Relation between Maximum Oral Muscle Pressure and Dentoalveolar Characteristics in Patients with Cleft Lip and/or Palate: A Prospective Comparative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Subject Recruitment
2.2. Assessment of Dentoalveolar Data
2.3. Assessment of Functional Habits
2.4. Assessment of Oral Muscle Pressure
2.5. Statistical Analysis
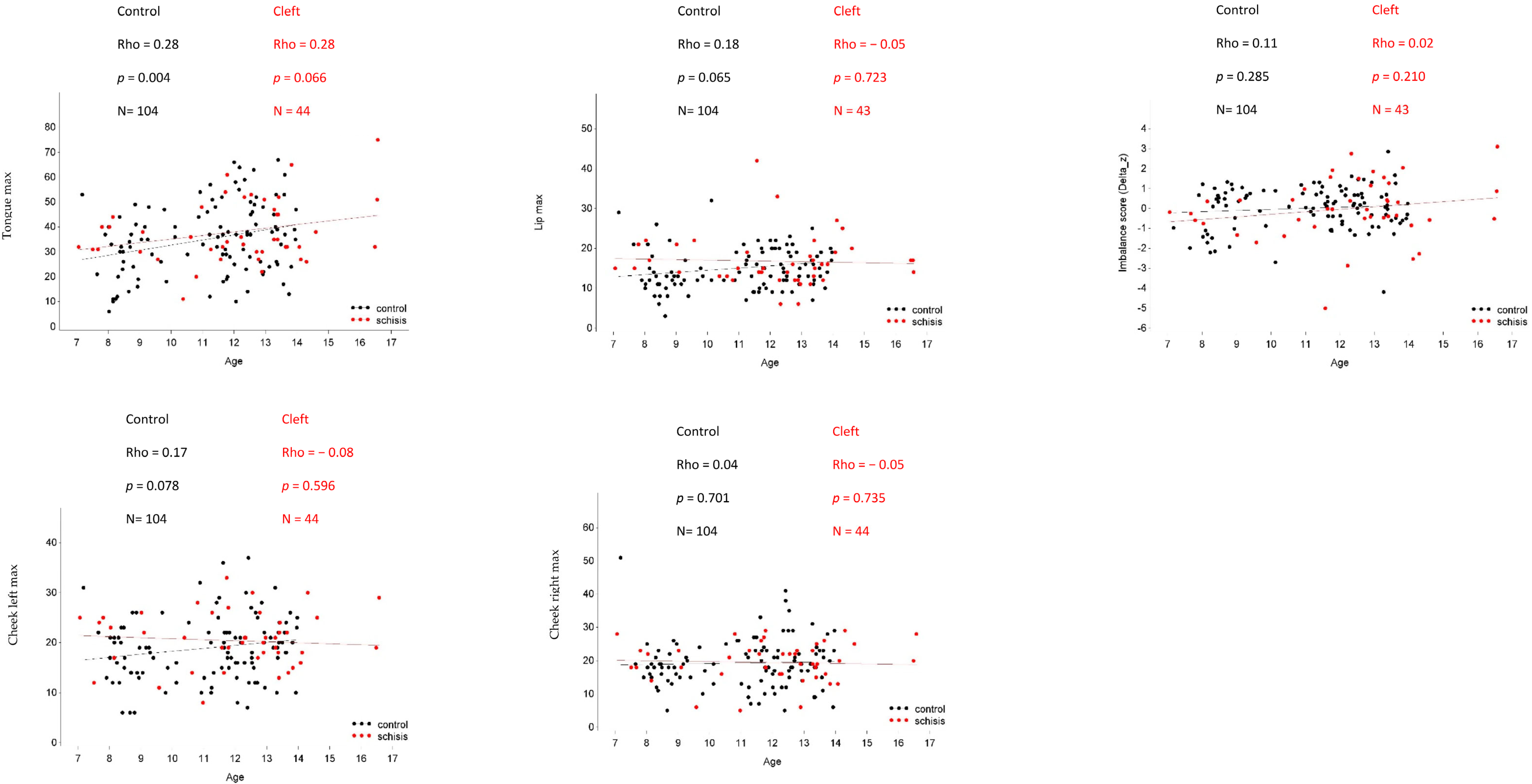
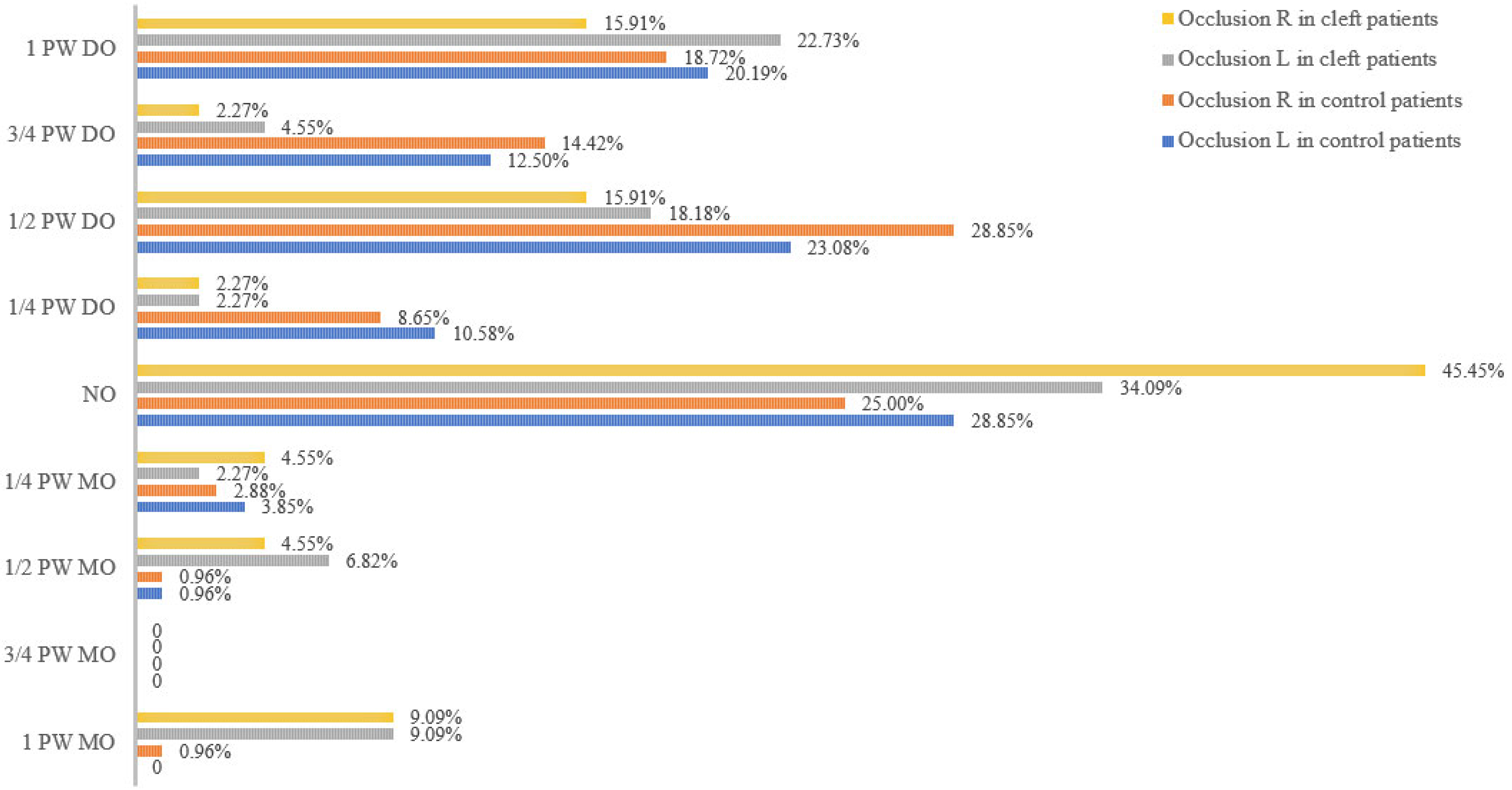
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leme, M.; Barbosa, T.; Gaviao, M. Relationship among oral habits, orofacial function and oral health related quality of life in children. Braz. Oral Res. 2013, 27, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Ruan, W.H.; Su, J.M.; Ye, X.W. Pressure from the lips and the tongue in children with class III malocclusion. J. Zhejiang Univ. Sci. B 2007, 8, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W. Muscle Pressures and Tooth Position: North American Whites and Australian Aborigines. Angle Orthod. 1975, 45, 1–11. [Google Scholar] [PubMed]
- Thüer, U.; Ingervall, B. Pressure from the lips on the teeth and malocclusion. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 234–242. [Google Scholar] [CrossRef]
- Doto, N.; Yamada, K. The relationship between maximum lip closing force and tongue pressure according to lateral craniofacial morphology. Orthod. Waves 2015, 74, 69–75. [Google Scholar] [CrossRef]
- Jung, M.H.; Yang, W.S.; Nahm, D.S. Maximum closing force of mentolabial muscles and type of malocclusion. Angle Orthod. 2010, 80, 72–79. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Crimi, S.; Badnjevic, A.; Cervino, G.; Bianchi, A.; Cicciu, M. Correlation between temporomandibular disorders (TMD) and Posture evaluated trough the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): A systematic Review with Meta-Anaylis. J. Clin. Med. 2023, 12, 2652. [Google Scholar] [CrossRef]
- Sweeney, W.M.; Lanier, S.T.; Purnell, C.A.; Gosain, A.K. Genetics of Cleft Palate and Velopharyngeal Insufficiency. J. Pediatr. Genet. 2015, 4, 9–16. [Google Scholar] [CrossRef]
- Trotman, C.A.; Faraway, J.J.; Phillips, C. Visual and Statistical Modeling of Facial Movement in Patients with Cleft Lip and Palate. Cleft Palate-Craniofac. J. 2005, 42, 245–254. [Google Scholar] [CrossRef]
- Szyska-Sommerfeld, L.; Wozniak, K.; Matthews-Brzozowska, T.; Kawala, B.; Mikulewicz, M. Electromyographic analysis of superior orbicularis oris muscle function in children surgically treated for unilateral complete cleft lip and palate. J. Cranio-Maxillofac. Surg. 2017, 45, 1547–1551. [Google Scholar] [CrossRef]
- Van Lierde, K.M.; Bettens, K.; Luyten, A. Oral strength in subjects with a unilateral cleft lip and palate. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 1306–1310. [Google Scholar] [CrossRef] [PubMed]
- Trotman, C.; Faraway, J.; Soltman, R.; Hartman, T.; Van Aalst, J. Facial soft tissue dynamics before and after primary lip repair. Cleft Palate-Craniofacial J. 2013, 50, 315–322. [Google Scholar] [CrossRef]
- Van Lieshout, P.H.H.M.; Rutjens, C.A.W.; Spauwen, P.H.M. The dynamics of interlip coupling in speakers with a repaired unilateral cleft-lip history. J. Speech Lang. Hear. Res. 2002, 45, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Nakatsuka, K.; Adachi, T.; Kato, T.; Murakami, M.; Yamada, K.; Masuda, Y. Asymmetric lip-closing forces in children with repaired unilateral cleft lip and/or palate. J. Oral Rehabil. 2011, 38, 921–928. [Google Scholar] [CrossRef]
- Van De Velde, A.; De Boodt, L.; Cadenas De Llano-Pérula, M. Short term effects of interceptive expansion treatment: A prospective study. Eur. J. Orthod. 2021, 43, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Van Dyck, C.; Dekeyser, A.; Vantricht, E. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: A pilot study. Eur. J. Orthod. 2016, 38, 227–234. [Google Scholar] [CrossRef]
- Vanderwegen, J.; Guns, C.; Van Nuffelen, G. The Influence of Age, Sex, Bulb Position, Visual Feedback and the Order of Testing on Maximum Anterior and Posterior Tongue Strength and Endurance in Healthy Belgian Adults. Dysphagia 2013, 28, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Schoenwolf, G.C.; Bleyl, S.B.; Brauer, P.R.; Francis-West, P.H. Larsen’s Human Embryology, 4th ed.; Elsevier: Amsterdam, The Netherlands, 2009; pp. 543–582. [Google Scholar]
- Clark, H.M.; Solomon, N.P. Age and sex differences in orofacial strength. Dysphagia 2012, 27, 2–9. [Google Scholar] [CrossRef]
- Ariawan, D.; Vitria, E.E.; Sulistyani, L.D.; Anindya, C.S.; Adrin, N.S.R. Prevalence of Simonart’s band in cleft children at a cleft center in Indonesia: A nine-year retrospective study. Dent. Med. Probl. 2022, 59, 509–515. [Google Scholar] [CrossRef]
- Da Silva Filho, O.G.; Santamaria, M., Jr.; Da Silva Dalben, G.; Semb, G. Prevalence of a Simonart’s band in patients with complete cleft lip and alveolus and complete cleft lip and palate. Cleft Palate-Craniofac. J. 2006, 43, 442–445. [Google Scholar] [CrossRef]
- Ezzat, C.F.; Chavarria, C.; Teichgraeber, J.F.; Chen, J.W.; Stratmann, R.G.; Gateno, J. Presurgical nasoalveolar molding therapy for the treatment of unilateral cleft lip and palate: A preliminary study. Cleft Palate-Craniofac. J. 2007, 44, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Alzain, I.; Batwa, W.; Cash, A.; Murshid, Z.A. Presurgical cleft lip and palate orthopedics: An overview. Clin. Cosmet. Investig. Dent. 2017, 9, 53–59. [Google Scholar] [CrossRef]
- Sommerlad, B.C. A technique for cleft palate repair. Plast. Reconstr. Surg. 2003, 112, 1542–1548. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, G.L.U.; Jacob, H.B.; Brunetto, M. A preliminary 3-D comparison of rapid and slow maxillary expansión in children: A randomized clinical trial. Int. J. Pediatr. Dent. 2020, 30, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Paradowska-Stolarz, A.; Mikulewicz, M.; Duś-Ilnicka, I. Current Concepts and Challenges in the Treatment of Cleft Lip and Palate Patients—A Comprehensive Review. J. Pers. Med. 2022, 12, 2089. [Google Scholar] [CrossRef]
- Pereira, A.C.; Jorge, T.M.; Ribeiro, P.D.; Berretin, G. Características das funções orais de indivíduos com má oclusão Classe III e diferentes tipos faciais. Rev. Dent. Press Ortodon. Ortop. Facial 2005, 10, 111–119. [Google Scholar] [CrossRef]
- Proffit, W.R. Equilibrium Theory Revisited: Factors Influencing Position of the teeth. Angle Orthod. 1978, 48, 175–186. [Google Scholar]
- Moss, M.L.; Salentijn, L. The primary role of functional matrices in facial growth. Am. J. Orthod. 1969, 55, 566–577. [Google Scholar] [CrossRef]
- Weinstein, S.; Haack, D.C.; Morris, L.Y.; Snyder, B.B.; Attaway, H.E.; Weinstein, S. On a equilibrium theory of tooth position. Angle Orthod. 1963, 33, 1–26. [Google Scholar]
- Proffit, W.; Fields, H.; Sarver, D. Contemporary Orthodontics, 6th ed.; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Thüer, U.; Janson, T.; Ingerval, B. Application in children of a new method for the measurement of forces from the lips on the teeth. Eur. J. Orthod. 1985, 7, 63–78. [Google Scholar] [CrossRef]
- Fröhlich, K.; Thüer, U.; Ingervall, B. Pressure from the tongue on the teeth in young adults. Angle Orthod. 1991, 61, 17–24. [Google Scholar]
- Kieser, J.A.; Farland, M.G.; Jack, H.; Farella, M.; Wang, Y.; Rohrle, O. The of oral soft tissue in swallowing function: What chan tongue pressure tell us? Aust. Dent. J. 2014, 59, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, I.; Abou-Ayash, S.; Genton, L.; Tsuga, K.; Leles, C.R.; Schimmel, M. Reliability and comparability of methods for assessing oral function: Chewing, tongue pressure and lip force. J. Oral Rehabil. 2020, 47, 862–871. [Google Scholar] [CrossRef]
- Youmans, S.R.; Stierwalt, J.A.G. Measures of Tongue Function Related to Normal Swallowing. Dysphagia 2006, 21, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Kikutani, T.; Tsuga, K.; Utanohara, Y.; Hayashi, R.; Akagawa, Y. Decreased Tongue Pressure Reflects Symptom of Dysphia. Dysphagia 2006, 21, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Gwak, D.W.; Jung, S.H.; Min, Y.S.; Park, J.S.; Cho, H.J.; Park, D.; Hong, M.W.; Kang, M.G. Correlation between maximal tongue pressure and swallowing function in spinal and bulbar muscular atrophy. Front. Neurol. 2021, 12, 704788. [Google Scholar] [CrossRef]
- Shetye, P.R.; Evans, C.A. Midfacial morphology in adult unoperated complete unilateral cleft lip and palate patients. Angle Orthod. 2006, 76, 810–816. [Google Scholar]
- Lambrechts, H.; De Baets, E.; Fieuws, S.; Willems, G. Lip and tongue pressure in orthodontic patients. Eur. J. Orthod. 2010, 32, 466–471. [Google Scholar] [CrossRef]
- Kecik, D.; Kocaderli, I.; Saatci, I. Evaluation of the treatment changes of functional posterior crossbite in the mixed dentition. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 202–215. [Google Scholar] [CrossRef]
- Szyska-Sommerfeld, L.; Wozniak, K.; Matthews-Brzozowska, T.; Kawala, B.; Mikulewicz, M.; Machoy, M. The electrical activity of the masticatory muscles in children with cleft lip and palate. J. Paediatr. Dent. 2018, 28, 257–265. [Google Scholar] [CrossRef]
- Helkimo, E.; Carlsson, G.E.; Helkimo, M. Bite force and state of dentition. Acta Odontol. Scand. 1977, 35, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Moussa, R.; O’Reilly, M.T.; Close, J.M. Long-term stability of rapid palatal expander treatment and edgewise mechanotherapy. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 478–488. [Google Scholar] [CrossRef] [PubMed]
- Stockfisch, H. Rapid expansion of the maxilla–success and relapse. Rep. Congr. Eur. Orthod. Soc. 1969, 469–481. [Google Scholar]
- Ramstad, T.; Jendal, T. A long-term study of transverse stability of maxillary teeth in patients with unilateral complete cleft lip and palate. J. Oral Rehabil. 1997, 24, 658–665. [Google Scholar] [CrossRef]
- Nicholson, P.T.; Plint, D.A. A long-term study of rapid maxillary expansion and bone grafting in cleft lip and palate patients. Eur. J. Orthod. 1989, 11, 186–192. [Google Scholar] [CrossRef]
- Bucci, R.; D’Antò, V.; Rongo, R.; Valletta, R.; Martina, R.; Michelotti, A. Dental and skeletal effects of palatal expansion techniques: A systematic review of the current evidence from systematic reviews and metaanalyses. J. Oral Rehabil. 2016, 43, 543–564. [Google Scholar] [CrossRef]
- Lin, C.J.; Lee, Y.S.; Hsue, C.F.; Liu, S.J.; Li, J.Y.; Ho, Y.L.; Chen, H.H. Effects of tongue strenghtening exercises on tongue muscle strength: A systematic review and meta-analysis of randomize controlled trials. Sci. Rep. 2022, 12, 10438. [Google Scholar]
| Abbreviations | Definition |
|---|---|
| OHRQoL | Oral Health-related Quality of Life |
| CP | Isolated cleft palate |
| UCLP | Unilateral cleft lip and palate |
| ICD | Intercanine distance |
| IMD | Intermolar distance |
| IOPI | Iowa Oral Performance Instrument |
| LCD | Liquid crystal display |
| CI | Confidence interval |
| SAS | Statistical Analysis System |
| PNAM | Presurgical nasoalveolar moulding |
| kPa | Kilopascal |
| 13g–23g | Distance between the most lingual and cervical points of the permanent maxillary canines, if present |
| 13c–23c | Distance between the cusps of the permanent maxillary canines, if present |
| 16g–26g | Distance between the most lingual and cervical points of the permanent maxillary first molar, if present |
| 16f–26f | Distance between the central fossae connected to the vestibular groove of the permanent maxillary first molar if present |
| 16MB–26MB | Distance between mesio-buccal cusps of the permanent maxillary first molar, if present |
| 16DB–26DB | Distance between disto-buccal cusps of the permanent maxillary first molar, if present |
| 33g–43g | Distance between the most lingual and cervical points of the permanent mandibular canines, if present |
| 33c–43c | Distance between the cusps of the permanent mandibular canines, if present |
| 36g–46g | Distance between the most lingual and cervical points of the permanent mandibular first molar, if present |
| 36f–46f | Distance between the central fossae connected to the vestibular groove of the permanent mandibular first molar, if present |
| 36MB–46MB | Distance between the mesio-buccal cusps of the permanent mandibular first molar, if present |
| 36DB–46DB | Distance between the disto-buccal cusps of the permanent mandibular first molar, if present |
| Control | CP + UCLP | CP | UCLP | ||
|---|---|---|---|---|---|
| General information | N | 104 | 44 | 16 | 28 (17 right) |
| Mean age (years) | 11.13 | 12.00 | 12.50 | 11.72 | |
| Age range (years) SD (years) | 7.17–13.97 1.948 | 7.06–16.57 2.409 | 8.04–14.60 1.702 | 7.06–16.57 2.721 | |
| Girls (n/N (%)) | 53 (50.96%) | 13 (29.55%) | 9 (56.25%) | 4 (14.29%) | |
| Boys (n/N (%)) | 51 (49.04%) | 31 (70.45%) | 7 (43.75%) | 24 (85.71%) | |
| Tongue pressure | N | 104 | 44 | 16 | 28 |
| Mean | 35.00 | 37.95 | 34.88 | 39.71 | |
| SD | 14.19 | 12.50 | 11.71 | 13.07 | |
| Lip pressure | N | 104 | 43 | 16 | 27 |
| Mean | 15.09 | 16.74 | 17.56 | 16.26 | |
| SD | 5.86 | 6.41 | 8.44 | 4.97 | |
| Left cheek pressure | N | 104 | 44 | 16 | 28 |
| Mean | 18.92 | 20.39 | 21.63 | 19.68 | |
| SD | 6.61 | 6.61 | 5.83 | 6.17 | |
| Right cheek pressure | N | 104 | 44 | 16 | 27 |
| Mean | 19.30 | 19.48 | 20.81 | 18.71 | |
| SD | 7.44 | 6.41 | 5.47 | 6.87 | |
| Imbalance score | N | 104 | 43 | 16 | 27 |
| Mean | 36.98 | 37.31 | 32.37 | 40.25 | |
| SD | 20.634 | 21.493 | 26.577 | 17.74 | |
| Muscle Pressure | CP + UCLP vs. Control | CP vs. Control | UCLP vs. Control | CP vs. UCLP | ||||
|---|---|---|---|---|---|---|---|---|
| Mean Diff (95% CI) | p Value | Mean Diff (95% CI) | p Value | Mean Diff (95% CI) | p Value | Mean Diff (95% CI) | p Value | |
| Tongue pressure | 0.957 (−3.919; 5.833) | 0.698 | −2.627 (−9.783; 4.530) | 0.469 | 3.137 (−2.680; 8.955) | 0.288 | −5.764 (−14.21; 2.680) | 0.179 |
| Lip pressure | 1.965 (−0.243; 4.173) | 0.081 | 1.913 (−1.297; 5.123) | 0.240 | 1.999 (−0.676; 4.673) | 0.142 | −0.086 (−3.905; 3.733) | 0.965 |
| Left cheek pressure | 1.018 (−1.357; 3.394) | 0.398 | 2.441 (−1.052; 5.934) | 0.169 | 0.153 (−2.687; 2.993) | 0.915 | 2.288 (−1.834; 6.410) | 0.274 |
| Right cheek pressure | 0.144 (−2.510; 2.798) | 0.915 | 1.525 (−2.383; 5.432) | 0.442 | −0.695 (−3.872; 2.481) | 0.666 | 2.220 (−2.391; 6.831) | 0.343 |
| Imbalance score | −2.975 (−10.62; 4.668) | 0.443 | −6.331 (−17.42; 4.754) | 0.261 | −0.813 (−10.05; 8.422) | 0.862 | −5.519 (−18.71; 7.669) | 0.410 |
| Maxilla | Mandible | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control (1) | CP + UCLP (2) | CP (3) | UCLP (4) | P 1–2 | P 1–3 | P 1–4 | P 3–4 | Control (1) | CP + UCLP (2) | CP (3) | UCLP (4) | P 1–2 | P 1–3 | P 1–4 | P 3–4 | ||||
| 13g–23g | N | 62 | 21 | 12 | 9 | N | 64 | 27 | 13 | 14 | |||||||||
| Mean | 26.66 | 25.05 | 25.77 | 24.08 | 0.171 | 0.452 | 0.083 | 0.349 | 33g–43g | Mean | 20.57 | 21.25 | 21.91 | 20.63 | 0.170 | 0.047 * | 0.923 | 0.225 | |
| Std | 3.903 | 3.993 | 2.497 | 5.426 | Std | 2.204 | 2.694 | 2.104 | 3.096 | ||||||||||
| 13c–23c | N | 62 | 21 | 12 | 9 | N | 64 | 27 | 13 | 14 | |||||||||
| Mean | 32.74 | 30.41 | 32.29 | 27.92 | <0.001 * | 0.584 | <0.001 * | 0.078 | 33c–43c | Mean | 26.06 | 25.64 | 26.06 | 25.25 | 0.552 | 1.000 | 0.286 | 0.539 | |
| Std | 2.497 | 5.634 | 2.828 | 7.491 | Std | 2.119 | 3.305 | 2.483 | 3.977 | ||||||||||
| 16g–26g | N | 103 | 36 | 14 | 22 | N | 102 | 35 | 13 | 22 | |||||||||
| Mean | 32.21 | 33.81 | 34.37 | 33.45 | 0.030 * | 0.011 * | 0.093 | 0.543 | 36g–46g | Mean | 32.62 | 34.10 | 33.80 | 34.28 | 0.020 * | 0.111 | 0.007 * | 0.687 | |
| Std | 2.749 | 4.321 | 4.061 | 4.535 | Std | 2.373 | 3.315 | 3.321 | 3.377 | ||||||||||
| 16f-26f | N | 103 | 36 | 14 | 22 | N | 102 | 35 | 13 | 22 | |||||||||
| Mean | 43.78 | 45.13 | 45.78 | 44.72 | 0.140 | 0.041 * | 0.283 | 0.563 | 36f-46f | Mean | 40.67 | 41.63 | 40.81 | 42.11 | 0.113 | 0.865 | 0.027 * | 0.366 | |
| Std | 3.210 | 5.253 | 4.680 | 5.655 | Std | 2.416 | 4.051 | 4.335 | 3.896 | ||||||||||
| 16MB–26MB | N | 103 | 36 | 14 | 22 | N | 102 | 35 | 13 | 22 | |||||||||
| Mean | 48.38 | 48.03 | 48.64 | 47.64 | 0.660 | 0.806 | 0.366 | 0.579 | 36MB–46MB | Mean | 43.93 | 44.39 | 43.45 | 44.95 | 0.310 | 0.579 | 0.155 | 0.330 | |
| Std | 3.165 | 5.140 | 5.825 | 4.757 | Std | 2.694 | 4.331 | 4.486 | 4.243 | ||||||||||
| 16DB–26DB | N | 102 | 35 | 13 | 22 | N | 101 | 35 | 13 | 22 | |||||||||
| Mean | 50.50 | 50.81 | 51.36 | 50.48 | 0.731 | 0.397 | 0.989 | 0.627 | 36DB–46DB | Mean | 46.21 | 47.39 | 46.68 | 47.80 | 0.152 | 0.630 | 0.047 * | 0.456 | |
| Std | 3.190 | 5.066 | 5.229 | 5.063 | Std | 3.192 | 4.205 | 4.370 | 4.152 | ||||||||||
| Jaw Width | Control | CP + UCLP | CP | UCLP | Control vs. CP + UCLP | Control vs. CP | Control vs. UCLP | CP vs. UCLP | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Slope (95% CI) | p-Value | Slope (95% CI) | p-Value | Slope (95% CI) | p-Value | Slope (95% CI) | p-Value | Test for Difference of Slopes between Groups p-Value | |||||
| Effect of tongue pressure | 13g–23g | −0.041 (−0.111; 0.030) | 0.252 | 0.028 (−0.114; 0.171) | 0.697 | −0.044 (−0.255; 0.167) | 0.680 | 0.219 (−0.015; 0.454) | 0.066 | 0.391 | 0.978 | 0.037 * | 0.101 |
| 13c–23c | −0.012 (−0.111; 0.030) | 0.703 | 0.023 (−0.106; 0.153) | 0.720 | −0.034 (−0.209; 0.141) | 0.700 | 0.332 (0.138; 0.526) | 0.001 * | 0.625 | 0.815 | 0.001 * | 0.007 * | |
| 16g–26g | 0.027 (−0.017; 0.070) | 0.229 | 0.092 (0.009; 0.174) | 0.029 * | 0.173 (0.022; 0.324) | 0.025 * | 0.076 (−0.026; 0.177) | 0.142 | 0.170 | 0.068 | 0.382 | 0.292 | |
| 16f-26f | −0.004 (−0.056; 0.048) | 0.883 | 0.132 (0.034; 0.229) | 0.008 * | 0.194 (0.014; 0.374) | 0.035 * | 0.130 (0.010; 0.251) | 0.035 * | 0.016 * | 0.038 * | 0.045 * | 0.562 | |
| 16MB–26MB | 0.033 (−0.017; 0.084) | 0.197 | 0.126 (0.031; 0.221) | 0.010 * | 0.309 (0.136; 0.481) | <0.001 * | 0.068 (−0.048; 0.184) | 0.245 | 0.092 | 0.003 * | 0.583 | 0.024 * | |
| 16DB–26DB | 0.006 (−0.045; 0.057) | 0.820 | 0.129 (0.034; 0.225) | 0.008 * | 0.296 (0.122; 0.470) | 0.001 * | 0.079 (−0.037; 0.196) | 0.180 | 0.025* | 0.002 * | 0.254 | 0.043 * | |
| 33g–43g | −0.007 (−0.047; 0.033) | 0.730 | 0.046 (−0.017; 0.110) | 0.150 | 0.042 (−0.070; 0.154) | 0.455 | 0.092 (0.007; 0.177) | 0.034 * | 0.162 | 0.412 | 0.038 * | 0.482 | |
| 33c–43c | −0.013 (−0.056; 0.030) | 0.552 | 0.054 (−0.014; 0.121) | 0.121 | 0.000 (−0.119; 0.120) | 0.995 | 0.117 (0.027; 0.208) | 0.012 * | 0.104 | 0.836 | 0.011 * | 0.124 | |
| 36g–46g | 0.007 (−0.029; 0.042) | 0.705 | 0.105 (0.038; 0.171) | 0.002 * | 0.076 (−0.048; 0.200) | 0.226 | 0.120 (0.037; 0.203) | 0.005 * | 0.012 * | 0.289 | 0.015 * | 0.561 | |
| 36f–46f | 0.010 (−0.027; 0.047) | 0.603 | 0.173 (0.103; 0.243) | <0.001 * | 0.189 (0.059; 0.320) | 0.005 * | 0.163 (0.076; 0.251) | <0.001 * | <0.001 * | 0.010 * | 0.002 * | 0.742 | |
| 36MB–46MB | 0.011 (−0.030; 0.053) | 0.600 | 0.167 (0.089; 0.245) | <0.001 * | 0.214 (0.069; 0.358) | 0.004 * | 0.140 (0.043; 0.237) | 0.005 * | <0.001 * | 0.009 * | 0.017 * | 0.406 | |
| 36DB–46DB | −0.003 (−0.049; 0.042) | 0.885 | 0.182 (0.097; 0.268) | <0.001 * | 0.211 (0.052; 0.369) | 0.010 * | 0.170 (0.064; 0.276) | 0.002 * | <0.001 * | 0.012 * | 0.004 * | 0.674 | |
| 13g–23g | −0.057 (−0.230; 0.115) | 0.508 | −0.232 (−0.591; 0.127) | 0.202 | −0.308 (−0.767; 0.150) | 0.184 | −0.104 (−0.691; 0.483) | 0.725 | 0.385 | 0.311 | 0.880 | 0.586 | |
| 13c–23c | 0.013 (−0.139; 0.165) | 0.866 | −0.378 (−0.695; −0.061) | 0.020 * | −0.444 (−0.830; −0.059) | 0.024 * | −0.263 (−0.756; 0.231) | 0.293 | 0.030 * | 0.030 * | 0.290 | 0.565 | |
| 16g–26g | 0.087 (−0.020; 0.194) | 0.110 | −0.190 (−0.394; 0.014) | 0.068 | 0.000 (−0.338; 0.339) | 0.999 | −0.285 (−0.543; −0.027) | 0.031 * | 0.019* | 0.630 | 0.009 * | 0.187 | |
| 16f–26f | 0.034 (−0.095; 0.163) | 0.602 | −0.202 (−0.448; 0.044) | 0.107 | 0.042 (−0.365; 0.450) | 0.838 | −0.326 (−0.637; −0.016) | 0.040 * | 0.095 | 0.969 | 0.036 * | 0.157 | |
| 16MB–26MB | 0.109 (−0.012; 0.230) | 0.078 | −0.393 (−0.625; −0.162) | 0.001 * | −0.320 (−0.706; 0.067) | 0.104 | −0.423 (−0.717; −0.128 | 0.005 * | <0.001 * | 0.038 * | 0.001 * | 0.675 | |
| 16DB–26DB | 0.072 (−0.052; 0.196) | 0.251 | −0.320 (−0.560; −0.080) | 0.009 * | −0.266 (−0.691; 0.159) | 0.219 | −0.335 (−0.635; −0.035) | 0.029 * | 0.005 * | 0.134 | 0.015 * | 0.794 | |
| 33g–43g | 0.020 (−0.080; 0.120) | 0.695 | −0.220 (−0.377; −0.064) | 0.006 * | −0.129 (−0.394; 0.135) | 0.334 | −0.252 (−0.449; −0.055) | 0.013 * | 0.012 * | 0.298 | 0.016 * | 0.462 | |
| 33c–43c | −0.032 (−0.136; 0.071) | 0.539 | −0.306 (−0.468; −0.145) | <0.001 * | −0.282 (−0.559; −0.005) | 0.046 * | −0.313 (−0.519; −0.107) | 0.003 * | 0.006 * | 0.050 * | 0.018 * | 0.859 | |
| 36g–46g | 0.140 (0.017; 0.191)) | 0.012 * | −0.071 (−0.240; 0.097) | 0.403 | −0.075 (−0.358; 0.207) | 0.600 | −0.076 (−0.289; 0.138) | 0.484 | 0.070 | 0.234 | 0.126 | 0.997 | |
| 36f–46f | 0.095 (−0.005; 0.194) | 0.063 | −0.175 (−0.360; 0.011) | 0.065 | −0.355 (−0.662; −0.048) | 0.024 * | −0.091 (−0.323; 0.141) | 0.438 | 0.013 * | 0.007 * | 0.147 | 0.177 | |
| 36MB–46MB | 0.137 (0.029; 0.245) | 0.014 * | −0.162 (−0.363; 0.040) | 0.115 | −0.302 (−0.636; 0.032) | 0.076 | −0.130 (−0.356; 0.149) | 0.419 | 0.011 * | 0.015 * | 0.086 | 0.350 | |
| 36DB–46DB | 0.100 (−0.019; 0.219) | 0.099 | −0.215 (−0.437; 0.007) | 0.057 | −0.353 (−0.723; 0.017) | 0.061 | −0.154 (−0.433; 0.125) | 0.277 | 0.015 * | 0.023 * | 0.100 | 0.398 | |
| 13g–23g | −0.024 (−0.087; 0.040) | 0.455 | 0.029 (−0.055; 0.112) | 0.497 | 0.013 (−0.091; 0.116) | 0.809 | 0.114 (−0.044; 0.271) | 0.155 | 0.322 | 0.551 | 0.111 | 0.290 | |
| 13c–23c | −0.028 (−0.085; 0.028) | 0.279 | 0.061 (−0.013; 0.135) | 0.104 | 0.056 (−0.029; 0.140) | 0.193 | 0.194 (0.065; 0.322) | 0.004 * | 0.059 | 0.095 | 0.002 * | 0.078 | |
| 16g–26g | 0.003 (−0.027; 0.033) | 0.837 | 0.078 (0.025; 0.131) | 0.004 * | 0.076 (−0.003; 0.155) | 0.059 | 0.087 (0.014; 0.159) | 0.020 * | 0.016 * | 0.090 | 0.037 * | 0.844 | |
| 16f–26f | −0.000 (−0.036; 0.035) | 0.987 | 0.097 (0.034; 0.160) | 0.003 * | 0.084 (−0.010; 0.178) | 0.079 | 0.116 (0.029; 0.202) | 0.009 * | 0.009 * | 0.099 | 0.015 * | 0.625 | |
| 16MB–26MB | 0.001 (−0.032; 0.035) | 0.940 | 0.140 (0.081; 0.199) | <0.001 * | 0.177 (0.089; 0.264) | <0.001 * | 0.117 (0.037; 0.198) | 0.005 * | <.0.001 * | <0.001* | 0.009 * | 0.323 | |
| 16DB–26DB | −0.008 (−0.042; 0.026) | 0.646 | 0.119 (0.058; 0.180) | <0.001 * | 0.153 (0.063; 0.243) | 0.001 * | 0.096 (0.014; 0.178) | 0.022 * | <0.001 * | 0.001* | 0.022 * | 0.359 | |
| 33g–43g | −0.028 (−0.064; 0.008) | 0.113 | 0.050 (0.011; 0.090) | 0.014 * | 0.032 (−0.025; 0.088) | 0.272 | 0.080 (0.025; 0.136) | 0.005 * | 0.005 * | 0.078 | 0.002 * | 0.227 | |
| 33c–43c | −0.016 (−0.054; 0.022) | 0.411 | 0.069 (0.027; 0.111) | 0.002 * | 0.046 (−0.015; 0.106) | 0.136 | 0.100 (0.041; 0.159) | 0.001 * | 0.004 * | 0.090 | 0.002 * | 0.206 | |
| 36g–46g | −0.018 (−0.042; 0.007) | 0.155 | 0.064 (0.021; 0.108) | 0.004 * | 0.055 (−0.010; 0.121) | 0.094 | 0.071 (0.012; 0.131) | 0.019 * | 0.001 * | 0.039* | 0.007 * | 0.724 | |
| 36f–46f | −0.012 (−0.038; 0.013) | 0.344 | 0.113 (0.067; 0.158) | <0.001 * | 0.135 (0.067; 0.204) | <0.001 * | 0.090 (0.028; 0.152) | 0.005 * | <0.001 * | <0.001* | 0.003 * | 0.333 | |
| 36MB–46MB | −0.018 (−0.047; 0.011) | 0.218 | 0.110 (0.059; 0.160) | <0.001 * | 0.137 (0.061; 0.212) | <0.001 * | 0.083 (0.014; 0.152) | 0.019 * | <0.001 * | <0.001* | 0.009 * | 0.300 | |
| 36DB–46DB | −0.020 (−0.052; 0.011) | 0.212 | 0.123 (0.068; 0.178) | <0.001 * | 0.142 (0.059; 0.224) | <0.001 * | 0.105 (0.029; 0.180) | 0.007 * | <0.001 * | <0.001* | 0.003 * | 0.517 | |
| 13g–23g | −0.019 (−0.145; 0.107) | 0.765 | −0.185 (−0.453; 0.083) | 0.173 | −0.152 (−0.588; 0.284) | 0.490 | −0.353 (−0.731; 0.024) | 0.066 | 0.268 | 0.561 | 0.098 | 0.489 | |
| 13c–23c | 0.036 (−0.068; 0.141) | 0.494 | −0.204 (−0.444; 0.036) | 0.094 | −0.374 (−0.736; −0.011) | 0.043 * | −0.377 (−0.690; −0.063) | 0.019 * | 0.075 | 0.034 * | 0.015 * | 0.990 | |
| 16g–26g | 0.038 (−0.047; 0.123) | 0.379 | 0.047 (−0.121; 0.214) | 0.582 | −0.032 (−0.365; 0.300) | 0.848 | 0.058 (−0.142; 0.259) | 0.567 | 0.927 | 0.686 | 0.854 | 0.645 | |
| 16f–26f | 0.025 (−0.077; 0.127) | 0.627 | −0.032 (−0.232; 0.168) | 0.755 | −0.070 (−0.467; 0.327) | 0.728 | −0.043 (−0.282; 0.197) | 0.726 | 0.618 | 0.648 | 0.608 | 0.908 | |
| 16MB–26MB | 0.053 (−0.047; 0.152) | 0.296 | −0.007 (−0.203; 0.189) | 0.941 | −0.096 (−0.484; 0.293) | 0.628 | 0.003 (−0.232; 0.237) | 0.981 | 0.589 | 0.466 | 0.699 | 0.669 | |
| 16DB–26DB | 0.018 (−0.081; 0.118) | 0.716 | 0.025 (−0.171; 0.222) | 0.801 | 0.048 (−0.342; 0.439) | 0.807 | 0.001 (−0.234; 0.236) | 0.995 | 0.951 | 0.884 | 0.892 | 0.837 | |
| 33g–43g | −0.032 (−0.108; 0.044) | 0.406 | 0.011 (−0.125; 0.147) | 0.872 | 0.032 (−0.213; 0.277) | 0.798 | −0.054 (−0.233; 0.125) | 0.553 | 0.586 | 0.624 | 0.824 | 0.578 | |
| 33c–43c | 0.009 (−0.073; 0.090) | 0.830 | −0.072 (−0.218; 0.074) | 0.329 | −0.146 (−0.409; 0.116) | 0.271 | −0.082 (−0.274; 0.111) | 0.401 | 0.338 | 0.265 | 0.391 | 0.694 | |
| 36g–46g | 0.029 (−0.040; 0.098) | 0.412 | 0.048 (−0.090; 0.186) | 0.493 | −0.199 (−0.468; 0.069) | 0.144 | 0.150 (−0.012; 0.312) | 0.069 | 0.807 | 0.106 | 0.175 | 0.029 * | |
| 36f–46f | 0.010 (−0.067; 0.087) | 0.795 | −0.041 (−0.193; 0.112) | 0.599 | −0.202 (−0.501; 0.097) | 0.183 | 0.042 (−0.138; 0.223) | 0.643 | 0.557 | 0.176 | 0.746 | 0.168 | |
| 36MB–46MB | 0.029 (−0.056; 0.113) | 0.504 | −0.041 (−0.207; 0.126) | 0.630 | −0.128 (−0.456; 0.200) | 0.442 | 0.019 (−0.178; 0.217) | 0.848 | 0.465 | 0.363 | 0.932 | 0.449 | |
| 36DB–46DB | 0.012 (−0.081; 0.104) | 0.800 | −0.039 (−0.221; 0.143) | 0.670 | −0.189 (−0.547; 0.170) | 0.300 | 0.036 (−0.181; 0.252) | 0.745 | 0.621 | 0.286 | 0.842 | 0.291 | |
| 13g–23g | −0.011 (−0.153; 0.130) | 0.874 | −0.188 (−0.493; 0.117) | 0.224 | 0.019 (−0.447; 0.485) | 0.935 | −0.506 (−0.937; −0.074) | 0.022 * | 0.300 | 0.901 | 0.033 * | 0.104 | |
| 13c–23c | 0.033 (−0.086; 0.152) | 0.587 | −0.148 (−0.424; 0.127) | 0.288 | −0.008 (−0.400; 0.384) | 0.967 | −0.557 (−0.920; −0.193) | 0.003 * | 0.241 | 0.844 | 0.003 * | 0.045 | |
| 16g–26g | 0.044 (−0.052; 0.139) | 0.366 | 0.008 (−0.169; 0.184) | 0.933 | 0.164 (−0.144; 0.472) | 0.294 | −0.093 (−0.313; 0.128) | 0.407 | 0.722 | 0.462 | 0.263 | 0.182 | |
| 16f–26f | 0.048 (−0.066; 0.161) | 0.407 | −0.066 (−0.276; 0.144) | 0.537 | 0.168 (−0.196; 0.533) | 0.363 | −0.212 (−0.473; 0.048) | 0.110 | 0.350 | 0.532 | 0.073 | 0.096 | |
| 16MB–26MB | 0.070 (−0.041; 0.181) | 0.216 | −0.021 (−0.227; 0.185) | 0.841 | 0.206 (−0.152; 0.564) | 0.257 | −0.160 (−0.416; 0.096) | 0.218 | 0.445 | 0.473 | 0.105 | 0.102 | |
| 16DB–26DB | 0.050 (−0.060; 0.160) | 0.370 | −0.012 (−0.218; 0.194) | 0.910 | 0.322 (−0.033; 0.678) | 0.075 | −0.199 (−0.452; 0.054) | 0.121 | 0.603 | 0.150 | 0.076 | 0.019 | |
| 33g–43g | −0.048 (−0.133; 0.036) | 0.259 | −0.008 (−0.153; 0.136) | 0.909 | 0.064 (−0.162; 0.289) | 0.576 | −0.111 (−0.307; 0.084) | 0.261 | 0.637 | 0.358 | 0.559 | 0.247 | |
| 33c–43c | −0.008 (−0.099; 0.084) | 0.868 | −0.089 (−0.244; 0.066) | 0.256 | −0.045 (−0.289; 0.199) | 0.714 | −0.163 (−0.374; 0.049) | 0.131 | 0.371 | 0.776 | 0.185 | 0.472 | |
| 36g–46g | 0.051 (−0.029; 0.130) | 0.210 | 0.022 (−0.125; 0.168) | 0.770 | −0.071 (−0.343; 0.200) | 0.603 | 0.077 (−0.103; 0.258) | 0.399 | 0.731 | 0.395 | 0.789 | 0.368 | |
| 36f–46f | 0.046 (−0.042; 0.133) | 0.302 | −0.031 (−0.193; 0.131) | 0.705 | 0.076 (−0.223; 0.375) | 0.615 | −0.046 (−0.245; 0.153) | 0.649 | 0.410 | 0.848 | 0.406 | 0.503 | |
| 36MB–46MB | 0.049 (−0.047; 0.144) | 0.313 | −0.039 (−0.215; 0.138) | 0.665 | 0.163 (−0.163; 0.488) | 0.324 | −0.091 (−0.307; 0.126) | 0.408 | 0.390 | 0.507 | 0.245 | 0.202 | |
| 36DB–46DB | 0.063 (−0.042; 0.168) | 0.240 | −0.033 (−0.226; 0.159) | 0.733 | 0.071 (−0.286; 0.429) | 0.695 | −0.052 (−0.290; 0.186) | 0.666 | 0.388 | 0.965 | 0.385 | 0.572 | |
| Control | CP + UCLP | CP | UCLP | Control vs. CP + UCLP | Control vs. CP | Control vs. UCLP | CP vs. UCLP | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Slope/OR (95% CI) | p-Value | Slope/OR (95% CI) | p-Value | Slope/OR (95% CI) | p-Value | Slope/OR (95% CI) | p-Value | Test for Difference of Slopes between Groups p-Value | |||||
| Effect of tongue pressure | Occlusion R | −0.002 (−0.008; 0.004) | 0.471 | −0.015 (−0.026; −0.005) | 0.005 * | −0.018 (−0.038; 0.003) | 0.086 | −0.013 (−0.026; 0.000) | 0.057 | 0.037 * | 0.150 | 0.156 | 0.670 |
| Occlusion L | −0.003 (−0.010; 0.003) | 0.303 | −0.016 (−0.027; −0.005) | 0.005 * | −0.016 (−0.037; 0.005) | 0.135 | −0.016 (−0.030; −0.002) | 0.021 * | 0.050 * | 0.255 | 0.096 | 0.991 | |
| Overjet | 0.022 (−0.020; 0.065) | 0.296 | −0.029 (−0.103; 0.045) | 0.439 | −0.049 (−0.185; 0.087) | 0.478 | 0.012 (−0.075; 0.098) | 0.791 | 0.235 | 0.322 | 0.825 | 0.459 | |
| Overbite | 0.028 (−0.003; 0.060) | 0.080 | −0.004 (−0.060; 0.052) | 0.886 | −0.086 (−0.191; 0.019) | 0.108 | 0.037 (−0.030; 0.104) | 0.280 | 0.321 | 0.041 * | 0.824 | 0.054 | |
| Cross bite | 1.000 (0.987; 1.030) | 0.976 | 1.013 (0.956; −1.073) | 0.663 | 1.011 (0.939; 1.088) | 0.767 | 1.000 (0.972; 1.030) | 0.976 | 0.708 | 0.933 | 0.916 | 0.791 | |
| Effect of lip pressure | Occlusion R | −0.007 (−0.022; 0.008) | 0.355 | 0.031 (0.010; 0.053) | 0.004 * | 0.025 (−0.002; 0.052) | 0.073 | 0.038 (0.003; 0.073) | 0.032 * | 0.004 * | 0.044 * | 0.020 * | 0.547 |
| Occlusion L | −0.005 (−0.020; 0.011) | 0.563 | 0.017 (−0.005; 0.040) | 0.135 | −0.002 (−0.030; 0.026) | 0.895 | 0.048 (0.011; 0.084) | 0.011 * | 0.120 | 0.869 | 0.010 * | 0.036 * | |
| Overjet | −0.108 (−0.209; −0.006) | 0.037 * | 0.069 (−0.076; 0.214) | 0.350 | 0.061 (−0.118; 0.239) | 0.504 | 0.020 (−0.211; 0.251) | 0.864 | 0.050 | 0.105 | 0.316 | 0.785 | |
| Overbite | 0.006 (−0.072; 0.085) | 0.874 | −0.006 (−0.118; 0.106) | 0.921 | 0.036 (−0.106; 0.179) | 0.615 | −0.091 (−0.274; 0.093) | 0.332 | 0.863 | 0.716 | 0.339 | 0.283 | |
| Cross bite | 1.010 (0.943; 1.083) | 0.773 | 1.066 (0.931; 1.221) | 0.352 | 0.963 (0.806; 1.150) | 0.675 | 1.010 (0.943; 1.083) | 0.773 | 0.486 | 0.165 | 0.206 | 0.620 | |
| Effect of imbalance score | Occlusion R | −0.000 (−0.004; 0.004) | 0.906 | −0.012 (−0.018; −0.006) | <0.001 * | −0.010 (−0.018; −0.001) | 0.025 * | −0.013 (−0.023; −0.004) | 0.007 * | 0.003 * | 0.050 | 0.015 * | 0.583 |
| Occlusion L | −0.002 (−0.007; 0.002) | 0.320 | −0.009 (-0.016; −0.003) | 0.006 * | -0.004 (-0.013; 0.005) | 0.411 | −0.017 (−0.027; −0.007) | 0.001 * | 0.075 | 0.767 | 0.010 * | 0.057 | |
| Overjet | 0.028 (−0.001; 0.057) | 0.059 | −0.022 (−0.065; 0.022) | 0.324 | −0.024 (−0.081; 0.033) | 0.402 | 0.010 (−0.054; 0.075) | 0.752 | 0.062 | 0.107 | 0.623 | 0.429 | |
| Overbite | 0.016 (−0.006; 0.038) | 0.156 | −0.008 (−0.041; 0.025) | 0.635 | −0.041 (−0.085; 0.003) | 0.071 | 0.041 (−0.009; 0.091) | 0.110 | 0.238 | 0.025 * | 0.369 | 0.017 * | |
| Cross bite | 0.998 (0.978; 1.018) | 0.811 | 0.991 (0.958; 1.025) | 0.880 | 1.020 (0.966; 1.077) | 0.483 | 0.998 (0.978; 1.018) | 0.811 | 0.730 | 0.155 | 0.252 | 0.459 | |
| Effect of right cheek pressure | Occlusion R | 0.003 (−0.009; 0.015) | 0.670 | 0.009 (−0.012; 0.031) | 0.396 | 0.018 (−0.024; 0.061) | 0.401 | 0.002 (−0.023; 0.028) | 0.861 | 0.593 | 0.488 | 0.981 | 0.527 |
| Occlusion L | 0.006 (−0.007; 0.018) | 0.357 | −0.002 (−0.024; 0.02.) | 0.870 | 0.004 (−0.041; 0.048) | 0.875 | −0.005 (−0.032; 0.021) | 0.695 | 0.554 | 0.923 | 0.456 | 0.737 | |
| Overjet | 0.025 (−0.056; 0.106) | 0.543 | −0.049 (−0.194; 0.096) | 0.506 | 0.168 (−0.106; 0.442) | 0.227 | −0.181 (−0.343; −0.018) | 0.029 * | 0.380 | 0.322 | 0.025 * | 0.032 * | |
| Overbite | 0.018 (−0.043; 0.079) | 0.560 | 0.011 (−0.100; 0.121) | 0.851 | 0.167 (−0.050; 0.385) | 0.130 | −0.057 (−0.185; 0.072) | 0.387 | 0.910 | 0.193 | 0.302 | 0.082 | |
| Cross bite | 0.991 (0.937; 1048) | 0.754 | 1.145 (1.016; 1.289) | 0.029 * | 1.215 (1.020; 1.448) | 0.030 * | 0.991 (0.937; 1.048) | 0.754 | 0.031 * | 0.457 | 0.349 | 0.030 * | |
| Effect of left cheek pressure | Occlusion R | 0.008 (−0.005; 0.021) | 0.240 | 0.015 (−0.007; 0.038) | 0.187 | 0.017 (−0.023; 0.057) | 0.393 | 0.010 (−0.018; 0.038) | 0.486 | 0.590 | 0.665 | 0.905 | 0.766 |
| Occlusion L | 0.010 (−0.004; 0.024) | 0.147 | 0.009 (−0.014; 0.033) | 0.435 | 0.023 (−0.019; 0.064) | 0.276 | 0.001 (−0.028; 0.030) | 0.934 | 0.994 | 0.568 | 0.582 | 0.399 | |
| Overjet | 0.073 (−0.017; 0.163) | 0.112 | −0.097 (−0.249; 0.056) | 0.212 | 0.056 (−0.198; 0.310) | 0.663 | −0.238 (−0.417; −0.059) | 0.010 * | 0.060 | 0.902 | 0.002 * | 0.064 | |
| Overbite | 0.065 (−0.004; 0.133) | 0.063 | 0.018 (−0.097; 0.134) | 0.754 | 0.203 (0.004; 0.403) | 0.046 * | −0.087 (−0.228; 0.054) | 0.224 | 0.500 | 0.196 | 0.057 | 0.020 * | |
| Cross bite | 0.987 (0.927; 1.052) | 0.694 | 1.095 (0.971; 1.234) | 0.139 | 1.155 (0.983; 1.356) | 0.079 | 0.987 (0.927; 1.052) | 0.694 | 0.136 | 0.368 | 0.685 | 0.075 | |
| Control | CP + UCLP | CP | UCLP | Control vs. CP + UCLP | Control vs. CP | Control vs. UCLP | CP vs. UCLP | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean Diff (95% CI) | p-Value | Mean Diff (95% CI) | p-Value | Mean Diff (95% CI) | p-Value | Mean Diff (95% CI) | p-Value | Test for Difference of Slopes between Groups p-Value | |||||
| Effect on tongue pressure | Nail biting | 2.665 (−3.278; 8.607) | 0.377 | 7.356 (−2.659; 17.372) | 0.149 | 12.500 (−2.932; 27.932) | 0.112 | 4.345 (−8.897; 17.588) | 0.517 | 0.427 | 0.242 | 0.819 | 0.429 |
| Pen chewing | 8.233 (−3.057; 19.52) | 0.152 | 3.873 (−5.779; 13.524) | 0.429 | 12.467 (−1.251; 26.184) | 0.075 | −2.065 (−16.46; 12.326) | 0.777 | 0.562 | 0.637 | 0.266 | 0.151 | |
| Thumb sucking | −0.822 (−20.11; 18.465) | 0.933 | −7.810 (−35.11; 19.488) | 0.572 | −5.200 (−33.08; 22.681) | 0.713 | - | - | 0.680 | 0.799 | - | - | |
| Bruxism | −1.430 (−10.02; 7.158) | 0.742 | 13.300 (−2.699; 29.299) | 0.103 | - | - | 12.083 (−4.317; 28.483) | 0.147 | 0.221 | - | 0.151 | - | |
| Infantile swallowing | −6.889 (−12.51; −1.266) | 0.017 * | −4.685 (−13.64; 4.264) | 0.302 | −3.833 (−19.08; 11.411) | 0.620 | −5.520 (−16.65; 5.609) | 0.328 | 0.681 | 0.711 | 0.829 | 0.860 | |
| Lip interposition | −4.306 (−11.88; 3.266) | 0.263 | −6.951 (−26.38; 12.479) | 0.480 | −5.200 (−33.02; 22.625) | 0.712 | −7.538 (−34.99; 19.916) | 0.588 | 0.802 | 0.951 | 0.823 | 0.906 | |
| Physiological tongue position at rest | 4.672 (−1.149; 10.494) | 0.115 | −3.818 (−11.81; 4.172) | 0.346 | −8.000 (−21.26; 5.256) | 0.235 | −1.429 (−11.45; 8.592) | 0.778 | 0.092 | 0.086 | 0.299 | 0.435 | |
| Caudal tongue position at rest | −0.36 (−6.501; 5.730) | 0.901 | 3.780 (−4.403; 11.964) | 0.362 | 8.000 (−5.400; 21.400) | 0.240 | 1.633 (−8.746; 12.013) | 0.756 | 0.421 | 0.262 | 0.741 | 0.459 | |
| Interdental tongue position at rest | −8.157 (−16.13; 0.182) | 0.045 * | −6.093 (−32.81; 20.621) | 0.652 | - | - | −8.000 (−34.84; 18.842) | 0.556 | 0.884 | - | 0.991 | - | |
| Effect on lip pressure | Nail biting | 2.456 (−0.233; 5.145) | 0.073 | −0.717 (−5.264; 3.830) | 0.756 | −1.417 (−8.440; 5.607) | 0.691 | −0.381 (−6.434; 5.672) | 0.901 | 0.237 | 0.311 | 0.399 | 0.825 |
| Pen chewing | 0.915 (−4.232; 6.062) | 0.726 | −2.344 (−6.760; 2.072) | 0.296 | −4.100 (−10.42; 2.216) | 0.201 | −1.545 (−8.194; 5.103) | 0.646 | 0.344 | 0.226 | 0.564 | 0.582 | |
| Thumb sucking | −5.600 (−14.20; 2.996) | 0.200 | −11.05 (−23.22; 1.120) | 0.075 | −12.33 (−24.75; 0.083) | 0.052 | - | - | 0.471 | 0.379 | - | - | |
| Bruxism | −1.782 (−5.690; 2.126) | 0.369 | −3.718 (−11.00; 3.569) | 0.315 | - | - | −3.362 (−10.85; 4.127) | 0.376 | 0.644 | - | 0.712 | - | |
| Infantile swallowing | −2.383 (−4.956; 0.190) | 0.069 | −2.150 (−6.264; 1.964) | 0.303 | −8.750 (−15.60; −1.902) | 0.013 * | 1.542 (−3.498; 6.581) | 0.546 | 0.925 | 0.087 | 0.171 | 0.018 * | |
| Lip interposition | −2.563 (−5.970; 0.844) | 0.139 | −5.550 (−14.30; 3.197) | 0.212 | −12.33 (−24.77; 0.104) | 0.052 | 0.720 (−11.56; 13.000) | 0.908 | 0.530 | 0.136 | 0.611 | 0.142 | |
| Physiological tongue position at rest | −0.500 (−3.199; 2.199) | 0.714 | 1.58 (−2.689; 4.806) | 0.577 | 3.875 (−2.274; 10.024) | 0.215 | −0.648 (−5.385; 4.089) | 0.787 | 0.505 | 0.200 | 0.957 | 0.251 | |
| Caudal tongue position at rest | 1.108 (−1.704; 3.921) | 0.437 | −1.023 (−4.826; 2.780) | 0.5954 | −3.875 (−10.04; 2.287) | 0.216 | 0.667 (−4.182; 5.515) | 0.786 | 0.374 | 0.148 | 0.876 | 0.254 | |
| Interdental tongue position at rest | −0.991 (−4.704; 2.721) | 0.599 | 0.262 (−12.18; 12.700) | 0.967 | - | - | 0.769 (−11.79; 13.326) | 0.904 | 0.849 | - | 0.791 | - | |
| Effect on imbalance score | Nail biting | −2.435 (−11.59; 6.724) | 0.600 | 8.624 (−6.863; 24.112) | 0.273 | 15.676 (−8.115; 39.467) | 0.195 | 4.490 (−16.02; 24.995) | 0.666 | 0.226 | 0.162 | 0.543 | 0.482 |
| Pen chewing | 10.036 (−7.217; 27.289) | 0.252 | 11.237 (−3.566; 26.040) | 0.136 | 24.810 (3.909; 45.711) | 0.020 * | 2.534 (−19.47; 24.534) | 0.820 | 0.917 | 0.281 | 0.595 | 0.149 | |
| Thumb sucking | 18.940 (−10.25; 48.130) | 0.202 | 30.505 (−10.82; 71.829) | 0.147 | 36.585 (−5.414; 78.585) | 0.087 | - | - | 0.652 | 0.496 | - | - | |
| Bruxism | 2.672 (−10.48; 15.818) | 0.688 | 21.729 (−2.784; 46.242) | 0.082 | - | - | 19.664 (−5.495; 44.823) | 0.125 | 0.178 | - | 0.239 | - | |
| Infantile swallowing | −3.152 (−11.98; 5.678) | 0.481 | 1.507 (−12.61; 15.625) | 0.833 | 22.810 (−0.661; 46.280) | 0.057 | −10.78 (−28.05; 6.497) | 0.219 | 0.581 | 0.042 * | 0.437 | 0.024 * | |
| Lip interposition | −0.455 (−12.11; 11.205) | 0.939 | 12.339 (−17.60; 42.273) | 0.416 | 36.585 (−5.818; 78.988) | 0.090 | −9.420 (−51.29; 32.449) | 0.657 | 0.432 | 0.098 | 0.684 | 0.129 | |
| Physiological tongue position at rest | 7.432 (−1.604; 16.469) | 0.106 | −7.110 (−19.66; 5.440) | 0.264 | −20.81 (−41.19; −0.431) | 0.045 * | 1.234 (−14.47; 16.934) | 0.877 | 0.065 | 0.013 * | 0.498 | 0.092 | |
| Caudal tongue position at rest | 1.201 (−8.31; 10.711) | 0.010 * | 7.036 (−5.825; 19.897) | 0.281 | 20.811 (0.166; 41.456) | 0.048 * | −1.045 (−17.29; 15.199) | 0.899 | 0.472 | 0.090 | 0.813 | 0.102 | |
| Interdental tongue position at rest | −16.15 (−28.42; −3.866) | 0.010 * | −6.862 (−48.00; 34.278) | 0.742 | - | - | −10.00 (−51.34; 31.329) | 0.633 | 0.669 | - | 0.778 | - | |
| Effect on right cheek pressure | Nail biting | 0.791 (−2.236; 3.819) | 0.606 | 0.085 (−5.021; 5.191) | 0.974 | 3.250 (−4.610; 11.110) | 0.415 | −2.582 (−9.327; 4.163) | 0.450 | 0.814 | 0.565 | 0.368 | 0.267 |
| Pen chewing | 2.674 (−3.081; 8.430) | 0.360 | −0.245 (−5.151; 4.661) | 0.921 | −2.100 (−9.138; 4.938) | 0.556 | 0.348 (−7.036; 7.732) | 0.926 | 0.446 | 0.301 | 0.624 | 0.636 | |
| Thumb sucking | −2.044 (−11.60; 7.514) | 0.673 | −13.81 (−27.39; −0.230) | 0.046 * | −15.80 (−29.61; −1.992) | 0.025 * | - | - | 0.164 | 0.108 | - | - | |
| Bruxism | −2.840 (−7.190; 1.511) | 0.199 | −3.033 (−11.13; 5.061) | 0.460 | - | - | −2.292 (−10.58; 5.998) | 0.585 | 0.967 | - | 0.908 | - | |
| Infantile swallowing | 1.004 (−1.875; 3.883) | 0.492 | −0.099 (−4.727; 4.528) | 0.966 | −6.083 (−13.86; 1.698) | 0.124 | 3.263 (−2.417; 8.944) | 0.258 | 0.690 | 0.093 | 0.484 | 0.057 | |
| Lip interposition | 1.633 (−2.147; 5.412) | 0.394 | −6.805 (−16.58; 2.972) | 0.171 | −15.80 (−29.63; −1.969) | 0.026 * | 1.346 (−12.30; 14.993) | 0.846 | 0.114 | 0.018 * | 0.968 | 0.083 | |
| Physiological tongue position at rest | 0.455 (−2.543; 3.452) | 0.765 | 0.682 (−3.430; 4.794) | 0.743 | 3.375 (−3.448; 10.198) | 0.329 | −0.857 (−6.015; 4.301) | 0.743 | 0.930 | 0.439 | 0.664 | 0.329 | |
| Caudal tongue position at rest | 0.447 (−2.685; 3.579) | 0.778 | −0.726 (−4.913; 3.461) | 0.732 | −3.375 (−10.23; 3.478) | 0.332 | 0.683 (−4.625; 5.992) | 0.799 | 0.658 | 0.317 | 0.940 | 0.356 | |
| Interdental tongue position at rest | −1.641 (−5.753; 2.472) | 0.431 | 0.535 (−13.24; 14.307) | 0.939 | - | - | 1.333 (−12.53; 15.200) | 0.849 | 0.765 | - | 0.685 | - | |
| Effect on left cheek pressure | Nail biting | −0.448 (−3.118; 2.222) | 0.740 | −0.242 (−4.814; 4.330) | 0.917 | 5.500 (−1.431; 12.431) | 0.119 | −4.809 (−10.76; 1.139) | 0.112 | 0.939 | 0.116 | 0.188 | 0.027 * |
| Pen chewing | 1.709 (−3.410; 6.829) | 0.510 | 0.388 (−4.009; 4.784) | 0.862 | −3.400 (−9.661; 2.861) | 0.285 | 3.207 (−3.361; 9.774) | 0.336 | 0.700 | 0.214 | 0.723 | 0.152 | |
| Thumb sucking | −2.967 (−11.66; 5.723) | 0.501 | −2.357 (−14.67; 9.960) | 0.706 | −3.867 (−16.42; 8.687) | 0.543 | - | - | 0.936 | 0.907 | - | - | |
| Bruxism | −0.354 (−4.270; 3.562) | 0.859 | 0.392 (−6.911; 7.694) | 0.916 | - | - | 1.292 (−6.171; 8.755) | 0.733 | 0.859 | - | 0.700 | - | |
| Infantile swallowing | −0.067 (−2.653; 2.519) | 0.959 | −0.419 (−4.567; 3.728) | 0.842 | −5.167 (−12.16; 1.822) | 0.146 | 2.283 (−2.819; 7.385) | 0.378 | 0.887 | 0.178 | 0.418 | 0.091 | |
| Lip interposition | 1.033 (−2.412; 4.478) | 0.554 | −1.890 (−10.71; 6.927) | 0.672 | −3.867 (−16.47; 8.741) | 0.545 | −0.538 (−12.98; 11.902) | 0.932 | 0.542 | 0.460 | 0.810 | 0.711 | |
| Physiological tongue position at rest | 0.687 (−1.982; 3.357) | 0.611 | −1.591 (−5.240; 2.058) | 0.390 | −1.500 (−7.576; 4.576) | 0.626 | −1.643 (−6.236; 2.950) | 0.480 | 0.320 | 0.515 | 0.387 | 0.970 | |
| Caudal tongue position at rest | 1.158 (−1.621; 3.937) | 0.411 | 1.585 (−2.119; 5.289) | 0.399 | 1.500 (−4.581; 7.581) | 0.626 | 1.467 (−3.244; 6.177) | 0.539 | 0.855 | 0.920 | 0.911 | 0.993 | |
| Interdental tongue position at rest | −3.322 (−6.943; 0.299) | 0.072 | −1.419 (−13.55; 10.709) | 0.817 | - | - | −0.704 (−12.91; 11.506) | 0.909 | 0.767 | - | 0.685 | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Geneugden, L.; Verdonck, A.; Willems, G.; Hens, G.; Cadenas de Llano-Pérula, M. Relation between Maximum Oral Muscle Pressure and Dentoalveolar Characteristics in Patients with Cleft Lip and/or Palate: A Prospective Comparative Study. J. Clin. Med. 2023, 12, 4598. https://doi.org/10.3390/jcm12144598
Van Geneugden L, Verdonck A, Willems G, Hens G, Cadenas de Llano-Pérula M. Relation between Maximum Oral Muscle Pressure and Dentoalveolar Characteristics in Patients with Cleft Lip and/or Palate: A Prospective Comparative Study. Journal of Clinical Medicine. 2023; 12(14):4598. https://doi.org/10.3390/jcm12144598
Chicago/Turabian StyleVan Geneugden, Lisa, Anna Verdonck, Guy Willems, Greet Hens, and Maria Cadenas de Llano-Pérula. 2023. "Relation between Maximum Oral Muscle Pressure and Dentoalveolar Characteristics in Patients with Cleft Lip and/or Palate: A Prospective Comparative Study" Journal of Clinical Medicine 12, no. 14: 4598. https://doi.org/10.3390/jcm12144598
APA StyleVan Geneugden, L., Verdonck, A., Willems, G., Hens, G., & Cadenas de Llano-Pérula, M. (2023). Relation between Maximum Oral Muscle Pressure and Dentoalveolar Characteristics in Patients with Cleft Lip and/or Palate: A Prospective Comparative Study. Journal of Clinical Medicine, 12(14), 4598. https://doi.org/10.3390/jcm12144598









