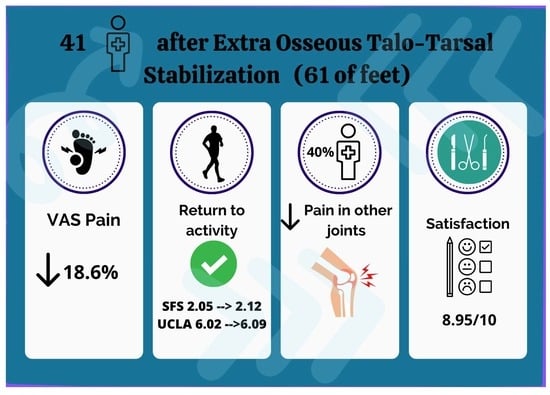
Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction
Abstract
1. Introduction
2. Materials and Methods
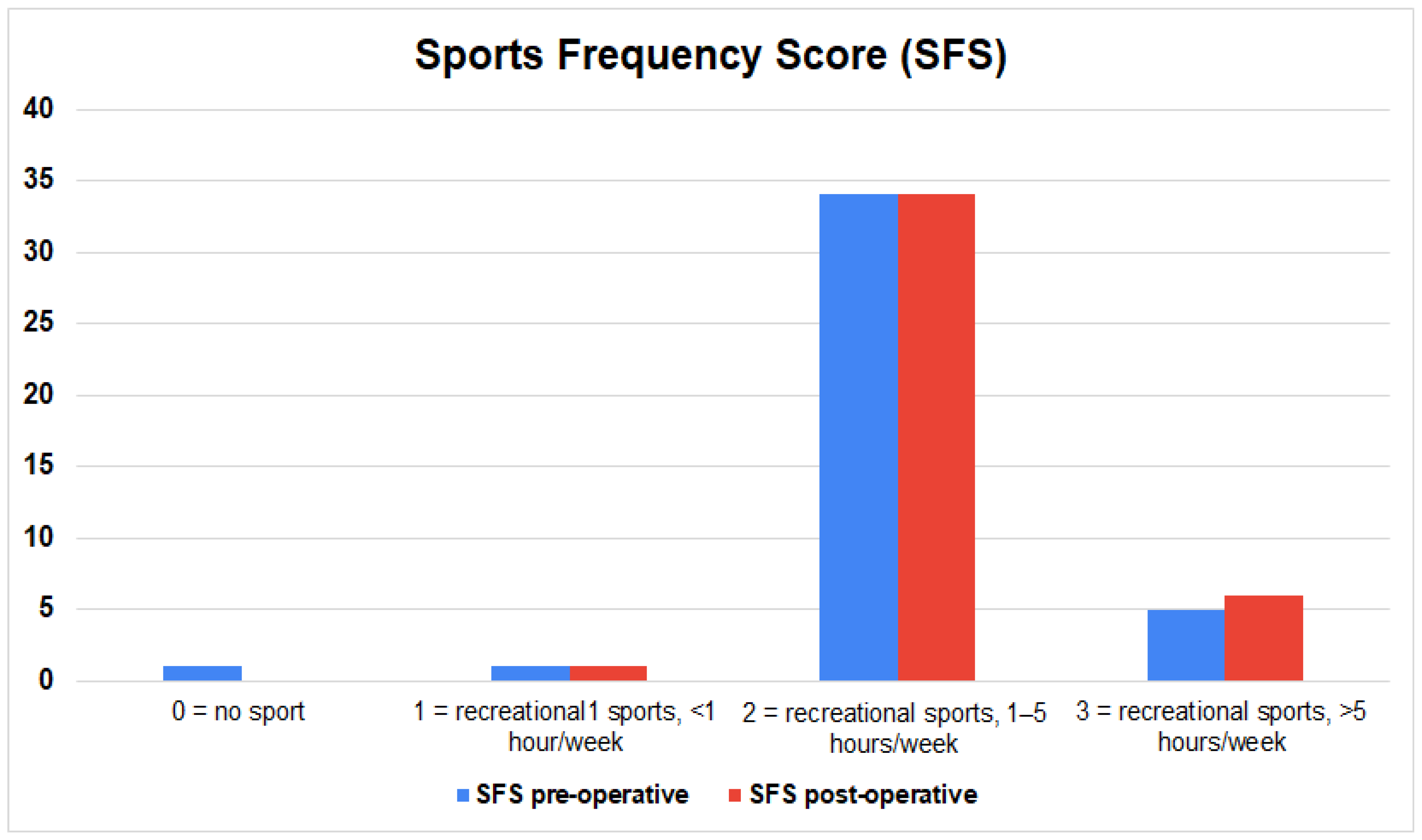
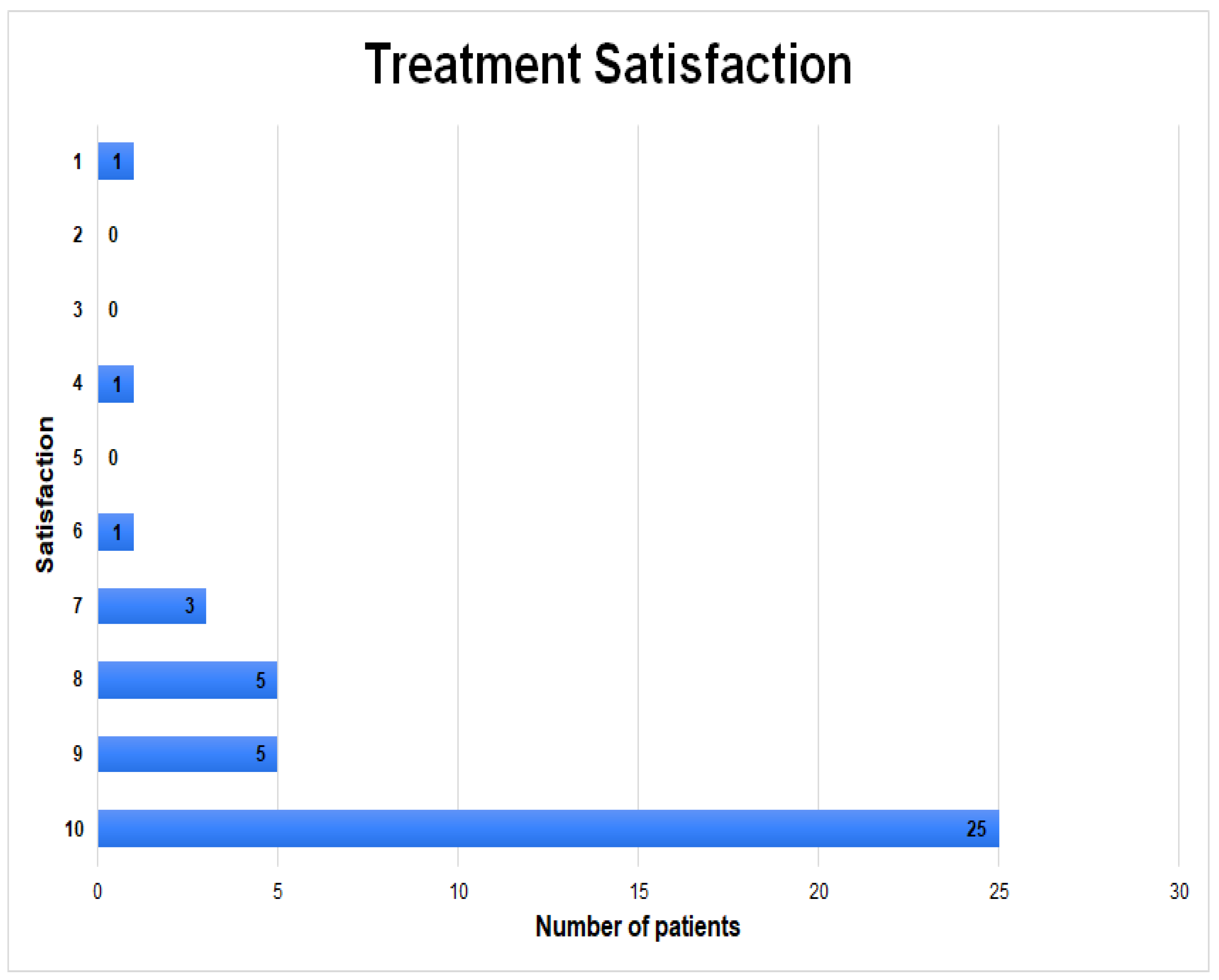
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huson, A. Biomechanics of the Tarsal Mechanism. A Key to the Function of the Normal Human Foot. J. Am. Podiatr. Med. Assoc. 2000, 90, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.E.; Jawrani, N.T.; Chikka, A. Extraosseous Talotarsal Stabilization Using HyProCure® in Adults: A 5-Year Retrospective Follow-Up. J. Foot Ankle Surg. 2012, 51, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.K.; Mak, A.F.; Evans, J.H. Biomedical Gait Evaluation of the Immediate Effect of Orthotic Treatment for Flexible Flat Foot. Prosthet. Orthot. Int. 1998, 22, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Blackwood, C.B.; Yuen, T.J.; Sangeorzan, B.J.; Ledoux, W.R. The Midtarsal Joint Locking Mechanism. Foot Ankle Int. 2005, 26, 1074–1080. [Google Scholar] [CrossRef]
- Biz, C.; Baldin, G.; Cappelletto, C.; Bragazzi, N.L.; Nicoletti, P.; Crimì, A.; Ruggieri, P. Isolated Medial Subtalar Joint Dislocation during Sports Activities: A Systematic Review of the Literature with Individual Participant Data Analysis. Osteology 2021, 1, 48–61. [Google Scholar] [CrossRef]
- Pereira, B.S.; Andrade, R.; Espregueira-Mendes, J.; Marano, R.P.C.; Oliva, X.M.; Karlsson, J. Current Concepts on Subtalar Instability. Orthop. J. Sports Med. 2021, 9, 23259671211021352. [Google Scholar] [CrossRef]
- Khamis, S.; Yizhar, Z. Effect of Feet Hyperpronation on Pelvic Alignment in a Standing Position. Gait Posture 2007, 25, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Giannini, S.; Catani, F.; Ceccarelli, F.; Girolami, M.; Benedetti, M.G. Kinematic and Isokinetic Evaluation of Patients with Flat Foot. Ital. J. Orthop. Traumatol. 1992, 18, 241–251. [Google Scholar]
- Inman, V.T. The Influence of the Foot-Ankle Complex on the Proximal Skeletal Structures. Artif. Limbs 1969, 13, 59–65. [Google Scholar]
- Kolodziej, L.; Summers, R.K.; Graham, M.E. The Effect of Extra-Osseous Talotarsal Stabilization (EOTTS) to Reduce Medial Knee Compartment Forces—An in Vivo Study. PLoS ONE 2019, 14, e0224694. [Google Scholar] [CrossRef]
- Saito, E.T.; Akashi, P.M.H.; de Camargo Neves Sacco, I. Global Body Posture Evaluation in Patients with Temporomandibular Joint Disorder. Clinics 2009, 64, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Gross, K.D.; Felson, D.T.; Niu, J.; Hunter, D.J.; Guermazi, A.; Roemer, F.W.; Dufour, A.B.; Gensure, R.H.; Hannan, M.T. Flat Feet Are Associated With Knee Pain and Cartilage Damage in Older Adults. Arthritis Care Res. 2011, 63, 937–944. [Google Scholar] [CrossRef]
- Tiberio, D. The Effect of Excessive Subtalar Joint Pronation on Patellofemoral Mechanics: A Theoretical Model. J. Orthop. Sports Phys. Ther. 1987, 9, 160–165. [Google Scholar] [CrossRef]
- Uden, H.; Scharfbillig, R.; Causby, R. The Typically Developing Paediatric Foot: How Flat Should It Be? A Systematic Review. J. Foot Ankle Res. 2017, 10, 37. [Google Scholar] [CrossRef]
- Stovitz, S.D.; Coetzee, J.C. Hyperpronation and Foot Pain: Steps toward Pain-Free Feet. Phys. Sportsmed. 2004, 32, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.E.; Jawrani, N.T.; Chikka, A.; Rogers, R.J. Surgical Treatment of Hyperpronation Using an Extraosseous Talotarsal Stabilization Device: Radiographic Outcomes in 70 Adult Patients. J. Foot Ankle Surg. 2012, 51, 548–555. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schon, L.C. Subtalar Arthroereisis: A New Exploration of an Old Concept. Foot Ankle Clin. 2007, 12, 329–339. [Google Scholar] [CrossRef]
- Viladot, R.; Pons, M.; Alvarez, F.; Omaña, J. Subtalar Arthroereisis for Posterior Tibial Tendon Dysfunction: A Preliminary Report. Foot Ankle Int. 2003, 24, 600–606. [Google Scholar] [CrossRef]
- Needleman, R.L. Current Topic Review: Subtalar Arthroereisis for the Correction of Flexible Flatfoot. Foot Ankle Int. 2005, 26, 336–346. [Google Scholar] [CrossRef]
- Graham, M.E.; Jawrani, N.T. Extraosseous Talotarsal Stabilization Devices: A New Classification System. J. Foot Ankle Surg. 2012, 51, 613–619. [Google Scholar] [CrossRef]
- Pagenstert, G.; Leumann, A.; Hintermann, B.; Valderrabano, V. Sports and Recreation Activity of Varus and Valgus Ankle Osteoarthritis before and after Realignment Surgery. Foot Ankle Int. 2008, 29, 985–993. [Google Scholar] [CrossRef]
- Steber, S.J. Analysis of Radiographic Outcomes Comparing Foot Orthosis to Extra-Osseous Talotarsal Stabilization in the Treatment of Recurrent Talotarsal Joint Dislocation. J. Minim. Invasive Orthop. 2015, 1, 1–11. [Google Scholar] [CrossRef]
- Martinelli, N.; Bianchi, A.; Martinkevich, P.; Sartorelli, E.; Romeo, G.; Bonifacini, C.; Malerba, F. Return to Sport Activities after Subtalar Arthroereisis for Correction of Pediatric Flexible Flatfoot. J. Pediatr. Orthop. B 2018, 27, 82. [Google Scholar] [CrossRef] [PubMed]
- Herdea, A.; Neculai, A.-G.; Ulici, A. The Role of Arthroereisis in Improving Sports Performance, Foot Aesthetics and Quality of Life in Children and Adolescents with Flexible Flatfoot. Children 2022, 9, 973. [Google Scholar] [CrossRef]
- Feng, P.; Li, J.; Ouyang, X.; Gao, F.; Zhang, H. Short-term effectiveness of hyprocure subtalar stabilization in treatment of adolescent flexible flatfoot. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2016, 30, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Jiang, J.; Fu, S.; Wang, C.; Su, Y.; Mei, G.; Xue, J.; Zou, J.; Li, X.; Shi, Z. HyProCure for Pediatric Flexible Flatfoot: What Affects the Outcome. Front. Pediatr. 2022, 10, 857458. [Google Scholar] [CrossRef]
- Kheyrandish, I.; Hadadnezhad, M.; Shojaedin, S.S. Comparison of Functional Lower Extremity Evaluation Scores in Active Adolescents with Normal and Flexible Flat Foot. Sci. J. Rehabil. Med. 2019, 7, 198–207. [Google Scholar] [CrossRef]
- Merkle, S.L.; Sluka, K.A.; Frey-Law, L.A. The Interaction between Pain and Movement. J. Hand Ther. 2020, 33, 60–66. [Google Scholar] [CrossRef]
- Fujita, T.; Hamai, S.; Shiomoto, K.; Okazawa, K.; Nasu, Y.; Hara, D.; Harada, S.; Motomura, G.; Ikemura, S.; Fujii, M.; et al. Analysis of Factors Influencing Patient Satisfaction after Total Hip Arthroplasty in a Japanese Cohort: The Significant Effect of Postoperative Physical Activity. J. Phys. Ther. Sci. 2022, 34, 76–84. [Google Scholar] [CrossRef]
- Ciechanowicz, D.; Kozłowski, J.; Kołodziej, Ł.; Kromuszczyńska, J. Return to Physical Activities after Scarf Osteotomy for Hallux Valgus. Ortop. Traumatol. Rehabil. 2020, 22, 95–106. [Google Scholar] [CrossRef]
- Martinelli, N.; Bianchi, A.; Prandoni, L.; Maiorano, E.; Sansone, V. Quality of Life in Young Adults after Flatfoot Surgery: A Case-Control Study. J. Clin. Med. 2021, 10, 451. [Google Scholar] [CrossRef] [PubMed]
- Fuller, R.M.; Eble, S.K.; Day, J.; Cororaton, A.D.; Rajan, L.; Deland, J.T.; Kumar, P.; Ellis, S.J. Return to Physical Activity Following Flatfoot Reconstruction. Foot Ankle Int. 2022, 43, 772–782. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; Riskowski, J.; Hannan, M.T. Musculoskeletal Conditions of the Foot and Ankle: Assessments and Treatment Options. Best Pract. Res. Clin. Rheumatol. 2012, 26, 345–368. [Google Scholar] [CrossRef]
- Gross, K.D.; Niu, J.; Zhang, Y.Q.; Felson, D.T.; McLennan, C.; Hannan, M.T.; Holt, K.G.; Hunter, D.J. Varus Foot Alignment and Hip Conditions in Older Adults. Arthritis Rheum. 2007, 56, 2993–2998. [Google Scholar] [CrossRef]
- Ålund, M. Subtalar Arthroereisis as a Surgical Option in the Reconstruction of Progressive Collapsing Foot Deformity: A Prospective 3-Year Follow-up Study on Patient Satisfaction and Causes for Implant Removal in 40 Cases Treated with the HyProCure Implant. J. Foot Ankle Surg. 2023, 10, 92–101. [Google Scholar] [CrossRef]
- Bresnahan, P.J.; Chariton, J.T.; Vedpathak, A. Extraosseous Talotarsal Stabilization Using HyProCure®: Preliminary Clinical Outcomes of a Prospective Case Series. J. Foot Ankle Surg. 2013, 52, 195–202. [Google Scholar] [CrossRef]


| Symptom-Related Ankle Activity Scale (SAAS) | Pre-Operative (n, %) | Post-Operative (n, %) |
|---|---|---|
| 0 = no ADL, disabled by ankle | 0 (0%) | 0 (0%) |
| 20 = symptoms with ADL, not disabled; sedentary work and walking on even ground possible | 1 (2.4%) | 0 (0%) |
| 40 = no symptoms with ADL; light work (e.g., nursing), swimming, walking on uneven ground possible | 3 (7.3%) | 3 (7.3%) |
| 60 = no symptoms with light work; moderate work (e.g., truck driving, heavy domestic work), recreational jogging, skiing, cycling possible | 17 (41.5%) | 6 (14.6%) |
| 80 = no symptoms with moderate work; strenuous work (e.g., building, forestry), jogging on uneven ground, competitive cycling, skiing possible | 11 (26.8%) | 14 (34.1%) |
| 100 = no symptoms with strenuous work, all recreational and competitive sports possible (e.g., soccer) | 9 (22.0%) | 18 (44.0%) |
| Pre-Operative | Post-Operative | p Value | |
|---|---|---|---|
| Number of physical activities [x/week], mean (SD) | 1.95 (±1.1) | 1.83 (±1.0) | 0.372 |
| Time of physical activity [min/week], mean (SD) | 153.7 (±126.3) | 170 (±102) | 0.145 |
| UCLA activity score, mean (SD) | 6.02 (±2.7) | 6.09 (±2.5) | 0.787 |
| SAAS, mean (SD) | 71.7 (±20.0) | 82.9 (±18.7) | 0.002 |
| LEFS, mean (SD) | 74.2 (±23.7) | 88.6 (±15.3) | 0.0006 |
| VAS, mean (SD) | 4.6 (±3.3) | 0.9 (±1.5) | <0.0001 |
| Physical Activity | Pre-Operative | Post-Operative | Change | Joint-Stress Activities |
|---|---|---|---|---|
| Walking | 19 | 19 | 0 | Low |
| Cycling | 17 | 17 | 0 | Low |
| Swimming | 7 | 7 | 0 | Low |
| Running | 6 | 6 | 0 | High |
| Weightlifting | 6 | 7 | +1 | High |
| Fitness | 6 | 4 | −2 | High |
| Nordic Walking | 4 | 4 | 0 | High |
| Skiing | 4 | 3 | −1 | High |
| Dance | 2 | 2 | 0 | High |
| Volleyball | 2 | 1 | −1 | High |
| Mountain trekking | 1 | 0 | −1 | High |
| Go-karts | 1 | 0 | −1 | Low |
| Canoeing | 1 | 0 | −1 | Low |
| Climbing | 1 | 1 | 0 | High |
| Martial arts | 1 | 1 | 0 | High |
| Squash | 1 | 1 | 0 | High |
| Time of Physical Activity [min/week], | Number of Physical Activities [x/week] | UCLA | SAAS | VAS | Satisfaction | LEFS | |
|---|---|---|---|---|---|---|---|
| MFS score | 0.2203 | 0.0981 | 0.0862 | 0.3241 | −0.4427 | 0.2552 | −0.1240 |
| p = 0.166 | p = 0.542 | p = 0.592 | p = 0.039 | p = 0.004 | p = 0.107 | p = 0.440 | |
| Pain | 0.2573 | 0.0287 | −0.1125 | 0.1418 | −0.5228 | 0.1284 | −0.1203 |
| p = 0.104 | p = 0.859 | p = 0.484 | p = 0.377 | p = 0.000 | p = 0.424 | p = 0.454 | |
| Distance walked | 0.2248 | 0.1687 | 0.0089 | 0.1581 | −0.0982 | 0.4231 | 0.0603 |
| p = 0.158 | p = 0.292 | p = 0.956 | p = 0.323 | p = 0.541 | p = 0.006 | p = 0.708 | |
| Stability | 0.0245 | 0.0096 | 0.1120 | 0.0520 | 0.0780 | −0.0532 | 0.1346 |
| p = 0.879 | p = 0.953 | p = 0.486 | p = 0.747 | p = 0.628 | p = 0.741 | p = 0.402 | |
| Support | -- | -- | -- | -- | -- | -- | -- |
| p = --- | p = --- | p = --- | p = --- | p = --- | p = --- | p = --- | |
| Limp | 0.2248 | 0.1687 | 0.0089 | 0.1581 | −0.0982 | 0.4231 | 0.0603 |
| p = 0.158 | p = 0.292 | p = 0.956 | p = 0.323 | p = 0.541 | p = 0.006 | p = 0.708 | |
| Shoes | 0.0137 | −0.0209 | 0.0995 | 0.3637 | −0.1795 | 0.1759 | −0.1324 |
| p = 0.932 | p = 0.897 | p = 0.536 | p = 0.019 | p = 0.261 | p = 0.271 | p = 0.409 | |
| Stairs | 0.1487 | 0.0305 | 0.3123 | 0.4492 | −0.0276 | 0.4996 | −0.0439 |
| p = 0.353 | p = 0.850 | p = 0.047 | p = 0.003 | p = 0.864 | p = 0.001 | p = 0.785 | |
| Terrain | −0.0404 | 0.1270 | 0.2367 | 0.1117 | −0.0921 | −0.1227 | −0.0233 |
| p = 0.802 | p = 0.429 | p = 0.136 | p = 0.487 | p = 0.567 | p = 0.445 | p = 0.885 | |
| Cosmesis | −0.1099 | 0.1178 | 0.1969 | −0.1458 | 0.0905 | −0.0042 | −0.1195 |
| p = 0.494 | p = 0.463 | p = 0.217 | p = 0.363 | p = 0.573 | p = 0.979 | p = 0.457 | |
| Motion | -- | -- | -- | -- | -- | -- | -- |
| p = --- | p = --- | p = --- | p = --- | p = --- | p = --- | p = --- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kołodziej, Ł.; Ciechanowicz, D.; Wójtowicz, M.; Król, M.; Szabałowska, M.; Kwiatkowski, S.; Szymczak, M.; Czajka, R. Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction. J. Clin. Med. 2023, 12, 4872. https://doi.org/10.3390/jcm12144872
Kołodziej Ł, Ciechanowicz D, Wójtowicz M, Król M, Szabałowska M, Kwiatkowski S, Szymczak M, Czajka R. Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction. Journal of Clinical Medicine. 2023; 12(14):4872. https://doi.org/10.3390/jcm12144872
Chicago/Turabian StyleKołodziej, Łukasz, Dawid Ciechanowicz, Maria Wójtowicz, Marta Król, Małgorzata Szabałowska, Sebastian Kwiatkowski, Mateusz Szymczak, and Radomir Czajka. 2023. "Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction" Journal of Clinical Medicine 12, no. 14: 4872. https://doi.org/10.3390/jcm12144872
APA StyleKołodziej, Ł., Ciechanowicz, D., Wójtowicz, M., Król, M., Szabałowska, M., Kwiatkowski, S., Szymczak, M., & Czajka, R. (2023). Prospective, Long-Term Functional Outcomes of Extra-Osseous Talotarsal Stabilization (EOTTS) Using HyProCure in Adult Patients with Talotarsal Joint Instability: Assessment of Physical Activity and Patient Satisfaction. Journal of Clinical Medicine, 12(14), 4872. https://doi.org/10.3390/jcm12144872