Analgesic Modalities in Patients Undergoing Open Pancreatoduodenectomy—A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
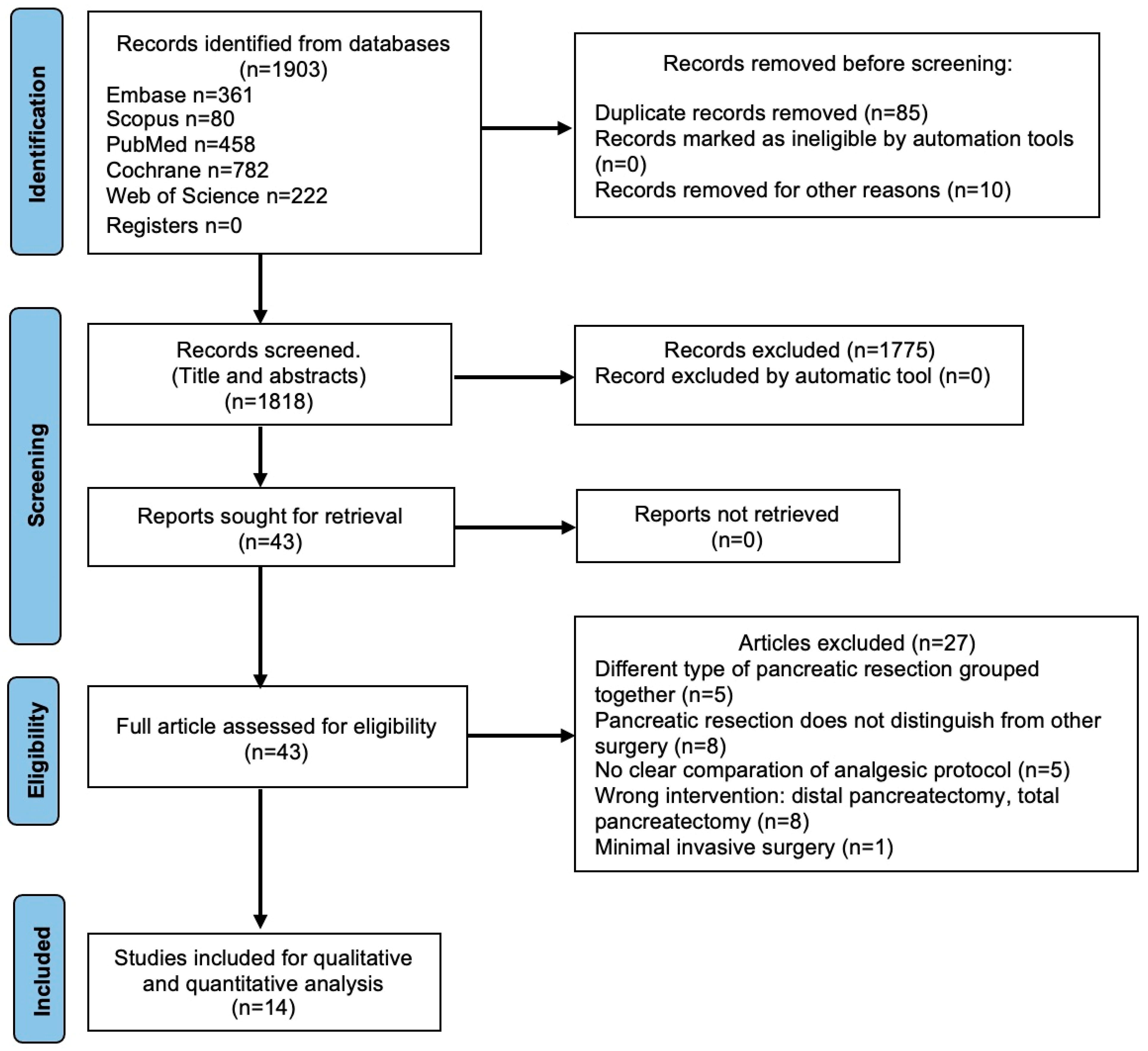
2. Material and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
2.3. Selection Process
2.4. Data Collection Process and Items
2.5. Primary and Secondary Outcomes Measurements
2.6. Study Quality Assessment
2.7. Statistical Analysis
3. Results
3.1. Study Characteristics
3.2. Risk of Bias Assessment
3.3. Primary Clinical Outcome
3.3.1. PCA versus EA
3.3.2. Regional Techniques versus EA
3.3.3. Sublingual Sufentanyl (SST) versus EA
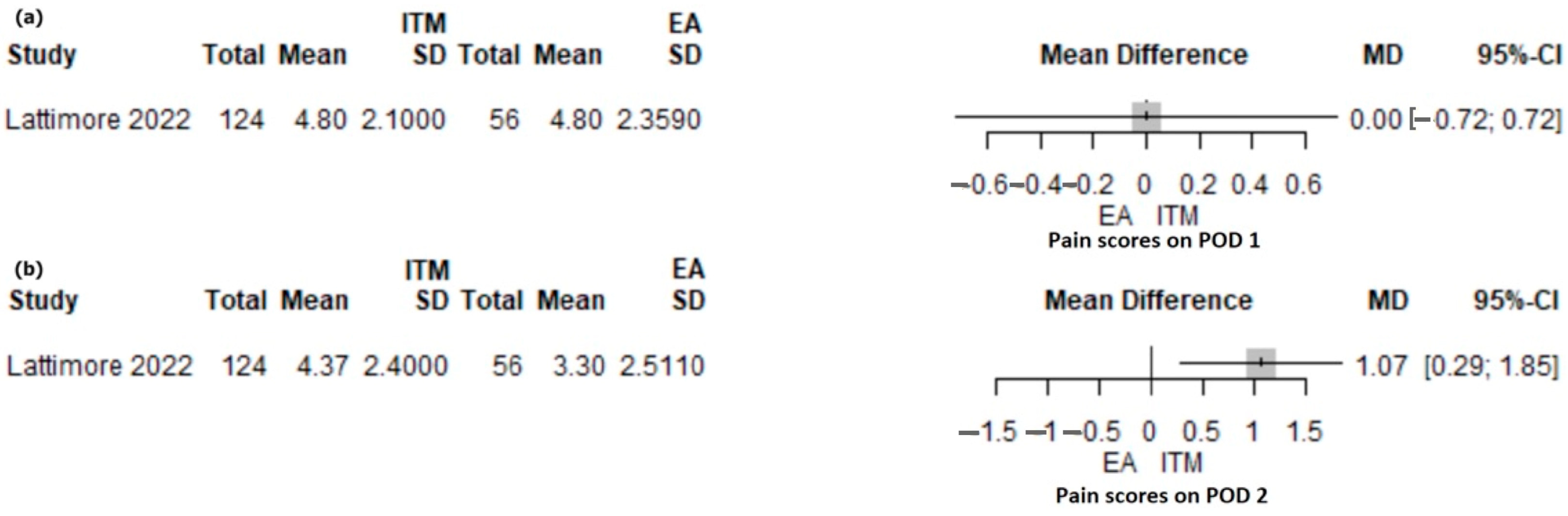
3.3.4. Intrathecal Morphine versus EA
3.3.5. PCA versus ITM Followed iv PCA (ITM-PCA) or versus ITM Followed iv PCA Plus Transversus Abdominis Block (ITM-TAP-PCA)
3.4. Secondary Clinical Outcomes
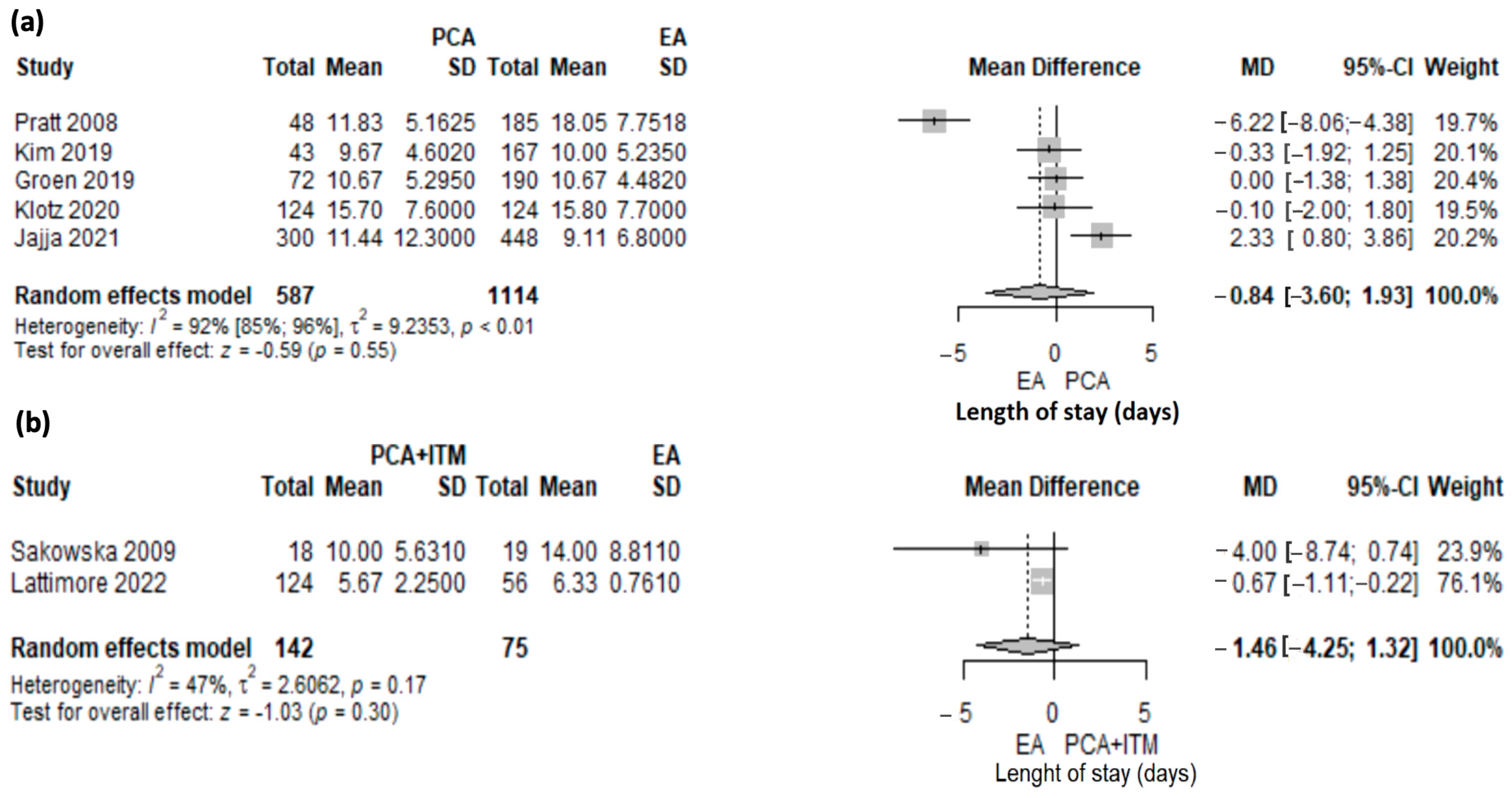
3.4.1. Duration of Hospital Stay
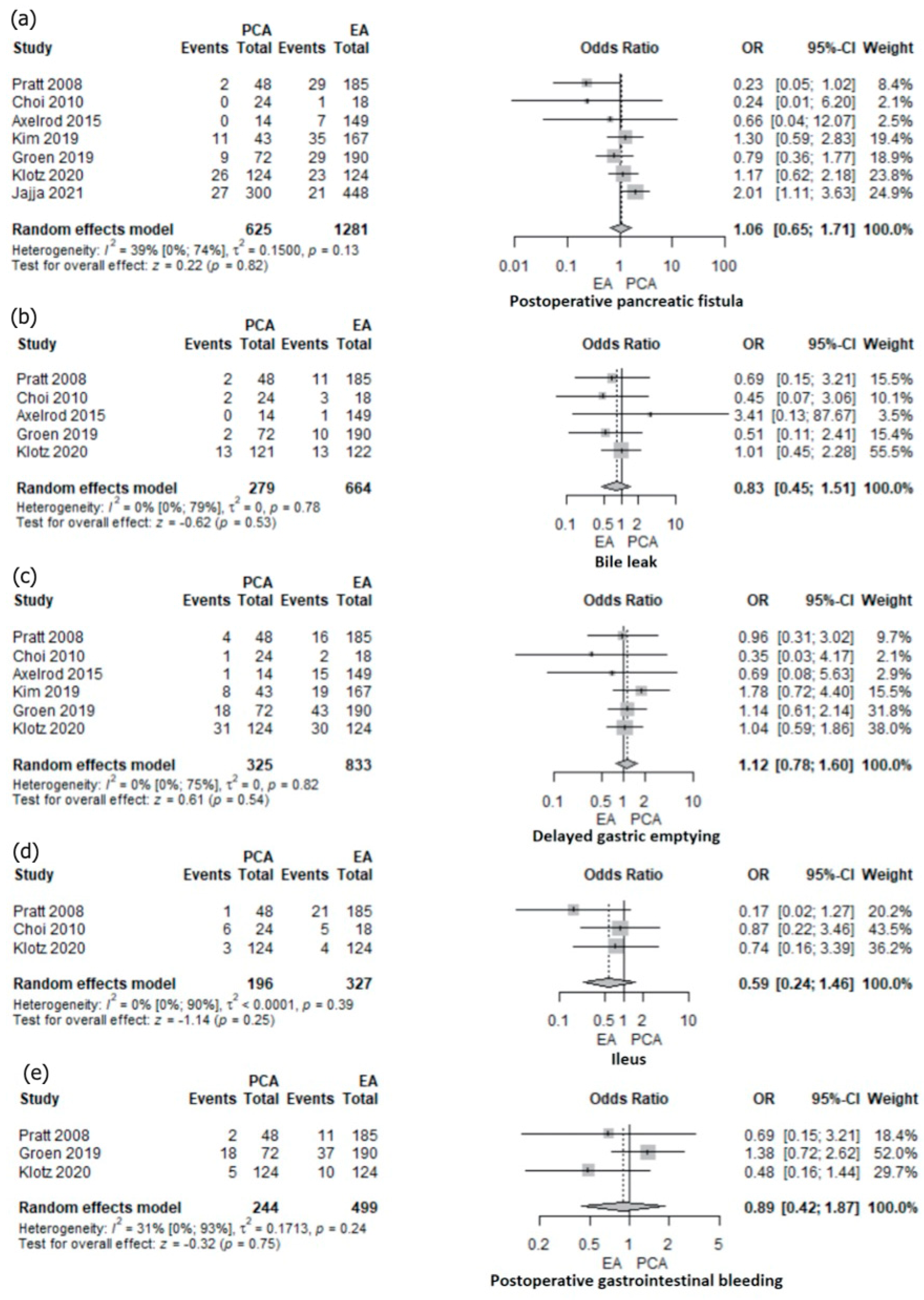
3.4.2. Specific Complications: Postoperative Pancreatic Fistula, Bile Leakage, Delayed Gastric Emptying, Ileus, and Gastrointestinal Bleeding
3.5. Risk of Bias across Studies
4. Discussions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aloia, T.A.; Kim, B.J.; Segraves-Chun, Y.S.; Cata, J.P.; Truty, M.J.; Shi, Q.; Holmes, A.; Soliz, J.M.; Popat, K.U.; Rahlfs, T.F.; et al. A Randomized Controlled Trial of Postoperative Thoracic Epidural Analgesia Versus Intravenous Patient-controlled Analgesia After Major Hepatopancreatobiliary Surgery. Ann. Surg. 2017, 266, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Newhook, T.E.; Dewhurst, W.L.; Vreeland, T.J.; Wang, X.; Soliz, J.; Speer, B.B.; Hancher-Hodges, S.; Feng, C.; Bruno, M.L.; Kim, M.P.; et al. Inpatient Opioid Use After Pancreatectomy: Opportunities for Reducing Initial Opioid Exposure in Cancer Surgery Patients. Ann. Surg. Oncol. 2019, 26, 3428–3435. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H.; Holte, K. Effect of postoperative analgesia on surgical outcome. Br. J. Anaesth. 2001, 87, 62–72. [Google Scholar] [CrossRef] [Green Version]
- Rawal, N. Current issues in postoperative pain management. Eur. J. Anaesthesiol. 2016, 33, 160–171. [Google Scholar] [CrossRef]
- Pirie, K.; Traer, E.; Finniss, D.; Myles, P.S.; Riedel, B. Current approaches to acute postoperative pain management after major abdominal surgery: A narrative review and future directions. Br. J. Anaesth. 2022, 129, 378–393. [Google Scholar] [CrossRef] [PubMed]
- Melloul, E.; Lassen, K.; Roulin, D.; Grass, F.; Perinel, J.; Adham, M.; Wellge, E.B.; Kunzler, F.; Besselink, M.G.; Asbun, H.; et al. Guidelines for perioperative care for pancreatoduodenectomy: Enhanced Recovery After Surgery (ERAS) Recommendations 2019. World J. Surg. 2020, 44, 2056–2084. [Google Scholar] [CrossRef]
- Rigg, J.R.; Jamrozik, K.; Myles, P.S.; Silbert, B.S.; Peyton, P.J.; Parsons, R.W.; Collins, K.S.; MASTER Anaethesia Trial Study Group. Epidural anaesthesia and analgesia and outcome of major surgery: A randomised trial. Lancet 2002, 359, 1276.e82. [Google Scholar] [CrossRef] [PubMed]
- Fotiadis, R.J.; Badvie, S.; Weston, M.D.; Allen-Mersh, T.G. Epidural analgesia in gastrointestinal surgery. Br. J. Surg. 2004, 91, 828.e841. [Google Scholar] [CrossRef]
- Simpson, R.E.; Fennerty, M.L.; Colgate, C.L.; Kilbane, E.M.; Ceppa, E.P.; House, M.G.; Zyromski, N.J.; Nakeeb, A.; Schmidt, C.M. Post-Pancreaticoduodenectomy Outcomes and Epidural Analgesia: A 5-year Single-Institution Experience. J. Am. Coll. Surg. 2019, 228, 453–462. [Google Scholar] [CrossRef]
- Jajja, M.R.; Williams, H.; Mahmooth, Z.; Nadeem, S.O.; Hashmi, S.S.; Sarmiento, J.M. Narcotic sparing postoperative analgesic strategies after pancreatoduodenectomy: Analysis of practice patterns for 1004 patients. HPB 2022, 24, 1145–1152. [Google Scholar] [CrossRef]
- Shi, W.Z.; Miao, Y.L.; Yakoob, M.Y.; Cao, J.B.; Zhang, H.; Jiang, Y.G.; Xu, L.H.; Mi, W.D. Recovery of gastrointestinal function with thoracic epidural vs. Systemic analgesia following gastrointestinal surgery. Acta Anaesthesiol. Scand. 2014, 58, 923.e32. [Google Scholar] [CrossRef] [PubMed]
- Salicath, J.H.; Yeoh, E.C.; Bennett, M.H. Epidural analgesia versus patient-controlled intravenous analgesia for pain following intra-abdominal surgery in adults. Cochrane Database Syst. Rev. 2018, 8, CD010434. [Google Scholar] [CrossRef] [PubMed]
- Guay, J.; Nishimori, M.; Kopp, S. Epidural local anaesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting and pain after abdominal surgery. Cochrane Database Syst. Rev. 2016, 7, CD001893. [Google Scholar] [CrossRef] [PubMed]
- Volk, T.; Wolf, A.; Van Aken, H.; Burkle, H.; Wiebalck, A.; Steinfeldt, T. Incidence of spinal haematoma after epidural puncture: Analysis from German network for safety in regional anaesthesia. Eur. J. Anaesthesiol. 2012, 29, 170–176. [Google Scholar] [CrossRef]
- Hermanides, J.; Hollmann, M.W.; Stevens, M.F.; Lirk, P. Failed epidural: Causes and management. Br. J. Anaesth. 2012, 109, 144.e54. [Google Scholar] [CrossRef] [Green Version]
- Pratt, W.B.; Steinbrook, R.A.; Maithel, S.K.; Vanounou, T.; Callery, M.P.; Vollmer, C.M., Jr. Epidural analgesia for pancreatoduodenectomy: A critical appraisal. J. Gastrointest. Surg. 2008, 12, 1207–1220. [Google Scholar] [CrossRef]
- Groen, J.V.; Slotboom, D.E.F.; Vuyk, J.; Martini, C.H.; Dahan, A.; Vahrmeijer, A.L.; Bonsing, B.A.; Mieog, J.S.D. Epidural and non-epidural analgesia in patients undergoing open pancreatectomy: A retrospective cohort study. J. Gastrointest. Surg. 2019, 23, 2439–2448. [Google Scholar] [CrossRef] [Green Version]
- Shah, D.R.; Brown, E.; Russo, J.E.; Li, C.S.; Martinez, S.R.; Coates, J.M.; Bold, R.J.; Canter, R.J. Negligible effect of perioperative epidural analgesia among patients undergoing elective gastric and pancreatic resections. J. Gastrointest. Surg. 2013, 17, 660–667. [Google Scholar] [CrossRef]
- Patel, A.; Stasiowska, M.; Waheed, U.; Brett, S.J.; Patel, P.B. Poor analgesic efficacy of epidural analgesia in critical care patients after pancreaticoduodenectomy. Pancreas 2014, 43, 373–379. [Google Scholar] [CrossRef]
- Choi, D.X.; Schoeniger, L.O. For patients undergoing pancreatoduodenectomy, epidural anesthesia and analgesia improves pain but increases rates of intensive care unit admissions and alterations in analgesics. Pancreas 2010, 39, 492–497. [Google Scholar] [CrossRef]
- Sugimoto, M.; Nesbit, L.; Barton, J.G.; Traverso, W.L. Epidural anesthesia dysfunction is associated with postoperative complications after pancreatectomy. J. Hepatobiliary Pancreat. Sci. 2016, 23, 102–109. [Google Scholar] [CrossRef]
- Axelrod, T.M.; Mendez, B.M.; Abood, G.J.; Sinacore, J.M.; Aranha, G.V.; Shoup, M. Perioperative epidural may not be the preferred form of analgesia in select patients undergoing pancreaticoduodenectomy. J. Surg. Oncol. 2015, 111, 306–310. [Google Scholar] [CrossRef]
- Marandola, M.; Cilli, T.; Alessandri, F.; Tellan, G.; Caronna, R.; Chirletti, P.; Delogu, G. Perioperative management in patients undergoing pancreatic surgery: The anesthesiologist’s point of view. Transpl. Proc. 2008, 40, 1195–1199. [Google Scholar] [CrossRef]
- Kim, S.S.; Niu, X.; Elliott, I.A.; Jiang, J.P.; Dann, A.M.; Damato, L.M.; Chung, H.; Girgis, M.D.; King, J.C.; Hines, O.J.; et al. Epidural analgesia improves postoperative pain control but impedes early discharge in patients undergoing pancreatic surgery. Pancreas 2019, 48, 719–725. [Google Scholar] [CrossRef]
- Pöpping, D.M.; Elia, N.; Van Aken, H.K.; Marret, E.; Schug, S.A.; Kranke, P.; Wenk, M.; Tramèr, M.R. Impact of epidural analgesia on mortality and morbidity after surgery: Systematic review and meta-analysis of randomize controlled trials. Ann. Surg. 2014, 259, 1056.e67. [Google Scholar] [CrossRef]
- Negrini, D.; Ihsan, M.; Freitas, K.; Pollazzon, C.; Graaf, J.; Andre, J.; Linhares, T.; Brandao, V.; Silva, G.; Fiorelli, R.; et al. The clinical impact of the perioperative epidural anesthesia on surgical outcomes after pancreaticoduodenectomy: A retrospective cohort study. Surg. Open. Sci. 2022, 10, 91–96. [Google Scholar] [CrossRef]
- Klotz, R.; Larmann, J.; Klose, C.; Bruckner, T.; Benner, L.; Doerr-Harim, C.; Tenckhoff, S.; Lock, J.F.; Brede, E.M.; Salvia, R.; et al. Gastrointestinal Complications After Pancreatoduodenectomy with Epidural vs. Patient-Controlled Intravenous Analgesia: A Randomized Clinical Trial. JAMA Surg. 2020, 155, e200794. [Google Scholar] [CrossRef]
- Hughes, M.J.; Ventham, N.T.; McNally, S.; Harrison, E.; Wigmore, S. Analgesia after open abdominal surgery in the setting of enhanced recovery surgery: A systematic review and meta-analysis. JAMA Surg. 2014, 149, 1224–1230. [Google Scholar] [CrossRef]
- Roughead, E.E.; Lim, R.; Ramsay, E.; Moffat, A.K.; Pratt, N.L. Persistence with opioids post discharge from hospitalisation for surgery in Australian adults: A retrospective cohort study. BMJ Open 2019, 9, e023990. [Google Scholar] [CrossRef] [Green Version]
- Grandhi, R.K.; Lee, S.; Abd-Elsayed, A. Does opioid use cause angiogenesis and metastasis? Pain Med. 2017, 18, 140.e51. [Google Scholar] [CrossRef] [Green Version]
- Ventham, N.T.; Hughes, M.; O’Neill, S.; Johns, N.; Brady, R.R.; Wigmore, S.J. Systematic review and meta-analysis of continuous local anaesthetic wound infiltration versus epidural analgesia for postoperative pain following abdominal surgery. Br. J. Surg. 2013, 100, 1280–1289. [Google Scholar] [CrossRef]
- Mungroop, T.H.; Bond, M.J.; Lirk, P.; Busch, O.R.; Hollmann, M.W.; Veelo, D.P.; Besselink, M.G. Preperitoneal or subcutaneous wound catheters as alternative for epidural analgesia in abdominal surgery: A systematic review and meta-analysis. Ann. Surg. 2019, 269, 252–260. [Google Scholar] [CrossRef]
- El-Boghdadly, K.; Madjdpour, C.; Chin, K.J. Thoracic paravertebral blocks in abdominal surgery—A systematic review of randomized controlled trials. Br. J. Anaesth. 2016, 117, 297–308. [Google Scholar] [CrossRef] [Green Version]
- Jackson, A.C.; Memory, K.; Issa, E.; Isherwood, J.; Graff-Baker, P.; Garcea, G. Retrospective observational study of patient outcomes with local wound infusion vs epidural analgesia after open hepato-pancreato-biliary surgery. BMC Anesthesiol. 2022, 22, 26. [Google Scholar] [CrossRef]
- Mungroop, T.H.; Veelo, D.P.; Busch, O.R.; van Dieren, S.; van Gulik, T.M.; Karsten, T.M.; de Castro, S.M.; Godfried, M.B.; Thiel, B.; Hollmann, M.W.; et al. Continuous wound infiltration versus epidural analgesia after hepato-pancreato-biliary surgery (POP-UP): A randomised controlled, open-label, non-inferiority trial. Lancet Gastroenterol. Hepatol. 2016, 1, 105–113. [Google Scholar] [CrossRef]
- Hutchins, J.L.; Grandelis, A.J.; Kaizer, A.M.; Jensen, E.H. Thoracic paravertebral block versus thoracic epidural analgesia for post-operative pain control in open pancreatic surgery: A randomized controlled trial. J. Clin. Anesth. 2018, 48, 41–45. [Google Scholar] [CrossRef]
- Perrin, J.; Ratnayake, B.; Wells, C.; Windsor, J.A.; Loveday, B.P.T.; MacLennan, N.; Lindsay, H.; Pandanaboyana, S. Epidural versus transabdominal wall catheters: A comparative study of outcomes after pancreatic resection. J. Surg. Res. 2021, 259, 473–479. [Google Scholar] [CrossRef]
- Koning, M.V.; Klimek, M.; Rijs, K.; Stolker, R.J.; Heesen, M.A. Intrathecal hydrophilic opioids for abdominal surgery: A meta-analysis, meta-regression, and trial sequential analysis. Br. J. Anaesth. 2020, 125, 358.e72. [Google Scholar] [CrossRef]
- Meylan, N.; Elia, N.; Lysakowski, C.; Tramer, M.R. Benefit and risk of intrathecal morphine without local anaesthetic in patients undergoing major surgery: Meta-analysis of randomized trials. Br. J. Anaesth. 2009, 102, 156–167. [Google Scholar] [CrossRef] [Green Version]
- Sakowska, M.; Docherty, E.; Linscott, D.; Connor, S. A change in practice from epidural to intrathecal morphine analgesia for hepato-pancreato-biliary surgery. World J. Surg. 2009, 33, 1802–1808. [Google Scholar] [CrossRef]
- Tang, J.Z.J.; Weinberg, L. A literature review of intrathecal morphine analgesia in patients undergoing major open hepato-pancreatic-biliary (HPB) surgery. Anesth. Pain Med. 2019, 9, e94441. [Google Scholar] [CrossRef] [Green Version]
- Dichtwald, S.; Ben-Haim, M.; Papismedov, L.; Hazan, S.; Cattan, A.; Matot, I. Intrathecal morphine versus intravenous opioid administration to impact postoperative analgesia in hepato-pancreatic surgery: A randomized controlled trial. J. Anesth. 2017, 31, 237–245. [Google Scholar] [CrossRef]
- Lattimore, C.M.; Kane, W.J.; Sarosiek, B.M.; Coleman, C.M.; Turrentine, F.E.; Forkin, K.T.; Bauer, T.W.; Adams, R.B.; Zaydfudim, V.M. Efficacy of opioid spinal analgesia for postoperative pain management after pancreatoduodenectomy. HPB 2022, 24, 1930–1936. [Google Scholar] [CrossRef]
- Burchard, P.R.; Melucci, A.D.; Lynch, O.; Loria, A.; Dave, Y.A.; Strawderman, M.; Schoeniger, L.O.; Galka, E.; Moalem, J.; Linehan, D.C. Intrathecal morphine and effect on opioid consumption and functional recovery after pancreaticoduodenectomy. J. Am. Coll. Surg. 2022, 235, 392–400. [Google Scholar] [CrossRef]
- Groen, J.V.; Boon, S.C.; Minderhoud, M.W.; Bonsing, B.A.; Martini, C.H.; Putter, H.; Vahrmeijer, A.L.; van Velzen, M.; Vuijk, J.; Mieog, J.S.D.; et al. Sublingual Sufentanil versus standard-of-care (patient-controlled analgesia with epidural Ropivacaine/Sufentanil or intravenous Morphine) for postoperative pain following pancreatoduodenectomy: A Randomized Trial. J. Pain Res. 2022, 15, 1775–1786. [Google Scholar] [CrossRef]
- Ringold, F.G.; Minkowitz, H.S.; Gan, T.J.; Aqua, K.A.; Chiang, Y.K.; Evashenk, M.A.; Palmer, P.P. Sufentanil sublingual tablet system for the management of postoperative pain following open abdominal surgery: A randomized, placebo-controlled study. Reg. Anesth. Pain Med. 2015, 40, 22–30. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Bijur, P.E.; Latimer, C.T.; Gallagher, E.J. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad. Emerg. Med. 2003, 10, 390–392. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid. Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef] [Green Version]
- Web Plot Digitizer. Available online: https://automeris.io/WebPlotDigitizer/ (accessed on 28 January 2023).
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Groen, J.V.; Khawar, A.A.J.; Bauer, P.A.; Bonsing, B.A.; Martini, C.H.; Mungroop, T.H.; Vahrmeijer, A.L.; Vuijk, J.; Dahan, A.; Mieog, J.S.D. Meta-analysis of epidural analgesia in patients undergoing pancreatoduodenectomy. BJS Open. 2019, 3, 559–571. [Google Scholar] [CrossRef]
- Akter, N.; Ratnayake, B.; Joh, D.B.; Chan, S.J.; Bonner, E.; Pandanaboyana, S. Postoperative Pain Relief after Pancreatic Resection: Systematic Review and Meta-Analysis of Analgesic Modalities. World J. Surg. 2021, 45, 3165–3173. [Google Scholar] [CrossRef]
- Kone, L.B.; Maker, V.K.; Banulescu, M.; Maker, A.V. Epidural analgesia is associated with prolonged length of stay after open HPB surgery in over 27,000 Patients. J. Gastrointest Surg. 2021, 25, 1716–1726. [Google Scholar] [CrossRef]
- Han, Y.; Dai, Y.; Shi, Y.; Zhang, X.; Xia, B.; Ji, Q.; Yu, X.; Bian, J.; Xu, T. Ultrasound-guided paravertebral blockade reduced perioperative opioids requirement in pancreatic resection: A randomized controlled trial. Front Surg. 2022, 9, 903441. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, K.L.; Chelly, J.E.; Lang, R.S.; Abuelkasem, E.; Geller, D.A.; Marsh, J.W.; Tsung, A.; Sakai, T. Epidural Versus Paravertebral Nerve Block for Postoperative Analgesia in Patients Undergoing Open Liver Resection: A randomized clinical trial. Reg. Anesth. Pain Med. 2016, 41, 460–468. [Google Scholar] [CrossRef]
- Spoto, M.R.; Zito, P.; Molinari, A.F.; Capretti, G.; Gavazzi, F.; Ridolfi, C.; Grimaldi, S.; Pesce, S.; Allavena, P.; Zerbi, A. A randomized clinical trial to compare the efficacy of continuous local anesthetic wound infusion with thoracic epidural analgesia in post-operative pain control after pancreatic surgery. Anaesth. Pain. Intensive Care 2015, 19, 429–436. [Google Scholar]

| Publication Year | Country | Recruitment Dates | Centers | Type of Pancreatic Resection | Analgesic Modalities Compared (n) | ||
|---|---|---|---|---|---|---|---|
| RCTs | |||||||
| Klotz et al. [27] | 2020 | Europe | 2015–2017 | 9 | PD | PCA (124) | EA (124) |
| Mungroop et al. [35] | 2016 | NL | 2015 | 2 | PD | CWI-PCA (18) | EA (18) |
| Hutchins et al. [36] | 2018 | USA | 2012–2015 | 1 | PD | TPVB (25) | EA (23) |
| Marandola et al. [23] | 2008 | Italy | 2002–2007 | 1 | PD | PCA (24) | EA (16) |
| Groen et al. [45] | 2022 | NL | 2018–2021 | 1 | PD | SST (10) | EA-PCEA (10) /PCA (1) |
| Cohort studies | |||||||
| Burchartd et al. [44] | 2022 | USA | 2014–2020 | 1 | PD | PCA (85) | PCA/ITM (115) PCA/ITM/TAP (33) |
| Lattimore et al. [43] | 2022 | USA | 2015–2020 | 1 | PD | ITM-PCA (124) | EA (58) |
| Jajja et al. [10] | 2021 | USA | 2010–2017 | 1 | PD | PCA (300) | EA (448) |
| Kim et al. ** [24] | 2019 | USA | 2013–2016 | 1 | PD | PCA (43) | EA (167) |
| Groen et al. * [17] | 2019 | NL | 2013–2017 | 1 | PD | PCA (59) | EA (154) |
| Axelrot et al. [22] | 2015 | USA | 2007–2011 | 1 | PD | PCA (14) | EA (149) |
| Shah et al. [18] | 2013 | USA | 2007–2011 | 1 | PD | PCA (15) | EA (87) |
| Choi et al. [20] | 2010 | USA | 2004–2007 | 1 | PD | PCA (24) | EA (18) |
| Sakowska et al. [40] | 2009 | NZ | 2005–2008 | 1 | PD | PCA-ITM (18) | EA (19) |
| Pratt et al. [16] | 2008 | USA | 2001–2007 | 1 | PD | PCA (48) | EA (185) |
| Randomization Process | Deviations from the Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall Risk of Bias | |
|---|---|---|---|---|---|---|
| Klotz et al. [27] 2020 | Low risk | Low risk | Low risk | Some concern | Low risk | Some concern |
| Mungroop et al. [35] 2016 | Low risk | Low risk | Low risk | Some concern | Low risk | Some concern |
| Marandola et al. [23] 2008 | High risk | High risk | Low risk | Some concern | Some concern | High risk |
| Groen et al. [45] 2022 | Low risk | Some concern | Low risk | Some concern | Low risk | Some concern |
| Hutchins et al. [36] 2018 | Low risk | Low risk | Low risk | Some concern | Some concern | Some concern |
| Bias Due to Confounding | Bias in Selection of Participants | Bias in Classification of Interventions | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of the Reported Result | Overall Bias | |
|---|---|---|---|---|---|---|---|---|
| Burchartd et al. [44] 2022 | moderate | low | low | low | low | moderate | moderate | moderate |
| Lattimore et al. [43] 2022 | moderate | low | low | low | low | moderate | moderate | moderate |
| Jajja et al. [10] 2021 | moderate | low | low | low | low | moderate | moderate | moderate |
| Kim et al. [24] 2019 | moderate | low | low | low | low | moderate | moderate | moderate |
| Groen et al. [17] 2019 | moderate | low | low | low | low | moderate | moderate | moderate |
| Axelrot et al. [22] 2015 | moderate | low | low | low | low | moderate | moderate | moderate |
| Shah et al. [18] 2013 | moderate | low | low | low | low | serious | moderate | serious |
| Choi et al. [20] 2010 | serious | low | low | low | low | serious | moderate | serious |
| Sakowska et al. [40] 2009 | moderate | low | low | low | low | low | moderate | moderate |
| Pratt et al. [16] 2008 | moderate | low | low | moderate | low | serious | moderate | serious |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mărgărit, S.; Bartoș, A.; Laza, L.; Osoian, C.; Turac, R.; Bondar, O.; Leucuța, D.-C.; Munteanu, L.; Vasian, H.N. Analgesic Modalities in Patients Undergoing Open Pancreatoduodenectomy—A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 4682. https://doi.org/10.3390/jcm12144682
Mărgărit S, Bartoș A, Laza L, Osoian C, Turac R, Bondar O, Leucuța D-C, Munteanu L, Vasian HN. Analgesic Modalities in Patients Undergoing Open Pancreatoduodenectomy—A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(14):4682. https://doi.org/10.3390/jcm12144682
Chicago/Turabian StyleMărgărit, Simona, Adrian Bartoș, Laura Laza, Cristiana Osoian, Robert Turac, Oszkar Bondar, Daniel-Corneliu Leucuța, Lidia Munteanu, and Horațiu Nicolae Vasian. 2023. "Analgesic Modalities in Patients Undergoing Open Pancreatoduodenectomy—A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 14: 4682. https://doi.org/10.3390/jcm12144682
APA StyleMărgărit, S., Bartoș, A., Laza, L., Osoian, C., Turac, R., Bondar, O., Leucuța, D.-C., Munteanu, L., & Vasian, H. N. (2023). Analgesic Modalities in Patients Undergoing Open Pancreatoduodenectomy—A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(14), 4682. https://doi.org/10.3390/jcm12144682





