Performing Advanced Trauma Life Support (ATLS) across Borders: Midterm Follow-Up of the Aeromedical Evacuation after Civilian Bus Accident at Madeira
Abstract
1. Introduction
2. Materials and Methods
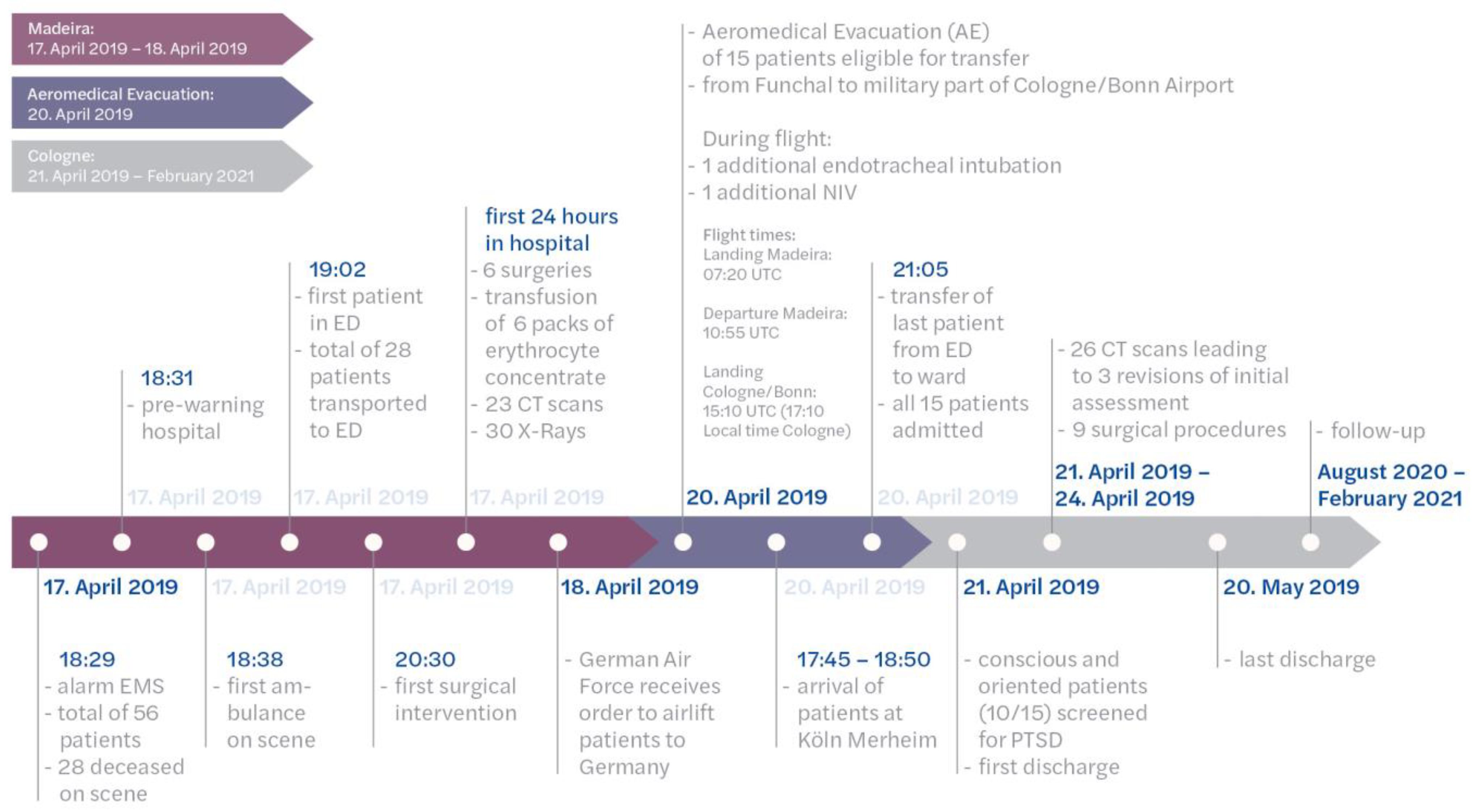
2.1. Madeira
2.2. Description of the Aeromedical Evacuation German Air Force
2.3. Cologne
2.4. Follow-Up
2.5. Statistical Analysis
3. Results
3.1. Patients
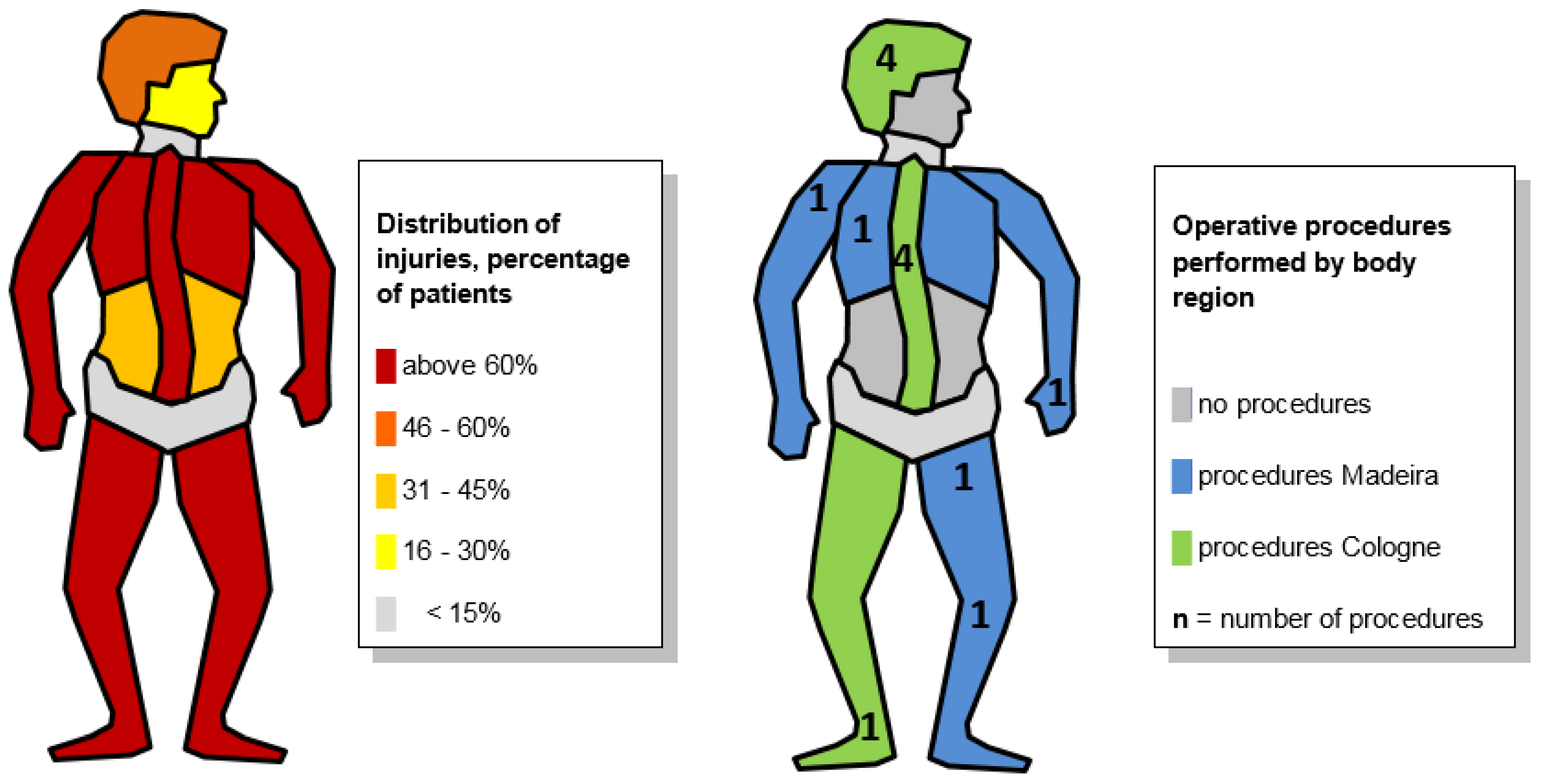
3.2. Madeira Perspective
- -
- Orthopedic trauma to limbs and pelvis: multiple cases
- -
- Head trauma: one patient with severe traumatic brain injury died in the ICU, and another had severe craniofacial trauma
- -
- Thoracic trauma: two patients had pulmonary contusions and hemothorax
- -
- Abdominal trauma: one patient with traumatic duodenal laceration was laparatomized
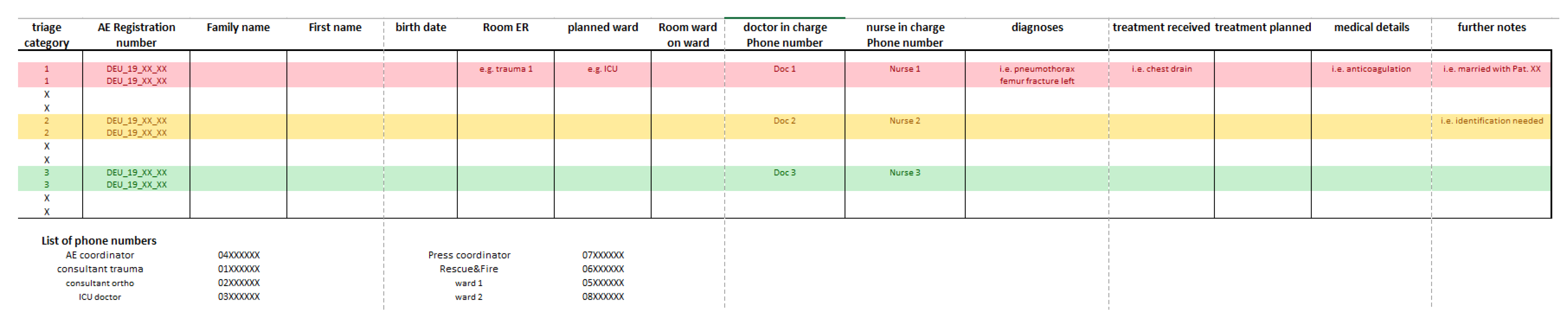
3.3. AE Perspective
3.4. Cologne Perspective
3.5. Follow-Up Patients
4. Discussion
4.1. Madeira, Portugal
4.2. Cologne, Germany
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maegele, M.; Gregor, S.; Steinhausen, E.; Bouillon, B.; Heiss, M.; Perbix, W.; Wappler, F.; Rixen, D.; Geisen, J.; Berger-Schreck, B.; et al. The long-distance tertiary air transfer and care of tsunami victims: Injury pattern and microbiological and psychological aspects. Crit. Care Med. 2005, 33, 1136–1140. [Google Scholar] [PubMed]
- Moecke, H.P.; Anding, K. Intensivtransportprotokoll. Notf. Rett. 2000, 3, 441–444. [Google Scholar]
- Stieglitz, R.-D.; Nyberg, E.; Albert, M.; Frommberger, U.; Berger, M. Entwicklung eines Screeninginstrumentes zur Identifizierung von Risikopatienten für die Entwicklung einer Posttraumatischen Belastungsstörung (PTB) nach einem Verkehrsunfall. Z. Klin. Psychol. Psychother. 2002, 31, 22–30. [Google Scholar]
- Schneider, A.; Lefering, R.; Neugebauer, E. Examination of quality criteria of the Freiburger Screening Fragebogen to identify patients at risk for the development of a post-traumatic stress disorder in the group of severely injured accident patients. Z. Psychiatr. Psychol. Psychother. 2011, 3, 241–250. [Google Scholar]
- Wirtz, M.A.; Morfeld, M.; Glaesmer, H.; Brähler, E. Normierung des SF-12 Version 2.0 zur Messung der gesundheitsbezogenen Lebensqualität in einer deutschen bevölkerungsrepräsentativen Stichprobe. Diagnostica 2018, 64, 3. [Google Scholar]
- Kamp, O.; Pfeifer, R.; Ritschel, M.; Flohe, S.; Bieler, D. Polytrauma outcome: Implementation of health-related quality of life assessment into the German Trauma Registry. Eur. J. Trauma Emerg. Surg. 2019, 47, 869–874. [Google Scholar]
- Brom, D.; Stokar, Y.; Lawi, C.; Nuriel-Porat, V.; Ziv, Y.; Lerner, K.; Ross, G. Somatic Experiencing for Posttraumatic Stress Disorder: A Randomized Controlled Outcome Study. J. Trauma. Stress 2017, 30, 304–312. [Google Scholar]
- Andersen, T.E.; Lahav, Y.; Ellegaard, H.; Manniche, C. A randomized controlled trial of brief Somatic Experiencing for chronic low back pain and comorbid post-traumatic stress disorder symptoms. Eur. J. Psychotraumatol. 2017, 8, 1331108. [Google Scholar]
- Münzberg, M.; Mutschler, M.; Paffrath, T.; Trentzsch, H.; Wafaisade, A.; Walcher, F.; Raum, M.; Flohé, S.; Wölfl, C. Level of Evidence Analysis for the Latest German National Guideline on Treatment of Patients with Severe and Multiple Injuries and ATLS. World J. Surg. 2015, 39, 2061–2067. [Google Scholar]
- Henry, S. ATLS 10th edition offers new insights into managing trauma patients. Bulletin of the American College of Surgeons, 1 June 2018. [Google Scholar]
- Navarro, S.; Montmany, S.; Rebasa, P.; Colilles, C.; Pallisera, A. Impact of ATLS Training on Preventable and Potentially Preventable Deaths. World J. Surg. 2014, 38, 2273–2278. [Google Scholar]
- Huber-Wagner, S.; Lefering, R.; Qvick, L.-M.; Körner, M.; Kay, M.V.; Pfeifer, K.-J.; Reiser, M.; Mutschler, W.; Kanz, K.-G. Effect of whole-body CT during trauma resuscitation on survival: A retrospective, multicentre study. Lancet 2009, 373, 1455–1461. [Google Scholar] [PubMed]
- Reinhold, M.; Audigé, L.; Schnake, K.J.; Bellabarba, C.; Dai, L.-Y.; Oner, F.C. AO spine injury classification system: A revision proposal for the thoracic and lumbar spine. Eur. Spine J. 2013, 22, 2184–2201. [Google Scholar] [PubMed]
- Kepler, C.K.; Vaccaro, A.R.; Koerner, J.D.; Dvorak, M.F.; Kandziora, F.; Rajasekaran, S.; Aarabi, B.; Vialle, L.R.; Fehlings, M.G.; Schroeder, G.D.; et al. Reliability analysis of the AOSpine thoracolumbar spine injury classification system by a worldwide group of naïve spinal surgeons. Eur. Spine J. 2016, 25, 1082–1086. [Google Scholar]
- Banaste, N.; Caurier, B.; Bratan, F.; Bergerot, J.-F.; Thomson, V.; Millet, I. Whole-Body CT in Patients with Multiple Traumas: Factors Leading to Missed Injury. Radiology 2018, 289, 374–383. [Google Scholar] [PubMed]
- Antevil, J.L.; Sise, M.J.; Sack, D.I.; Kidder, B.; Hopper, A.; Brown, C.V.R. Spiral Computed Tomography for the Initial Evaluation of Spine Trauma: A New Standard of Care? J. Trauma Acute Care Surg. 2006, 61, 382–387. [Google Scholar]
- Eurin, M.; Haddad, N.; Zappa, M.; Lenoir, T.; Dauzac, C.; Vilgrain, V.; Mantz, J.; Paugam-Burtz, C. Incidence and predictors of missed injuries in trauma patients in the initial hot report of whole-body CT scan. Injury 2012, 43, 73–77. [Google Scholar]
- Bernstein, M.P.; Mirvis, S.E.; Shanmuganathan, K. Chance-Type Fractures of the Thoracolumbar Spine: Imaging Analysis in 53 Patients. Am. J. Roentgenol. 2006, 187, 859–868. [Google Scholar]
- Chapman, J.; Bransford, R. Geriatric Spine Fractures: An Emerging Healthcare Crisis. J. Trauma Acute Care Surg. 2007, 62, S61–S62. [Google Scholar]
- Sammito, S.; Post, J.; Ritter, D.M.; Hossfeld, B.; Erley, O.M. Innereuropäische Aeromedical-Evacuation-Transporte im Rahmen von COVID-19. Notarzt 2020, 36, 263–270. [Google Scholar]
- Van Vledder, M.G.; Kwakernaak, V.; Hagenaars, T.; Van Lieshout, E.M.M.; On behalf of the South West Netherlands Trauma Region Study Group. Patterns of injury and outcomes in the elderly patient with rib fractures: A multicenter observational study. Eur. J. Trauma Emerg. Surg. 2019, 45, 575–583. [Google Scholar]
- Tecic, T.; Schneider, A.; Althaus, A.; Schmidt, Y.; Bierbaum, C.; Lefering, R.; Mueller, D.; Bouillon, B.; Janssen, C.; Pfaff, H.; et al. Early Short-Term Inpatient Psychotherapeutic Treatment versus Continued Outpatient Psychotherapy on Psychosocial Outcome: A Randomized Controlled Trial in Trauma Patients. J. Trauma Inj. Infect. Crit. Care 2011, 70, 433–441. [Google Scholar]
- Steenkamp, M.M.; Litz, B.T.; Hoge, C.W.; Marmar, C.R. Psychotherapy for Military-Related PTSDA Review of Randomized Clinical Trials. JAMA 2015, 314, 489–500. [Google Scholar] [PubMed]
- Bandelow, B.; Koch, M.; Zimmermann, P.; Biesold, K.-H.; Wedekind, D.; Falkai, P. Posttraumatic stress disorder (PTSD) in the German Armed Forces: A retrospective study in inpatients of a German army hospital. Eur. Arch. Psychiatry Clin. Neurosci. 2012, 262, 459–467. [Google Scholar] [PubMed]
- World Health Organisation. Mass Casualty Management Systems: Strategies and Guidelines for Building Health Sector Capacity. 2007. Available online: https://apps.who.int/iris/bitstream/handle/10665/43804/9789241596053_eng.pdf (accessed on 1 July 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Imach, S.; Deschler, A.; Sammito, S.; Reis, M.; Michaelis, S.; Marche, B.; Paffrath, T.; Bouillon, B.; Tjardes, T. Performing Advanced Trauma Life Support (ATLS) across Borders: Midterm Follow-Up of the Aeromedical Evacuation after Civilian Bus Accident at Madeira. J. Clin. Med. 2023, 12, 4556. https://doi.org/10.3390/jcm12144556
Imach S, Deschler A, Sammito S, Reis M, Michaelis S, Marche B, Paffrath T, Bouillon B, Tjardes T. Performing Advanced Trauma Life Support (ATLS) across Borders: Midterm Follow-Up of the Aeromedical Evacuation after Civilian Bus Accident at Madeira. Journal of Clinical Medicine. 2023; 12(14):4556. https://doi.org/10.3390/jcm12144556
Chicago/Turabian StyleImach, Sebastian, Andreas Deschler, Stefan Sammito, Miguel Reis, Sylta Michaelis, Beneditk Marche, Thomas Paffrath, Bertil Bouillon, and Thorsten Tjardes. 2023. "Performing Advanced Trauma Life Support (ATLS) across Borders: Midterm Follow-Up of the Aeromedical Evacuation after Civilian Bus Accident at Madeira" Journal of Clinical Medicine 12, no. 14: 4556. https://doi.org/10.3390/jcm12144556
APA StyleImach, S., Deschler, A., Sammito, S., Reis, M., Michaelis, S., Marche, B., Paffrath, T., Bouillon, B., & Tjardes, T. (2023). Performing Advanced Trauma Life Support (ATLS) across Borders: Midterm Follow-Up of the Aeromedical Evacuation after Civilian Bus Accident at Madeira. Journal of Clinical Medicine, 12(14), 4556. https://doi.org/10.3390/jcm12144556





