. has received lecture fees from Boehringer Ingelheim, Shionogi, Kyorin, and Thermo Fisher (not related to this study). T.A. has received lecture fees from Boehringer Ingelheim and Shionogi for activities not connected with the submitted work. The remaining authors have no competing interest.
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Kurahara, Y.; Kobayashi, T.; Shintani, S.; Matsuda, Y.; Tamiya, A.; Sugawara, R.; Arai, T.; Tachibana, K.; Okishio, K.; Matsui, H. Clinical characteristics of COVID-19 in Osaka, Japan: Comparison of the first-third waves with the fourth waves. Respir. Investig. 2021, 59, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, S.F.; Lakhani, D.A.; Sohail, A.H.; Maurer, J.; Sofka, S.; Sarwari, A.; Hadi, Y.B. Patients with idiopathic pulmonary fibrosis have poor clinical outcomes with COVID-19 disease: A propensity matched multicentre research network analysis. BMJ Open Respir. Res. 2021, 8, e000969. [Google Scholar] [CrossRef] [PubMed]
- Drake, T.M.; Docherty, A.B.; Harrison, E.M.; Quint, J.K.; Adamali, H.; Agnew, S.; Babu, S.; Barber, C.M.; Barratt, S.; Bendstrup, E.; et al. Outcome of Hospitalization for COVID-19 in Patients with Interstitial Lung Disease. An International Multicenter Study. Am. J. Respir. Crit. Care Med. 2020, 202, 1656–1665. [Google Scholar] [CrossRef]
- Esposito, A.J.; Menon, A.A.; Ghosh, A.J.; Putman, R.K.; Fredenburgh, L.E.; El-Chemaly, S.Y.; Goldberg, H.J.; Baron, R.M.; Hunninghake, G.M.; Doyle, T.J. Increased Odds of Death for Patients with Interstitial Lung Disease and COVID-19: A Case–Control Study. Am. J. Respir. Crit. Care Med. 2020, 202, 1710–1713. [Google Scholar] [CrossRef]
- Gallay, L.; Uzunhan, Y.; Borie, R.; Lazor, R.; Rigaud, P.; Marchand-Adam, S.; Hirschi, S.; Israel-Biet, D.; Valentin, V.; Cottin, V. Risk Factors for Mortality after COVID-19 in Patients with Preexisting Interstitial Lung Disease. Am. J. Respir. Crit. Care Med. 2021, 203, 245–249. [Google Scholar] [CrossRef]
- RECOVERY Collaborative Group; Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; et al. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, C.H.; Lee, J. Coronavirus disease 2019 pneumonia may present as an acute exacerbation of idiopathic pulmonary fibrosis. J. Thorac. Dis. 2020, 12, 3902–3904. [Google Scholar] [CrossRef]
- Kitayama, T.; Kitamura, H.; Hagiwara, E.; Higa, K.; Okabayashi, H.; Oda, T.; Baba, T.; Komatsu, S.; Iwasawa, T.; Ogura, T. COVID-19 Pneumonia Resembling an Acute Exacerbation of Interstitial Pneumonia. Intern. Med. 2020, 59, 3207–3211. [Google Scholar] [CrossRef]
- Kondoh, Y.; Kataoka, K.; Ando, M.; Awaya, Y.; Ichikado, K.; Kataoka, M.; Komase, Y.; Mineshita, M.; Ohno, Y.; Okamoto, H.; et al. COVID-19 and acute exacerbation of interstitial lung disease. Respir. Investig. 2021, 59, 675–678. [Google Scholar] [CrossRef]
- Omote, N.; Kanemitsu, Y.; Inoue, T.; Yonezawa, T.; Ichihashi, T.; Shindo, Y.; Sakamoto, K.; Ando, A.; Suzuki, A.; Niimi, A.; et al. Successful treatment with high-dose steroids for acute exacerbation of idiopathic pulmonary fibrosis triggered by COVID-19: A case report. Intern. Med. 2021; online ahead of print. [Google Scholar] [CrossRef]
- Arai, T.; Tachibana, K.; Sugimoto, C.; Inoue, Y.; Tokura, S.; Okuma, T.; Akira, M.; Kitaichi, M.; Hayashi, S.; Inoue, Y. High-dose prednisolone after intravenous methyl prednisolone improves prognosis of acute exacerbation in idiopathic interstitial pneumonias. Respirology 2017, 22, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Collard, H.R.; Ryerson, C.J.; Corte, T.J.; Jenkins, G.; Kondoh, Y.; Lederer, D.J.; Lee, J.S.; Maher, T.M.; Wells, A.U.; Antoniou, K.M.; et al. Acute exacerbation of idiopathic pulmonary fibrosis. An international working group report. Am. J. Respir. Crit. Care Med. 2016, 194, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Travis, W.D.; Costabel, U.; Hansell, D.M.; King, T.E., Jr.; Lynch, D.A.; Nicholson, A.G.; Ryerson, C.J.; Ryu, J.H.; Selman, M.; Wells, A.U.; et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 2013, 188, 733–748. [Google Scholar] [CrossRef] [PubMed]
- Raghu, G.; Remy-Jardin, M.; Myers, J.L.; Richeldi, L.; Ryerson, C.J.; Lederer, D.J.; Behr, J.; Cottin, V.; Danoff, S.K.; Morell, F.; et al. Diagnosis of Idiopathic Pulmonary Fibrosis. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2018, 198, e44–e68. [Google Scholar] [CrossRef]
- Arnett, F.C.; Edworthy, S.M.; Bloch, D.A.; Mcshane, D.J.; Fries, J.F.; Cooper, N.S.; Healey, L.A.; Kaplan, S.R.; Liang, M.H.; Luthra, H.S.; et al. The american rheumatism association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31, 315–324. [Google Scholar] [CrossRef]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef]
- Bohan, A.; Peter, J.B. Polymyositis and dermatomyositis (first of two parts). N. Engl. J. Med. 1975, 292, 344–347. [Google Scholar] [CrossRef]
- Clinical Management of Patients with COVID-19. A Guide for Front-Line Health Care Workers, 5th ed.; Japanese Ministry of Health, Labour and Welfare: Tokyo, Japan, 2021. Available online: https://www.mhlw.go.jp/content/000785119.pdf (accessed on 8 July 2021). (In Japanese)
- Grein, J.; Ohmagari, N.; Shin, D.; Diaz, G.; Asperges, E.; Castagna, A.; Feldt, T.; Green, G.; Green, M.L.; Lescure, F.X.; et al. Compassionate Use of Remdesivir for Patients with Severe COVID-19. N. Engl. J. Med. 2020, 382, 2327–2336. [Google Scholar] [CrossRef]
- Kalil, A.C.; Patterson, T.F.; Mehta, A.K.; Tomashek, K.M.; Wolfe, C.R.; Ghazaryan, V.; Marconi, V.C.; Ruiz-Palacios, G.M.; Hsieh, L.; Kline, S.; et al. Baricitinib plus Remdesivir for Hospitalized Adults with COVID-19. N. Engl. J. Med. 2021, 384, 795–807. [Google Scholar] [CrossRef]
- National Institute of Infectious Diseases. New Mutant Strain of New Coronavirus (SARS-CoV-2), Which Is Concerned about Increased Infectivity/Transmission and Changes in Antigenicity (6th Report). Published on 15 February 2021. Available online: https://www.niid.go.jp/niid/ja/2019-ncov/10169-covid19-35.html (accessed on 11 June 2022). (In Japanese).
- National Institute of Infectious Diseases. New Mutant Strain of New Coronavirus (SARS-CoV-2), Which Is Concerned about Increased Infectivity/Transmission and Changes in Antigenicity (8th Report). Published on 7 April 2021. Available online: https://www.niid.go.jp/niid/ja/2019-ncov/2484-idsc/10280-covid19-41.html (accessed on 11 June 2022). (In Japanese).
- National Institute of Infectious Diseases. New Mutant Strain of New Coronavirus (SARS-CoV-2), Which Is Concerned about Increased Infectivity/Transmission and Changes in Antigenicity (9th Report). Published on 14 June 2021. Available online: https://www.niid.go.jp/niid/ja/2019-ncov/2484-idsc/10434-covid19-43.html (accessed on 11 June 2022). (In Japanese).
- National Institute of Infectious Diseases. New Mutant Strain of New Coronavirus (SARS-CoV-2), Which Is Concerned about Increased Infectivity/Transmission and Changes in Antigenicity (13th Report). Published on 28 April 2021. Available online: https://www.niid.go.jp/niid/ja/2019-ncov/2484-idsc/10623-covid19-57.html (accessed on 11 June 2022). (In Japanese).
- Ishikawa, N.; Hattori, N.; Yokoyama, A.; Kohno, N. Utility of KL-6/MUC1 in the clinical management of interstitial lung diseases. Respir. Investig. 2012, 50, 3–13. [Google Scholar] [CrossRef]
- Beltramo, G.; Cottenet, J.; Mariet, A.-S.; Georges, M.; Piroth, L.; Tubert-Bitter, P.; Bonniaud, P.; Quantin, C. Chronic respiratory diseases are predictors of severe outcome in COVID-19 hospitalised patients: A nationwide study. Eur. Respir. J. 2021, 58, 2004474. [Google Scholar] [CrossRef]
- Lin, H.X.J.; Cho, S.; Aravamudan, V.M.; Sanda, H.Y.; Palraj, R.; Molton, J.S.; Venkatachalam, I. Remdesivir in Coronavirus Disease 2019 (COVID-19) treatment: A review of evidence. Infection 2021, 49, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Yamada, T.; Kataoka, S.; Arai, Y.; Miura, K.; Ochi, Y.; Ihara, H.; Koyama, R.; Sasaki, S.; Takahashi, K. Prognostic differences among patients with idiopathic interstitial pneumonias with acute exacerbation of varying pathogenesis: A retrospective study. Respir. Res. 2019, 20, 287. [Google Scholar] [CrossRef] [PubMed]
- Yokomichi, H.; Mochizuki, M.; Lee, J.J.; Kojima, R.; Yokoyama, T.; Yamagata, Z. Incidence of hospitalization for severe complications of influenza virus infection in Japanese patients between 2012 and 2016: A cross-sectional study using routinely collected administrative data. BMJ Open 2019, 9, e024687. [Google Scholar] [CrossRef] [PubMed]
- McGonagle, D.; Bridgewood, C.; Meaney, J.F.M. A tricompartmental model of lung oxygenation disruption to explain pulmonary and systemic pathology in severe COVID-19. Lancet Respir. Med. 2021, 9, 665–672. [Google Scholar] [CrossRef]
- Arai, T.; Matsuoka, H.; Hirose, M.; Kida, H.; Yamamoto, S.; Ogata, Y.; Mori, M.; Hatsuda, K.; Sugimoto, C.; Tachibana, K.; et al. Prognostic significance of serum cytokines during acute exacerbation of idiopathic interstitial pneumonias treated with thrombomodulin. BMJ Open Respir. Res. 2021, 8, e000889. [Google Scholar] [CrossRef]
- Sugiyama, M.; Kinoshita, N.; Ide, S.; Nomoto, H.; Nakamoto, T.; Saito, S.; Ishikane, M.; Kutsuna, S.; Hayakawa, K.; Hashimoto, M.; et al. Serum CCL17 level becomes a predictive marker to distinguish between mild/moderate and severe/critical disease in patients with COVID-19. Gene 2021, 766, 145145. [Google Scholar] [CrossRef]
- Zhao, Y.; Qin, L.; Zhang, P.; Li, K.; Liang, L.; Sun, J.; Xu, B.; Dai, Y.; Li, X.; Zhang, C.; et al. Longitudinal COVID-19 profiling associates IL-1RA and IL-10 with disease severity and RANTES with mild disease. J. Clin. Investig. 2020, 5, e139834. [Google Scholar] [CrossRef]
- Sakamoto, S.; Homma, S.; Miyamoto, A.; Kurosaki, A.; Fujii, T.; Yoshimura, K. Cyclosporin A in the Treatment of Acute Exacerbation of Idiopathic Pulmonary Fibrosis. Intern. Med. 2010, 49, 109–115. [Google Scholar] [CrossRef]
- Homma, S.; Sakamoto, S.; Kawabata, M.; Kishi, K.; Tsuboi, E.; Motoi, N.; Yoshimura, K. Cyclosporin Treatment in Steroid-resistant and Acutely Exacerbated Interstitial Pneumonia. Intern. Med. 2005, 44, 1144–1150. [Google Scholar] [CrossRef][Green Version]
- Galvez-Romero, J.L.; Palmeros-Rojas, O.; Real-Ramírez, F.A.; Sánchez-Romero, S.; Tome-Maxil, R.; Ramírez-Sandoval, M.P.; Olivos-Rodríguez, R.; Flores-Encarnación, S.E.; Cabrera-Estrada, A.A.; Ávila-Morales, J.; et al. Cyclosporine A plus low-dose steroid treatment in COVID-19 improves clinical outcomes in patients with moderate to severe disease: A pilot study. J. Intern. Med. 2021, 289, 906–920. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, M.; Summer, R.; Roman, J. Acute Exacerbation of Interstitial Lung Disease as a Sequela of COVID-19 Pneumonia. Am. J. Med. Sci. 2020, 361, 126–129. [Google Scholar] [CrossRef]
- Aronson, K.I.; Podolanczuk, A.J. Lungs after COVID-19: Evolving knowledge of post-COVID-19 international lung disease. Ann. Am. Thorac. Soc. 2021, 18, 773–779. [Google Scholar] [CrossRef]
- Myall, K.J.; Mukherjee, B.; Castanheira, A.M.; Lam, J.L.; Benedetti, G.; Mak, S.M.; Preston, R.; Thillai, M.; Dewar, A.; Molyneaux, P.L.; et al. Persistent post-COVID-19 interstitial lung disease. An observational study of corticosteroid treatment. Ann. Am. Thorac. Soc. 2021, 18, 799–806. [Google Scholar] [CrossRef] [PubMed]
- George, P.M.; Wells, A.U.; Jenkins, R.G. Pulmonary fibrosis and COVID-19: The potential role for anti-fibrotic therapy. Lancet Respir. Med. 2020, 8, 805–815. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, A.; Kondoh, Y.; Brown, K.K.; Johkoh, T.; Kataoka, K.; Fukuoka, J.; Kimura, T.; Matsuda, T.; Yokoyama, T.; Fukihara, J.; et al. Acute exacerbations of fibrotic interstitial lung diseases. Respirology 2020, 25, 525–534. [Google Scholar] [CrossRef]
- Oda, K.; Ishimoto, H.; Yamada, S.; Kushima, H.; Ishii, H.; Imanaga, T.; Harada, T.; Ishimatsu, Y.; Matsumoto, N.; Naito, K.; et al. Autopsy analysis in acute exacerbation of idiopathic pulmonary fibrosis. Respir. Res. 2014, 15, 109. [Google Scholar] [CrossRef] [PubMed]
- Bösmüller, H.; Matter, M.; Fend, F.; Tzankov, A. The pulmonary pathology of COVID-19. Virchows Arch. 2021, 478, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Churg, A.; Müller, N.L.; Silva, C.I.S.; Wright, J.L. Acute Exacerbation (Acute Lung Injury of Unknown Cause) in UIP and Other Forms of Fibrotic Interstitial Pneumonias. Am. J. Surg. Pathol. 2007, 31, 277–284. [Google Scholar] [CrossRef]
- Doglioni, C.; Ravaglia, C.; Chilosi, M.; Rossi, G.; Dubini, A.; Pedica, F.; Piciucchi, S.; Vizzuso, A.; Stella, F.; Maitan, S.; et al. COVID-19 Interstitial Pneumonia: Histological and Immunohistochemical Features on Cryobiopsies. Respiration 2021, 100, 488–498. [Google Scholar] [CrossRef]
- Pogatchnik, B.P.; Swenson, K.E.; Sharifi, H.; Bedi, H.; Berry, G.J.; Guo, H.H. Radiology–Pathology Correlation Demonstrating Organizing Pneumonia in a Patient Who Recovered from COVID-19. Am. J. Respir. Crit. Care Med. 2020, 202, 598–599. [Google Scholar] [CrossRef] [PubMed]
- Kory, P.; Kanne, J.P. SARS-CoV-2 organising pneumonia: ‘Has there been a widespread failure to identify and treat this prevalent condition in COVID-19?’. BMJ Open Respir. Res. 2020, 7, e000724. [Google Scholar] [CrossRef] [PubMed]
- Hatabu, H.; Hunninghake, G.M.; Richeldi, L.; Brown, K.K.; Wells, A.U.; Remy-Jardin, M.; Verschakelen, J.; Nicholson, A.G.; Beasley, M.B.; Christiani, D.C.; et al. Interstitial lung abnormalities detected incidentally on CT: A Position Paper from the Fleischner Society. Lancet Respir. Med. 2020, 8, 726–737. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Li, X.; Zhang, L.; Wan, S.; Zhang, L.; Zhou, F. SARS-CoV-2 Omicron variant: Recent progress and future perspectives. Signal Transduct. Target. Ther. 2022, 7, 14. [Google Scholar] [CrossRef] [PubMed]
- Trunfio, M.; Portesani, F.; Vicinanza, S.; Nespoli, P.; Traverso, F.; Cortese, G.; Bonora, S.; Calcagno, A.; Di Perri, G. Real life evidence of lower lung virulence in COVID-19 inpatients infected with SARS-CoV-2 Omicron variant compared to wild-type and delta SARS-CoV-2 pneumonia. Lung 2002, 200, 573–577. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).