Effects of Robot-Assisted Activity Using a Communication Robot on Neurological Activity in Older Adults with and without Cognitive Decline
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Intervention
“This is Chapit. Chapit is a communication robot. Chapit will respond when you talk with Chapit. Let us talk with Chapit using words from the phrase list.”
2.3. Outcome Measures
2.4. Statistical Analyses
3. Results
4. Discussion
- Changing the content of the conversation to be more comprehensible for subjects with cognitive impairment.
- Create a conversation program for the communication robot around content that the cognitively impaired subjects remember well (past enjoyable events, daily routines, etc.).
- Physical contact with the robot (e.g., stroking, hugging) should be possible to provide more stimulation to the subject.
- Increasing the duration or frequency of interventions may improve or increase the effectiveness of RAA-CR.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef]
- Cerejeira, J.; Lagarto, L.; Mukaetova-Ladinska, E.B. Behavioral and psychological symptoms of dementia. Front. Neurol. 2012, 3, 73. [Google Scholar] [CrossRef] [PubMed]
- Okura, T.; Plassman, B.L.; Steffens, D.C.; Llewellyn, D.J.; Potter, G.G.; Langa, K.M. Neuropsychiatric symptoms and the risk of institutionalization and death: The aging, demographics, and memory study. J. Am. Geriatr. Soc. 2011, 59, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Hiyoshi-Taniguchi, K.; Becker, C.B.; Kinoshita, A. What behavioral and psychological symptoms of dementia affect caregiver burnout? Clin. Gerontol. 2018, 41, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Dyer, S.M.; Harrison, S.L.; Laver, K.; Whitehead, C.; Crotty, M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int. Psychogeriatr. 2018, 30, 295–309. [Google Scholar] [CrossRef]
- de Oliveira, A.M.; Radanovic, M.; de Mello, P.C.H.; Buchain, P.C.; Vizzotto, A.D.B.; Celestino, D.L.; Stella, F.; Piersol, C.V.; Forlenza, O.V. Nonpharmacological interventions to reduce behavioral and psychological symptoms of dementia: A systematic review. BioMed Res. Int. 2015, 2015, 218980. [Google Scholar] [CrossRef] [PubMed]
- Shibata, T.; Inoue, K.; Irie, R. Emotional robot for intelligent system-artificial emotional creature project. In Proceedings of the 5th IEEE International Workshop on Robot and Human Communication, RO-MAN’96, Tsukuba, Japan, 11–14 November 1996; pp. 466–471. [Google Scholar] [CrossRef]
- Shibata, T.; Wada, K. Robot therapy: A new approach for mental healthcare of the elderly—A mini-review. Gerontology 2011, 57, 378–386. [Google Scholar] [CrossRef]
- Jones, C.; Moyle, W.; Murfield, J.; Draper, B.; Shum, D.; Beattie, E.; Thalib, L. Does cognitive impairment and agitation in dementia influence intervention effectiveness? Findings from a cluster-randomized-controlled trial with the therapeutic robot, PARO. J. Am. Med. Dir. Assoc. 2018, 19, 623–626. [Google Scholar] [CrossRef]
- Moyle, W.; Jones, C.J.; Murfield, J.E.; Thalib, L.; Beattie, E.R.A.; Shum, D.K.H.; O’Dwyer, S.T.; Mervin, M.C.; Draper, B.M. Use of a robotic seal as a therapeutic tool to improve dementia symptoms: A cluster-randomized controlled trial. J. Am. Med. Dir. Assoc. 2017, 18, 766–773. [Google Scholar] [CrossRef]
- Valentí Soler, M.; Agüera-Ortiz, L.; Olazarán Rodríguez, J.; Mendoza Rebolledo, C.; Pérez Muñoz, A.; Rodríguez Pérez, I.; Osa Ruiz, E.; Barrios Sánchez, A.; Herrero Cano, V.; Carrasco Chillón, L.; et al. Social robots in advanced dementia. Front. Aging Neurosci. 2015, 7, 133. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J.; Mintzer, J.E. Time for change: The role of nonpharmacological interventions in treating behavior problems in nursing home residents with dementia. Alzheimer Dis. Assoc. Disord. 2005, 19, 37–40. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J.; Werner, P. Management of verbally disruptive behaviors in nursing home residents. J. Gerontol. A Biol. Sci. Med. Sci. 1997, 52, M369–M377. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Lou, V.W.; Tan, K.C.; Wai, M.Y.; Chan, L.L. Effects of a humanoid companion robot on dementia symptoms and caregiver distress for residents in long-term care. J. Am. Med. Dir. Assoc. 2020, 21, 1724–1728.e3. [Google Scholar] [CrossRef]
- Ke, C.; Lou, V.W.; Tan, K.C.; Wai, M.Y.; Chan, L.L. Changes in technology acceptance among older people with dementia: The role of social robot engagement. Int. J. Med. Inform. 2020, 141, 104241. [Google Scholar] [CrossRef]
- Obayashi, K.; Kodate, N.; Masuyama, S. Enhancing older people’s activity and participation with socially assistive robots: A multicentre quasi-experimental study using the ICF framework. Adv. Robot. 2018, 32, 1207–1216. [Google Scholar] [CrossRef]
- Obayashi, K.; Kodate, N.; Masuyama, S. Measuring the impact of age, gender and dementia on communication-robot interventions in residential care homes. Geriatr. Gerontol. Int. 2020, 20, 373–378. [Google Scholar] [CrossRef]
- Riches, S.; Azevedo, L.; Vora, A.; Kaleva, I.; Taylor, L.; Guan, P.; Jeyarajaguru, P.; McIntosh, H.; Petrou, C.; Pisani, S.; et al. Therapeutic engagement in robot-assisted psychological interventions: A systematic review. Clin. Psychol. Psychother. 2022, 29, 857–873. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.H.; Jeon, S.; Im, K.; Kwon, H.; Lee, B.H.; Kim, G.Y.; Jeong, H.; Han, N.E.; Seo, S.W.; Cho, H.; et al. Structural brain changes after traditional and robot-assisted multi-domain cognitive training in community-dwelling healthy elderly. PLoS ONE 2015, 10, e0123251. [Google Scholar] [CrossRef]
- Petersen, S.; Houston, S.; Qin, H.; Tague, C.; Studley, J. The utilization of robotic pets in dementia care. J. Alzheimer’s Dis. 2017, 55, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Goda, A.; Shimura, T.; Murata, S.; Kodama, T.; Nakano, H.; Ohsugi, H. Effects of robot-assisted activity using a communication robot in elderly individuals. Jpn. J. Health Promot. Phys. Ther. 2020, 10, 131–136. [Google Scholar] [CrossRef]
- Goda, A.; Shimura, T.; Murata, T.; Kodama, T.; Nakano, H.; Ohsugi, H. Psychological and neurophysiological effects of robot assisted activity in elderly people with cognitive decline. Gerontol. Geriatr. Med. 2020, 6, 2333721420969601. [Google Scholar] [CrossRef]
- Pascual-Marqui, R.D. Standardized low-resolution brain electromagnetic tomography (sLORETA): Technical details. Methods Find. Exp. Clin. Pharmacol. 2002, 24 (Suppl. D), 5–12. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Sugishita, M.; Hemmi, I.; Takeuchi, T. Reexamination of the validity and reliability of the Japanese version of the Mini-Mental State ExaminationM (MSE-J). Jpn. J. Cogn. Neurosci. 2016, 18, 168–183. [Google Scholar]
- Miyanaga, Y.; Takahashi, W.; Yoshizawa, S.A. Robust Speech Communication into Smart Info-Media System. IEICE Trans. Fundam. Electron. Commun. Comput. Sci. 2013, E96, 2074–2080. [Google Scholar] [CrossRef]
- Al-Qazzaz, N.K.; Sabir, M.K.; Ali, S.H.B.M.; Ahmad, S.A.; Grammer, K. Electroencephalogram Profiles for Emotion Identification over the Brain Regions Using Spectral, Entropy and Temporal Biomarkers. Sensors 2019, 20, 59. [Google Scholar] [CrossRef]
- Collins, D.L.; Holmes, C.J.; Peters, T.M.; Evans, A.C. Automatic 3-D model-based neuroanatomical segmentation. Hum. Brain Mapp. 1995, 3, 190–208. [Google Scholar] [CrossRef]
- Pascual-Marqui, R. Instantaneous and lagged measurements of linear and nonlinear dependence between groups of multivariate time series: Frequency decomposition. arXiv 2007, arXiv:0711.1455. [Google Scholar]
- Dauwels, J.; Vialatte, F.; Cichocki, A. Diagnosis of Alzheimer’s disease from EEG signals: Where are we standing? Curr. Alzheimer Res. 2010, 7, 487–505. [Google Scholar] [CrossRef]
- Raicher, I.; Takahashi, D.Y.; Kanda, P.A.M.; Nitrini, R.; Anghinah, R. qEEG spectral peak in Alzheimer’s disease: A possible tool for treatment follow-up. Dement. Neuropsychol. 2008, 2, 9–12. [Google Scholar] [CrossRef]
- Schmidt, M.T.; Kanda, P.A.; Basile, L.F.; da Silva Lopes, H.F.; Baratho, R.; Demario, J.L.; Jorge, M.S.; Nardi, A.E.; Machado, S.; Ianof, J.N.; et al. Index of alpha/theta ratio of the electroencephalogram: A new marker for Alzheimer’s disease. Front. Aging Neurosci. 2013, 5, 60. [Google Scholar] [CrossRef] [PubMed]
- Babiloni, C.; Triggiani, A.I.; Lizio, R.; Cordone, S.; Tattoli, G.; Bevilacqua, V.; Soricelli, A.; Ferri, R.; Nobili, F.; Gesualdo, L.; et al. Classification of single normal and Alzheimer’s disease individuals from cortical sources of resting state EEG rhythms. Front. Neurosci. 2016, 10, 47. [Google Scholar] [CrossRef] [PubMed]
- Mitsukura, Y.; Sumali, B.; Watanabe, H.; Ikaga, T.; Nishimura, T. Frontotemporal EEG as potential biomarker for early MCI: A case-control study. BMC Psychiatry 2022, 22, 289. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.C.; Baxter, L.C.; Wilder, L.S.; Pipe, J.G.; Heiserman, J.E.; Prigatano, G.P. Neural correlates of self-reflection. Brain 2002, 125, 1808–1814. [Google Scholar] [CrossRef] [PubMed]
- Newman, S.D.; Malaia, E.; Seo, R.; Cheng, H. The effect of individual differences in working memory capacity on sentence comprehension: An FMRI study. Brain Topogr. 2013, 26, 458–467. [Google Scholar] [CrossRef]
- Villain, N.; Desgranges, B.; Viader, F.; de la Sayette, V.; Mézenge, F.; Landeau, B.; Baron, J.C.; Eustache, F.; Chételat, G. Relationships between hippocampal atrophy, white matter disruption, and gray matter hypometabolism in Alzheimer’s disease. J. Neurosci. 2008, 28, 6174–6181. [Google Scholar] [CrossRef]
- Leech, R.; Sharp, D.J. The role of the posterior cingulate cortex in cognition and disease. Brain 2014, 137, 12–32. [Google Scholar] [CrossRef]
- Cavanna, A.E.; Trimble, M.R. The precuneus: A review of its functional anatomy and behavioural correlates. Brain 2006, 129, 564–583. [Google Scholar] [CrossRef]
- Wolpert, D.M.; Goodbody, S.J.; Husain, M. Maintaining internal representations: The role of the human superior parietal lobe. Nat. Neurosci. 1998, 1, 529–533. [Google Scholar] [CrossRef]
- Amodio, D.M.; Frith, C.D. Meeting of minds: The medial frontal cortex and social cognition. Nat. Rev. Neurosci. 2006, 7, 268–277. [Google Scholar] [CrossRef]
- Jeannerod, M. Neural simulation of action: A unifying mechanism for motor cognition. Neuroimage 2001, 14, S103–S109. [Google Scholar] [CrossRef]
- Scales, K.; Zimmerman, S.; Miller, S.J. Evidence-Based Nonpharmacological Practices to Address Behavioral and Psychological Symptoms of Dementia. Gerontologist 2018, 58, S88–S102. [Google Scholar] [CrossRef]
- Kempler, D.; Goral, M. Language and dementia: Neuropsychological aspects. Annu. Rev. Appl. Linguist. 2008, 28, 73–90. [Google Scholar] [CrossRef] [PubMed]
- Small, J.A.; Geldart, K.; Gutman, G. Communication between individuals with dementia and their caregivers during activities of daily living. Am. J. Alzheimer’s Dis. Other Demen. 2000, 15, 291–302. [Google Scholar] [CrossRef]
- Bora, E.; Walterfang, M.; Velakoulis, D. Theory of mind in behavioural-variant frontotemporal dementia and Alzheimer’s disease: A meta-analysis. J. Neurol. Neurosurg. Psychiatry 2015, 86, 714–719. [Google Scholar] [CrossRef]
- Ruffman, T.; Henry, J.D.; Livingstone, V.; Phillips, L.H. A meta-analytic review of emotion recognition and aging: Implications for neuropsychological models of aging. Neurosci. Biobehav. Rev. 2008, 32, 863–881. [Google Scholar] [CrossRef] [PubMed]
- Seeley, W.W. The Salience Network: A neural system for perceiving and responding to homeostatic demands. J. Neurosci. 2019, 39, 9878–9882. [Google Scholar] [CrossRef]
- Sheline, Y.I.; Raichle, M.E. Resting state functional connectivity in preclinical Alzheimer’s disease. Biol. Psychiatry 2013, 74, 340–347. [Google Scholar] [CrossRef]
| Variable | Cognitive Decline Group (n = 11) | Control Group (n = 18) | p-Value |
|---|---|---|---|
| Gender (male/female; n) | 7/4 | 5/13 | 0.12 |
| Age (year) | 79.00 (5.46) | 79.89 (7.92) | 0.75 |
| BMI (kg/m2) | 21.3 (3.36) | 23.40 (3.32) | 0.16 |
| MMSE (Score) | 17.82 (3.79) | 27.53 (2.37) | <0.01 |
| MNI Coordinates | |||
|---|---|---|---|
| Brain Region | BA | (x, y, z) | T-Value |
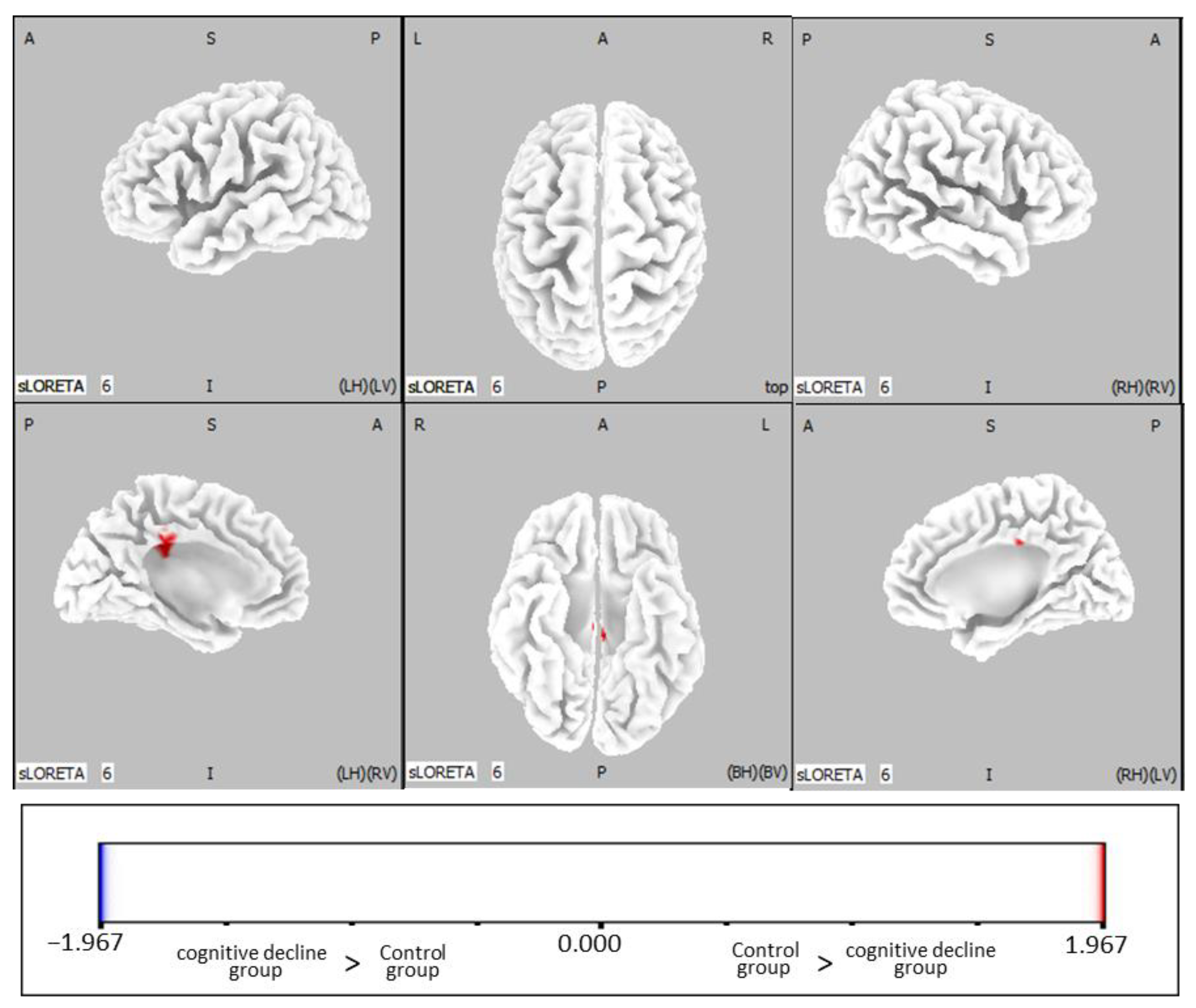
| Cingulate Gyrus | 23 1, 24 1, 31 1 | −10, −30, 40 | −2.05 |
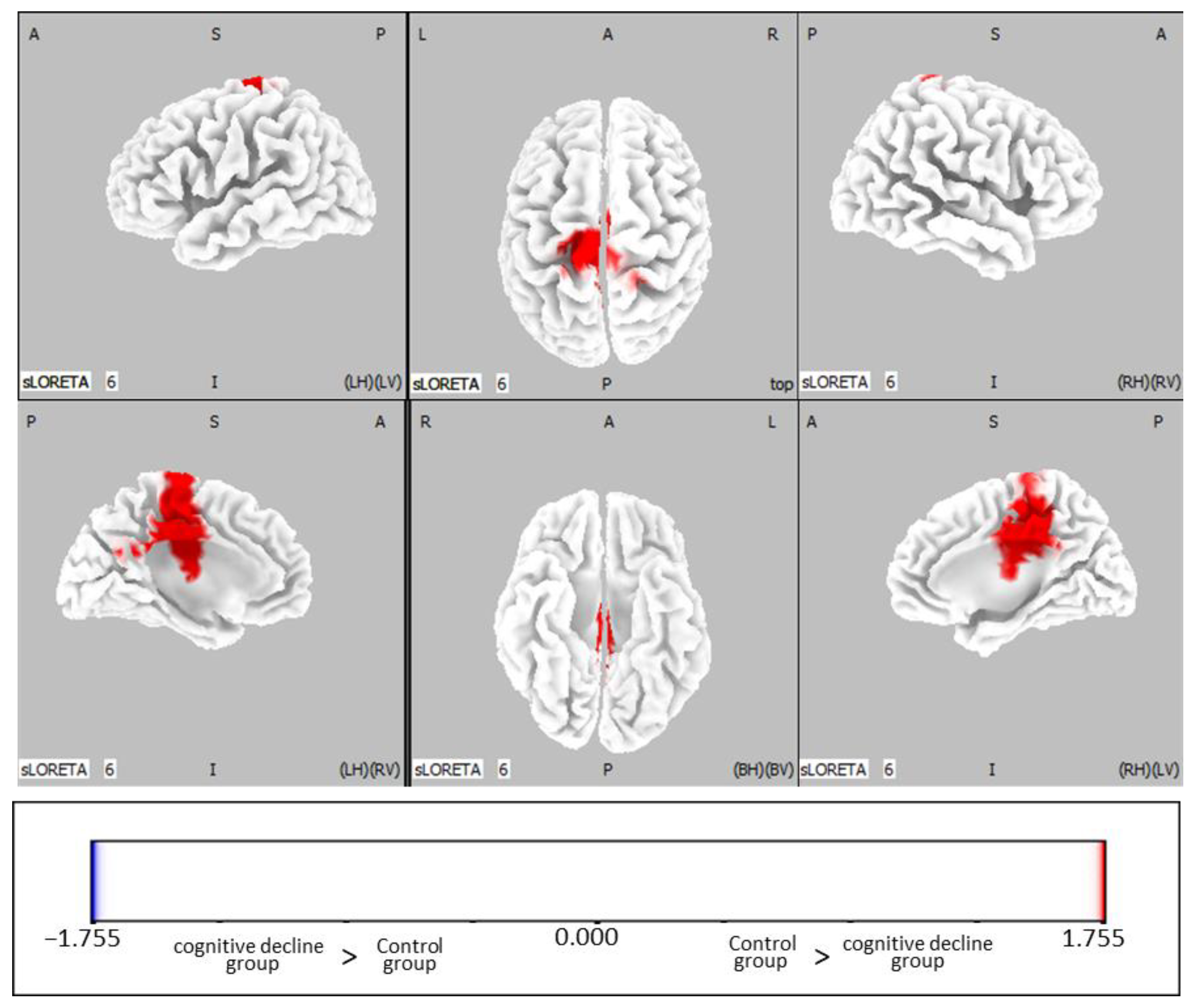
| MNI Coordinates | |||
|---|---|---|---|
| Brain Region | BA | (x, y, z) | T-Value |
| Cingulate gyrus | 23 1, 24 1, 31 1 | −5, −25, 50 | −1.85 |
| Precuneus | 7 1, 31 1 | −5, −25, 50 | −1.85 |
| Paracentral lobule | 4 1, 5 1, 6 1 | −5, −25, 55 | −1.84 |
| Medial frontal gyrus | 6 1 | −5, −25, 55 | −1.84 |
| Posterior cingulate | 23 1 | 0, −25, 35 | −1.82 |
| Precentral gyrus | 4 1 | −15, −30, 65 | −1.80 |
| Postcentral gyrus | 3 1 | −20, −30, 70 | −1.79 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goda, A.; Shimura, T.; Murata, S.; Kodama, T.; Nakano, H.; Ohsugi, H. Effects of Robot-Assisted Activity Using a Communication Robot on Neurological Activity in Older Adults with and without Cognitive Decline. J. Clin. Med. 2023, 12, 4818. https://doi.org/10.3390/jcm12144818
Goda A, Shimura T, Murata S, Kodama T, Nakano H, Ohsugi H. Effects of Robot-Assisted Activity Using a Communication Robot on Neurological Activity in Older Adults with and without Cognitive Decline. Journal of Clinical Medicine. 2023; 12(14):4818. https://doi.org/10.3390/jcm12144818
Chicago/Turabian StyleGoda, Akio, Takaki Shimura, Shin Murata, Takayuki Kodama, Hideki Nakano, and Hironori Ohsugi. 2023. "Effects of Robot-Assisted Activity Using a Communication Robot on Neurological Activity in Older Adults with and without Cognitive Decline" Journal of Clinical Medicine 12, no. 14: 4818. https://doi.org/10.3390/jcm12144818
APA StyleGoda, A., Shimura, T., Murata, S., Kodama, T., Nakano, H., & Ohsugi, H. (2023). Effects of Robot-Assisted Activity Using a Communication Robot on Neurological Activity in Older Adults with and without Cognitive Decline. Journal of Clinical Medicine, 12(14), 4818. https://doi.org/10.3390/jcm12144818






