Depressive Symptoms and Their Impact on Quality of Life in Parkinson’s Disease: An Exploratory Network Analysis Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Extracted Variables
2.3. Statistical Analyses
3. Results
3.1. Descriptive Analyses
3.2. Network Analyses
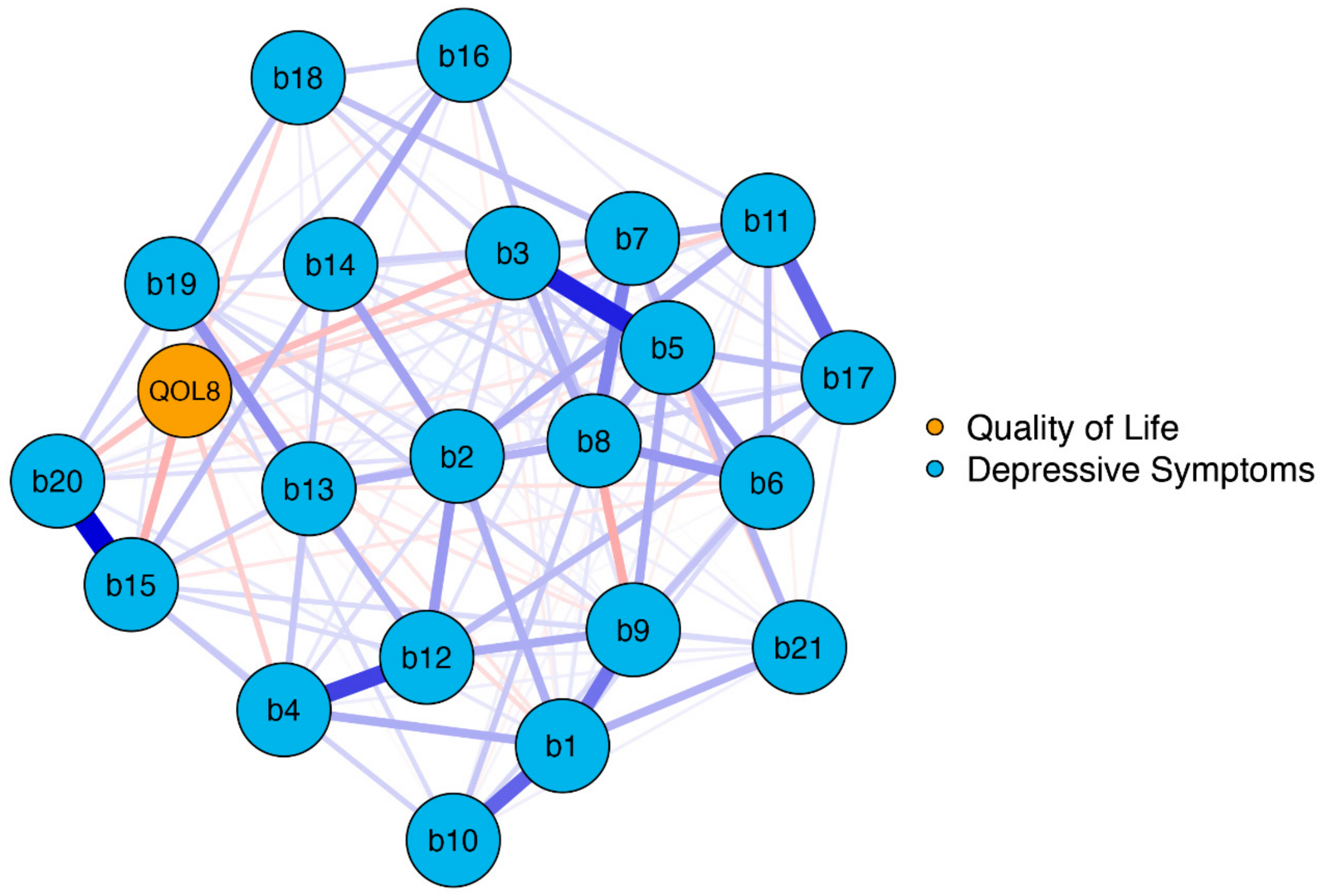
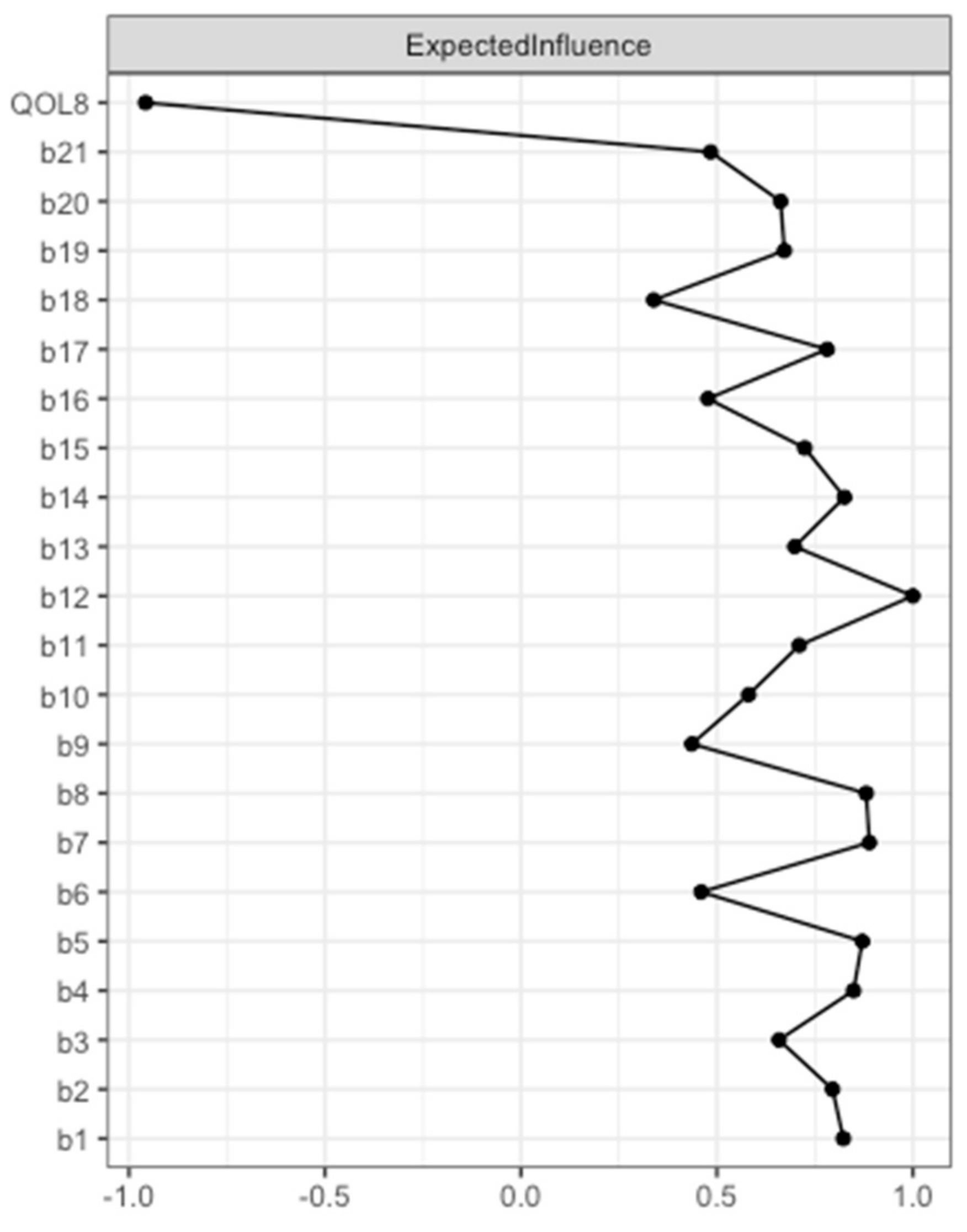
3.2.1. Network Model 1: Association between BDI-II Items and Overall QoL (EUROHIS-QOL 8-Item Index)
3.2.2. Network Model 2: Association between BDI-II Items and the Eight EUROHIS-QOL Items
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Titova, N.; Qamar, M.A.; Chaudhuri, K.R. The Nonmotor Features of Parkinson’s Disease. Int. Rev. Neurobiol. 2017, 132, 33–54. [Google Scholar] [CrossRef] [PubMed]
- Menon, B.; Nayar, R.; Kumar, S.; Cherkil, S.; Venkatachalam, A.; Surendran, K.; Deepak, K.S. Parkinson’s Disease, Depression, and Quality-of-Life. Indian J. Psychol. Med. 2015, 37, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Martin, P.; Rodriguez-Blazquez, C.; Kurtis, M.M.; Chaudhuri, K.R. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov. Disord. 2011, 26, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Bock, M.A.; Brown, E.G.; Zhang, L.; Tanner, C. Association of Motor and Nonmotor Symptoms With Health-Related Quality of Life in a Large Online Cohort of People With Parkinson Disease. Neurology 2022, 98, e2194–e2203. [Google Scholar] [CrossRef] [PubMed]
- Santos-García, D.; de la Fuente-Fernández, R. Impact of non-motor symptoms on health-related and perceived quality of life in Parkinson’s disease. J. Neurol. Sci. 2013, 332, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Meyers, A.R.; Gage, H.; Hendricks, A. Health-related quality of life in neurology. Arch. Neurol. 2000, 57, 1224–1227. [Google Scholar] [CrossRef]
- Schrag, A. Quality of life and depression in Parkinson’s disease. J. Neurol. Sci. 2006, 248, 151–157. [Google Scholar] [CrossRef]
- Tandberg, E.; Larsen, J.P.; Aarsland, D.; Cummings, J.L. The Occurrence of Depression in Parkinson’s Disease: A Community-Based Study. Arch. Neurol. 1996, 53, 175–179. [Google Scholar] [CrossRef]
- Reijnders, J.S.; Ehrt, U.; Weber, W.E.; Aarsland, D.; Leentjens, A.F. A systematic review of prevalence studies of depression in Parkinson’s disease. Mov. Disord. 2008, 23, 183–189; quiz 313. [Google Scholar] [CrossRef]
- Schönenberg, A.; Zipprich, H.M.; Teschner, U.; Grosskreutz, J.; Witte, O.W.; Prell, T. Impact of subthreshold depression on health-related quality of life in patients with Parkinson’s disease based on cognitive status. Health Qual. Life Outcomes 2021, 19, 107. [Google Scholar] [CrossRef]
- Bahadoran, P.; Varela, R.; De Angelis, A.; Paviour, D.; Agrawal, N. Screening for depression in movement disorders clinic. Neurol. Sci. 2021, 42, 969–978. [Google Scholar] [CrossRef] [PubMed]
- Goodarzi, Z.; Mrklas, K.J.; Roberts, D.J.; Jette, N.; Pringsheim, T.; Holroyd-Leduc, J. Detecting depression in Parkinson disease: A systematic review and meta-analysis. Neurology 2016, 87, 426–437. [Google Scholar] [CrossRef]
- Martinez-Martin, P.; Jeukens-Visser, M.; Lyons, K.E.; Rodriguez-Blazquez, C.; Selai, C.; Siderowf, A.; Welsh, M.; Poewe, W.; Rascol, O.; Sampaio, C.; et al. Health-related quality-of-life scales in Parkinson’s disease: Critique and recommendations. Mov. Disord. 2011, 26, 2371–2380. [Google Scholar] [CrossRef] [PubMed]
- Fried, E.I. Studying Mental Health Problems as Systems, Not Syndromes. Curr. Dir. Psychol. Sci. 2022, 31, 500–508. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Santos-García, D.; Mir, P.; Cubo, E.; Vela, L.; Rodríguez-Oroz, M.C.; Martí, M.J.; Arbelo, J.M.; Infante, J.; Kulisevsky, J.; Martínez-Martín, P.; et al. COPPADIS-2015 (COhort of Patients with PArkinson’s DIsease in Spain, 2015), a global--clinical evaluations, serum biomarkers, genetic studies and neuroimaging--prospective, multicenter, non-interventional, long-term study on Parkinson’s disease progression. BMC Neurol. 2016, 16, 26. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Brown, G.K. Manual for the Beck Depression Inventory-II; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Nosikov, A.; Gudex, C. Development of a common instrument for quality of life. EUROHIS Dev. Common Instrum. Health Surv. 2003, 57, 145. [Google Scholar]
- WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): Development and general psychometric properties. Soc. Sci. Med. 1998, 46, 1569–1585. [Google Scholar] [CrossRef]
- Schmidt, S.; Mühlan, H.; Power, M. The EUROHIS-QOL 8-item index: Psychometric results of a cross-cultural field study. Eur. J. Public. Health 2006, 16, 420–428. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef]
- Fahn, S.; Elton, R. Recent developments in Parkinson’s disease. Macmillan Health Care Inf. 1987, 2, 293–304. [Google Scholar]
- Chaudhuri, K.R.; Martinez-Martin, P.; Brown, R.G.; Sethi, K.; Stocchi, F.; Odin, P.; Ondo, W.; Abe, K.; Macphee, G.; Macmahon, D.; et al. The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: Results from an international pilot study. Mov. Disord. 2007, 22, 1901–1911. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Hevey, D. Network analysis: A brief overview and tutorial. Health Psychol. Behav. Med. 2018, 6, 301–328. [Google Scholar] [CrossRef] [PubMed]
- Foygel, R.; Drton, M. Extended Bayesian information criteria for Gaussian graphical models. arXiv 2010, arXiv:1011.6640. [Google Scholar]
- Chen, J.; Chen, Z. Extended Bayesian information critera for model selection with large model spaces. Biometrika 2008, 95, 759–771. [Google Scholar] [CrossRef]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Olsson, U. Maximum likelihood estimation of the polychoric correlation coefficient. Psychometrika 1979, 44, 443–460. [Google Scholar] [CrossRef]
- Fruchterman, T.M.; Reingold, E.M. Graph drawing by force-directed placement. Softw. Pract. Exp. 1991, 21, 1129–1164. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Robinaugh, D.J.; Millner, A.J.; McNally, R.J. Identifying highly influential nodes in the complicated grief network. J. Abnorm. Psychol. 2016, 125, 747–757. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.J.; Ma, R.; McNally, R.J. Bridge Centrality: A Network Approach to Understanding Comorbidity. Multivar. Behav. Res. 2021, 56, 353–367. [Google Scholar] [CrossRef] [PubMed]
- Haslbeck, J.M.B.; Waldorp, L.J. How well do network models predict observations? On the importance of predictability in network models. Behav. Res. Methods 2018, 50, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Reiff, J.; Schmidt, N.; Riebe, B.; Breternitz, R.; Aldenhoff, J.; Deuschl, G.; Witt, K. Subthreshold depression in Parkinson’s disease. Mov. Disord. 2011, 26, 1741–1744. [Google Scholar] [CrossRef]
- Krupp, L.B.; Pollina, D.A. Mechanisms and management of fatigue in progressive neurological disorders. Curr. Opin. Neurol. 1996, 9, 456–460. [Google Scholar] [CrossRef]
- Barone, P.; Antonini, A.; Colosimo, C.; Marconi, R.; Morgante, L.; Avarello, T.; Bottacchi, E.; Cannas, A.; Ceravolo, G.; Ceravolo, R.; et al. The PRIAMO study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov. Disord. 2009, 24, 1641–1649. [Google Scholar] [CrossRef]
- Pont-Sunyer, C.; Hotter, A.; Gaig, C.; Seppi, K.; Compta, Y.; Katzenschlager, R.; Mas, N.; Hofeneder, D.; Brücke, T.; Bayés, A.; et al. The onset of nonmotor symptoms in Parkinson’s disease (the ONSET PD study). Mov. Disord. 2015, 30, 229–237. [Google Scholar] [CrossRef]
- Friedman, J.H.; Friedman, H. Fatigue in Parkinson’s disease: A nine-year follow-up. Mov. Disord. 2001, 16, 1120–1122. [Google Scholar] [CrossRef]
- Alves, G.; Wentzel-Larsen, T.; Larsen, J.P. Is fatigue an independent and persistent symptom in patients with Parkinson disease? Neurology 2004, 63, 1908–1911. [Google Scholar] [CrossRef]
- Herlofson, K.; Kluger, B.M. Fatigue in Parkinson’s disease. J. Neurol. Sci. 2017, 374, 38–41. [Google Scholar] [CrossRef]
- Stocchi, F.; Abbruzzese, G.; Ceravolo, R.; Cortelli, P.; D’Amelio, M.; De Pandis, M.F.; Fabbrini, G.; Pacchetti, C.; Pezzoli, G.; Tessitore, A.; et al. Prevalence of fatigue in Parkinson disease and its clinical correlates. Neurology 2014, 83, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Jason, L.A.; Evans, M.; Brown, M.; Porter, N. What is fatigue? Pathological and nonpathological fatigue. PM&R 2010, 2, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Franssen, M.; Winward, C.; Collett, J.; Wade, D.; Dawes, H. Interventions for fatigue in Parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2014, 29, 1675–1678. [Google Scholar] [CrossRef]
- Elbers, R.G.; Berendse, H.W.; Kwakkel, G. Treatment of Fatigue in Parkinson Disease. JAMA 2016, 315, 2340–2341. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, C.; Barreto, M.; Oliveira, S. The Link Between Major Life Events and Quality of Life: The Role of Compassionate Abilities. Community Ment. Health J. 2021, 57, 219–227. [Google Scholar] [CrossRef]
- Dohrenwend, B.P. Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychol. Bull. 2006, 132, 477–495. [Google Scholar] [CrossRef]
- Mundt, C.; Reck, C.; Backenstrass, M.; Kronmüller, K.; Fiedler, P. Reconfirming the role of life events for the timing of depressive episodes. A two-year prospective follow-up study. J. Affect. Disord. 2000, 59, 23–30. [Google Scholar] [CrossRef]
- Kessing, L.V.; Agerbo, E.; Mortensen, P.B. Does the impact of major stressful life events on the risk of developing depression change throughout life? Psychol. Med. 2003, 33, 1177–1184. [Google Scholar] [CrossRef]
- Lickel, B.; Kushlev, K.; Savalei, V.; Matta, S.; Schmader, T. Shame and the motivation to change the self. Emotion 2014, 14, 1049–1061. [Google Scholar] [CrossRef]
- Rubenstein, L.M.; Freed, R.D.; Shapero, B.G.; Fauber, R.L.; Alloy, L.B. Cognitive Attributions in Depression: Bridging the Gap between Research and Clinical Practice. J. Psychother. Integr. 2016, 26, 103–115. [Google Scholar] [CrossRef]
- Ferreira, C.; Mendes, A.L.; Marta-Simões, J. The Role of Maladaptive Psychological Strategies in the Association between Shame and Psychological Quality of Life. Eur. Psychiatry 2017, 41, S86. [Google Scholar] [CrossRef]
- Zhang, H.; Carr, E.R.; Garcia-Williams, A.G.; Siegelman, A.E.; Berke, D.; Niles-Carnes, L.V.; Patterson, B.; Watson-Singleton, N.N.; Kaslow, N.J. Shame and Depressive Symptoms: Self-compassion and Contingent Self-worth as Mediators? J. Clin. Psychol. Med. Settings 2018, 25, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Berrios, G.E.; Olivares, J.M. The anhedonias: A conceptual history. Hist. Psychiatry 1995, 6, 453–470. [Google Scholar] [CrossRef]
- Kaji, Y.; Hirata, K. Apathy and anhedonia in Parkinson’s disease. ISRN Neurol. 2011, 2011, 219427. [Google Scholar] [CrossRef]
- Billones, R.R.; Kumar, S.; Saligan, L.N. Disentangling fatigue from anhedonia: A scoping review. Transl. Psychiatry 2020, 10, 273. [Google Scholar] [CrossRef] [PubMed]
- Heimrich, K.G.; Schönenberg, A.; Mühlhammer, H.M.; Mendorf, S.; Santos-García, D.; Prell, T. Longitudinal analysis of the Non-Motor Symptoms Scale in Parkinson’s Disease (NMSS): An exploratory network analysis approach. Front. Neurol. 2023, 14, 972210. [Google Scholar] [CrossRef] [PubMed]
- Heimrich, K.G.; Schönenberg, A.; Santos-García, D.; Mir, P.; Group, C.S.; Prell, T. The Impact of Nonmotor Symptoms on Health-Related Quality of Life in Parkinson’s Disease: A Network Analysis Approach. J. Clin. Med. 2023, 12, 2573. [Google Scholar] [CrossRef]
- Stohlman, S.L.; Barrett, M.J.; Sperling, S.A. Factor structure of the BDI-II in Parkinson’s disease. Neuropsychology 2021, 35, 540–546. [Google Scholar] [CrossRef]


| Variable | |
|---|---|
| Age | 64 (57–70) |
| Disease duration | 5 (2–8) |
| HY off | 2 (2–2) |
| UPDRS III off | 21 (14–30) |
| UPDRS IV off | 1 (0–3) |
| NMSS, total score | 35 (19–61) |
| MMSE, total score | 30 (29–30) |
| BDI-II, total score | 7 (3–13) |
| 1. Sadness | 0 (0–1) |
| 2. Pessimism | 0 (0–1) |
| 3. Past failure | 0 (0–0) |
| 4. Loss of pleasure | 0 (0–1) |
| 5. Guilty feelings | 0 (0–0) |
| 6. Punishment feelings | 0 (0–0) |
| 7. Self-dislike | 0 (0–0) |
| 8. Self-criticalness | 0 (0–1) |
| 9. Suicidal thoughts or wishes | 0 (0–0) |
| 10. Crying | 0 (0–1) |
| 11. Agitation | 0 (0–1) |
| 12. Loss of interest | 0 (0–1) |
| 13. Indecisiveness | 0 (0–1) |
| 14. Worthlessness | 0 (0–1) |
| 15. Loss of energy | 1 (0–1) |
| 16. Changes in sleeping pattern | 1 (0–2) |
| 17. Irritability | 0 (0–1) |
| 18. Changes in appetite | 0 (0–1) |
| 19. Concentration difficulty | 1 (0–1) |
| 20. Tiredness or fatigue | 1 (0–1) |
| 21. Loss of interest in sex | 0 (0–1) |
| EUROHIS-QOL 8-item index | 31 (28–33) |
| 1. QOL, quality | 4 (3–4) |
| 2. HEA, health | 3 (3–4) |
| 3. ENE, energy | 4 (3–4) |
| 4. ACT, activities | 4 (3–4) |
| 5. YOU, yourself | 4 (3–4) |
| 6. REL, relationships | 4 (4–4) |
| 7. MON, money | 4 (3–4) |
| 8. LIV, living | 4 (4–5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heimrich, K.G.; Mendorf, S.; Schönenberg, A.; Santos-García, D.; Mir, P.; COPPADIS Study Group; Prell, T. Depressive Symptoms and Their Impact on Quality of Life in Parkinson’s Disease: An Exploratory Network Analysis Approach. J. Clin. Med. 2023, 12, 4616. https://doi.org/10.3390/jcm12144616
Heimrich KG, Mendorf S, Schönenberg A, Santos-García D, Mir P, COPPADIS Study Group, Prell T. Depressive Symptoms and Their Impact on Quality of Life in Parkinson’s Disease: An Exploratory Network Analysis Approach. Journal of Clinical Medicine. 2023; 12(14):4616. https://doi.org/10.3390/jcm12144616
Chicago/Turabian StyleHeimrich, Konstantin G., Sarah Mendorf, Aline Schönenberg, Diego Santos-García, Pablo Mir, COPPADIS Study Group, and Tino Prell. 2023. "Depressive Symptoms and Their Impact on Quality of Life in Parkinson’s Disease: An Exploratory Network Analysis Approach" Journal of Clinical Medicine 12, no. 14: 4616. https://doi.org/10.3390/jcm12144616
APA StyleHeimrich, K. G., Mendorf, S., Schönenberg, A., Santos-García, D., Mir, P., COPPADIS Study Group, & Prell, T. (2023). Depressive Symptoms and Their Impact on Quality of Life in Parkinson’s Disease: An Exploratory Network Analysis Approach. Journal of Clinical Medicine, 12(14), 4616. https://doi.org/10.3390/jcm12144616








