Subcutaneous Immunotherapy (SCIT) with the New Polymerized Molecular Allergoid Alt a1: A Pilot Study in Children with Allergic Rhinitis Sensitized to Alternaria Alternata
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Serological Biomarkers
2.3. Nasal Nitric Oxide (nFeNO)
2.4. Mean Nasal Flow (mNF) at AAR
2.5. Nasal Eosinophils Count at Nasal Cytology
2.6. Nasal Symptom Score (NSS)
2.7. Forced Expiratory Volume in the First Second (FEV1) at Spirometry
2.8. Schedule of Modigoid Administration
2.9. Statistical Analysis
3. Results
4. Discussion
4.1. Strength of the Study
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sarchet, P. The Allergy Epidemic. New Sci. 2018, 239, 28–33. [Google Scholar] [CrossRef]
- D’Amato, G.; Chong-Neto, H.J.; Monge Ortega, O.P.; Vitale, C.; Ansotegui, I.; Rosario, N.; Haahtela, T.; Galan, C.; Pawankar, R.; Murrieta-Aguttes, M.; et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy 2020, 75, 2219–2228. [Google Scholar] [CrossRef]
- D’Amato, G.; Holgate, S.T.; Pawankar, R.; Ledford, D.K.; Cecchi, L.; Al-Ahmad, M.; Al-Enezi, F.; Al-Muhsen, S.; Ansotegui, I.; Baena-Cagnani, C.E.; et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ. J. 2015, 8, 25. [Google Scholar] [CrossRef]
- Rao, C.Y.; Riggs, M.A.; Chew, G.L.; Muilenberg, M.L.; Thorne, P.S.; Van Sickle, D.; Dunn, K.H.; Brown, C. Characterization of Airborne Molds, Endotoxins, and Glucans in Homes in New Orleans after Hurricanes Katrina and Rita. Appl. Environ. Microbiol. 2007, 73, 1630–1634. [Google Scholar] [CrossRef]
- Harley, K.G.; Macher, J.M.; Lipsett, M.; Duramad, P.; Holland, N.T.; Prager, S.S.; Ferber, J.; Bradman, A.; Eskenazi, B.; Tager, I.B. Fungi and pollen exposure in the first months of life and risk of early childhood wheezing. Thorax 2009, 64, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Arbes, S.J., Jr.; Gergen, P.J.; Elliott, L.; Zeldin, D.C. Prevalences of positive skin test responses to 10 common allergens in the US population: Results from the Third National Health and Nutrition Examination Survey. J. Allergy Clin. Immunol. 2005, 116, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, D.; Tabar, A.I.; Castillo, M.; Martínez-Gomariz, M.; Dobski, I.C.; Palacios, R. Changes in the Sensitization Pattern to Alternaria alternata Allergens in Patients Treated with Alt a 1 Immunotherapy. J. Fungi 2021, 7, 974. [Google Scholar] [CrossRef] [PubMed]
- Salo, P.; Arbesjr, S.; Sever, M.; Jaramillo, R.; Cohn, R.; London, S.; Zeldin, D. Exposure to Alternaria alternata in US homes is associated with asthma symptoms. J. Allergy Clin. Immunol. 2006, 118, 892–898. [Google Scholar] [CrossRef]
- Downs, S.H.; Mitakakis, T.Z.; Marks, G.B.; Car, N.G.; Belousova, E.G.; Leüppi, J.D.; Xuan, W.; Downie, S.R.; Tobias, A.; Peat, J.K. Clinical Importance of Alternaria Exposure in Children. Am. J. Respir. Crit. Care Med. 2001, 164, 455–459. [Google Scholar] [CrossRef]
- Hernandez-Ramirez, G.; Barber, D.; Tome-Amat, J.; Garrido-Arandia, M.; Diaz-Perales, A. Alternaria as an Inducer of Allergic Sensitization. J. Fungi Basel Switz. 2021, 7, 838. [Google Scholar] [CrossRef]
- Rick, E.; Woolnough, K.; Pashley, C.; Wardlaw, A. Allergic Fungal Airway Disease. J. Investig. Allergol. Clin. Immunol. 2016, 26, 344–354. [Google Scholar] [CrossRef] [PubMed]
- De Vittori, V.; Pacilio, A.; Indinnimeo, L.; Marazzato, M.; De Castro, G.; Brindisi, G.; Schiavi, L.; Tosca, M.; Duse, M.; Zicari, A.M. When asthma and rhinitis coexist, could rhinitis reduce asthma control in children? Allergy Asthma Proc. 2019, 40, 210. [Google Scholar] [CrossRef] [PubMed]
- Brindisi, G.; De Vittori, V.; De Nola, R.; Di Mauro, A.; De Castro, G.; Baldassarre, M.E.; Cicinelli, E.; Cinicola, B.; Duse, M.; Zicari, A.M. The Role of Nasal Nitric Oxide and Anterior Active Rhinomanometry in the Diagnosis of Allergic Rhinitis and Asthma: A Message for Pediatric Clinical Practice. J. Asthma Allergy 2021, 14, 265–274. [Google Scholar] [CrossRef]
- Ridolo, E.; Incorvaia, C.; Heffler, E.; Cavaliere, C.; Paoletti, G.; Canonica, G.W. The Present and Future of Allergen Immunotherapy in Personalized Medicine. J. Pers. Med. 2022, 12, 774. [Google Scholar] [CrossRef] [PubMed]
- Alvaro-Lozano, M.; Akdis, C.A.; Akdis, M.; Alviani, C.; Angier, E.; Arasi, S.; Arzt-Gradwohl, L.; Arasi, L.; Barber, D.; Bazire, R.; et al. Allergen Immunotherapy in Children User’s Guide. Pediatr. Allergy Immunol. 2020, 31, 1–101. [Google Scholar] [CrossRef]
- Kucuksezer, U.C.; Ozdemir, C.; Cevhertas, L.; Ogulur, I.; Akdis, M.; Akdis, C.A. Mechanisms of allergen-specific immunotherapy and allergen tolerance. Allergol. Int. 2020, 69, 549–560. [Google Scholar] [CrossRef]
- Tabar, A.I.; Lizaso, M.T.; García, B.E.; Gómez, B.; Echechipía, S.; Aldunate, M.T.; Madariaga, B.; Martínez, A. Double-blind, placebo-controlled study of Alternaria alternata immunotherapy: Clinical efficacy and safety. Pediatr. Allergy Immunol. 2007, 19, 67–75. [Google Scholar] [CrossRef]
- Lizaso, M.T.; Tabar, A.I.; García, B.E.; Gómez, B.; Algorta, J.; Asturias, J.A.; Martínez, A. Double-blind, placebo-controlled Alternaria alternata immunotherapy: In vivo and in vitro parameters. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2008, 19, 76–81. [Google Scholar] [CrossRef]
- Kuna, P.; Kaczmarek, J.; Kupczyk, M. Efficacy and safety of immunotherapy for allergies to Alternaria alternata in children. J. Allergy Clin. Immunol. 2011, 127, 502–508.e6. [Google Scholar] [CrossRef]
- Prieto, L.; Palacios, R.; Aldana, D.; Ferrer, A.; Perez-Frances, C.; Lopez, V.; Rojas, R. Effect of allergen-specific immunotherapy with purified Alt a1 on AMP responsiveness, exhaled nitric oxide and exhaled breath condensate pH: A randomized double blind study. Allergy Asthma Clin. Immunol. 2010, 6, 27. [Google Scholar] [CrossRef]
- Tabar, A.I.; Prieto, L.; Alba, P.; Nieto, A.; Rodríguez, M.; Torrecillas, M.; Huertas, B.; Gómez, E.; Fernández, F.J.; Blanca, M.; et al. Double-blind, randomized, placebo-controlled trial of allergen-specific immunotherapy with the major allergen Alt a 1. J. Allergy Clin. Immunol. 2019, 144, 216–223.e3. [Google Scholar] [CrossRef] [PubMed]
- Musa, F.; Al-Ahmad, M.; Arifhodzic, N.; Al-Herz, W. Compliance with allergen immunotherapy and factors affecting compliance among patients with respiratory allergies. Hum. Vaccines Immunother. 2017, 13, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Pfützner, W.; Möbs, C. AIT: New Avenues in Allergen Immunotherapy. In Allergic Diseases—From Basic Mechanisms to Comprehensive Management and Prevention; Traidl-Hoffmann, C., Zuberbier, T., Werfel, T., Eds.; Handbook of Experimental Pharmacology; Springer International Publishing: Cham, Switzerland, 2021; Volume 268, pp. 135–149. ISBN 978-3-030-84047-1. [Google Scholar]
- Roberts, G.; Pfaar, O.; Akdis, C.A.; Ansotegui, I.J.; Durham, S.R.; Gerth Van Wijk, R.; Halken, S.; Larenas-Linnemann, D.; Pawankar, R.; Pitsios, C.; et al. EAACI Guidelines on Allergen Immunotherapy: Allergic rhinoconjunctivitis. Allergy 2018, 73, 765–798. [Google Scholar] [CrossRef] [PubMed]
- Schiavi, L.; Brindisi, G.; De Castro, G.; De Vittori, V.; Loffredo, L.; Spalice, A.; Duse, M.; Zicari, A.M. Nasal reactivity evaluation in children with allergic rhinitis receiving grass pollen sublingual immunotherapy. Allergy Asthma Proc. 2020, 41, 357–362. [Google Scholar] [CrossRef]
- Brożek, J.L.; Bousquet, J.; Agache, I.; Agarwal, A.; Bachert, C.; Bosnic-Anticevich, S.; Brignardello-Petersen, R.; Canonica, G.W.; Casale, T.; Chavannes, N.H.; et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines—2016 revision. J. Allergy Clin. Immunol. 2017, 140, 950–958. [Google Scholar] [CrossRef]
- Reddel, H.K.; Bacharier, L.B.; Bateman, E.D.; Brightling, C.E.; Brusselle, G.G.; Buhl, R.; Cruz, A.A.; Duijts, L.; Drazen, J.M.; FitzGerald, J.M.; et al. Global Initiative for Asthma Strategy 2021: Executive summary and rationale for key changes. Eur. Respir. J. 2022, 59, 2102730. [Google Scholar] [CrossRef]
- Cipriani, F.; Tripodi, S.; Panetta, V.; Perna, S.; Potapova, E.; Dondi, A.; Bernardini, R.; Caffarelli, C.; Casani, A.; Cervone, R.; et al. Early molecular biomarkers predicting the evolution of allergic rhinitis and its comorbidities: A longitudinal multicenter study of a patient cohort. Pediatr. Allergy Immunol. 2019, 30, 325–334. [Google Scholar] [CrossRef]
- American Thoracic Society; European Respiratory Society. ATS/ERS Recommendations for Standardized Procedures for the Online and Offline Measurement of Exhaled Lower Respiratory Nitric Oxide and Nasal Nitric Oxide, 2005. Am. J. Respir. Crit. Care Med. 2005, 171, 912–930. [Google Scholar] [CrossRef]
- Manna, A.; Montella, S.; Maniscalco, M.; Maglione, M.; Santamaria, F. Clinical application of nasal nitric oxide measurement in pediatric airway diseases: Nasal Nitric Oxide in Pediatric Airways. Pediatr. Pulmonol. 2015, 50, 85–99. [Google Scholar] [CrossRef]
- Clement, P.a.R.; Gordts, F. Standardisation Committee on Objective Assessment of the Nasal Airway, IRS, and ERS Consensus report on acoustic rhinometry and rhinomanometry. Rhinology 2005, 43, 169–179. [Google Scholar]
- Cilluffo, G.; Zicari, A.M.; Ferrante, G.; Malizia, V.; Fasola, S.; Duse, M.; De Castro, G.; De Vittori, V.; Schiavi, L.; Brindisi, G.; et al. Assessing repeatability and reproducibility of Anterior Active Rhinomanometry (AAR) in children. BMC Med. Res. Methodol. 2020, 20, 86. [Google Scholar] [CrossRef] [PubMed]
- Zapletal, A.; Chalupová, J. Nasal airflow and resistance measured by active anterior rhinomanometry in healthy children and adolescents: Rhinomanometry in Healthy Children. Pediatr. Pulmonol. 2002, 33, 174–180. [Google Scholar] [CrossRef]
- Gelardi, M.; Iannuzzi, L.; Quaranta, N.; Landi, M.; Passalacqua, G. NASAL cytology: Practical aspects and clinical relevance. Clin. Exp. Allergy 2016, 46, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.R. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef] [PubMed]
- Matricardi, P.M. Molecular profile clustering of IgE responses and potential implications for specific immunotherapy. Curr. Opin. Allergy Clin. Immunol. 2013, 13, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Matricardi, P.M.; Dramburg, S.; Potapova, E.; Skevaki, C.; Renz, H. Molecular diagnosis for allergen immunotherapy. J. Allergy Clin. Immunol. 2019, 143, 831–843. [Google Scholar] [CrossRef]
- Asturias, J.A.; Ibarrola, I.; Ferrer, A.; Andreu, C.; López-Pascual, E.; Quiralte, J.; Florido, F.; Martínez, A. Diagnosis of Alternaria alternata sensitization with natural and recombinant Alt a 1 allergens. J. Allergy Clin. Immunol. 2005, 115, 1210–1217. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, A. Clinical evaluation of subcutaneous immunotherapy with a polymerized molecular allergoid of Alt a 1 in patients with allergic rhinoconjunctivitis and/or allergic asthma caused by the mould Alternaria alternata. Eur. Ann. Allergy Clin. Immunol. 2022, 1–18. [Google Scholar] [CrossRef]
- Morales, M.; Gallego, M.T.; Iraola, V.; Moya, R.; Santana, S.; Carnés, J. Preclinical safety and immunological efficacy of Alternaria alternata polymerized extracts. Immunity Inflamm. Dis. 2018, 6, 234–244. [Google Scholar] [CrossRef]
- Liu, J.; Li, J.; Yin, J. Clinical relevance of Alternaria alternata sensitization in patients within type 2-high and type 2-low asthma. Int. Immunopharmacol. 2021, 101, 108333. [Google Scholar] [CrossRef]
- Chruszcz, M.; Chapman, M.D.; Osinski, T.; Solberg, R.; Demas, M.; Porebski, P.J.; Majorek, K.A.; Pomés, A.; Minor, W. Alternaria alternata allergen Alt a 1: A unique β-barrel protein dimer found exclusively in fungi. J. Allergy Clin. Immunol. 2012, 130, 241–247.e9. [Google Scholar] [CrossRef] [PubMed]
- Hasan-Abad, A.M.; Mohammadi, M.; Mirzaei, H.; Mehrabi, M.; Motedayyen, H.; Arefnezhad, R. Impact of oligomerization on the allergenicity of allergens. Clin. Mol. Allergy 2022, 20, 5. [Google Scholar] [CrossRef] [PubMed]
- Olivier, C.E. The use of Allergoids and Adjuvants in Allergen Immunotherapy. Arch. Asthma Allergy Immunol. 2017, 1, 40–60. [Google Scholar] [CrossRef]
- Grammer, L.C.; Patterson, R. Development of polymerized allergens for immunotherapy. Asian Pac. J. Allergy Immunol. 1983, 1, 55–58. [Google Scholar] [PubMed]




| Characteristic | Control Group | Treatment Group | p-Value |
|---|---|---|---|
| N. patients, n (%) | 25 | 17 | |
| Male | 21 (84%) | 15 (88.2%) | |
| Age, mean ± SD, years | 12.25 ± 6.26 | 12.55 ± 2.88 | 0.265 |
| Weight, mean ± SD, Kg | 43.19 ± 9.22 | 44.55 ± 8.23 | 0.672 |
| Height, mean ± SD, cm | 152.36 ± 10.80 | 154.68 ± 10.96 | 0.564 |
| Allergic Rhinitis | |||
| Moderately persistent, n (%) | 25 (100%) | 17 (100%) | |
| Asthma | |||
| mild intermittent, n (%) | 25 (100%) | 17 (100%) |
| Characteristic | Value | p-Value Intragroup | |||
|---|---|---|---|---|---|
| T0 | T1 | ||||
| Mean ± SD | p-Value Intergroup | Mean ± SD | p-Value Intergroup | ||
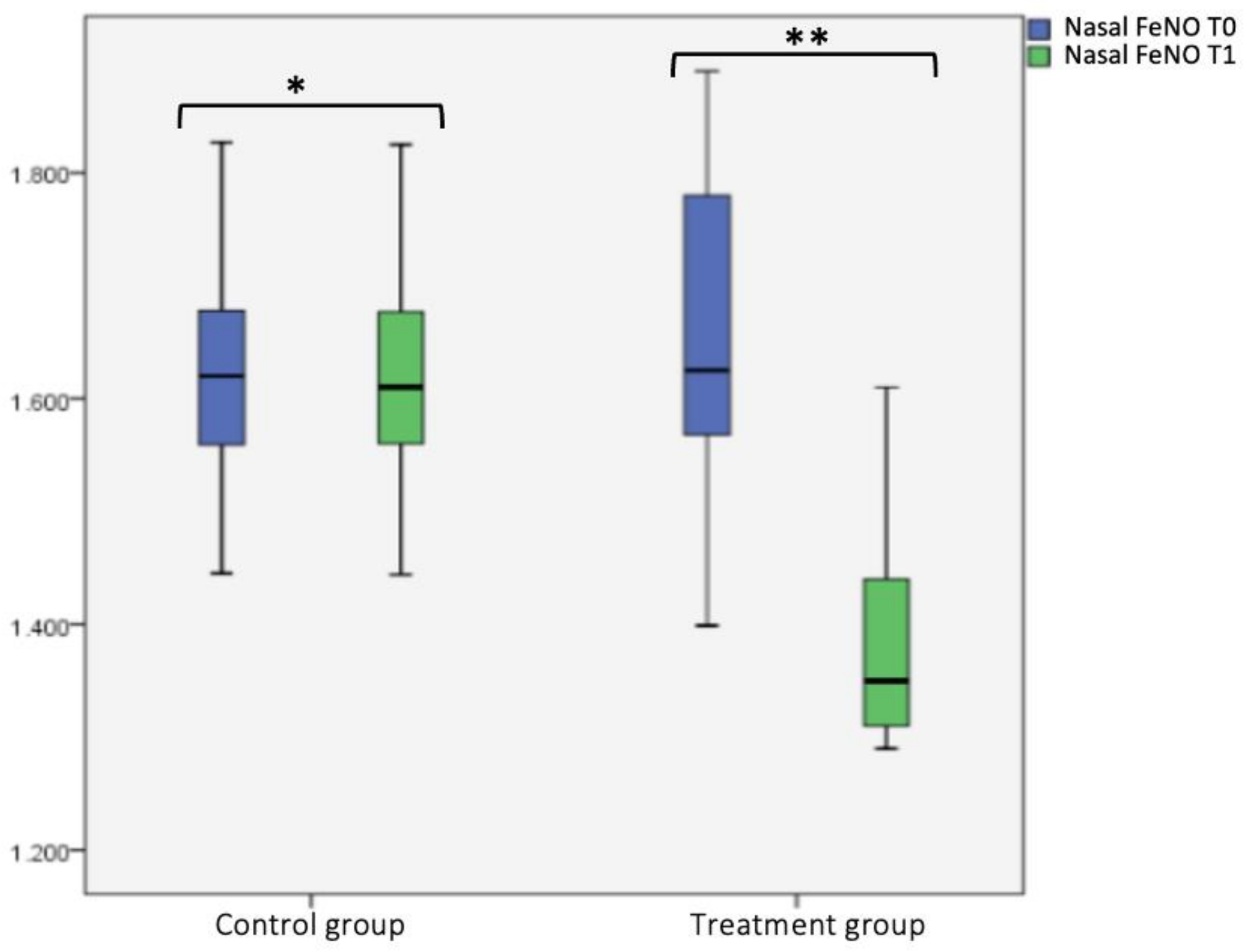
| Nasal FeNO (nFeNO) | |||||
| -Control group | 1613.40 ± 104.63 | p = 0.341 | 1612.84 ± 104.47 | p < 0.001 | p = 0.248 |
| -Treatment group | 1651.06 ± 149.18 | 1394.12 ± 108.98 | p < 0.001 | ||
| IgE total, Ku/L | |||||
| -Control group | 311.84 ± 156.22 | p = 0.994 | 311.89 ± 156.41 | p < 0.001 | p = 0.813 |
| -Treatment group | 311.48 ± 144.18 | 164.74 ± 50.69 | p < 0.001 | ||
| Alt a1, Ku/L | |||||
| -Control group | 28.12± 11.46 | p = 0.902 | 27.95 ± 11.38 | p = 0.006 | p = 0.457 |
| -Treatment group | 28.58 ± 12.69 | 19.54 ± 7.37 | p < 0.001 | ||
| mNF (%) pre-hydrazine | |||||
| -Control group | 63.67 ± 12.23 | p = 0.652 | 80.8 8± 5.54 | p < 0.001 | p = 0.75 |
| -Treatment group | 61.98 ± 11.65 | 62.04 ± 12.09 | p < 0.001 | ||
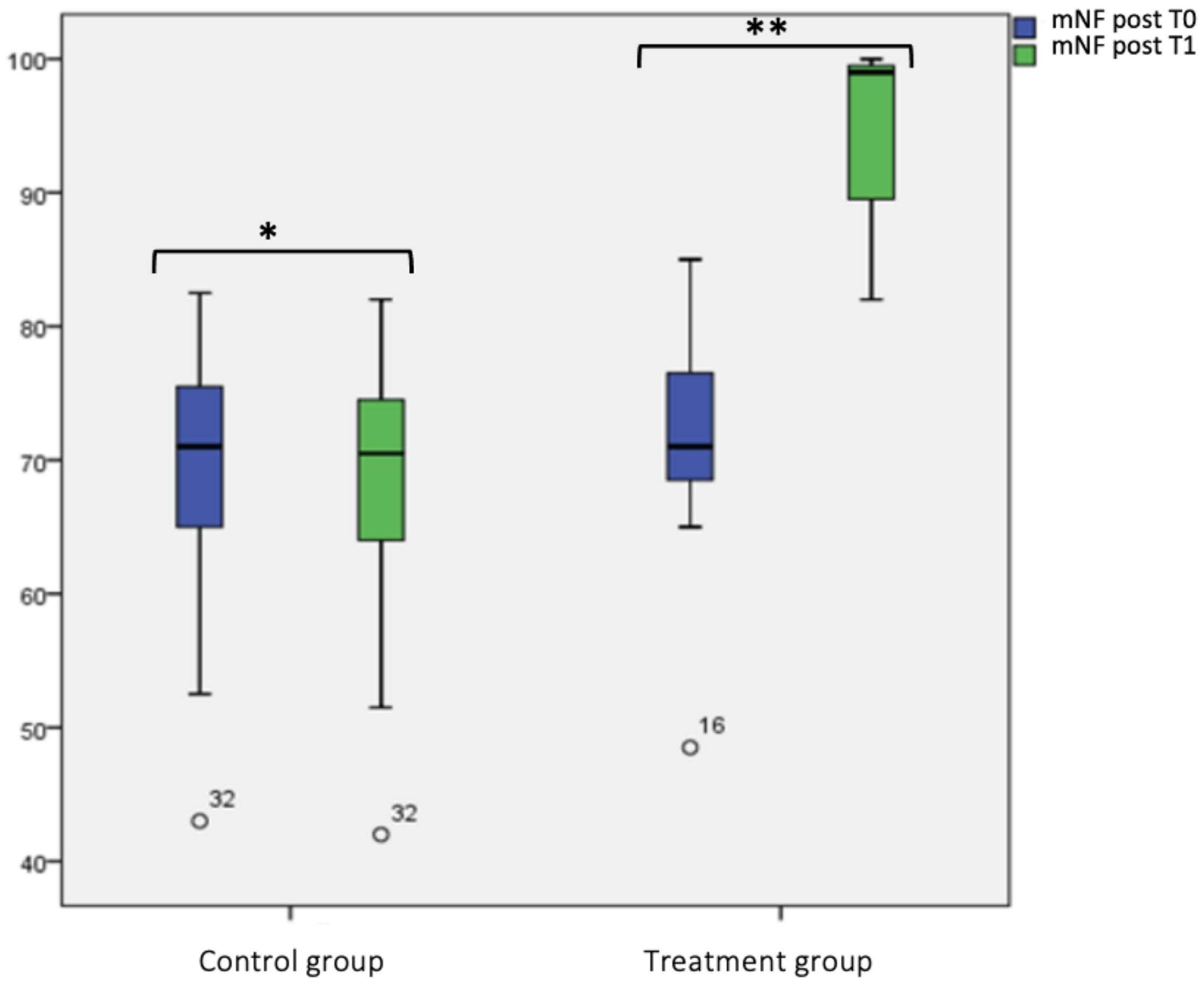
| mNF (%) post-hydrazine | |||||
| -Control group | 71.61 ± 8.65 | p = 0.8 | 95.12 ± 5.9 | p < 0.001 | p = 0.988 |
| -Treatment group | 69.12 ± 9.13 | 69.12 ± 9.44 | p < 0.001 | ||
| Nasal eosinophils | |||||
| -Control group | 18.96 ± 2.45 | p = 0.541 | 18.96 ± 2.34 | p < 0.001 | p = 0.995 |
| -Treatment group | 19.47 ± 2.87 | 9.65 ± 4.20 | p < 0.001 | ||
| Nasal symptom score | |||||
| -Control group | 20.58 ± 2.34 | p = 0.4 | 14.88 ± 1.65 | p < 0.001 | p = 0.841 |
| -Treatment group | 21.16 ± 1.77 | 21.2 ± 1.58 | p < 0.001 | ||
| FEV1 pre-broncodilatation | |||||
| -Control group | 84.92± 3.94 | p = 0.579 | 84.96 ± 4.35 | p < 0.001 | p = 0.846 |
| -Treatment group | 85.7± 5.16 | 100.23 ± 1.35 | p < 0.001 | ||
| FEV1 post-broncodilatation | |||||
| -Control group | 93.84± 5.01 | p = 0.385 | 93.88 ± 5.44 | p < 0.001 | p = 0.845 |
| -Treatment group | 95.59± 7.91 | 116.65 ± 5.95 | p < 0.001 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brindisi, G.; Gori, A.; Anania, C.; Martinelli, I.; Capponi, M.; De Castro, G.; Zicari, A.M. Subcutaneous Immunotherapy (SCIT) with the New Polymerized Molecular Allergoid Alt a1: A Pilot Study in Children with Allergic Rhinitis Sensitized to Alternaria Alternata. J. Clin. Med. 2023, 12, 4327. https://doi.org/10.3390/jcm12134327
Brindisi G, Gori A, Anania C, Martinelli I, Capponi M, De Castro G, Zicari AM. Subcutaneous Immunotherapy (SCIT) with the New Polymerized Molecular Allergoid Alt a1: A Pilot Study in Children with Allergic Rhinitis Sensitized to Alternaria Alternata. Journal of Clinical Medicine. 2023; 12(13):4327. https://doi.org/10.3390/jcm12134327
Chicago/Turabian StyleBrindisi, Giulia, Alessandra Gori, Caterina Anania, Ivana Martinelli, Martina Capponi, Giovanna De Castro, and Anna Maria Zicari. 2023. "Subcutaneous Immunotherapy (SCIT) with the New Polymerized Molecular Allergoid Alt a1: A Pilot Study in Children with Allergic Rhinitis Sensitized to Alternaria Alternata" Journal of Clinical Medicine 12, no. 13: 4327. https://doi.org/10.3390/jcm12134327
APA StyleBrindisi, G., Gori, A., Anania, C., Martinelli, I., Capponi, M., De Castro, G., & Zicari, A. M. (2023). Subcutaneous Immunotherapy (SCIT) with the New Polymerized Molecular Allergoid Alt a1: A Pilot Study in Children with Allergic Rhinitis Sensitized to Alternaria Alternata. Journal of Clinical Medicine, 12(13), 4327. https://doi.org/10.3390/jcm12134327






