Surgery and Prophylaxis with Susoctocog-Alfa in Acquired Hemophilia: Case Series and Literature Review
Abstract
1. Introduction
2. Materials and Methods
3. Case Reports and Results
3.1. Case Reports
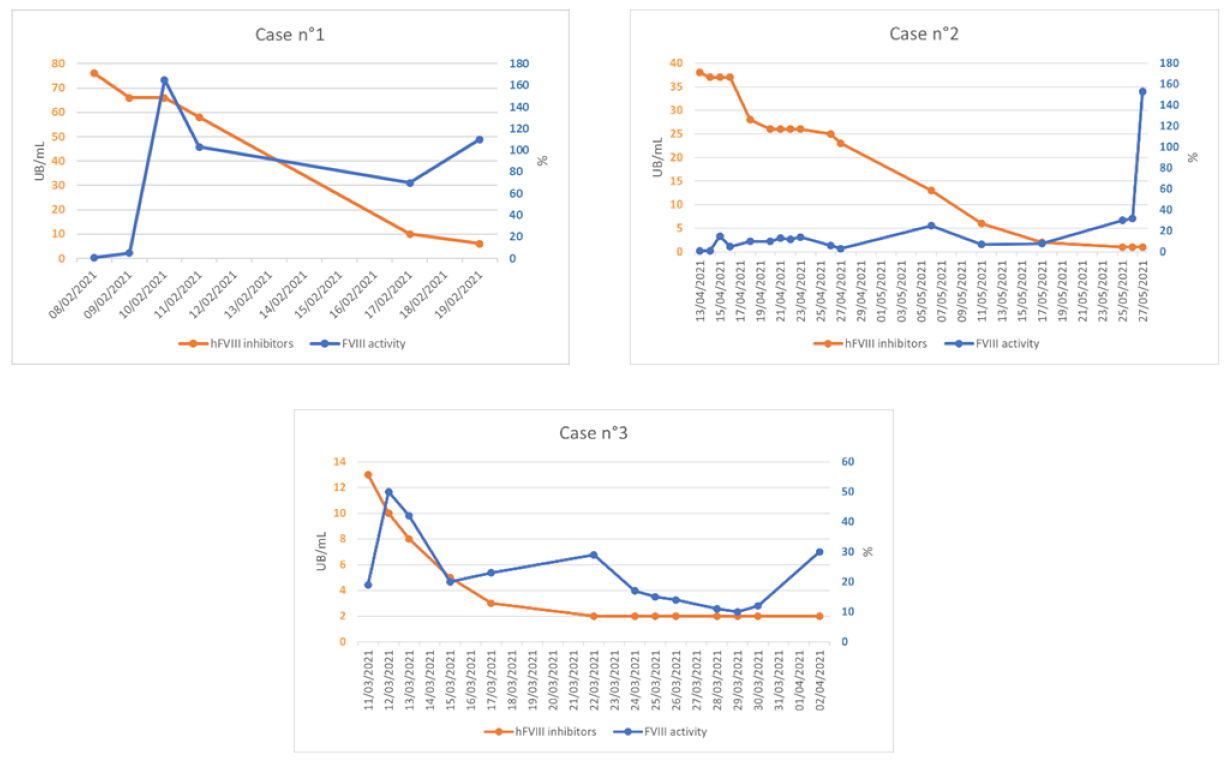
3.1.1. Case 1
3.1.2. Case 2
3.1.3. Case 3
3.2. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kruse-Jarres, R.; Kempton, C.L.; Baudo, F.; Collins, P.W.; Knoebl, P.; Leissinger, C.A.; Tiede, A.; Kessler, C.M. Acquired hemophilia A: Updated review of evidence and treatment guidance. Am. J. Hematol. 2017, 92, 695–705. [Google Scholar] [CrossRef]
- Coppola, A.; Franchini, M.; Tripodi, A.; Santoro, R.C.; Castaman, G.; Marino, R.; Zanon, E.; Santoro, C.; Rivolta, G.F.; Contino, L.; et al. Acquired haemophilia A: Italian Consensus Recommendations on diagnosis, general management and treatment of bleeding. Blood Transfus. 2022, 20, 245. [Google Scholar] [CrossRef]
- Radwi, M.; Farsi, S. A case report of acquired hemophilia following COVID-19 vaccine. J. Thromb. Haemost. 2021, 19, 1515–1518. [Google Scholar] [CrossRef] [PubMed]
- Franchini, M.; Glingani, C.; De Donno, G.; Casari, S.; Caruso, B.; Terenziani, I.; Perotti, C.; Del Fante, C.; Sartori, F.; Pagani, M. The first case of acquired hemophilia A associated with SARS-CoV-2 infection. Am. J. Hematol. 2020, 95, E197. [Google Scholar] [CrossRef] [PubMed]
- Collins, P.W.; Hirsch, S.; Baglin, T.P.; Dolan, G.; Hanley, J.; Makris, M.; Keeling, D.M.; Liesner, R.; Brown, S.A.; Hay, C.R.M.; et al. Acquired hemophilia A in the United Kingdom: A 2-year national surveillance study by the United Kingdom Haemophilia Centre Doctors’ Organisation. Blood 2006, 109, 1870–1877. [Google Scholar] [CrossRef] [PubMed]
- Knoebl, P.; Marco, P.; Baudo, F.; Collins, P.; Huth-Kühne, A.; Nemes, L.; Pellegrini, F.; Tengborn, L.; Lévesque, H.; EACH2 Registry Contributors. Demographic and clinical data in acquired hemophilia A: Results from the European Acquired Haemophilia Registry (EACH2). J. Thromb. Haemost. 2012, 10, 622–631. [Google Scholar] [CrossRef]
- Tiede, A.; Klamroth, R.; Scharf, R.E.; Trappe, R.U.; Holstein, K.; Huth-Kühne, A.; Gottstein, S.; Geisen, U.; Schenk, J.; Scholz, U.; et al. Prognostic factors for remission of and survival in acquired hemophilia A (AHA): Results from the GTH-AH 01/2010 study. Blood 2015, 125, 1091–1097. [Google Scholar] [CrossRef]
- Franchini, M.; Castaman, G.; Coppola, A.; Santoro, C.; Zanon, E.; Di Minno, G.; Morfini, M.; Santagostino, E.; Rocino, A. Acquired inhibitors of clotting factors: AICE recommendations for diagnosis and management. Blood Transfus. 2015, 13, 498–513. [Google Scholar] [CrossRef]
- Allegato, I. Riassunto delle Caratteristiche del Prodotto. Available online: https://www.ema.europa.eu/en/documents/product-information/obizur-epar-product-information_it.pdf (accessed on 21 July 2022).
- Kruse-Jarres, R.; St-Louis, J.; Greist, A.; Shapiro, A.; Smith, H.; Chowdary, P.; Drebes, A.; Gomperts, E.; Bourgeois, C.; Mo, M.; et al. Efficacy and safety of OBI-1, an antihaemophilic factor VIII (recombinant), porcine sequence, in subjects with acquired haemophilia A. Haemophilia 2015, 21, 162–170. [Google Scholar] [CrossRef]
- Ma, A.D.; Carrizosa, D. Acquired Factor VIII Inhibitors: Pathophysiology and Treatment. Hematology 2006, 2006, 432–437. [Google Scholar] [CrossRef]
- Astermark, J.; Donfield, S.M.; DiMichele, D.M.; Gringeri, A.; Gilbert, S.A.; Waters, J.; Berntorp, E.; FENOC Study Group. A randomized comparison of bypassing agents in hemophilia complicated by an inhibitor: The FEIBA NovoSeven Comparative (FENOC) Study. Blood 2006, 109, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Tiede, A.; Amano, K.; Ma, A.; Arkhammar, P.; El Fegoun, S.B.; Rosholm, A.; Seremetis, S.; Baudo, F. The use of recombinant activated factor VII in patients with acquired haemophilia. Blood Rev. 2015, 29, S19–S25. [Google Scholar] [CrossRef] [PubMed]
- Ma, A.D.; Kessler, C.M.; Al-Mondhiry, H.a.B.; Gut, R.Z.; Cooper, D.L. US experience with recombinant factor VIIa for surgery and other invasive procedures in acquired haemophilia: Analysis from the Hemostasis and Thrombosis Research Society Registry. Haemophilia 2016, 22, e18–e24. [Google Scholar] [CrossRef] [PubMed]
- Novembrino, C.; Quaglia, I.; Molinari, A.C.; Borchiellini, A.; Coppola, A.; Santoro, R.C.; Boscolo-Anzoletti, M.; Galbiati, E.; Zanon, E.; Valpreda, A. Analytical Performance of Different Laboratory Methods for Measuring Susoctocog-Alfa. Diagnostics 2022, 12, 1999. [Google Scholar] [CrossRef] [PubMed]
- Baudo, F.; Collins, P.; Huth-Kühne, A.; Lévesque, H.; Marco, P.; Nemes, L.; Pellegrini, F.; Tengborn, L.; Knoebl, P. Management of bleeding in acquired hemophilia A: Results from the European Acquired Haemophilia (EACH2) Registry. Blood 2012, 120, 39–46. [Google Scholar] [CrossRef]
- Sumner, M.J.; Geldziler, B.D.; Pedersen, M.; Seremetis, S. Treatment of acquired haemophilia with recombinant activated FVII: A critical appraisal. Haemophilia 2007, 13, 451–461. [Google Scholar] [CrossRef]
- Tarantino, M.D.; Cuker, A.; Hardesty, B.; Roberts, J.C.; Sholzberg, M. Recombinant porcine sequence factor VIII (rpFVIII) for acquired haemophilia A: Practical clinical experience of its use in seven patients. Haemophilia 2017, 23, 25–32. [Google Scholar] [CrossRef]
- Campbell, S.; Mason, J.; Prasad, R.; Ambrose, H.; Hunt, S.; Tran, H. Acquired haemophilia and haemostatic control with recombinant porcine factor VIII: Case series. Intern. Med. J. 2021, 51, 215–219. [Google Scholar] [CrossRef]
- Zanon, E.; Pasca, S.; Borchiellini, A.; Lodigiani, C.; Molinari, A.C.; Ambaglio, C.; Valeri, F.; Preti, P.S.; Moscatelli, P.; Simioni, P. Susoctocog-alfa (Obizur®) in the treatment of nine elderly patients with acquired haemophilia A: An Italian multicentre real world experience. Blood Transfus. 2020, 18, 312. [Google Scholar] [CrossRef]
- Ellsworth, P.; Chen, S.-L.; Kasthuri, R.S.; Key, N.S.; Mooberry, M.J.; Ma, A.D. Recombinant porcine FVIII for bleed treatment in acquired hemophilia A: Findings from a single-center, 18-patient cohort. Blood Adv. 2020, 4, 6240–6249. [Google Scholar] [CrossRef]
- Tiede, A.; Collins, P.; Knoebl, P.; Teitel, J.; Kessler, C.; Shima, M.; Minno, G.D.; d’Oiron, R.; Salaj, P.; Jiménez-Yuste, V.; et al. International recommendations on the diagnosis and treatment of acquired hemophilia A. Haematologica 2020, 105, 1791–1801. [Google Scholar] [CrossRef] [PubMed]
- Türkantoz, H.; Königs, C.; Knöbl, P.; Klamroth, R.; Holstein, K.; Huth-Kühne, A.; Heinz, J.; Eichler, H.; Tiede, A. Cross-reacting inhibitors against recombinant porcine factor VIII in acquired hemophilia A: Data from the GTH-AH 01/2010 Study. J. Thromb. Haemost. 2020, 18, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Bowyer, A.; Shepherd, F.; Platton, S.; Guy, S.; Kitchen, S.; Maclean, R. Cross-reacting recombinant porcine FVIII inhibitors in patients with acquired haemophilia A. Haemophilia 2020, 26, 1181–1186. [Google Scholar] [CrossRef]
- Zanon, E.; Pasca, S.; Spiezia, L.; Poletto, F.; Gherardi, S.; Simioni, P. Acquired haemophilia A, concomitant acute myocardial infarction and urgent major surgery: How to successfully treat a critical patient with rpFVIII (Obizur®). Thromb. Res. 2020, 195, 125–127. [Google Scholar] [CrossRef] [PubMed]
- Shatzel, J.J.; Azar, S.; Scherber, R.; Gay, N.; Deloughery, T.G.; VanSandt, A.; Kruse-Jarres, R.; Recht, M.; Taylor, J.A. Unexpected pharmacokinetics of recombinant porcine factor VIII in a patient with acquired factor VIII deficiency and spontaneous epidural haematoma. Haemophilia 2017, 23, e453–e456. [Google Scholar] [CrossRef] [PubMed]
- Martin, K.; Kasthuri, R.; Mooberry, M.J.; Chen, S.-L.; Key, N.S.; Ma, A.D. Lower doses of recombinant porcine factor VIII maintain excellent haemostatic efficacy. Haemophilia 2016, 22, e549–e551. [Google Scholar] [CrossRef]
- Buczma, A.; Baran, B.; Korwin, M.; Odnoczko, E.; Windyga, J. Successful perioperative prophylaxis with susoctocog alfa in a patient with acquired haemophilia A: A case study. Haemophilia 2022, 28, e39–e41. [Google Scholar] [CrossRef]
- Khan, D.; Raza-Burton, S.; Baker, P.; Harper, S.; Beavis, J.; Desborough, M.; Shapiro, S. Acquired haemophilia A treated with recombinant porcine factor VIII: A single centre UK experience. Br. J. Haematol. 2020, 189, e130–e133. [Google Scholar] [CrossRef]
- Zanon, E.; Pasca, S.; Siragusa, S.; Napolitano, M.; Santoro, C.; Mameli, L.; Rocino, A.; FAIR Study Group. Low dose of aPCC after the initial treatment in acquired haemophilia A is useful to reduce bleeding relapses: Data from the FAIR registry. Thromb. Res. 2019, 174, 24–26. [Google Scholar] [CrossRef]
- Pishko, A.M.; Doshi, B.S. Acquired Hemophilia A: Current Guidance and Experience from Clinical Practice. J. Blood Med. 2022, 13, 255–265. [Google Scholar] [CrossRef]
- Bowyer, A.; Gray, E.; Lowe, A.; Murphy, P.; Platton, S.; Riddell, A.; Chowdary, P.; Lester, W.; Jenkins, P.V. Laboratory coagulation tests and recombinant porcine factor VIII: A United Kingdom Haemophilia Centre Doctors’ Organisation guideline. Haemophilia 2022, 28, 515–519. [Google Scholar] [CrossRef] [PubMed]
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Gender | Female | Male | Female |
| Age (years) | 70 | 79 | 31 |
| Comorbidities | Myasthenia gravis, Hashimoto Thyroiditis and Glaucoma | Gastric Carcinoma, Urothelial neoplasia, Polymyalgia rheumatica | Episode of major depression after son’s death |
| Thromboembolic risk factor | Surgery, age, prolonged immobilization | Surgery, neoplasia, age, prolonged immobilization | Post-partum |
| Bleeding type/site | Right-upper-limb Hematoma | Ilio-psoas hematoma, upper and lower limbs hematomas, hematuria | 1 Right-lower-limb hematoma; 2 ilio-psoas hematomas |
| Surgery during AHA | Left hemicolectomy with terminal stomia | Tissue biopsy and laser ablation in the nearby region of neoplastic lesion | None |
| aPTT ratio | 3.07 | 2.57 | 1 3.26; 2 1.8 |
| FVIII at diagnosis (%) | 0.9 | 1.7 | 1 1; 2 19 |
| hFVIII inhibitors titer (UB/mL) | 76 | 23 | 1 64; 2 11.2 |
| rpFVIII inhibitors titer Pre-therapy (UB/mL) | 44 | 12 | 11 |
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Lines of IST | 2 | 3 | 1 |
| Type of IST | Steroid, cyclophosphamide | Steroid, cyclophosphamide and rituximab | Steroid |
| First hemostatic therapy with rFVIIa dose (mcg/kg) | 90 | 90 | 90 |
| Days on rFVIIa treatment | 4 | 5 | 1 7 and 2 3 |
| Second hemostatic therapy | rpFVIII | rpFVIII | rpFVIII |
| rpFVIII loading dose (U/kg) | 200 | 200 | 200 |
| Recovery FVIII level within 1 h (%) | 125 | 94 | 213 |
| rpFVIII following dose (U/kg) | 200 | 100 | 100 |
| FVIII trough level (%) | 60 | 10 | 30 |
| Treatment schedule | Prolongation of administration interval (every 12–36–48 h) until ending | Full dose and half dose on alternate days and then half dose until ending | Half dose starting from 36 h after first dose, then half dose every other day |
| Days on rpFVIII treatment | 11 | 44 | 22 |
| Total treatment dose (U) | 125.000 | 155.000 | 55.000 |
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Hb at diagnosis (g/dL) | 9.1 | 7.4 | 1 6; 2 9.2 |
| RBC transfusions (n°) | 3 | 2 | 2 |
| RBC transfusion after first dose of rpFVIII (n°) | 0 | 0 | 0 |
| Increase in inhibitor rpFVIII titer | No | No | Yes |
| Thromboembolic events | None | None | None |
| Hb at discharge (g/dL) | 9.3 | 10.5 | 1 8.9; 2 10.5 |
| Bleeding relapse | No | No | No |
| Case 1 | Case 2 | Zanon et al. [25] | Buczuma et al. [28] | |
|---|---|---|---|---|
| Weight (kg) | 57.5 | 50 | 80 | 69 |
| Total dose (U) | 125.000 | 5000 | 136.000 | 108.000 |
| Total exposures (days) | 11 | 1 | 15 | 8 |
| Total dose for weight (U/kg) | 2174 | 100 | 1700 | 1565 |
| Total dose for day (U/die) | 11,364 | 5000 | 9067 | 13,500 |
| Total dose for weight for day (U/kg/die) | 198 | 100 | 113 | 196 |
| FVIII level at diagnosis (%) | 0.9 | 1.7 | <1 | N/A |
| hFVIII inhibitors titer (UB/mL) | 76 | 23 | 110 | 0.64 |
| Recovery FVIII level within 1 h (%) | 125 | 94 | 51 | 173 |
| Case 3 | Tarantino et al. [18] | Tarantino et al. [18] | |
|---|---|---|---|
| Weight (kg) | 55 | 72 | 97 |
| Total dose (U) | 55.000 | 149.760 | 63.064 |
| Total exposures (days) | 22 | 26 | 14 |
| Total exposures as outpatient (days) | 16 | 16 | 6 |
| Total dose for weight (U/kg) | 1000 | 2080 | 650 |
| Total dose for day (U/die) | 2500 | 5760 | 4505 |
| Total dose for weight for day (U/kg/die) | 45 | 80 | 46 |
| FVIII level at diagnosis (%) | 1 | <1 | <1 |
| hFVIII inhibitors titer (UB/mL) | 64 | 32 | N/A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sella, C.; Bardetta, M.; Valeri, F.; Dainese, C.; Valpreda, A.; Massaia, M.; Grimaldi, D.; Porreca, A.; Bruno, B.; Borchiellini, A. Surgery and Prophylaxis with Susoctocog-Alfa in Acquired Hemophilia: Case Series and Literature Review. J. Clin. Med. 2023, 12, 4590. https://doi.org/10.3390/jcm12144590
Sella C, Bardetta M, Valeri F, Dainese C, Valpreda A, Massaia M, Grimaldi D, Porreca A, Bruno B, Borchiellini A. Surgery and Prophylaxis with Susoctocog-Alfa in Acquired Hemophilia: Case Series and Literature Review. Journal of Clinical Medicine. 2023; 12(14):4590. https://doi.org/10.3390/jcm12144590
Chicago/Turabian StyleSella, Carola, Marco Bardetta, Federica Valeri, Cristina Dainese, Alessandra Valpreda, Massimo Massaia, Daniele Grimaldi, Annamaria Porreca, Benedetto Bruno, and Alessandra Borchiellini. 2023. "Surgery and Prophylaxis with Susoctocog-Alfa in Acquired Hemophilia: Case Series and Literature Review" Journal of Clinical Medicine 12, no. 14: 4590. https://doi.org/10.3390/jcm12144590
APA StyleSella, C., Bardetta, M., Valeri, F., Dainese, C., Valpreda, A., Massaia, M., Grimaldi, D., Porreca, A., Bruno, B., & Borchiellini, A. (2023). Surgery and Prophylaxis with Susoctocog-Alfa in Acquired Hemophilia: Case Series and Literature Review. Journal of Clinical Medicine, 12(14), 4590. https://doi.org/10.3390/jcm12144590






