“Multiple Mode Procedures” of Ultra-Pulse Fractional CO2 Laser: A Novel Treatment Modality of Facial Atrophic Acne Scars
Abstract
1. Introduction
2. Methods
2.1. Clinical Data
2.2. Treatment Procedures
2.2.1. Preoperative Preparation
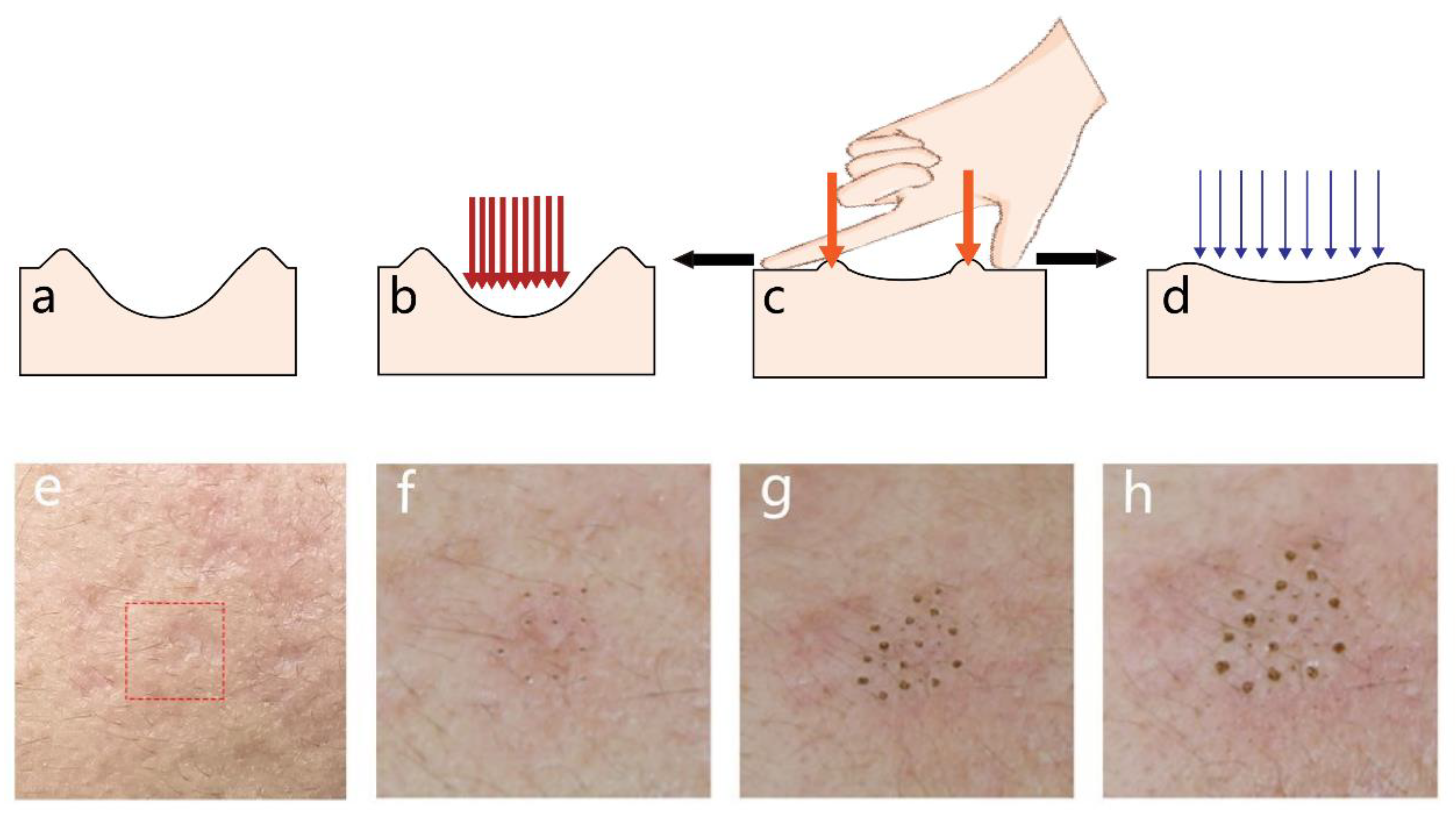
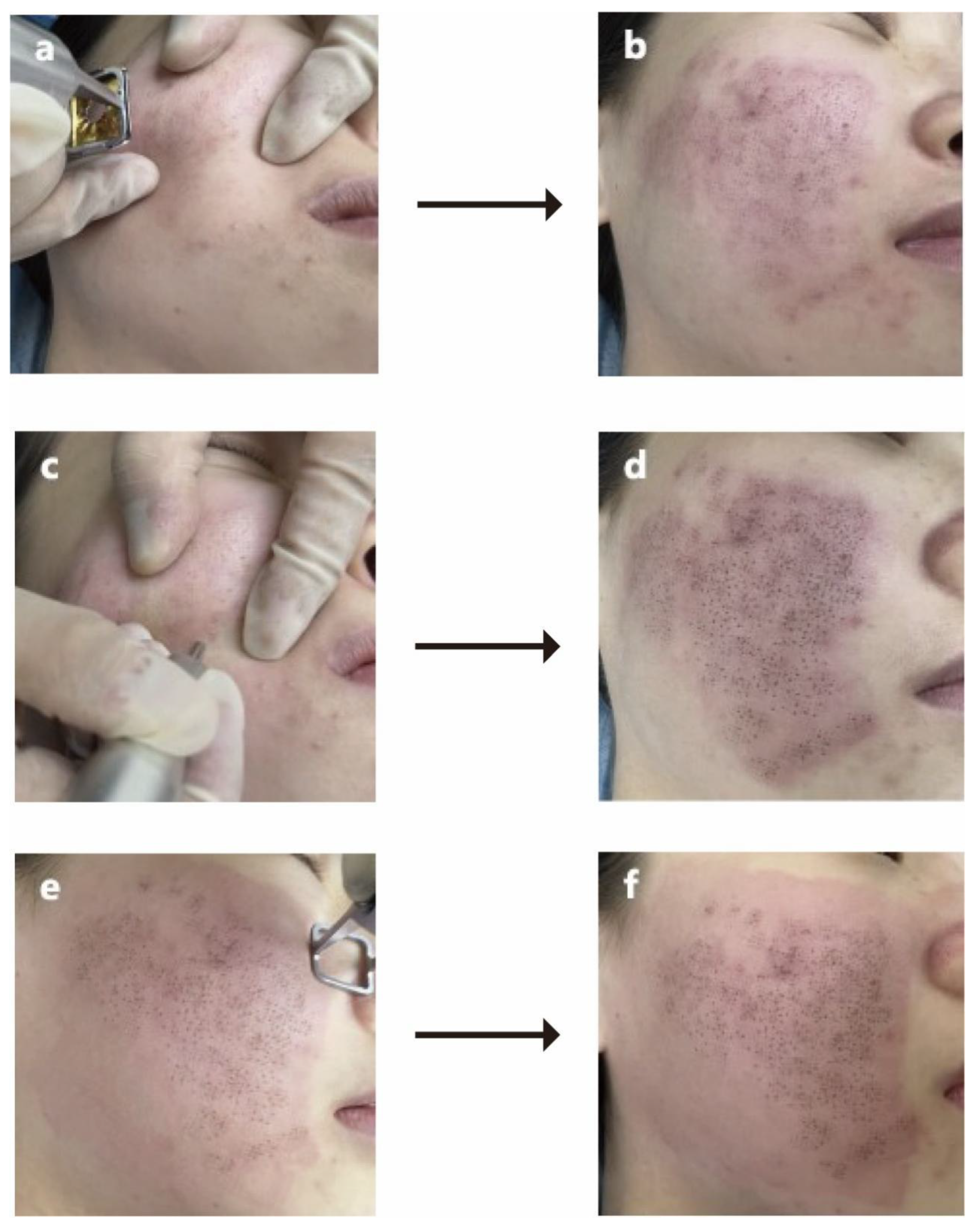
2.2.2. Details of MMP Technique
FFLT
MFT
Fractional Laser
2.2.3. Postoperative Care
2.3. Assessment of Clinical Characteristics
2.4. Statistic Analysis
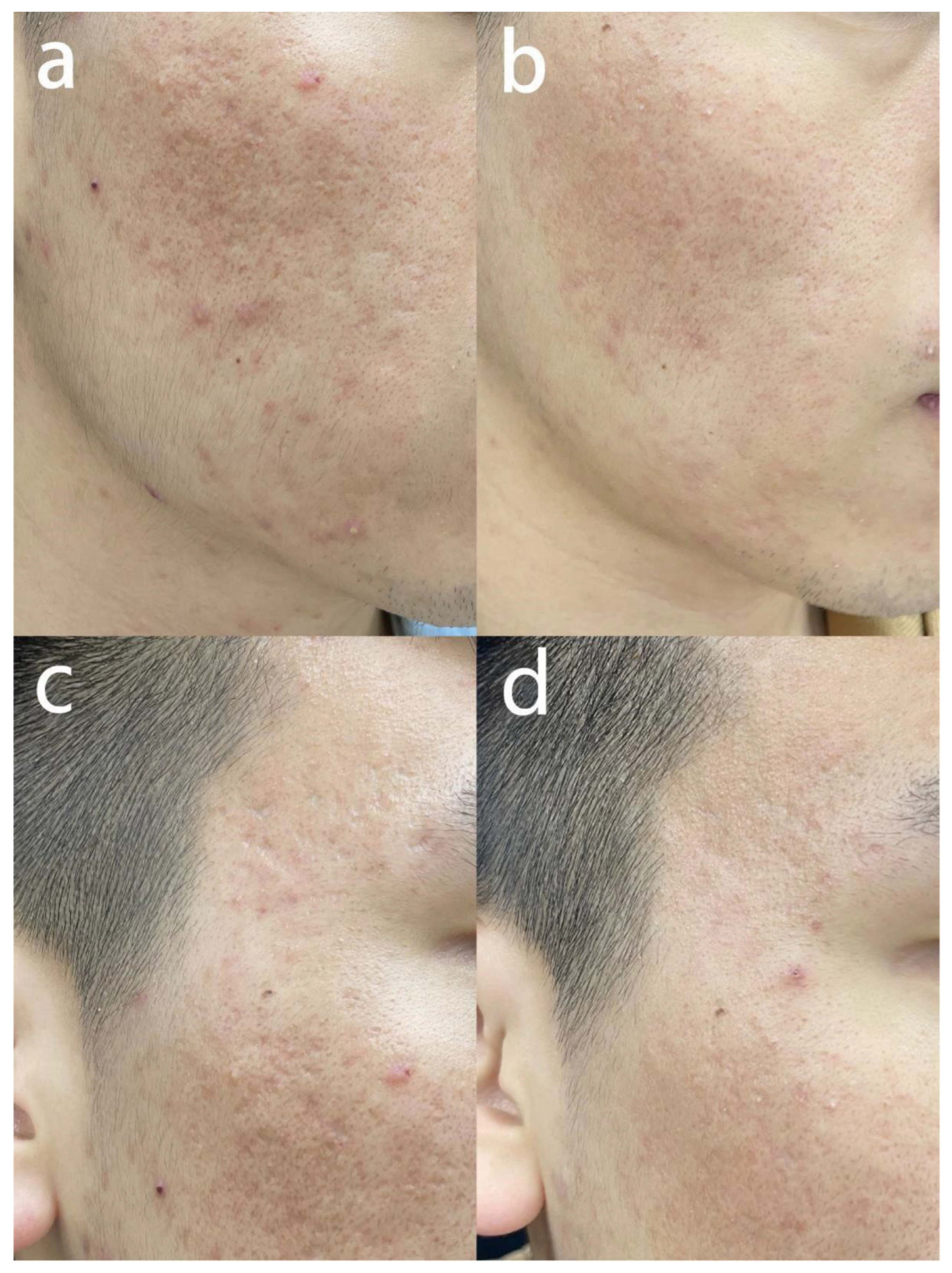
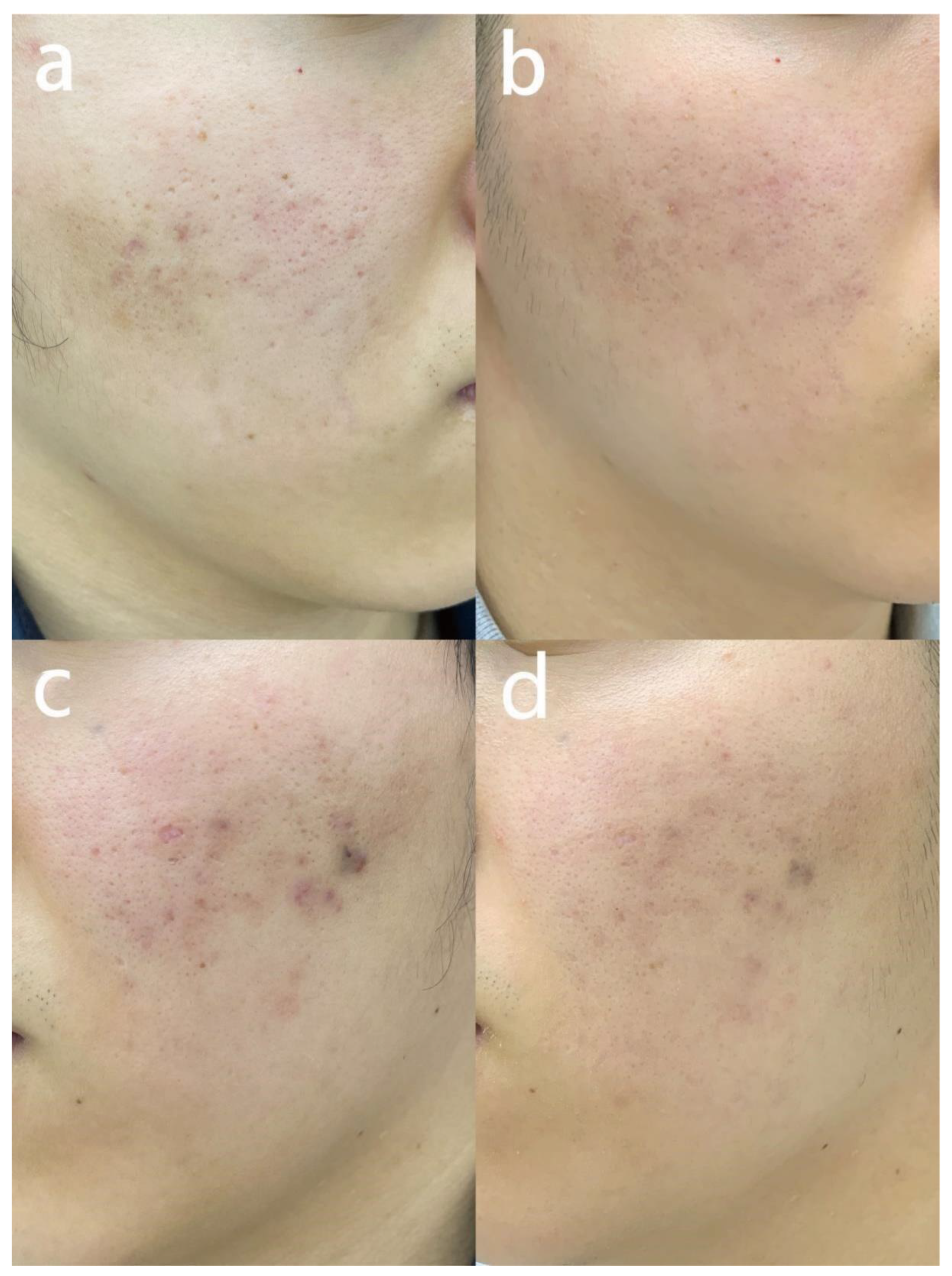
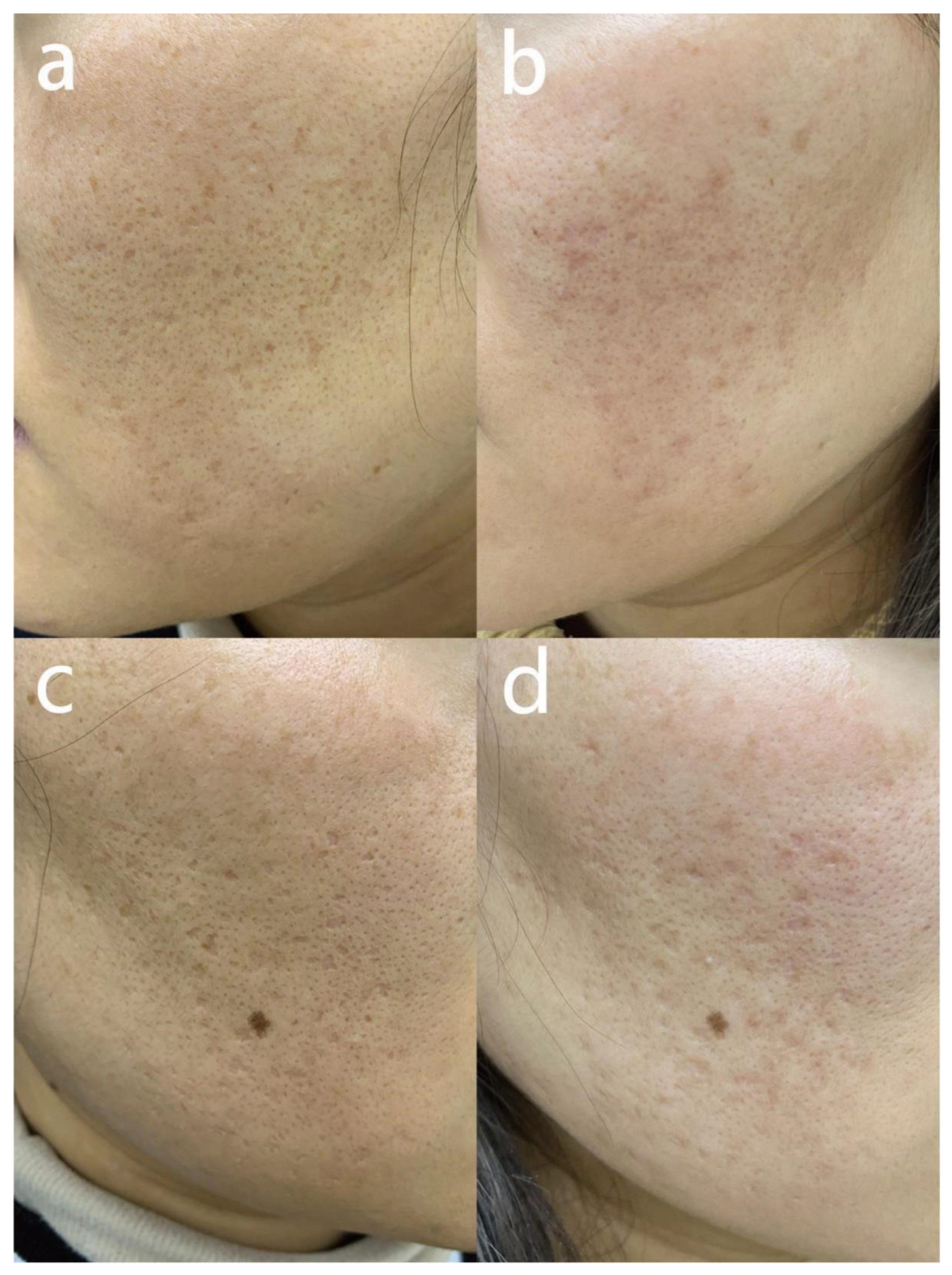
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lynn, D.D.; Umari, T.; Dunnick, C.A.; Dellavalle, R.P. The epidemiology of acne vulgaris in late adolescence. Adolesc. Health Med. Ther. 2016, 7, 13–25. [Google Scholar] [CrossRef]
- Thiboutot, D.M.; Dréno, B.; Abanmi, A.; Alexis, A.F.; Araviiskaia, E.; Barona Cabal, M.I.; Bettoli, V.; Casintahan, F.; Chow, S.; da Costa, A.; et al. Practical management of acne for clinicians: An international consensus from the Global Alliance to Improve Outcomes in Acne. J. Am. Acad. Dermatol. 2018, 78 (Suppl. 1), S1–S23.e1. [Google Scholar] [CrossRef]
- Abad-Casintahan, F.; Chow, S.K.; Goh, C.L.; Kubba, R.; Hayashi, N.; Noppakun, N.; See, J.; Suh, D.H.; Xiang, L.H.; Kang, S. Frequency and characteristics of acne-related post-inflammatory hyperpigmentation. J. Dermatol. 2016, 43, 826–828. [Google Scholar] [CrossRef]
- Connolly, D.; Vu, H.L.; Mariwalla, K.; Saedi, N. Acne Scarring-Pathogenesis, Evaluation, and Treatment Options. J. Clin. Aesthetic Dermatol. 2017, 10, 12–23. [Google Scholar]
- Clark, A.K.; Saric, S.; Sivamani, R.K. Acne Scars: How Do We Grade Them? Am. J. Clin. Dermatol. 2018, 19, 139–144. [Google Scholar] [CrossRef]
- Samuels, D.V.; Rosenthal, R.; Lin, R.; Chaudhari, S.; Natsuaki, M.N. Acne vulgaris and risk of depression and anxiety: A meta-analytic review. J. Am. Acad. Dermatol. 2020, 83, 532–541. [Google Scholar] [CrossRef]
- Khorasani, M.; Gibson, I.; Ghasemi, A.H.; Hadavi, E.; Rolfe, B. Laser subtractive and laser powder bed fusion of metals: Review of process and production features. Rapid Prototyp. J. 2023, 29, 935–958. [Google Scholar] [CrossRef]
- Manstein, D.; Herron, G.S.; Sink, R.K.; Tanner, H.; Anderson, R.R. Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg. Med. 2004, 34, 426–438. [Google Scholar] [CrossRef]
- Sobanko, J.F.; Alster, T.S. Management of acne scarring, part I: A comparative review of laser surgical approaches. Am. J. Clin. Dermatol. 2012, 13, 319–330. [Google Scholar] [CrossRef]
- Prignano, F.; Campolmi, P.; Bonan, P.; Ricceri, F.; Cannarozzo, G.; Troiano, M.; Lotti, T. Fractional CO2 laser: A novel therapeutic device upon photobiomodulation of tissue remodeling and cytokine pathway of tissue repair. Dermatol. Ther. 2009, 22 (Suppl. 1), S8–S15. [Google Scholar] [CrossRef]
- Prado, A.; Andrades, P.; Danilla, S.; Benitez, S.; Reyes, S.; Valenzuela, G.; Guridi, R.; Fuentes, P. Full-face carbon dioxide laser resurfacing: A 10-year follow-up descriptive study. Plast. Reconstr. Surg. 2008, 121, 983–993. [Google Scholar] [CrossRef]
- Wang, Y.; Yu, W.; Zhang, J.; Li, J. Effect and Safety Analysis of PRP and Yifu Combined with Ultrapulsed CO2 Lattice Laser in Patients with Sunken Acne Scar. J. Healthc. Eng. 2022, 2022, 6803988. [Google Scholar] [CrossRef]
- Kang, W.H.; Kim, Y.J.; Pyo, W.S.; Park, S.J.; Kim, J.H. Atrophic acne scar treatment using triple combination therapy: Dot peeling, subcision and fractional laser. J. Cosmet. Laser Ther. 2009, 11, 212–215. [Google Scholar] [CrossRef]
- Jin, W.; Li, Z.; Jin, Z.; Jin, C. A novel technique for treating atrophic facial scars in Asians using ultra-pulse CO2 laser. J. Cosmet. Dermatol. 2020, 19, 1099–1104. [Google Scholar] [CrossRef]
- Li, B.; Ren, K.; Yin, X.; She, H.; Liu, H.; Zhou, B. Efficacy and adverse reactions of fractional CO2 laser for atrophic acne scars and related clinical factors: A retrospective study on 121 patients. J. Cosmet. Dermatol. 2022, 21, 1989–1997. [Google Scholar] [CrossRef]
- Fang, F.; Yang, H.; Liu, X.; Ding, H.; Yang, Y.; Ge, Y.; Lin, T. Treatment of acne scars with fractional carbon dioxide laser in Asians: A retrospective study to search for predicting factors associated with efficacy. Lasers Med. Sci. 2022, 37, 2623–2627. [Google Scholar] [CrossRef]
- Preissig, J.; Hamilton, K.; Markus, R. Current Laser Resurfacing Technologies: A Review that Delves Beneath the Surface. Semin. Plast. Surg. 2012, 26, 109–116. [Google Scholar] [CrossRef]
- Hongjin, W.; Bingrong, Z.; Shufen, X.; Jiaan, Z.; Jin, L.; Juan, L.; Fei, Y.; Shen, W.; Lichao, Z.; Dan, L. The efficacy and adverse reactions of fractional CO2 laser for treatment of atrophic acne scars. Chin. J. Dermatol. 2015, 48, 881–885. [Google Scholar]
- Zhang, J.A.; Liu, J.; Wu, H.J.; Xu, Y.; Si, C.C.; Zhou, B.R.; Luo, D. The effects of Antimicrobial Peptides and Hyaluronic Acid compound mask on wound healing after ablative fractional Carbon Dioxide laser resurfacing. J. Cosmet. Laser Ther. 2019, 21, 217–224. [Google Scholar] [CrossRef]
- Lei, Y.; Li, S.F.; Yu, Y.L.; Tan, J.; Gold, M.H. Clinical efficacy of utilizing Ultrapulse CO2 combined with fractional CO2 laser for the treatment of hypertrophic scars in Asians-A prospective clinical evaluation. J. Cosmet. Dermatol. 2017, 16, 210–216. [Google Scholar] [CrossRef]
- Dreno, B.; Khammari, A.; Orain, N.; Noray, C.; Mérial-Kieny, C.; Méry, S.; Nocera, T. ECCA grading scale: An original validated acne scar grading scale for clinical practice in dermatology. Dermatology 2007, 214, 46–51. [Google Scholar] [CrossRef]
- Beausang, E.; Floyd, H.; Dunn, K.W.; Orton, C.I.; Ferguson, M.W. A new quantitative scale for clinical scar assessment. Plast. Reconstr. Surg. 1998, 102, 1954–1961. [Google Scholar] [CrossRef]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of Digital Visual Analog Scale Pain Scoring With a Traditional Paper-based Visual Analog Scale in Adults. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e088. [Google Scholar] [CrossRef]
- Zhang, D.D.; Zhao, W.Y.; Fang, Q.Q.; Wang, Z.C.; Wang, X.F.; Zhang, M.X.; Hu, Y.Y.; Zheng, B.; Tan, W.Q. The efficacy of fractional CO2 laser in acne scar treatment: A meta-analysis. Dermatol. Ther. 2021, 34, e14539. [Google Scholar] [CrossRef]
- Fabbrocini, G.; Cacciapuoti, S.; Fardella, N.; Pastore, F.; Monfrecola, G. CROSS technique: Chemical reconstruction of skin scars method. Dermatol. Ther. 2008, 21 (Suppl. 3), S29–S32. [Google Scholar] [CrossRef]
- Schweiger, E.S.; Sundick, L. Focal Acne Scar Treatment (FAST), a new approach to atrophic acne scars: A case series. J. Drugs Dermatol. 2013, 12, 1163–1167. [Google Scholar]
- Qin, L.; Kaiping, Z.; Jianbo, W.; Yuehua, Y.; Guifeng, X.; Jiquan, S. The efficacy and security of focal fractional laser in treatment of atrophic acne scars. Chin. J. Med. Aesthet. Cosmetol. 2019, 25, 71–73. [Google Scholar]
- Asilian, A.; Salimi, E.; Faghihi, G.; Dehghani, F.; Tajmirriahi, N.; Hosseini, S.M. Comparison of Q-Switched 1064-nm Nd: YAG laser and fractional CO2 laser efficacies on improvement of atrophic facial acne scar. J. Res. Med. Sci. 2011, 16, 1189–1195. [Google Scholar]
- Kim, D.H.; Ryu, H.J.; Choi, J.E.; Ahn, H.H.; Kye, Y.C.; Seo, S.H. A comparison of the scar prevention effect between carbon dioxide fractional laser and pulsed dye laser in surgical scars. Dermatol. Surg. 2014, 40, 973–978. [Google Scholar] [CrossRef]
- Lee, C.J.; Whang, J.H.; Lazova, R.; Ciesielski, T.E.; Thomson, J.G.; McCarthy, T.; Persing, J.A. Growth factor expression with different wound treatments after laser resurfacing. Aesthetic Surg. J. 2007, 27, 55–64. [Google Scholar]
| Mean ± SD | |
|---|---|
| Age (Years) | 28.6 ± 5.1 |
| ECCA scores before treatment | 162.7 ± 47.6 |
| Duration (Years) | 10.1 ± 5.1 |
| N (%) | |
| Gender | |
| Female | 83 (80.6%) |
| Male | 20 (19.4%) |
| Scar type | |
| Boxcar | 49 (47.6%) |
| Icepick | 35 (34.0%) |
| Rolling | 19 (18.4%) |
| Accompanied by active acne lesions | |
| Yes | 14 (13.6%) |
| No | 89 (86.4%) |
| Mean ± SD | |
|---|---|
| The number of treatment sessions | 1.8 ± 0.8 |
| GAS score | 2.3 ± 0.9 |
| ECCA score after treatment | 93.1 ± 34.7 |
| Modified Manchester Scar Scale (Color) | 2.0 ± 0.9 |
| Modified Manchester Scar Scale (Distortion) | 2.2 ± 0.9 |
| Modified Manchester Scar Scale (Texture) | 2.3 ± 0.8 |
| Pain level | 3.9 ± 0.8 |
| Persistent erythema (Days) | 30.7 ± 3.5 |
| Pigmentation (one month after treatment) | |
| No | 100 (97.1%) |
| Yes | 3 (2.9%) |
| Scar Type | Boxcar | Icepick | Rolling | p-Value |
|---|---|---|---|---|
| Number | 49 | 35 | 19 | |
| ECCA score before treatment | 165.5 ± 35.9 | 143.4 ± 53.6 | 190.8 ± 48.9 | <0.001 |
| ECCA score after treatment | 83.3 ± 29.6 | 92.6 ± 33.9 | 119.5 ± 36.1 | <0.001 |
| Modified Manchester Scar Scale (Color) | 2.4 ± 0.9 | 1.5 ± 0.7 | 1.8 ± 0.6 | <0.001 |
| Modified Manchester Scar Scale (Distortion) | 2.5 ± 0.9 | 1.8 ± 0.8 | 2.1 ± 0.8 | 0.002 |
| Modified Manchester Scar Scale (Texture) | 2.6 ± 0.8 | 1.7 ± 0.8 | 2.3 ± 0.7 | <0.001 |
| GAS Score | 2.7 ± 0.8 | 1.7 ± 0.8 | 2.3 ± 0.8 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pan, Z.; Tang, Y.; Hua, H.; Hou, Z.; Zhou, B. “Multiple Mode Procedures” of Ultra-Pulse Fractional CO2 Laser: A Novel Treatment Modality of Facial Atrophic Acne Scars. J. Clin. Med. 2023, 12, 4388. https://doi.org/10.3390/jcm12134388
Pan Z, Tang Y, Hua H, Hou Z, Zhou B. “Multiple Mode Procedures” of Ultra-Pulse Fractional CO2 Laser: A Novel Treatment Modality of Facial Atrophic Acne Scars. Journal of Clinical Medicine. 2023; 12(13):4388. https://doi.org/10.3390/jcm12134388
Chicago/Turabian StylePan, Zhonglan, Yanqiu Tang, Hui Hua, Zuoqiong Hou, and Bingrong Zhou. 2023. "“Multiple Mode Procedures” of Ultra-Pulse Fractional CO2 Laser: A Novel Treatment Modality of Facial Atrophic Acne Scars" Journal of Clinical Medicine 12, no. 13: 4388. https://doi.org/10.3390/jcm12134388
APA StylePan, Z., Tang, Y., Hua, H., Hou, Z., & Zhou, B. (2023). “Multiple Mode Procedures” of Ultra-Pulse Fractional CO2 Laser: A Novel Treatment Modality of Facial Atrophic Acne Scars. Journal of Clinical Medicine, 12(13), 4388. https://doi.org/10.3390/jcm12134388








